
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Kyung-San Min | + 2727 word(s) | 2727 | 2021-03-29 05:37:35 | | | |
| 2 | Dean Liu | -944 word(s) | 1783 | 2021-04-09 05:26:23 | | |
Video Upload Options
Endodontic microsurgery is a highly predictable treatment option in most cases when conventional endodontic treatment is not feasible.
1. Introduction
Endodontic treatment aims to disinfect the root canal system, followed by sealing this space to prevent recontamination [1]. For this purpose, nonsurgical endodontic treatment is the first option in most cases, but a surgical approach may be indicated when peri-radicular pathosis cannot be solved by a nonsurgical method [2]. Surgical endodontic treatment has evolved considerably owing to new technological advances such as dental operating microscopes, cone-beam computed tomography (CBCT), computer-aided design/computer-aided manufacturing (CAD/CAM), and three-dimensional printing technology. Most endodontists now consider the above equipment essential for surgical endodontic treatment.
Nevertheless, clinicians still consider mandibular molars to be the most difficult targets. The success rate for mandibular molars is lower than that for any other type of teeth in the oral cavity [3]. The difficulty posed by mandibular molars is their anatomical location in the posterior areas of the oral cavity. Even in a retrospective study that used a 15-year database obtained in the 21st century, molars showed a higher probability of failure than anterior teeth, and tooth type might be the only factor contributing to the outcomes of microsurgery [4]. Therefore, microsurgery of mandibular molars requires an adequate evaluation of the surgical access and the relationship of the roots to anatomical structures such as the mental foramen and mandibular canal [5].
2. Anatomical Considerations
2.1. Thickness of the Buccal Bone
The buccal bone of the mandibular molar area is thicker than in other areas. The thickness of the posterior buccal cortical plate is generally 2–3 mm on average (Figure 1a). Furthermore, this thickness may increase posteriorly (oblique ridge), limiting access to the molar roots (Figure 1b). While the mesial root of the mandibular first molar is reasonably close to the buccal cortical plate, the distal root is centrally located in the bone and the roots of the second molar are significantly closer to the lingual cortical plate [6]. Therefore, mandibular molars with a thick buccal bone plate pose a challenging problem in endodontic surgery, especially for precise root-end localization.
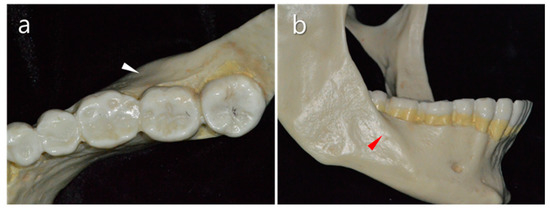
Figure 1. Anatomical features of the mandibular molar area. (a) Thick buccal bone of the mandible (white triangle). (b) Oblique ridge in the second mandibular molar area (red triangle).
Recently, Bi et al. [7] reported a sophisticated approach that reduced the distance between the roots and the buccal cortical plate by orthodontic movement. By orthodontic movement toward the buccal aspect for 2 months, the distance between the two anatomical structures was decreased from 4.5 mm to 1.5 mm (mesial root) and 7.1 mm to 4.5 mm (distal root). Therefore, the surgical procedure became easier and the results were successful. Furthermore, Ahn et al. [8] performed osteotomy and apex localization effectively using a CAD/CAM-guided surgical template in a mandibular molar with a thick buccal bone plate (Figure 2). Indeed, the surgical template manufactured by using CAD/CAM technology combined with CBCT can determine the three-dimensional extent of the required cortical bony window. Therefore, with this guide, the surgical approach to the apical region is less invasive and less traumatic so that minimizes bone loss in comparison to the traditional osteotomy techniques [9]. However, even with this static technique, clinicians may have problems regarding the instrumentation during the surgical procedure. In this respect, most recently, dynamic navigation systems for dental implant positioning were applied to endodontic microsurgery [10]. This dynamic navigation integrates surgical procedure and radiologic images by using an optical positioning device controlled by a dedicated computerized interface. Consequently, with the help of cutting-edge guiding technologies, clinicians can perform a safe and less traumatic surgical procedure in the mandibular molar area, and unfavorable complications including increased postoperative pain, delayed healing, and nerve damage can be avoided.
