
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Felipe De la Fuente | + 1823 word(s) | 1823 | 2021-01-07 07:52:38 | | | |
| 2 | Vicky Zhou | Meta information modification | 1823 | 2021-01-27 03:50:47 | | |
Video Upload Options
Type 2 diabetes mellitus (T2DM) is a public health challenge that must be addressed considering the large number of risk factors involved in its appearance. Some environmental risk factors are currently described as predictors of diabetes, with access to green spaces being an element to consider in urban settings.
1. Introduction
Type 2 diabetes mellitus (T2DM) is a complex metabolic disease characterized by continuous hyperglycemia in the absence of treatment. T2DM is the most common type of diabetes, affecting around 90% of diabetics, including beta-cell dysfunction and insulin resistance [1][2].
According to the International Diabetes Federation, the global prevalence of T2DM in 2019 was 9.3, 95% confidence interval (CI) (7.4–12.1), and it is projected to increase to 10.9%, 95% CI (8.4–14.1) by 2045, affecting 700.2 million people worldwide. This prevalence is projected to be higher in countries where economies move from low-to middle-income, revealing the social complexities that need to be taken into account when studying this disease [1]. T2DM represents a huge economic burden on health systems around the world, which can be measured by direct medical expenses, indirect expenses due to productivity losses, premature deaths, and deleterious effects of diabetes on the countries’ gross domestic product [1].
In 2015, the global spending on this health condition reached 1.33 trillion dollars, and by 2030 it is projected that total spending related to T2DM will reach 8.39 trillion dollars [3]. As a result of the urbanization process, 310.3 million people with T2DM live in urban areas, representing a prevalence of 10.8%, while in rural areas the prevalence reaches 7.2% [1]. This phenomenon is more evident in low- and middle-income countries [1][4].
Some risk factors have been associated with the onset of diabetes, such as overweight, obesity, and physical inactivity [5]. Other factors associated with T2DM prevalence are ethnicity, gender, socioeconomic status, age, malnutrition, glucose intolerance, and hypertension [5][6].
Structural and social determinants of health outcomes, such as income and social position, education level, working conditions, health services access, and physical environment, generate different conditions and exposures that have a clear impact on non-communicable chronic diseases such as a T2DM; and their recognition allows healthcare workers and stakeholders to perform in multidisciplinary spaces to design and implement public policies and health interventions in those conditions that can be modified [7][8][9][10], highlighting the importance of implementing prevention and health-promotion strategies at an early age.
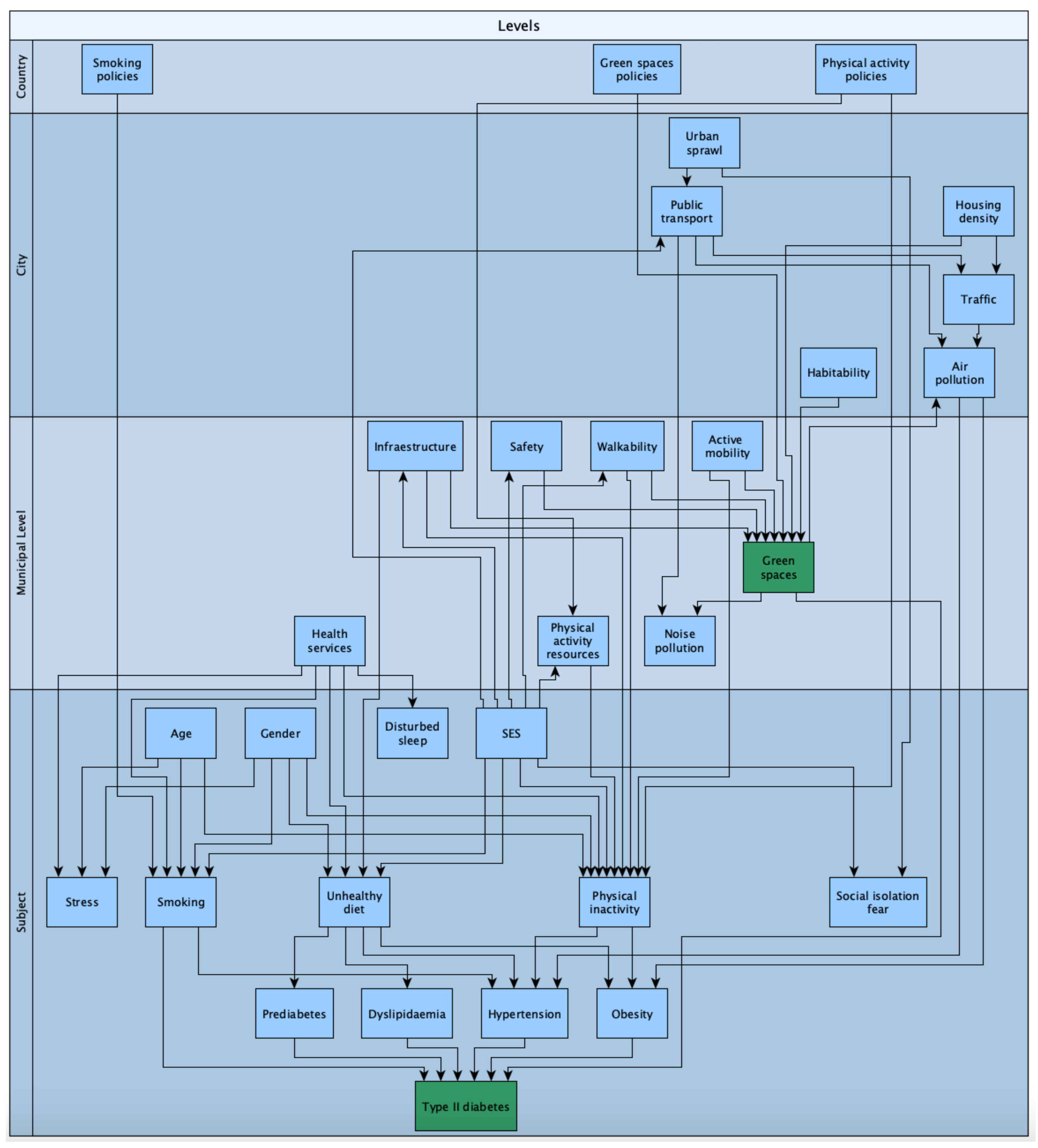
