
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | FUMIHIKO Matsumoto | + 894 word(s) | 894 | 2021-02-24 05:23:37 | | | |
| 2 | Vicky Zhou | Meta information modification | 894 | 2021-03-02 07:21:04 | | |
Video Upload Options
Well-differentiated thyroid carcinoma (WDTC) is a slow-growing cancer with a good prognosis, but may show extraglandular progression involving the invasion of tumor-adjacent tissues, such as the trachea, esophagus, and recurrent laryngeal nerve. Tracheal invasion by WDTC is infrequent. Since this condition is rare, relevant high-level evidence about it is lacking. Tracheal invasion by a WDTC has a negative impact on survival, with intraluminal tumor development constituting a worse prognostic factor than superficial tracheal invasion. In WDTC, curative resection is often feasible with a small safety margin, and complete resection can ensure a good prognosis. Despite its resectability, accurate knowledge of the tracheal and peritracheal anatomy and proper selection of surgical techniques are essential for complete resection. However, there is no standard guideline on surgical indications and the recommended procedure in trachea-invading WDTC. This review discusses the indications for radical resection and the three currently available major resection methods: shaving, window resection, and sleeve resection with end-to-end anastomosis.
1. Introduction
Well-differentiated thyroid carcinoma (WDTC) is a slow-growing cancer that has a good prognosis. The trachea has posterior anatomical proximity to the thyroid gland and is affected by extraglandular extension of thyroid cancer. Tracheal invasion by WDTC is infrequent, exemplified by a rate of 3.4–13% [1][2][3][4][5]. Since this condition is rare, relevant high-level evidence about it is lacking. In tracheal invasion by thyroid cancer, the symptoms range from none to fatal, such as airway obstruction and bleeding. McCarty et al. [6] reported that 22% of 40 patients with obvious tracheal invasion had hoarseness, 11% had hemoptysis, and 5% had respiratory distress. In general, tracheal tumor invasion indicates higher biological tumor aggressiveness compared to tumors limited to the thyroid gland [7]. McCaffrey et al. [8] and Ito et al. [9] found that invasion of the aerodigestive tract was an important negative prognostic factor. Thus, data indicate that tracheal invasion decreases long-term survival; intraluminal tumor development constitutes a worse prognostic factor than superficial tracheal invasion [10][11]. However, in WDTC, even with tracheal invasion, curative resection is often possible with a large margin of safety, and complete resection can ensure a good prognosis. Despite tracheal invasion, WDTC has an excellent prognosis, with more than 90% of patients surviving to 10 years after complete resection [12][13][14]. A far advanced or rapidly progressing tumor may be unresectable, and only tracheostomy or stenting can be undertaken. Even in resectable WDTC, accurate knowledge of the anatomy of the trachea and its adjacent tissues, as well as the proper selection of surgical techniques, is necessary for complete resection. Current guidelines do not provide specific guidance on the resection of tracheal invasion by WDTC. The 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer indicated that the decision for surgical treatment should be based on the feasibility of complete resection and the resultant functional impairment following resection; however, the surgical indications and the recommended procedure in trachea-invasive WDTC were not specified [15].
