
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Stefano Orlando | + 1299 word(s) | 1299 | 2021-03-29 10:41:08 | | | |
| 2 | Lily Guo | Meta information modification | 1299 | 2021-04-02 08:42:17 | | | | |
| 3 | Lily Guo | Meta information modification | 1299 | 2021-04-02 08:42:57 | | | | |
| 4 | Lily Guo | Meta information modification | 1299 | 2021-04-02 08:44:33 | | |
Video Upload Options
Eighty percent of people with stroke live in low- to middle-income nations, particularly in sub-Saharan Africa (SSA) where stroke has increased by more than 100% in the last decades. More than one-third of all epilepsy−related deaths occur in SSA. HIV infection is a risk factor for neurological disorders, including stroke and epilepsy. The vast majority of the 38 million people living with HIV/AIDS are in SSA, and the burden of neurological disorders in SSA parallels that of HIV/AIDS.
1. The Epidemiologic Transition Is Changing the Health Scenario in Sub-Saharan Africa
Sub-Saharan Africa (SSA) demography has deeply changed in the last decades. Interactions among environmental determinants also are incriminated in changes of disease burden. The SSA population almost doubled in the last 20 years, from 660 million to 1.1 billion people [1]. Life expectancy is 61 years (80.6 in high income countries—HIC, as in Europe in 1950 [2][3]), 10 years more than in 2000 [2] (Figure 1).
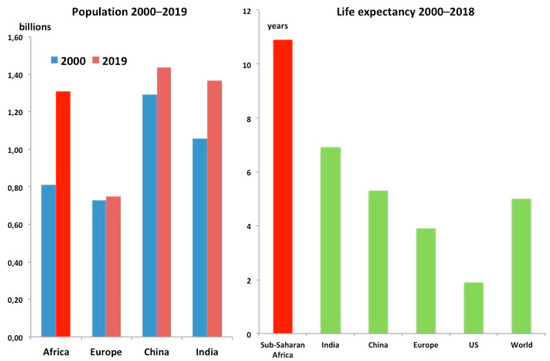
Figure 1. The epidemiologic transition: changes in the global population (left panel) and life expectancy increases from 2000 to 2018 (right panel) (ref. [1][2][3]).
This deep demographic change has increased the burden of noncommunicable diseases (NCDs) that today are responsible for more than 40% of the total disease burden in SSA [4][5]. The rise of stroke and epilepsy is alarming: from 1990 to 2017 disability-adjusted life years (DALYs) increase for stroke was +37.7% and epilepsy 68.8% [4]. Stroke and epilepsy can be largely prevented and treated in SSA and deserve more attention (Figure 2).
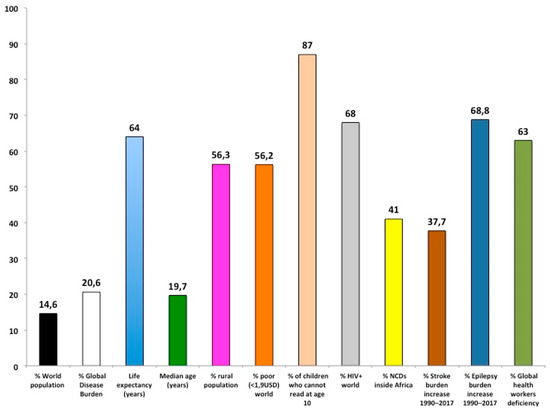
Figure 2. Overview of sub-Saharan Africa condition (see body text for details). NCDs: Noncommunicable diseases.
2. Stroke in Sub-Saharan Africa
Stroke has become the second leading cause of death worldwide and ranks as the biggest (67.3%) contributor to the global burden of neurological disorders [6]. In the last 20 years, stroke greatly increased in low- to middle-income countries (LMIC); 80% of people who have had a stroke live there [7]. Mortality rate (number of deaths per 100,000 general population) for stroke in SSA is up to 5 times higher compared to Western countries—caused by fast demographic and lifestyle changes and other local factors including poor access to primary care [8]. In 2016, the death rate by stroke was 37 deaths per 100,000 inhabitants in SSA, similar to malaria and TB (40 deaths per 100,000 inhabitants) [5]. In 75% of SSA countries, stroke is among the three leading causes of death [8] (Figure 3).
