
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Antonino Maniaci | + 1020 word(s) | 1020 | 2021-03-05 06:39:07 | | | |
| 2 | Lily Guo | + 283 word(s) | 1303 | 2021-03-14 10:45:46 | | |
Video Upload Options
Nasal obstruction is a frequent disorder that interferes with the daily patient’s quality of life. The key element in the pathophysiology of the disorder is the inferior turbinate hypertrophy related to multiple conditions such as allergic rhinitis (AR). Many patients are managed using conventional drug therapies such as antihistamines, decongestants, and intranasal steroid sprays, anticholinergic agents, mast cell stabilizers, and desensitizing vaccines. When traditional therapy failed to relieve AR symptoms, surgical inferior turbinate reduction (ITR) is indicated. A vast variety of surgical techniques have been reported in the literature for AR such as resectioning, coagulating, and laser procedures.
1. Introduction
Nasal obstruction is a common disease that interferes with the daily patient’s quality of life [1].
The key element in the pathophysiology of the disorder is the inferior turbinate hypertrophy related to multiple conditions such as allergic rhinitis (AR), pseudo-allergy, and non-allergic rhinitis eosinophilic, and iatrogenic syndrome [2][3][4].
The inferior turbinates (IT) execute a central function in modulating airflow and nasal resistance through vasodilation and consequent nasal obstruction, congestion, and discomfort [5].
Signs of AR result consequent to an inhaled allergen are characterized by a T helper 2 response and higher serum IgE levels and eosinophilia [6][7].
The interaction between allergens and nasal mucosa is mediated by antigen-presenting cells (dendritic cells, APCs) and naïve T cells [8].
Consequently, the T lymphocytes change into T helper type 2 (Th2) cells and produce interleukin 4 (IL-4), IL-5, and IL-13, promoting the B cell phenotype producing related IgE. Subsequently, IgE bound to the distinct receptors (FcεRI) of mast cells, and basophils cause cell activation; we illustrated Il5-13 pathways between eosinophils and mast cells in Figure 1 [9].
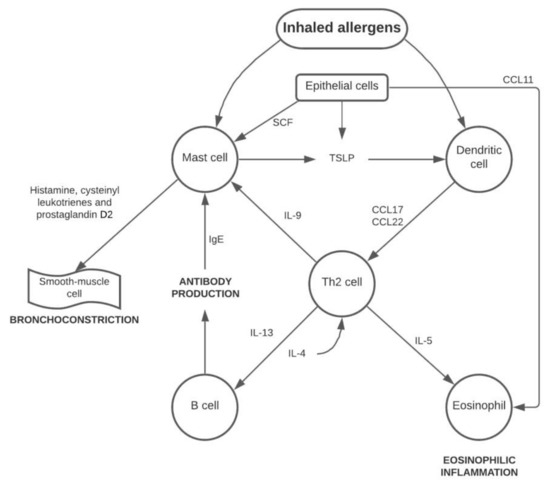
Figure 1. Immunophlogistic cascade of the allergic pathway. Abbreviations: CCL11, C-C motif chemokine 11; CCL17, C-C motif chemokine 17; CCL22, C-C motif chemokine 22; IL-4, Interleukin 4; IL-5, Interleukin 5; IL-9, Interleukin 9; IL-13, Interleukin 13; SCF, stem cell factor; TSLP, Thymic stromal lymphopoietin.
Re-exposure to sensitized allergens leads to cascade disorders and allergic rhinitis (RA) manifestations.
Many patients are treated with the use of conventional drug therapies such as antihistamines, decongestants and intranasal steroid sprays, anticholinergic agents, mast cell stabilizers, and desensitizing vaccines [10].
Although medical treatment is often useful in restoring good nasal breathing, sometimes nasal obstruction becomes disabling, leading inexorably to use and abuse local nasal spray with a consequent high risk of iatrogenic outcomes.
When traditional therapy fails to reduce AR symptoms, inferior turbinate reduction (ITR) is one of the simplest procedures made for the surgical treatment of nasal blocking. A series of techniques concerning reducing turbinates are currently feasible as cryosurgery, electrocautery, laser turbinectomy, partial or total turbinectomy, and Vidian’s neurectomy give different results. Due to direct manipulation of the mucous membrane during surgery, adverse accidents such as bleeding, pain, crusting, smell change, dry nose, and synechia can happen [11][12][13][14].
