Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ronald B. Brown | -- | 1102 | 2024-03-13 13:59:08 | | | |
| 2 | Peter Tang | Meta information modification | 1102 | 2024-03-14 03:30:16 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Brown, R.B. Salt in Low Back Pain and Comorbid Conditions. Encyclopedia. Available online: https://encyclopedia.pub/entry/56215 (accessed on 13 January 2026).
Brown RB. Salt in Low Back Pain and Comorbid Conditions. Encyclopedia. Available at: https://encyclopedia.pub/entry/56215. Accessed January 13, 2026.
Brown, Ronald B.. "Salt in Low Back Pain and Comorbid Conditions" Encyclopedia, https://encyclopedia.pub/entry/56215 (accessed January 13, 2026).
Brown, R.B. (2024, March 13). Salt in Low Back Pain and Comorbid Conditions. In Encyclopedia. https://encyclopedia.pub/entry/56215
Brown, Ronald B.. "Salt in Low Back Pain and Comorbid Conditions." Encyclopedia. Web. 13 March, 2024.
Copy Citation
Low back pain is the world’s leading disability, but the etiology of the majority of low back pain is non-specific with no known cause. Moreover, overuse of opioids to treat low back pain is a widespread problem. Many global populations consume excess sodium chloride, which can lead to fluid overload in hypervolemia, and cause swelling and temporary weight gain associated with low back pain. Numerous conditions comorbid with low back pain are also potentially mediated by excessive salt intake, including migraine headache, hypertension, cardiovascular disease, venous thromboembolism, liver disease, respiratory disorders, chronic kidney disease, pregnancy complications, and multiple sclerosis.
non-specific low back pain
edema
dietary salt
sodium chloride
posterior lumbar subcutaneous edema
hypervolemia
stiff joints
1. Introduction
For the past three decades, low back pain (LBP) has been the world-leading non-fatal cause of disability [1], burdening the U.S. healthcare system with costs exceeded only by diabetes and ischemic heart disease [2]. However, with the exception of LPB arising from pathological mechanisms, specific causes of most LPB (~85%) are unknown [3][4]. Discussing management of non-specific low back pain, the Lancet noted that overuse of opioids, diagnostic imaging, and surgery “remains a widespread problem” [5]. Back pain (in general) is the second most common diagnosis for opioid prescriptions in emergency departments, next to non-fracture injuries, and 45.2% of patients with back pain receive opioids [6]. Other researchers pointed out that although opioids have short-term analgesic effects in chronic back pain, “benefits for function are less clear” [7]. Furthermore, “complications of opioid use include addiction and overdose related mortality, which have risen in parallel with prescription rates.” On the other hand, from a primary prevention perspective, the Lancet predicted that novel approaches to identify and mitigate the cause of non-specific LBP have “potential to help the many people with disabling low back pain worldwide” [5].
Excess body weight has been associated with overall back pain [8], but not all overweight people have back pain, nor are all people with back pain overweight, implying that other etiological factors are involved. Even highly conditioned athletes commonly have low back pain from a “benign” source [9]. Additionally, low-quality dietary patterns with high intake of sodium, saturated fat, and added sugars have been associated with spinal pain [10]. Excessive sodium in the body can cause increased water retention in edema, which could affect tissues involved in LBP of young and old individuals, regardless of body weight and health status.
2. Posterior Lumbar Subcutaneous Edema
Posterior lumbar subcutaneous edema (PLSE) affects deep perifascial soft tissue in the lumbar spine (lumbar vertebrae L1–L5), which is commonly ignored as an incidental finding on spinal magnetic resonance images (MRI) [11]. Importantly, PLSE should not be confused with edema caused by serious trauma and injury. In addition to subcutaneous edema, a case control study found that structures within the lumbar spine may also be affected by edema associated with LBP, such as interspinous ligament edema, facet joint effusion, paraspinal muscle edema, as well as neocyst formation [12]. An important study limitation is that “there was no correlation between the lesions and the intensity of symptoms (degree of pain)”.
Symptoms of edema include swelling, tightness, pain, and stiff joints [13], and cases with PLSE may be accompanied by these edema symptoms. Similar to pain and limited mobility with restricted range of motion associated with edema of peripheral limbs [14], LBP is associated with restricted lumbar range of motion and mobility impairment, sometimes in combination with lower extremity pain [15]. Additionally, qualitative studies of patients with LBP report symptoms of stiffness, which is consistent with tightness and stiff joints from edema [16], although the authors noted that “feeling stiff” is not a reliable biomarker of biomechanical impairment. Importantly, the Mayo Foundation for Medical Education and Research, associated with the Mayo Clinic—the top ranked U.S. hospital in 2021–2022 [17], listed adverse effects from medical administration of sodium chloride. Listed symptoms include joint pain, stiffness and swelling when given orally [18] and pain of the low back when injected [19].