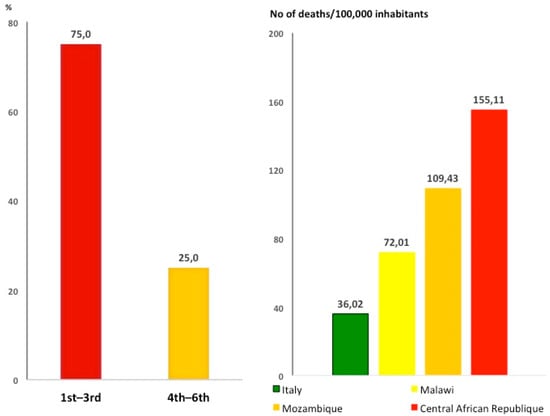
Figure 3. Stroke is a leading cause of death in sub-Saharan Africa. Left panel: stroke ranks as first to third leading cause of death in 75% of sub-Saharan countries (ref. [9]). Right panel: mortality for stroke in Italy compared to sub-Saharan Africa countries.
The main causes of stroke and related risks factors in SSA differ from Western countries [9][10], and modifiable risk factors account for more than 80% of stroke risk in SSA [7]. After hypertension, HIV is the second main risk factor [9], and HIV has been shown to be the main risk factor for stroke in patients below 45 years of age [9]. Compared to Western countries, stroke is more common in young people in SSA [10]. Severity, mortality, and occurrence of stroke are increased by poor socioeconomic conditions, particularly at younger ages [11]; extreme poverty (people living with less than 1.9 USD per day) affects more than 40% of the SSA population [12].
Tobacco use, dyslipidaemia, and atherosclerosis are observed less frequently in SSA stroke patients compared to Europe [7][9].
Although more than 50% of the population is under 20 [13], hypertension affects between 16% and 40% (median 31%) of the adult SSA population; most of them are not aware of their condition [14][15]. The same applies to diabetic patients (8% of general population) [15]. In general, more than half of the SSA population live in rural areas with poor access to health care, so that most hypertension and diabetes—major contributors to stroke—remain undisclosed and poorly treated and controlled [15].
3. Epilepsy in Sub-Saharan Africa
Epilepsy is a chronic NCD of the brain, one of the most common neurological diseases [16]: in 2016 there were 45.9 million patients with active epilepsy worldwide [17]. Eighty percent of epileptic patients live in poor countries, from 5 to 12 million in SSA [17][18][19]. In many regions of SSA, idiopathic epilepsy represents the second most frequent neurological disorder [6][17]. The risk of premature death among people with epilepsy is 3 times higher than in the general population and even higher in SSA [20]. More than one- third of all epilepsy-related deaths occur in SSA [19]. In a global burden of disease review, epilepsy was between the 16th and 25th leading cause of death in SSA, while in HIC it was ranked between 43 and 63 [21].
The treatment gap (people with epilepsy not getting the treatment they need) exceeds 70% in most of the SSA countries [16][18], and up to 70% of these epileptic patients could live seizure-free if properly diagnosed and treated [16].
Low adherence to antiepileptic drugs (AEDs) [22] is among the causes favouring convulsive status epilepticus [23], particularly in HIV and malaria patients, which in turn increases the risk of brain damage and death [24]. Interventions to improve medication adherence in epilepsy are very limited in SSA [25]. A short course health education programme did not improve adherence in SSA, suggesting the need for long-term interventions [26].
A shortage of antiepileptic medicines in public health centres is a challenge in SSA, and in some cases lack of drugs may undermine the effectiveness of the same. Many people think epilepsy is the result of witchcraft, which leads parents of children with epilepsy to seek the services of traditional healers [16]. Those children cannot go to school because of stigma, so that the illness brings the hard consequences of stigma as illiteracy, restriction in social contacts, marriage, work, etc. [23]. Patients and their families very often suffer from stigma and discrimination too. Resources to treat an epileptic patient in Western countries and SSA differ considerably: 2051–11,354 USD [27] and <2 USD [28], respectively. The disparity underlines the need for more investments to treat epilepsy in SSA.