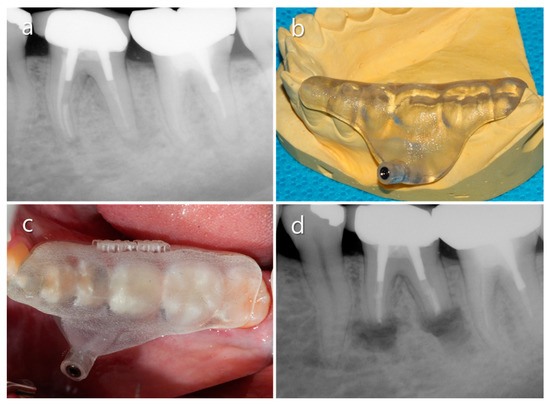
Figure 2. Clinical case using a computer-aided design/computer-aided manufacturing (CAD/CAM)-guided surgical template to localize the root apex through thick. (a) Diagnostic periapical X-ray. (b) A manufactured surgical template. (c) The surgical template was positioned on the tooth. (d) Postoperative radiograph.
2.2. Vestibular Fornix
The depth of the vestibular fornix is considered a reliable predictor of the possible difficulty that may be encountered during periapical surgery of the mandibular posterior teeth [11]. If the vestibular fornix is shallow, the buccal alveolar bone overlying the roots will be thick and consequently access to the root end will be limited. In some cases, therefore, the buccal cortical plate can be reduced before exploring for the periapical lesion or root end (Figure 3). In this procedure, the surgical concept of vestibuloplasty can be applied. However, clinicians should bear in mind that this procedure may destroy a considerable amount of bone. Instead of endodontic surgery, extraction and replantation/dental implantation can be a less traumatic alternative, especially for mandibular second molars.
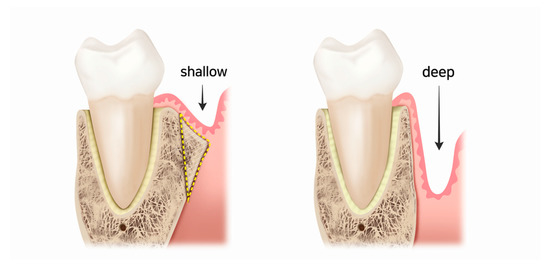
Figure 3. Drawings of mandibular molars and their mesiodistal supporting structures. The vestibular fornix becomes deeper by reducing the buccal cortical plate.
2.3. Mandibular Canal
The mandibular canal is sometimes in the proximity of the roots of all mandibular molars (Figure 4a). According to a systematic review, the shortest distances from the superior cortical bone of the mandibular canal to the first and second molars were 3.82 mm and 1.4 mm, respectively [12]. Even a direct contact relationship was found in 3.3% of the first molar and 16% of the second molar [13]. Furthermore, the distance from the root to the canal was shorter in younger people (<21-year-old) than in older people [13][14]. Anatomically, the mandibular canal is situated lingually to the roots of the mandibular first molars (Figure 4b).
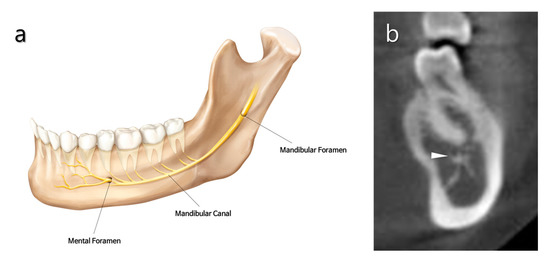
Figure 4. Anatomical features of the mandibular canal and mental foramen. (a) Schematic illustration of human mandible showing the innervation of mandibular and mental nerves. (b) Transverse section of a cone-beam compute tomography (CBCT) scan through the mandible in the region of the root of the first molar. The mandibular canal (white triangle) is closely located lingual to the root apex.
The borders of the mandibular canal are often difficult to visualize with conventional radiographic techniques (Figure 5a). A parallel periapical radiograph, either horizontally or vertically positioned, can usually provide a reasonably accurate image of the relationship between the superior border of the mandibular canal and the root apices. CBCT imaging can be very useful for identifying the location of the mandibular canal and determining its relationship to the root apices (Figure 5b) [15]. Martí et al. [16] reported that periapical surgery is a valid treatment option for mandibular molars, even those situated in close proximity to the mandibular canal (less than 2 mm).