Figure 1 describes the multilevel dependency of this phenomenon, considering the individual factors, neighborhood, municipal level, city, and country variables. This theoretical scheme has been proposed by the authors to explain the relationships of environmental, demographic, and health variables that can explain the unequal distribution of T2DM and give a theoretical base to the present entry.
Other risk factors have emerged to explain the socioeconomic gradients in the T2DM prevalence. Because of this, preventive measures emerge from the result of multisectoral work to reduce the prevalence of diabetes risk factor, in particular, the ones that can be modified—such as overweight, obesity, lack of physical activity, and an unhealthy diet—through a combination of fiscal policies, laws, regulation of marketing strategies, environmental policies, and urban changes; with emphasis on social and environmental determinants with a multisectoral, promotional, and preventive approach [11][12][13].
The major determinants of T2DM are socioeconomic factors that influence urban exposure. In this regard, the link between T2DM prevention and urbanization processes needs to be understood as an environmental health factor [4][8][13][14].According to a meta-analysis that studied the influence of the built environment in urban areas on T2DM, living in an urban area was associated with higher T2DM risk: odds ratio (OR) = 1.40, 95% CI (1.2–1.6), compared to living in rural areas. Moreover, the study highlighted that environmental characteristics such as neighborhood green spaces were associated with lower rates of T2DM [13]. In addition, exposure to green spaces have been associated with higher levels of physical activity, better physical and mental health, and lower stress, making it possible to achieve higher social capital [15][16]. In particular, green spaces have been studied and proposed as health determinants, because their distribution differs across populations and impacts the health status and wellbeing of the population [17][18][19].
In the urban context, green spaces can be defined as open spaces with natural elements such as parks, playgrounds, and recreation areas, both public and private, which can be used by the population for individual and social activities. These areas are known as urban land covered by vegetation [17][18]. It is well known that the urbanization process reduces time spent in contact with nature, but in the urban context, green spaces, forests, fields, street trees, and urban parks can play a protective role in the development of non-communicable diseases [19]. In this sense, the possible theoretical pathways of green space exposure and improvements on health are based on mitigation of air and noise pollution, because greenspaces are not sites of pollutant emission and also provide an acoustic barrier while reducing heat island effects, i.e., urban areas with more buildings than natural landscapes and have higher temperatures than outlying areas. Green spaces also reduce stress, increases positive emotions, and allow recovery from fatigue, thereby increase physical activity levels, and also provide a place for social contact [17][18][19][20].