Eosinophils, mast cells, and other immune cells play a critical role in allergic rhinitis: surgical treatment help prevent eosinophil and immune cell-mediated allergic diseases. Mladina et al. in 78 patients treated with turbinate surgery found improvements in 90% of cases of post-operative cytologic findings both in allergic and non-allergic subjects [15].
Moreover, Cassano et al. stated symptoms’ reduction in 51.4% of allergic rhinitis [16]. In contrast, the authors found improvements in 42.8% with non-allergic rhinitis with eosinophils (NARES) and 64.3% of mast cells with eosinophils (NARESMA).
The primary goals of turbinal surgery, according to the clinical practice guidelines (2015), are based on observational studies, with a preponderance of benefit over damage, evaluating:
The scar tissue that develops inside the submucosal layer leads to damage of both to the vascularization and the glandular structures, preventing their regrowth through fibrosis with the reduction of the amount of specific IgE present on the nasal mucosa and of eosinophils [18].
Mucosa’s preservation that remains perfectly functioning allows, after the ITH procedure, both the maintenance of enough air space to support air’s humidification and purification and the maintenance of airways physiological resistance.
The purpose of the narrative review performed was to list and better clarify the specific characteristics of each surgical technique described in the literature to date in the treatment of AR refractory to medical therapy (Figure 2).
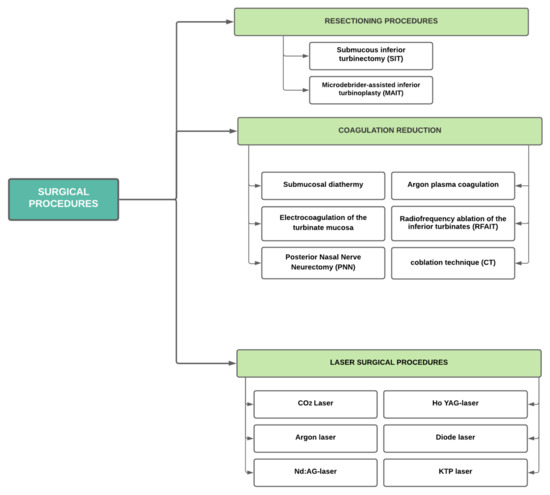
Figure 2. Main surgical techniques currently described in the literature in the surgical treatment of allergic rhinitis. Abbreviations: PNN, posterior nasal nerve neurectomy; APC, Argon plasma coagulation; RFAIT, radiofrequency ablation of the inferior turbinate; CT, coblation technique; Ho:YAG-laser, Holmium:yttrium-aluminium-granat-laser; Nd:YAG-laser, Neodymium: yttrium aluminium garnet laser; KTP laser, Potassium titanyl phosphate laser.
2. Surgical Therapy of the Inferior Turbinate in AR
Techniques for turbinate reduction show that there is no absolute technique that supports long-term success but that the outcome is mainly linked to complications that occur in the short–long term (Table 1) [19].
Table 1. Main studies identified in the literature and principal features described.
