
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Fabrizio Luppi | + 1212 word(s) | 1212 | 2021-01-11 10:28:49 | | | |
| 2 | Lily Guo | Meta information modification | 1212 | 2021-01-27 14:31:48 | | |
Video Upload Options
In 2015 the European Respiratory Society (ERS) and the American Thoracic Society (ATS) “Task Force on Undifferentiated Forms of Connective Tissue Disease-associated Interstitial Lung Disease” proposed classification criteria for a new research category defined as “Interstitial Pneumonia with Autoimmune Features” (IPAF), to uniformly define patients with interstitial lung disease (ILD) and features of autoimmunity, without a definite connective tissue disease. These classification criteria were based on a variable combination of features obtained from three domains: a clinical domain consisting of extra-thoracic features, a serologic domain with specific autoantibodies, and a morphologic domain with imaging patterns, histopathological findings, or multicompartment involvement. Features suggesting a systemic vasculitis were excluded. Since publication of ERS/ATS IPAF research criteria, various retrospective studies have been published focusing on prevalence; clinical, morphological, and serological features; and prognosis of these patients showing a broad heterogeneity in the results. Recently, two prospective, cohort studies were performed, confirming the existence of some peculiarities for this clinical entity and the possible progression of IPAF to a defined connective tissue disease (CTD) in about 15% of cases. Moreover, a non-specific interstitial pneumonia pattern, an anti-nuclear antibody positivity, and a Raynaud phenomenon were the most common findings. In comparison with idiopathic pulmonary fibrosis (IPF), IPAF patients showed a better performance in pulmonary function tests and less necessity of oxygen delivery. However, at this stage of our knowledge, we believe that further prospective studies, possibly derived from multicenter cohorts and through randomized control trials, to further validate the proposed classification criteria are needed.
1. Introduction
Interstitial lung diseases (ILDs) refer to a broad category of more than 200 lung diseases including a variety of illnesses with diverse causes, treatments, and prognoses. These disorders are grouped together because of similarities in their clinical presentation, plain chest radiographic appearance, and physiologic features leading ultimately—at least in a number of cases—to pulmonary fibrosis. ILDs contain several categories, characterized by different prognoses—including idiopathic interstitial pneumonias (IIPs) and connective tissue disease (CTD)-associated interstitial lung disease (CTD-ILD)[1].
The IIPs are a group of heterogeneous disorders characterized by diffuse parenchymal lung involvement with overlapping clinical and radiologic features[2]. They are generally categorized by histopathologic pattern, and the term chronic fibrosing interstitial pneumonia (IP) has recently been used to encompass the histopathologic patterns of usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP)[1].
CTDs are a group of diseases with heterogeneous systemic features and possible immune-mediated, multi-organ dysfunction. The respiratory tract can be targeted, with different frequencies, in virtually every CTD and with a multitude of manifestations. However, among pulmonary manifestations, ILD is considered the most frequent and serious pulmonary complication, resulting in significant morbidity and mortality [3].
Distinguishing CTD-ILD from an IIP, specifically idiopathic pulmonary fibrosis (IPF), is of paramount importance because CTD-ILD has generally a more favorable prognosis and the available therapeutic options differ significantly [4].
However, in clinical practice, it is common to come across patients with an “idiopathic” interstitial pneumonia (IIP) associated with features suggestive of, but not diagnostic for, a classical CTD [5][6].
On the basis of previous studies, in 2015 the European Respiratory Society (ERS) and the American Thoracic Society (ATS) “Task Force on Undifferentiated Forms of Connective Tissue Disease-associated Interstitial Lung Disease” proposed classification criteria for a new research category defined as “Interstitial Pneumonia with Autoimmune Features” (IPAF). The classification of IPAF can therefore be considered an overlap between an idiopathic interstitial pneumonia and CTD-ILDs[7].
2. Criteria for Interstitial Pneumonia with Autoimmune Features: The European Respiratory Society/American Thoracic Society Research Statement
As discussed above, there is agreement that some patients with an idiopathic ILD may have some features that suggest the presence of a systemic autoimmune process but do not meet classification criteria for a defined CTD[8][9][10]. Therefore, it is common to have discordance among specialists about how to diagnose such patients. A correct identification of patients with CTD-ILD can be challenging if the lung is the predominant or the primary organ involved and clinical evidence of a systemic autoimmune disease is subtle or absent[9].
Moreover, different IIPs may have different prognoses and the available therapeutic options may significantly differ[11][12][13].
In contrast to the adverse effects observed in patients with IPF [14], CTD-ILD could benefit from immunosuppressive treatment, including steroids[15][16]. On the other hand, patients with IPF benefit from antifibrotic agents[17][18], currently under investigation in CTD-ILD patients[19][20]. The lack of consensus over nomenclature and classification criteria limits the ability to perform prospective studies in patients with this particular subset of interstitial pneumonia.