Although this is not about pandemics, we cannot disentangle ourselves from the potential impacts of green space exposure and urban policy modifications that must be discussed in light of the COVID-19 pandemic. In the COVID-19 pandemic context, diabetes and other non-communicable diseases have been confirmed to make people more vulnerable to getting a confirmed SARS-CoV-2 test and to dying because of complications of this virus [21][22]. Particularly, T2DM was associated with a higher incidence of COVID-19 relative risk (RR) = 2.38, CI (1.88–3.03) and mortality RR = 2.12, CI (1.44–3.11) [22]. Furthermore, T2DM and COVID-19 are called “socially transmitted diseases,” and it is well accepted that these conditions are driven by environmental factors, such as urban green spaces [21]. In addition, it is important to promote the maintenance of green spaces and accessible urban parks during COVID-19 (and any other pandemic) because it is beneficial for both physical and mental health, taking into account health recommendations to prevent transmission of COVID-19 [23].
In this regard, it is possible to infer that some of the modifiable structural conditions relevant in this context are urban planning policies that can be directed to allow everyone to live in healthier environments and have access to green spaces close to home. Unfortunately, access to green spaces and urban parks is not evenly distributed and reflects deep social inequalities in urban areas [24][25][26][27]. This evidence suggests that environmental factors such as green spaces can influence the appearance of T2DM; however, the limitations with regard to the quality and quantity of the studies do not allow us to infer causality [10].
2. Green Space Exposure Association with Type 2 Diabetes Mellitus, Physical Activity, and Obesity
Different definitions of green spaces and greenness measurements were found. Green space exposure had different measurement methods, such as distance to parks, normalized difference vegetation index (NDVI)—used to measure living vegetation by the reflectance levels that the vegetation emits from the photosynthesis process—the density of trees in the neighborhood, park areas per km2, geographic information system, postal code use, and by self-reported questionnaires. There is no consensus yet about which kind of methodology is best for answering this research question [28]. It is important to discuss the methodology spectrum to assess the validity measure of green spaces. Thus, subjective measures such as questionaries and self-reported are usually of lower cost and easier to implement than objective measurements such as direct assessment of green spaces, e.g., NVDI and other georeference methods.
T2DM was measured by medical records, surveys, and blood tests. Secondary outcomes such as physical activity and obesity were included due to the causal pathway between these risk factors regarding T2DM.
The relationship between greenness or greenspaces has been studied in differing contexts. It suggests that green spaces play a key protective role against air pollution, allowing to avoid chronic inflammation processes [29]. The causal pathway to understanding this relationship also includes demographic factors such as age, gender, ethnicity, and socioeconomic status and living context, such as cultural factors, safety and infrastructure, local and regional policy, and rural or urban setting. These factors can moderate the opportunities or barriers to the use of green spaces, which if they are available, promote relaxation activities, encourage physical activity, interaction with nature, and social interactions within greenspaces and participation in group activities [30]. Furthermore, neighborhood characteristics, including green areas, can promote or strengthen the city’s social capital [31]. It results in agreement with other studies that focus on the built environment, including green spaces and health-related outcomes, highlighting the urban context’s role in chronic conditions and signaling the importance of addressing inequalities to allow a more homogeneous distribution of the urban green spaces [10]. Other studies have proposed the effect of the green spaces as promoters of endocrinological effects and highlighted the role of nature in the inflammatory response and chronic conditions [32]. There is also evidence in the same causal direction of this entry, supporting the idea that vegetation in the urban context contributes to improving human health and social well-being, by showing that the majority of people exposed to green spaces had a smaller risk of having T2DM and other risk factors such as obesity and sedentarism [33].
Regarding the available evidence, more primary studies need to be conducted, considering the type of green space exposure and the measurement of main outcomes such as diabetes but also confounders, risk factors, precursors, and effect modifiers, to properly isolate the effect. It would be relevant that these studies include a gender approach since some results showed that there are significant gender differences to be considered. In the same direction, ethnicity and other determinants should be considered when analyzing the results.