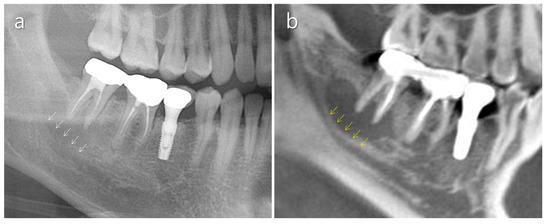
Figure 5. Usefulness of CBCT for identifying the mandibular canal. (a) Unclear mandibular canal border in a conventional panoramic radiograph. Periapical bone resorption adjacent to the mandibular canal makes identification of the upper border of the canal difficult (white arrows). (b) A CBCT scan shows the upper border of the mandibular canal remarkably well (yellow arrows).
2.4. Mental Nerve
The mental nerve, a branch of the inferior alveolar nerve, emerges with the mental artery through the mental foramen to supply the oral mucosa and the skin of the lower lip and chin (Figure 6). It can be damaged during flap retraction, and paresthesia may occur. The mental foramen usually appears on a radiograph as a round radiolucent area below the mandibular second premolar root apex. However, its location varies and it may be seen at the same level or superior to the root apices [11].
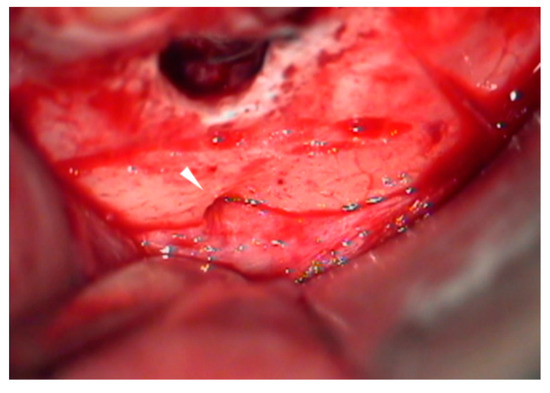
Figure 6. Clinical features of the mental foramen and nerve bundle (white triangle) that are detected during the surgical procedure.
The mental foramen is most usually single in humans; when it is double or multiple, the additional foramen is termed an accessory mental foramen. Accessory mental foramina are reported to be rare, with a prevalence ranging from 1.4% to 10% [17][18][19][20]. Moreover, Iwanaga et al. [21] reported that accessory mental foramina smaller than 1.3 mm2 were not clearly identified on surface-rendered CBCT images. In this respect, paresthesia may occur even if the clinician does not recognize the damage to the mental nerve [22][23].
Gutmann and Harrison [5] suggested protecting the mental nerve by positioning the periosteal retractor between the mental foramen and the intraosseous surgical site. More recently, Kim and Kratchman [24] suggested an effective tip, the “groove technique”, to prevent mental nerve damage. Briefly, a 15-mm-long horizontal groove is prepared beyond the root apex and the retractor is positioned within the groove (Figure 7a). This technique permits the secure retraction of the flap protecting the nerve during the procedure. Recently, the use of a piezoelectric saw instead of a bur has been shown to be useful to obtain a groove as narrow as is practical for the placement of the retractor (Figure 7b). By using this method, excessive bone removal can be avoided.

Figure 7. The groove technique. (a) A narrow horizontal groove is positioned just above the mental foramen (white line). (b) Clinical feature of a practically narrow groove made using the piezoelectric saw. Note that the nerve/vessel bundle comes from the foramen (white arrow).
2.5. Distolingual Root
Mandibular first permanent molars usually have two roots located mesially and distally, but in Asian populations, an additional distolingual root is considered a normal morphological variant [25][26]. In two studies conducted in Korea, the prevalence of independent distolingual roots was 24.5% and 22.8%, respectively [27][28]. These separate distolingual roots of mandibular first molars are considered too difficult for performing periapical surgery due to the considerable distance from the buccal cortical plate (8.63 mm) [28].
Due to this difficulty, few case reports have described surgical endodontic management of these roots. To our knowledge, only one report was found [29], and the authors performed a reduced amount (2 mm) of root resection and root-end preparation and suggested that distolingual roots can be successfully treated by modifying the standard protocol. Nevertheless, periapical surgery for the distolingual root should be undertaken with careful deliberation due to the technical difficulty.