Between 2010 and 2012, different studies proposed different, but partially overlapping, criteria and terms to describe these patients, including “undifferentiated CTD-associated ILD” (UCTD-ILD) [21][22], “lung-dominant CTD” [23] or “autoimmune-featured ILD”[24]. However, each term was capturing different patients and, therefore, none has been universally accepted.
The main limitation of these criteria was their poor applicability and heterogeneity. Studies using one set of criteria were not likely to be applicable to cohorts from different centers using other sets of criteria.
In an effort to systematically compare these four proposed criteria, Assayag and colleagues applied them to a cohort of 119 patients with ILD, showing that only 18% met all four definitions [25]. This study definitely showed that a uniform definition and nomenclature were needed to study these patients apparently affected by IIP but showing an “autoimmune flavor”.
The term “interstitial pneumonia with autoimmune features” (IPAF) was proposed in 2015 by the ERS/ATS “Task Force on Undifferentiated Forms of Connective Tissue Disease-associated Interstitial Lung Disease” to describe individuals with interstitial pneumonia and features suggestive of an underlying systemic autoimmune condition who do not meet current criteria for a specific CTD [7].
The purpose of the statement was to standardize nomenclature and classification of such patients and to create a more uniform population in order to provide a platform for future research investigations and to elucidate prognostic and therapeutic dilemmas. The statement was not intended to provide criteria for the clinical management of these patients.
Several a priori requirements must be fulfilled for the classification of IPAF: Individuals must have evidence of interstitial pneumonia by high-resolution computed tomography (HRCT) imaging and/or by surgical lung biopsy; known causes for interstitial pneumonia must have been excluded after a thorough clinical evaluation; and patients must not meet criteria for a characterizable CTD. Then, the classification criteria combine features from three primary domains: (1) a clinical domain consisting of specific extra-thoracic signs or symptoms; (2) a serologic domain with specific circulating autoantibodies; (3) a morphologic domain with imaging and/or histopathological patterns and multicompartment involvement.
To be classified as having IPAF, patients must meet all of the a priori requirements and have at least one feature from at least two of the three domains (Table 1).
Table 1. Classification criteria for interstitial pneumonia with autoimmune features.
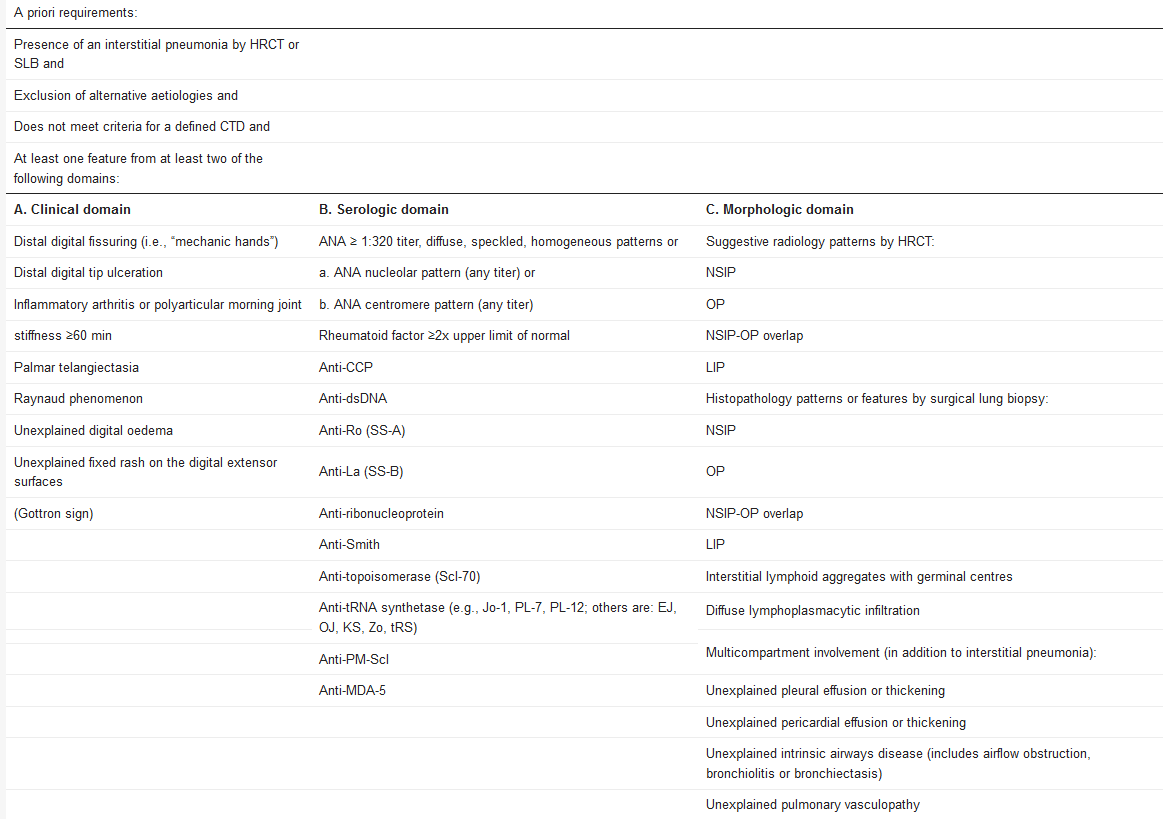
The included features were chosen for their higher specificity for CTDs. The term “connective tissue disease” was specifically avoided due to concerns that such labeling may give a false impression that these individuals have a defined CTD. In contrast, specific features suggesting vasculitis were deliberately excluded.