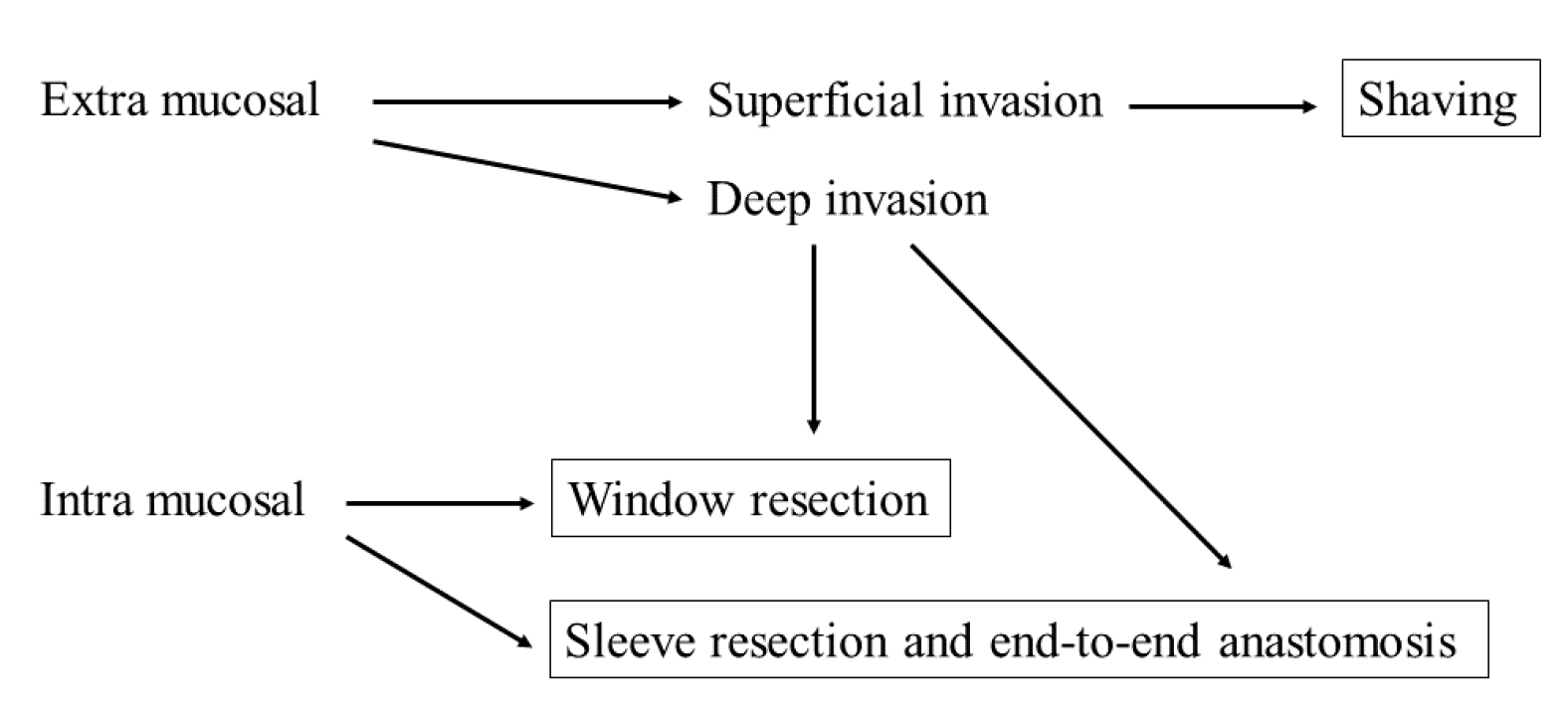
On a case-by-case basis, the possibility of resection, expected postoperative functional disability, and patient’s background (e.g., general condition and expected prognosis) should be considered before deciding on surgical intervention. This review discusses the indications for radical resection and the three major resection methods currently available: shaving, window resection, and sleeve resection with end-to-end anastomosis (Table 1).
Table 1. Features of the surgical method.
| Techniques | Advantage | Disadvantage |
|---|---|---|
| Shaving | Maintaining the tracheal lumen Low morbidity |
Risk of local recurrence |
| Window resection | Microscopic resection Postoperative maintenance of airway |
The need for multiple surgeries |
| Sleeve resection with end-to-end anastomosis | More radical resection Lumen is covered with tracheal mucosa |
Risk of fatal complications |
2. Surgical Management of Tracheal Invasion by Well-Differentiated Thyroid Cancer
There is a general consensus that the order of curability of radical surgical treatment for tracheal invasion is sleeve > window > shaving resection. However, shaving is the least invasive surgery. In the case of superficial invasion of the trachea up to the perichondrium or cartilage, there is consensus that shaving is generally sufficient if the preoperative evaluation is accurate, although it is sometimes difficult to determine the degree of invasion. In a much deeper invasion, many reports indicate that shaving may increase the risk of local recurrence because of microscopic tumor remnants; therefore, shaving may not be sufficient. Moreover, there is consensus that a full-laminar resection is necessary if the disease extends into the lumen or tracheal mucosa. In such cases, there are two possible resection methods: window resection and circumferential resection. Notably, the perioperative risk of sleeve resection is higher than that of window resection, and window resection is not less invasive due to the need for another surgery to close the tracheocutaneous fistula and the possibility of stenosis. However, apart from these complications, window resection is relatively safe, which is a great advantage. Nonetheless, the evidence is inconclusive and requires prospective review. The decision will be based on the patient’s general condition, tumor status, expected duration of prognosis, and the facility’s strengths and weaknesses (Figure 1). In cases of advanced disease or poor patient condition that makes radical resection intolerable, a less invasive approach should be provided. For this reason, accurate preoperative workup is necessary for choosing the suitable surgical procedure for patients with suspected tracheal invasion. CT, US, and bronchoscopy are essential tests for preoperative evaluation. In addition, MRI and EBUS should be considered depending on the situation (Figure 1).