2.6. Mandibular Second Molars
Due to their location, endodontic microsurgery for mandibular second molars is seldom attempted even by endodontic specialists. Access to the root apex of the teeth is usually obtained by intentional replantation since the roots often have a convergent form. Nevertheless, a surgical approach for mandibular second molars is attempted in certain situations, such as abutment of fixed prosthodontics (Figure 8). In endodontic surgery for second molars, the position of the mandibular canal should be considered carefully. The mandibular canal is located buccal to the apex of the second molar, but lingual to the apex of the first molar in most cases [30]. Furthermore, it was reported that the second molars had a close distance to the canal (mean, 3.7 mm).
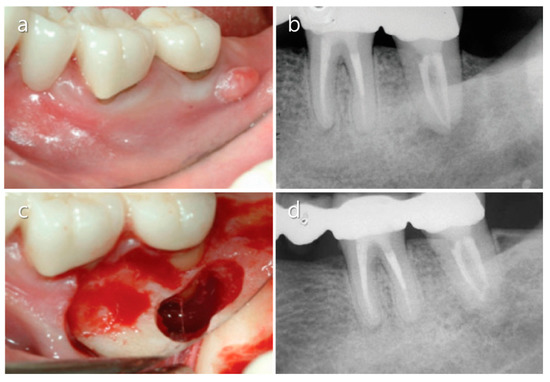
Figure 8. Endodontic surgery of a mandibular second molar. (a) Sinus tract formed on the buccal aspect of a left mandibular second molar. (b) Diagnostic periapical X-ray image showing that the tooth was an abutment for a fixed prosthodontic restoration. (c) The root apex was exposed after osteotomy. (d) A five-year follow-up radiograph shows complete bony healing. Images were modified from Song [31] after receiving permission from the journal.
References
- Tabassum, S.; Khan, F.R. Failure of endodontic treatment: The usual suspects. Eur. J. Dent. 2016, 10, 144–147.
- Monaghan, L.; Jadun, S.; Darcey, J. Endodontic microsurgery. Part one: Diagnosis, patient selection and prognoses. Br. Dent. J. 2019, 226, 940–948.
- Pallarés-Serrano, A.; Glera-Suarez, P.; Tarazona-Alvarz, B.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Prognostic factors after endodontic microsurgery: A retrospective Study of 111 cases with 5-9 years of follow-up. J. Endod. 2021, 47, 397–403.
- Kim, D.; Kim, S.; Song, M.; Kang, D.R.; Kohli, M.R.; Kim, E. Outcome of endodontic micro-resurgery: A retrospective study based on propensity score-matched survival analysis. J. Endod. 2018, 44, 1632–1640.
- Wang, X.; Chen, K.; Wang, S.; Tiwari, S.K.; Ye, L.; Peng, L. Relationship between the mental foramen, mandibular canal, and the surgical access line of the mandibular posterior teeth: A cone-beam computed tomographic analysis. J. Endod. 2017, 43, 1262–1266.
- Gutmann, J.L.; Harroson, J.W. Posterior endodontic surgery: Anatomical considerations and clinical techniques. Int. Endod. J. 1985, 18, 8–34.
- Bi, C.; Zhou, M.; Han, X.; Zhang, Y.; Zheng, P. Endodontic microsurgery with orthodontic treatment in a mandibular left molar with symptomatic apical periodontitis. J. Endod. 2020, in press.
- Ahn, S.Y.; Kim, N.H.; Kim, S.; Karabucak, B.; Kim, E. Computer-aided design/computer-aided manufacturing-guided endodontic surgery: Guided osteotomy and apex localization in a mandibular molar with a thick buccal bone plate. J. Endod. 2018, 44, 665–670.
- Kim, J.E.; Shim, J.S.; Shin, Y. A new minimally invasive guided endodontic microsurgery by cone beam computed tomography and 3-dimensional printing technology. Restor. Dent. Endod. 2019, 44, e29.
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic microsurgery using dynamic avigation system: A case report. J. Endod. 2019, 45, 1397–1402.
- Lin, L.; Skribner, J.; Shovlin, F.; Langeland, K. Periapical surgery of mandibular posterior teeth: Anatomical and surgical considerations. J. Endod. 1983, 9, 496–501.
- Puciło, M.; Lipski, M.; Sroczyk-Jaszczyńska, M.; Puciło, A.; Nowicka, A. The anatomical relationship between the roots of erupted permanent teeth and the mandibular canal: A systematic review. Surg. Radiol. Anat. 2020, 42, 529–542.