Further research needs to be carried out to determine the social and biological links between green spaces and type 2 diabetes mellitus, especially in low- and middle-income countries, to identify potential barriers of use, inequities in distribution, and to encourage stakeholders to generate public policies where urban and health factors are considered to reduce health impacts of chronic conditions such as T2DM.
3. Conclusions
There is significant evidence supporting the protective role of green spaces in the urban context against T2DM and other chronic health conditions such as obesity and sedentarism. People and communities living in neighborhoods with more green spaces and closer to parks with sports facilities had less risk of having T2DM. The exposure to green spaces also reduced the likelihood to be obese and boosted the probability to perform physical activity.
In times of the COVID-19 pandemic, communities’ access is more restricted to proximal green spaces, thus resulting in poor air quality and high rates of respiratory diseases and other health outcomes, making neighborhoods more vulnerable to poorer health outcomes and to being disproportionately harmed by health costs and economic and social aspects of the COVID-19 pandemic that underlie the health conditions of those neighborhoods [34].
References
- International Diabetes Federation. IDF Diabetes Atlas, Ninth Edition. 2019. Available online: https://diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf (accessed on 15 September 2020).
- World Health Organization. International Diabetes Federation Diagnosis and Management of Type 2 Diabetes-(HEARTS-D); World Health Organization: Geneva, Switzerland, 2020.
- Bommer, C.; Sagalova, V.; Heesemann, E.; Manne-Goehler, J.; Atun, R.; Bärnighausen, T.; Davies, J.; Vollmer, S. Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030. Diabetes Care 2018, 41, 963–970.
- Gassasse, Z.; Smith, D.; Finer, S.; Gallo, V. Association between urbanisation and type 2 diabetes: An ecological study. BMJ Glob. Health 2017, 2, e000473.
- Fletcher, B.; Gulanick, M.; Lamendola, C. Risk factors for type 2 diabetes mellitus. J. Cardiovasc. Nurs. 2002, 16, 17–23.
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocr. Rev. 2016, 37, 278–316.
- Clark, M.L.; Utz, S.W. Social determinants of type 2 diabetes and health in the United States. World J. Diabetes 2014, 5, 296–304.
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017, 52, S5–S12.
- Graham, H.; White, P.C.L. Social determinants and lifestyles: Integrating environmental and public health perspectives. Public Health 2016, 141, 270–278.
- Dendup, T.; Feng, X.; Clingan, S.; Astell-Burt, T. Environmental Risk Factors for Developing Type 2 Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 78.
- Scott, A.; Chambers, D.; Goyder, E.; O’Cathain, A. Socioeconomic inequalities in mortality, morbidity and diabetes management for adults with type 1 diabetes: A systematic review. PLoS ONE 2017, 12, e0177210.
- Ramón, C.L.; García, M.I.Á. Diabetes mellitus hacia una perspectiva social. Rev. Cuba. Salud Pública 2013, 39, 331–345.
- Den Braver, N.R.; Lakerveld, J.; Rutters, F.; Schoonmade, L.J.; Brug, J.; Beulens, J.W.J. Built environmental characteristics and diabetes: A systematic review and meta-analysis. BMC Med. 2018, 16, 12.
- Freedman, V.A.; Grafova, I.B.; Rogowski, J. Neighborhoods and Chronic Disease Onset in Later Life. Am. J. Public Health 2011, 101, 79–86.
- Rojas-Rueda, D.; Nieuwenhuijsen, M.J.; Gascon, M.; Perez-Leon, D.; Mudu, P. Green spaces and mortality: A systematic review and meta-analysis of cohort studies. Lancet Planet. Health 2019, 3, e469–e477.
- Jennings, V.; Bamkole, O. The Relationship between Social Cohesion and Urban Green Space: An Avenue for Health Promotion. Int. J. Environ. Res. Public Health 2019, 16, 452.
- Swanwick, C.; Dunnett, N.; Woolley, H. Nature, Role and Value of Green Space in Towns and Cities: An Overview. Built Environ. 2003, 29, 94–106.
- World Health Organization. Regional Office for Europe Urban Green Spaces a Brief for Action 2017; World Health Organization: Geneva, Switzerland, 2017.