| Reference | Year | Study Design | Features (Allergic Patients vs. Control Group) | Follow-Up Time | Objective Evaluation (p-Value) | Subjective Evaluation (p-Value) |
|---|---|---|---|---|---|---|
| Türk | 2018 | Prospective non-randomized | RFA (23 allergic vs. 36 non allergic) | 3, 6 months | Nasal obstruction (<0.001); Acoustic rhinometry (<0.001) | VAS (<0.001) |
| De Corso | 2016 | Prospective | RFA (114 allergic vs. 191 non-allergic) | 1 month, yearly for 5 years | NOSE (<0.05) | |
| Di Rienzo Businco | 2014 | Randomized controlled trial | QMR (145 treated vs. 145 control) | 3 months | Active anterior rhinomanometry (<0.05); Rhinoendoscopy clinic score (<0.05); STT (No statistically different from pretreatment) | SNOT-22 (<0.05); VAS (<0.05) |
| Gunhan | 2011 | Prospective randomized | RFT (28) vs. INS (27) | 12 months | Active anterior rhinomanometry (<0.003) | VAS (<0.05); RQLQ (<0.05) |
| Ravichandran | 2020 | Randomized controlled trial | KTP (105) vs. Diode (104) [allergy not specified] | 1, 2 days, 1, 3 months | STT (Severely prolonged, statistically insignificant. ‘Need more time to follow-up’) | NOSE (<0.001) |
| Gupta | 2018 | Descriptive cross-sectional | Diode (60) | 3 months | VAS (significant) | |
| Vijayakumar | 2016 | Descriptive | KTP (30) | 1 week, 1, 3 months | STT (Return to preoperative value by the end of 3 months) | SNOT (<0.0001) |
| Parida | 2013 | Prospective | Diode (45) [allergy not specified] | 1 week, 1, 3, 6 months | STT (Return to preoperative value by the end of 6 months) | VAS (<0.001) |
| Sroka | 2007 | Retrospective non-randomized comparative | Ho:Yag or Diode (44 allergic vs. 46 non allergic) | 6 months, 3 years | Active anterior rhinomanometry (<0.001) | Subjective questionnaires (85% improvement) |
| Lee | 2013 | Prospective | MAIT (60) | 3, 6, 12 months | Acustic rhinometry (<0.05) | VAS (<0.05) |
| Chen | 2008 | Prospective | MAITL (80) vs. SR (80) | 1, 2, 3 years | Active anterior rhinomanometry (<0.05); STT (<0.05) | VAS (<0.05) |
| Liu | 2009 | Prospective | MAIT (60) vs. RAIT (60) | 6 months, 1, 2, 3 years | Active anterior rhinomanometry (<0.05); STT (<0.05) | VAS (<0.05) |
| Huang | 2006 | Prospective | MAIT (50) | 1 year | Active anterior rhinomanometry (<0.001) | RQLQ (<0.005) |
| Nagalingeswaran | 2020 | Retrospective | PNN Selective Resection (212) | 2 weeks, 1, 2, 6, 12 months | ND | SNOT-22 (<0.001) |
| Krespi | 2018 | Prospective | Diode Laser PNN (32) | 1, 3 months | ND | TNSS (<0.001) |
| Lai | 2017 | Retrospective | Diode laser-assisted VN (43) vs. Cold instrument (75) | 6 months | ND | VAS (<0.001) |
| Tan | 2012 | Prospective | Bilateral VN (93) vs. Partial inferior turbinectomy and/or septoplasty (51) vs. Control group (92) | 6 months, 1, 3 years | ND | VAS (<0.05); RQLQ (<0.05) |
Based on these criteria, turbinate reduction studies only meet the terms of evidence levels 3 and 4: only two studies have yet reached evidence level 2 where long-term follow-ups of 6 and 5 years were conducted, respectively [10][20].
Each technique is judged on two basic criteria:
-
how effective the method was in decreasing hypersecretion from respiratory obstruction, headaches, and sneezing episodes;
-
side outcomes occurring in the short and long term.
It would be a mistake to concentrate entirely on expanding the nasal passages in endoscopic findings, rhinomanometry, and acoustic rhinometry.
A wider nasal cavity does not necessarily mean the nose works better: It is now known that total turbinectomy is nearly out-of-date and radical resection of the inferior turbinate can cause atrophic rhinitis, chronic osteitis, or paradoxical nasal obstruction. The following complication is the hallmark of empty nose syndrome (ENS).
In order to systematize the different surgical techniques, it is possible to outline a subdivision of techniques into three surgical groups: lateralization or lateropexy (it is named only for the sake of completeness), resection, and coagulation procedures.
References
- Juniper, E.F. Impact of upper respiratory allergic diseases on quality of life. J. Allergy Clin. Immunol. 1998, 101, S386–S391.
- Lippert, B.M.; Werner, J.A. Nd: YAG-laserlichtinduzierte Nasenmuschelreduktion. Laryngorhinootologie 1996, 75, 523–528.
- Ottaviani, F.; Capaccio, P.; Cesana, B.M.; Manzo, R.; Peri, A. Argon plasma coagulation in the treatment of non-allergic hy-pertrophic inferior nasal turbinates. Am. J. Otolaryngol. 2003, 24, 306–310.
- Cocuzza, S.; Maniaci, A.; Di Luca, M.; La Mantia, I.; Grillo, C.; Spinato, G.; Motta, G.; Testa, D.; Ferlito, S. Long-term results of nasal surgery: Comparison of mini-invasive turbinoplasty. J. Biol. Regul. Homeost. Agents 2020, 34, 1203–1208.