References
- Sciuto, R.; Romano, L.; Rea, S.; Marandino, F.; Sperduti, I.; Maini, C.L. Natural history and clinical outcome of differentiated thyroid carcinoma: A retrospective analysis of 1503 patients treated at a single institution. Ann. Oncol. 2009, 20, 1728–1735.
- Hundahl, S.A.; Cady, B.; Cunningham, M.P.; Mazzaferri, E.; McKee, R.F.; Rosai, J.; Shah, J.P.; Fremgen, A.M.; Stewart, A.K.; Holzer, S. Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the United States during 1996: An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer 2000, 89, 202–217.
- Youngwirth, L.M.; Adam, M.A.; Scheri, R.P.; Roman, S.A.; Sosa, J.A. Extrathyroidal extension is associated with compromised survival in patients with thyroid cancer. Thyroid 2017, 27, 626–631.
- Andersen, P.E.; Kinsella, J.; Loree, T.R.; Shaha, A.R.; Shah, J.P. Differentiated carcinoma of the thyroid with extrathyroidal extension. Am. J. Surg 1995, 170, 467–470.
- Kim, H.; Jung, H.J.; Lee, S.Y.; Kwon, T.K.; Kim, K.H.; Sung, M.W.; Hun Hah, J. Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur. Arch. Oto Rhino Laryngol. 2016, 273, 1919–1926.
- McCarty, T.M.; Kuhn, J.A.; Williams, W.L., Jr.; Ellenhorn, J.D.; O’Brien, J.C.; Preskitt, J.T.; Lieberman, Z.H.; Stephens, J.; Odom-Maryon, T.; Clarke, K.G.; et al. Surgical management of thyroid cancer invading the airway. Ann. Surg. Oncol. 1997, 4, 403–408.
- Chernichenko, N.; Shaha, A.R. Role of tracheal resection in thyroid cancer. Curr. Opin. Oncol. 2012, 24, 29–34.
- McCaffrey, J.C. Aerodigestive tract invasion by well-differentiated thyroid carcinoma: Diagnosis, management, prognosis, and biology. Laryngoscope 2006, 116, 1–11.
- Ito, Y.; Tomoda, C.; Uruno, T.; Takamura, Y.; Miya, A.; Kobayashi, K.; Matsuzuka, F.; Kuma, K.; Miyauchi, A. Prognostic significance of extrathyroid extension of papillary thyroid carcinoma: Massive but not minimal extension affects the relapse-free survival. World J. Surg. 2006, 30, 780–786.
- Hotomi, M.; Sugitani, I.; Toda, K.; Kawabata, K.; Fujimoto, Y. A novel definition of extrathyroidal invasion for patients with papillary thyroid carcinoma for predicting prognosis. World J. Surg. 2012, 36, 1231–1240.
- Wada, N.; Nakayama, H.; Masudo, Y.; Suganuma, N.; Rino, Y. Clinical outcome of different modes of resection in papillary thyroid carcinomas with laryngotracheal invasion. Langenbecks Arch. Surg. 2006, 391, 545–549.
- Hay, I.D.; McConahey, W.M.; Goellner, J.R. Managing patients with papillary thyroid carcinoma: Insights gained from the Mayo Clinic’s experience of treating 2,512 consecutive patients during 1940 through 2000. Trans. Am. Clin. Climatol. Assoc. 2002, 113, 241–260.
- Ishihara, T.; Yamazaki, S.; Kobayashi, K.; Inoue, H.; Fukai, S.; Ito, K.; Mimura, T. Resection of the trachea infiltrated by thyroid carcinoma. Ann. Surg. 1982, 195, 496–500.
- Brennan, M.D.; Bergstralh, E.J.; van Heerden, J.A.; McConahey, W.M. Follicular thyroid cancer treated at the Mayo Clinic, 1946 through 1970: Initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin. Proc. 1991, 66, 11–22.
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133.