- Mears, M.; Brindley, P.; Jorgensen, A.; Maheswaran, R. Population-level linkages between urban greenspace and health inequality: The case for using multiple indicators of neighbourhood greenspace. Health Place 2020, 62, 102284.
- Hibbard, K.A.; Hoffman, F.M.; Huntzinger, D.; West, T.O.; Wuebbles, D.J.; Fahey, D.W.; Hibbard, K.A.; Dokken, D.J.; Stewart, B.C.; Maycock, T.K. Ch. 10: Changes in Land Cover and Terrestrial Biogeochemistry. 2017. Available online: https://science2017.globalchange.gov/chapter/10/ (accessed on 20 October 2020).
- Sheldon, T.A.; Wright, J. Twin epidemics of covid-19 and non-communicable disease. BMJ 2020, 369, m2618.
- Huang, I.; Lim, M.A.; Pranata, R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia—A systematic review, meta-analysis, and meta-regression. Diabetes Metab. Syndr. 2020, 14, 395–403.
- Slater, S.J. Recommendations for Keeping Parks and Green Space Accessible for Mental and Physical Health During COVID-19 and Other Pandemics. Prev. Chronic Dis. 2020, 17, E59.
- Braubach, M.; Egorov, A.; Mudu, P.; Wolf, T.; Ward Thompson, C.; Martuzzi, M. Effects of Urban Green Space on Environmental Health, Equity and Resilience. In Nature-Based Solutions to Climate Change Adaptation in Urban Areas: Linkages between Science, Policy and Practice; Kabisch, N., Korn, H., Stadler, J., Bonn, A., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 187–205. ISBN 978-3-319-56091-5.
- Lin, B.; Meyers, J.; Barnett, G. Understanding the potential loss and inequities of green space distribution with urban densification. Urban For. Urban Green. 2015, 14, 952–958.
- De la Barrera, F.; Henriquez, C.; Ruiz, V.; Inostroza, L. Urban Parks and Social Inequalities in the Access to Ecosystem Services in Santiago, Chile. IOP Conf. Ser. Mater. Sci. Eng. 2019, 471, 102042.
- Wüstemann, H.; Kalisch, D.; Kolbe, J. Access to urban green space and environmental inequalities in Germany. Landsc. Urban Plan. 2017, 164, 124–131.
- Dalton, A.M.; Jones, A.P.; Sharp, S.J.; Cooper, A.J.M.; Griffin, S.; Wareham, N.J. Residential neighbourhood greenspace is associated with reduced risk of incident diabetes in older people: A prospective cohort study. BMC Public Health 2016, 16, 1117.
- Groenewegen, P.P.; Zock, J.-P.; Spreeuwenberg, P.; Helbich, M.; Hoek, G.; Ruijsbroek, A.; Strak, M.; Verheij, R.; Volker, B.; Waverijn, G.; et al. Neighbourhood social and physical environment and general practitioner assessed morbidity. Health Place 2018, 49, 68–84.
- Lachowycz, K.; Jones, A.P. Towards a better understanding of the relationship between greenspace and health: Development of a theoretical framework. Landsc. Urban Plan. 2013, 118, 62–69.
- Waverijn, G.; Heijmans, M.; Groenewegen, P.P. Chronic illness self-management: A mechanism behind the relationship between neighbourhood social capital and health? Eur. J. Public Health 2017, 27, 594–599.
- Rook, G.A. Regulation of the immune system by biodiversity from the natural environment: An ecosystem service essential to health. Proc. Natl. Acad. Sci. USA 2013, 110, 18360–18367.
- Vieira, J.; Matos, P.; Mexia, T.; Silva, P.; Lopes, N.; Freitas, C.; Correia, O.; Santos-Reis, M.; Branquinho, C.; Pinho, P. Green spaces are not all the same for the provision of air purification and climate regulation services: The case of urban parks. Environ. Res. 2018, 160, 306–313.
- Liu, L.; Zhong, Y.; Ao, S.; Wu, H. Exploring the Relevance of Green Space and Epidemic Diseases Based on Panel Data in China from 2007 to 2016. Int. J. Environ. Res. Public Health 2019, 16, 2551.