- Aksoy, U.; Aksoy, S.; Orhan, K. A cone-beam computed tomography study of the anatomical relationships between mandibular teeth and the mandibular canal, with a review of the current literature. Microsc. Res. Tech. 2018, 81, 308–314.
- Kawashima, Y.; Sakai, O.; Shosho, D.; Kaneda, T.; Gohel, A. Proximity of the mandibular canal to teeth and cortical bone. J. Endod. 2016, 42, 221–224.
- Velvart, P.; Hecker, H.; Tillinger, G. Detection of the apical lesion and the mandibular canal in conventional radiography and computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 92, 682–688.
- Martí, E.; Peñarrocha, M.; García, B.; Martínez, J.M.; Gay-Escoda, C. Distance between periapical lesion and mandibular canal as a factor in periapical surgery in mandibular molars. J. Oral Maxillofac. Surg. 2008, 66, 2461–2466.
- Igarashi, C.; Kobayashi, K.; Yamamoto, A.; Morita, Y.; Tanaka, M. Double mental foramina of the mandible on computed tomography images: A case report. Oral Radiol. 2004, 20, 68–71.
- Cagirankaya, L.B.; Kansu, H. An accesory mental foramen: A case report. J. Contemp. Dent. Pract. 2008, 9, 98–104.
- Kieser, J.; Kuzmanovic, D.; Payne, A.; Dennison, J.; Herbison, P. Patterns of emergence of the human mental nerve. Arch. Oral Biol. 2002, 47, 743–747.
- Han, S.S.; Hwang, J.J.; Jeong, H.G. Accessory mental foramina associated with neurovascular bundle in Korean population. Surg. Radiol. Anat. 2016, 38, 1169–1174.
- Iwanaga, J.; Watanabe, K.; Saga, T.; Kikuta, S.; Tabira, Y.; Kitashima, S.; Fisahn, C.; Alonso, F.; Tubbs, R.S.; Kusukawa, J.; et al. Undetected small accessory mental foramina using cone-beam computed tomography. Cureus 2017, 9, e1210.
- Iwanaga, J.; Saga, T.; Tabira, Y.; Nakamura, M.; Kitashima, S.; Watanabe, K.; Kusukawa, J.; Yamaki, K.I. The clinical anatomy of accessory mental nerves and foramina. Clin. Anat. 2015, 28, 848–856.
- Concepcion, M.; Rankow, H.J. Accessory branch of the mental nerve. J. Endod. 2000, 26, 619–620.
- Kim, S.; Kratchman, S. Modern endodontic surgery concepts and practice: A review. J. Endod. 2006, 32, 601–623.
- Wang, Y.; Zheng, Q.H.; Zhou, X.D.; Tang, L.; Wang, Q.; Zheng, G.N.; Huang, D.M. Evaluation of the root and canal morphology of mandibular first permanent molars in a western Chinese population by cone-beam computed tomography. J. Endod. 2010, 36, 1786–1789.
- Tu, M.G.; Tsai, C.C.; Jou, M.J.; Chen, W.L.; Chang, Y.F.; Chen, S.Y.; Cheng, H.W. Prevalence of three-rooted mandibular first molars among Taiwanese individuals. J. Endod. 2007, 33, 1163–1166.
- Song, J.S.; Choi, H.J.; Jung, I.Y.; Jung, H.S.; Kim, S.O. The prevalence and morphologic classification of distolingual roots in the mandibular molars in a Korean population. J. Endod. 2010, 36, 653–657.
- Kim, S.Y.; Yang, S.E. Cone-beam computed tomography study of incidence of distolingual root and distance from distolingual canal to buccal cortical bone of mandibular first molars in a Korean population. J. Endod. 2012, 38, 301–304.
- Wang, H.G.; Xu, N.; Yu, Q. Endodontic microsurgical treatment of a three-rooted mandibular first molar with separate distolingual root: Report of one case. Chin. J. Dent. Res. 2016, 19, 171–174.
- Littner, M.M.; Kaffe, I.; Tamise, A.; Dicapua, P. Relationship between the apices of the lower molars and mandibular canals—A radiographic study. Oral Surg. Oral Med. Oral Pathol. 1986, 62, 595–602.
- Song, Y. Periapical surgery of the mandibular 2nd molar: Case report. J. Kor. Acad. Endod. 2012, 13, 41–45.