- Goyal, P.; Hwang, P. Surgery of the septum and turbinates. In Rhinology: Diseases of the Nose, Sinuses, and Skull Base; Kennedy, D.P.H., Ed.; Thieme: New York, NY, USA, 2012.
- Hansen, I.; Klimek, L.; Mösges, R.; Hörmann, K. Mediators of inflammation in the early and the late phase of allergic rhinitis. Curr. Opin. Allergy Clin. Immunol. 2004, 4, 159–163.
- Dullaers, M.; De Bruyne, R.; Ramadani, F.; Gould, H.J.; Gevaert, P.; Lambrecht, B.N. The who, where, and when of IgE in allergic airway disease. J. Allergy Clin. Immunol. 2012, 129, 635–645.
- Nurieva, R.I.; Liu, X.; Dong, C. Yin-Yang of costimulation: Crucial controls of immune tolerance and function. Immunol. Rev. 2009, 229, 88–100.
- Mori, S.; Fujieda, S.; Igarashi, M.; Fan, G.K.; Saito, H. Submucous turbinectomy decreases not only nasal stiffness but also sneezing and rhinorrhea in patients with perennial allergic rhinitis. Clin. Exp. Allergy 1999, 29, 1542–1548.
- Passàli, D.; Anselmi, M.; Lauriello, M.; Bellussi, L. Treatment of Hypertrophy of the Inferior Turbinate: Long-Term Results in 382 Patients Randomly Assigned to Therapy. Ann. Otol. Rhinol. Laryngol. 1999, 108, 569–575.
- Serrano, E.; Percodani, J.; Yardeni, E.; Lombard, L.; Laffitte, F.; Pessey, J.J. The holmium:YAG laser for treatment of inferior turbinate hypertrophy. Rhinol. J. 1998, 36, 77–80.
- Elwany, S.; Abel Salaam, S. Laser surgery for allergic rhinitis: The effect on seromucinous glands. Otolaryngol Head Neck Surg. 1999, 120, 742–744.
- Seidman, M.D.; Gurgel, R.K.; Lin, S.Y.; Schwartz, S.R.; Baroody, F.M.; Bonner, J.R.; Dawson, D.E.; Dykewicz, M.S.; Hackell, J.M.; Han, J.K.; et al. Clinical practice guideline: Allergic rhinitis. Otolaryngol. Head Neck Surg. 2015, 152, S1–S43.
- Lin, H.-C.; Lin, P.-W.; Friedman, M.; Chang, H.-W.; Su, Y.-Y.; Chen, Y.-J.; Pulver, T.M. Long-term Results of Radiofrequency Turbinoplasty for Allergic Rhinitis Refractory to Medical Therapy. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 892.
- Mladina, R.; Risavi, R.; Subaric, M. CO2 laser anterior turbinectomy in the treatment of non-allergic vasomotor rhinopathia. A prospective study upon 78 patients. Rhinol. J. 1991, 29, 267–271.
- Cassano, M.; Del Giudice, A.M.; Russo, G.; Russo, L.; Ciprandi, G. The Role of Nasal Cytology in the Management of Inferior Turbinate Hypertrophy. Int. J. Immunopathol. Pharmacol. 2013, 26, 207–215.
- Passàli, D.; Passàli, F.M.; Passàli, G.C.; Damiani, V.; Bellussi, L. Treatment of Inferior Turbinate Hypertrophy: A Randomized Clinical Trial. Ann. Otol. Rhinol. Laryngol. 2003, 112, 683–688.
- Wise, S.K.; Lin, S.Y.; Toskala, E.; Orlandi, R.R.; Akdis, C.A.; Alt, J.A.; Azar, A.; Baroody, F.M.; Bachert, C.; Canonica, G.W.; et al. International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis. Int. Forum Allergy Rhinol. 2018, 8, 108–352.
- Mol, M.K.; Huizing, E.H. Treatment of inferior turbinate pathology: A review and critical evaluation of the different techniques. Rhinology 2000, 38, 157–166.
- Joniau, S.; Wong, I.; Rajapaksa, S.; Carney, S.A.; Wormald, P.-J. Long-Term Comparison Between Submucosal Cauterization and Powered Reduction of the Inferior Turbinates. Laryngoscope 2006, 116, 1612–1616.