The Task Force included an international, multidisciplinary panel of CTD-ILD experts, including 13 pulmonologists, four rheumatologists, one thoracic radiologist, and one pulmonary pathologist. The proposed criteria reflected the panel’s expert opinion and Authors recognized that they should be tested and validated in future prospective studies, as a high-quality patient cohort for validation does not exist at the moment.
References
- Travis, W.D.; Costabel, U.; Hansell, D.M.; King, T.E.; Lynch, D.A.; Nicholson, A.G.; Ryerson, C.J.; Ryu, J.H.; Selman, M.; Wells, A.U.; et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013, 188, 733–748, doi:10.1164/rccm.201308-1483ST.
- Travis, W.D.; King, T.E.; Bateman, E.D.; Lynch, D.A.; Capron, F.; Center, D.; Colby, T.V.; Cordier, J.F.; DuBois, R.M.; Galvin, J.; et al. American thoracic society/European respiratory society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2002, 165, 277–304, doi:10.1164/ajrccm.165.2.ats01.
- Palm, Ø.; Garen, T.; Enger, T.B.; Jensen, J.L.; Lund, M.B.; AalØkken, T.M.; Gran, J.T. Clinical pulmonary involvement in primary Sjögren’s syndrome: Prevalence, quality of life and mortality—A retrospective study based on registry data. Rheumatology 2013, 52, 173–179, doi:10.1093/rheumatology/kes311.
- Fischer, A. Interstitial Pneumonia with Autoimmune Features. Clin. Chest Med. 2019, 40, 609–616, doi:10.1016/j.ccm.2019.05.007.
- Luppi, F.; Wells, A.U. Interstitial pneumonitis with autoimmune features (IPAF): A work in progress. Eur. Respir. J. 2016, 47, doi:10.1183/13993003.00690-2016.
- Atienza-Mateo, B.; Remuzgo-Martínez, S.; Mora Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.; Prieto-Peña, D.; Calderón-Goercke, M.; Corrales, A.; Blanco Rodríguez, G.; Gómez-Román, J.J.; et al. The Spectrum of Interstitial Lung Disease Associated with Autoimmune Diseases: Data of a 3.6-Year Prospective Study from a Referral Center of Interstitial Lung Disease and Lung Transplantation. J. Clin. Med. 2020, 9, 1606, doi:10.3390/jcm9061606.
- Fischer, A.; Antoniou, K.M.; Brown, K.K.; Cadranel, J.; Corte, T.J.; Du Bois, R.M.; Lee, J.S.; Leslie, K.O.; Lynch, D.A.; Matteson, E.L.; et al. An official European Respiratory Society/American Thoracic Society research statement: Interstitial pneumonia with autoimmune features. Eur. Respir. J. 2015, 46, 976–987, doi:10.1183/13993003.00150-2015.
- McLean-Tooke, A.; Moore, I.; Lake, F. Idiopathic and immune-related pulmonary fibrosis: Diagnostic and therapeutic challenges. Clin. Transl. Immunol. 2019, 8, e1086, doi:10.1002/cti2.1086.
- Fischer, A.; Lee, J.S.; Cottin, V. Interstitial lung disease evaluation: Detecting connective tissue disease. Respiration 2015, 90, 177–184, doi:10.1159/000440665.
- Ferri, C.; Manfredi, A.; Sebastiani, M.; Colaci, M.; Giuggioli, D.; Vacchi, C.; Della Casa, G.; Cerri, S.; Torricelli, P.; Luppi, F. Interstitial pneumonia with autoimmune features and undifferentiated connective tissue disease: Our interdisciplinary rheumatology-pneumology experience, and review of the literature. Autoimmun. Rev. 2016, 15, doi:10.1016/j.autrev.2015.09.003.