4. The Double Burden of HIV and Neurologic Disorders in Sub-Saharan Africa
The double burden of HIV and stroke and epilepsy challenges patients, health care services, and governments in SSA. It has been shown that HIV infection is a risk factor for stroke [9] and epilepsy [29] even when viral load is undetectable. Small amounts of virus remain in the nervous system of HIV patients permanently to interfere to various extents with normal functioning of neurons, glial cells, and vessels, thus predisposing millions of HIV patients to neurologic disorders [30]. The lasting HIV pandemic will further increase the burden of stroke and epilepsy in SSA. In fact, the total number of people living with HIV (PLWH) continues to increase as the result of longer life expectancy due to more effective antiretroviral treatment regimens and the decreased occurrence of new infections [31][32]. New HIV infections decreased from 1.9 in 2015 to 1.7 million in 2019, about a 2%/year reduction rate [33]. At this rate, in 2050 new infections will still be about 1 million/year. On the other hand, the number of PLWH continued to increase from 30.7 in 2010 to 38 million in 2019, even faster than what has been observed from 2000 (24 million) to 2010: 7.3 million increase from 2010 to 2019 and 6.7 million from 2000 to 2010) [33] (Figure 4). In 2019, there were 26 million PLWH in SSA (68% of the total) [31].
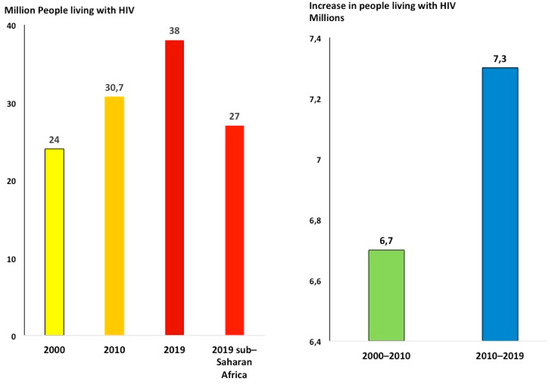
Figure 4. People living with HIV continue to increase (ref. [34]). More than two-thirds of people living with HIV across the world are in sub-Saharan Africa.
To reduce the number of PLWH, renewed efforts are needed to prevent new infections. The most effective HIV prevention is antiretroviral treatment (ART) [34]; bringing ART to all patients living with HIV in SSA patients in the period 2018–2050 will cost about 373 billion USD [35]. SSA governments and development assistance for health (DAH), the two major sources covering health expenditure in SSA, could provide a total of 248.6 billion USD in that period (according to the yearly change observed in the last five years in HIV expenditure of SSA governments plus DAH, +3.3% and −1.9%, respectively—reference period 2010–2017) [36] so that 124.4 billion USD will be lacking. In addition, to effectively reduce new infections, the major share of the resources will be needed in the next few years [35].
Integrated prevention programmes in primary care settings have the potential to greatly improve the condition in SSA.
References
- Population Pyramids of the World from 1950 to 2100. Available online: (accessed on 12 January 2021).
- Worldbank Indicators. Available online: (accessed on 12 January 2021).
- Life Expectancy. Available online: (accessed on 12 January 2021).
- Gouda, H.N.; Charlson, F.; Sorsdahl, K.; Ahmadzada, S.; Ferrari, A.J.; Erskine, H.; Leung, J.; Santamauro, D.; Lund, C.; Aminde, L.N.; et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: Results from the Global Burden of Disease Study Lancet Glob. Health 2019, 7, e1375–e1387.
- Causes of Death. Available online: (accessed on 12 January 2021).
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study. Lancet 2017, 388, 1990–2015.
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123.
- Country Health Profiles. Available online: (accessed on 12 January 2021).
- Benjamin, L.A.; Corbett, E.L.; Connor, M.D.; Mzinganjira, H.; Kampondeni, S.; Choko, A.T.; Hopkins, M.; Emsley, H.C.A.; Bryer, A.; Faragher, B.; et al. HIV, antiretroviral treatment, hypertension, and stroke in Malawian adults. Neurology 2016, 86, 324–333.
- Owolabi, M.O.; Ugoya, S.; Platz, T. Racial disparity in stroke risk factors: The Berlin-Ibadan experience; a retrospective study. Acta Neurol. Scand. 2009, 119, 81–87.
- Aslanyan, S.; Weir, C.J.; Lees, K.R.; Reid, J.L.; McInnes, G.T. Effect of Area-Based Deprivation on the Severity, Subtype, and Outcome of Ischemic Stroke. Stroke 2003, 34, 2623–2628.
- 85% of Africans Live on Less Than $5.50 Per Day. Available online: (accessed on 12 January 2021).
- Africa Population. Available online: (accessed on 12 January 2021).
- Ataklte, F.; Erqou, S.; Kaptoge, S.; Taye, B.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Burden of Undiagnosed Hypertension in Sub-Saharan Africa. Hypertens. 2015, 65, 291–298.
- Report on the Status of Major Health Risk Factors for Noncommunicable Diseases: WHO African Region. 2015. Available online: (accessed on 12 January 2021).