- Park, J.H.; Kim, D.S.; Park, I.-N.; Jang, S.J.; Kitaichi, M.; Nicholson, A.G.; Colby, T. V Prognosis of fibrotic interstitial pneumonia: Idiopathic versus collagen vascular disease-related subtypes. Am. J. Respir. Crit. Care Med. 2007, 175, 705–711, doi:10.1164/rccm.200607-912OC.
- Fischer, A.; Du, B.R. Interstitial lung disease in connective tissue disorders. Lancet 2012, 380, 689–698.
- Cottin, V. Significance of connective tissue diseases features in pulmonary fibrosis. Eur. Respir. Rev. 2013, 22, 273–280, doi:10.1183/09059180.00003013.
- Idiopathic Pulmonary Fibrosis Clinical Research Network; Raghu, G.; Anstrom, K.J.; King, T.E.; Lasky, J.A.; Martinez, F.J. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N. Engl. J. Med. 2012, 366, 1968–1977, doi:10.1056/NEJMoa1113354.
- Vacchi, C.; Sebastiani, M.; Cassone, G.; Cerri, S.; Della Casa, G.; Salvarani, C.; Manfredi, A. Therapeutic options for the treatment of interstitial lung disease related to connective tissue diseases. A narrative review. J. Clin. Med. 2020, 9, 407, doi:10.3390/jcm9020407.
- Cassone, G.; Manfredi, A.; Vacchi, C.; Luppi, F.; Coppi, F.; Salvarani, C.; Sebastiani, M. Treatment of Rheumatoid Arthritis-Associated Interstitial Lung Disease: Lights and Shadows. J. Clin. Med. 2020, 9, doi:10.3390/jcm9041082.
- Richeldi, L.; du Bois, R.M.; Raghu, G.; Azuma, A.; Brown, K.K.; Costabel, U.; Collard, H.R. Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis—ProQuest. N. Engl. J. Med. 2014, doi:10.1056/NEJMoa1402584.
- King, T.E.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A Phase 3 Trial of Pirfenidone in Patients with Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2014, doi:10.1056/nejmoa1402582.
- Flaherty, K.R.; Wells, A.U.; Cottin, V.; Devaraj, A.; Walsh, S.L.F.; Inoue, Y.; Richeldi, L.; Kolb, M.; Tetzlaff, K.; Stowasser, S.; et al. Nintedanib in progressive fibrosing interstitial lung diseases. N. Engl. J. Med. 2019, doi:10.1056/NEJMoa1908681.
- Luppi, F.; Spagnolo, P.; Cerri, S.; Richeldi, L. The big clinical trials in idiopathic pulmonary fibrosis. Curr. Opin. Pulm. Med. 2012, 18, 428–432, doi:10.1097/MCP.0b013e3283567ff9.
- Kinder, B.W.; Collard, H.R.; Koth, L.; Daikh, D.I.; Wolters, P.J.; Elicker, B.; Jones, K.D.; King, T.E. Idiopathic nonspecific interstitial pneumonia: Lung manifestation of undifferentiated connective tissue disease? Am. J. Respir. Crit. Care Med. 2007, 176, 691–697, doi:10.1164/rccm.200702-220OC.
- Corte, T.J.; Copley, S.J.; Desai, S.R.; Zappala, C.J.; Hansell, D.M.; Nicholson, A.G.; Colby, T.V.; Renzoni, E.; Maher, T.M.; Wells, A.U. Significance of connective tissue disease features in idiopathic interstitial pneumonia. Eur. Respir. J. 2012, 39, 661–668, doi:10.1183/09031936.00174910.
- Fischer, A.; West, S.G.; Swigris, J.J.; Brown, K.K.; du Bois, R.M. Connective tissue disease-associated interstitial lung disease: A call for clarification. Chest 2010, 138, 251–256, doi:10.1378/chest.10-0194.
- Vij, R.; Noth, I.; Strek, M.E. Autoimmune-featured interstitial lung disease: A distinct entity. Chest 2011, 140, 1292–1299, doi:10.1378/chest.10-2662.
- Assayag, D.; Kim, E.J.; Elicker, B.M.; Jones, K.D.; Golden, J.A.; King, T.E.; Koth, L.L.; Shum, A.K.; Wolters, P.J.; Collard, H.R.; et al. Survival in interstitial pneumonia with features of autoimmune disease: A comparison of proposed criteria. Respir. Med. 2015, 109, 1326–1331, doi:10.1016/j.rmed.2015.08.010.