- Epilepsy: A Public Health Imperative. Available online: (accessed on 12 January 2021).
- Beghi, E.; Giussani, G.; Nichols, E.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; Abraha, H.N.; Adib, M.G.; Agrawal, S.; Alahdab, F.; et al. Global, regional, and national burden of epilepsy, 1990–2016: A systematic analysis for the Global Burden of Disease Study. Lancet Neurol. 2019, 18, 357–375.
- Chin, J.H. Epilepsy treatment in sub-Saharan Africa: Closing the gap. Afr. Health Sci. 2012, 12, 186–192.
- Epilepsy and WHO. Available online: (accessed on 12 January 2021).
- Diop, A.G.; Hesdorffer, D.C.; Logroscino, G.; Hauser, W.A. Epilepsy and Mortality in Africa: A Review of the Literature. Epilepsia 2005, 46, 33–35.
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study. Lancet 2012, 380, 2095–2128.
- Wagner, R.G.; Kabudula, C.W.; Forsgren, L.; Ibinda, F.; Lindholm, L.; Kahn, K.; Tollman, S.; Newton, C.R. Epilepsy care cascade, treatment gap and its determinants in rural South Africa. Seizure 2020, 80, 175–180.
- Faught, E.; Duh, M.S.; Weiner, J.R.; Guerin, A.; Cunnington, M.C. Nonadherence to antiepileptic drugs and increased mortality: Findings from the RANSOM Study. Neurology 2008, 71, 1572–1578.
- Kariuki, S.M.; Kakooza-Mwesige, A.; Wagner, R.G.; Chengo, E.; White, S.; Kamuyu, G.; Ngugi, A.K.; Sander, J.W.; Neville, B.G.; Newton, C.R.; et al. Prevalence and factors associated with convulsive status epilepticus in Africans with epilepsy. Neurology 2015, 84, 1838–1845.
- Al-Aqeel, S.; Gershuni, O.; Al-Sabhan, J.; Hiligsmann, M. Strategies for improving adherence to antiepileptic drug treatment in people with epilepsy. Cochrane Database Syst. Rev. 2020, 10, CD008312.
- Ibinda, F.; Mbuba, C.K.; Kariuki, S.M.; Chengo, E.; Ngugi, A.K.; Odhiambo, R.; Lowe, B.; Fegan, G.; Carter, J.A.; Newton, C.R. Evaluation of K ilifi E pilepsy E ducation P rogramme: A randomized controlled trial. Epilepsia 2014, 55, 344–352.
- Begley, C.E.; Durgin, T.L. The direct cost of epilepsy in the United States: A systematic review of estimates. Epilepsia 2015, 56, 1376–1387.
- Chisholm, D.; Saxena, S. Cost effectiveness of strategies to combat neuropsychiatric conditions in sub-Saharan Africa and South East Asia: Mathematical modelling study. BMJ 2012, 344, e609.
- Mateen, F.J.; Shinohara, R.T.; Carone, M.; Miller, E.N.; McArthur, J.C.; Jacobson, L.P.; Sacktor, N.; Multicenter AIDS Cohort Study (MACS) Investigators. Neurologic disorders incidence in HIV+ vs HIV- men: Multicenter AIDS Cohort Study, 1996–2011. Neurology 2012, 79, 1873–1880.
- Benjamin, L.; Khoo, S. HIV infection and stroke. Handb. Clin. Neurol. 2018, 152, 187–200.
- HIV/AIDS. Available online: (accessed on 12 January 2021).
- Eisinger, R.W.; Folkers, G.K.; Fauci, A.S. Ending the Human Immunodeficiency Virus Pandemic: Optimizing the Prevention and Treatment Toolkits. Clin. Infect. Dis. 2019, 69, 2212–2217.
- Fact Sheet—World Aids Day 2020. Available online: (accessed on 12 January 2021).
- Cohen, M.S.; Chen, Y.Q.; McCauley, M.; Gamble, T.; Hosseinipour, M.C.; Kumarasamy, N.; Hakim, J.G.; Kumwenda, J.; Grinsztejn, B.; Pilotto, J.H.; et al. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N. Engl. J. Med. 2016, 375, 830–839.
- Atun, R.; Chang, A.Y.; Ogbuoji, O.; Silva, S.; Resch, S.; Hontelez, J.; Bärnighausen, T. Long-term financing needs for HIV control in sub-Saharan Africa in 2015–2050: A modelling study. BMJ Open 2016, 6, e009656.
- Health Data. Available online: (accessed on 12 January 2021).