3. Salt and Hypervolemia
Swelling and temporary weight gain in edema is often associated with fluid overload in hypervolemia due to sodium and water retention; as the body’s total sodium content increases, serum levels of sodium in hypervolemia can be high, normal, or low [20], (hypernatremia, eunatremia, and hyponatremia, respectively). Serum sodium becomes dysregulated when renal function is burdened, especially in combination with high dietary sodium intake [21]. The body’s requirement for sodium is low, 500 mg per day [22]. Yet, salt (sodium chloride) contributes excessive amounts of sodium in the diet of many global populations, with an average salt intake of 9−12 g per day [23]. Importantly, the taste for salt decreases as people are exposed to lower dietary intake levels [24]. Potassium also aids renal elimination of sodium to maintain sodium and fluid balance, but dietary potassium intake is often inadequate as consumption of processed foods increases in many populations.
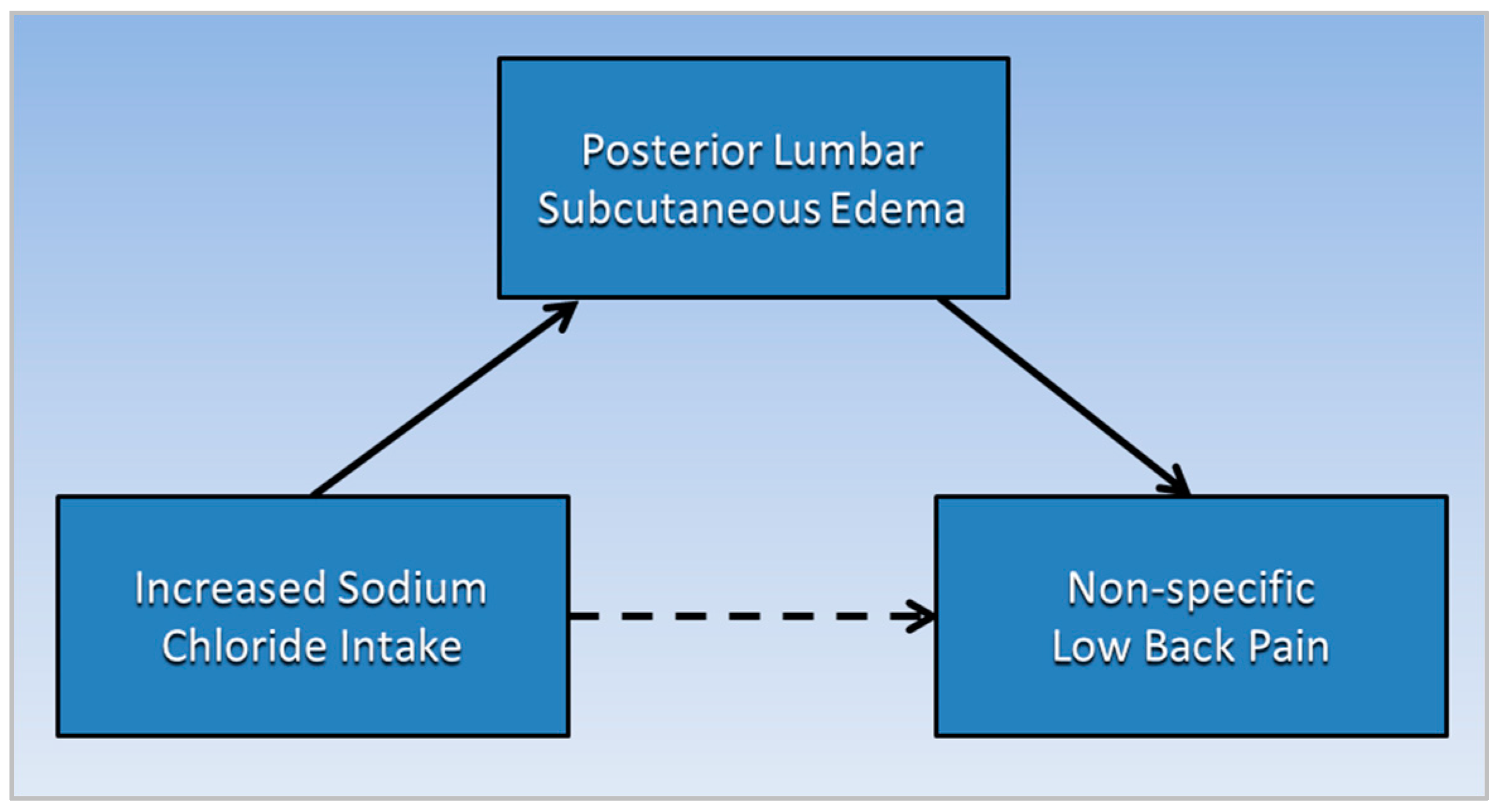
Figure 1 is a directed acyclic graph illustrating the proposed causative pathways (solid lines) in which posterior lumbar subcutaneous edema potentially mediates the association (dotted line) between increased sodium chloride intake and non-specific low back pain. Note that a mediator, or an intermediate variable, is a causative factor that “lies on the causal pathway” [25].
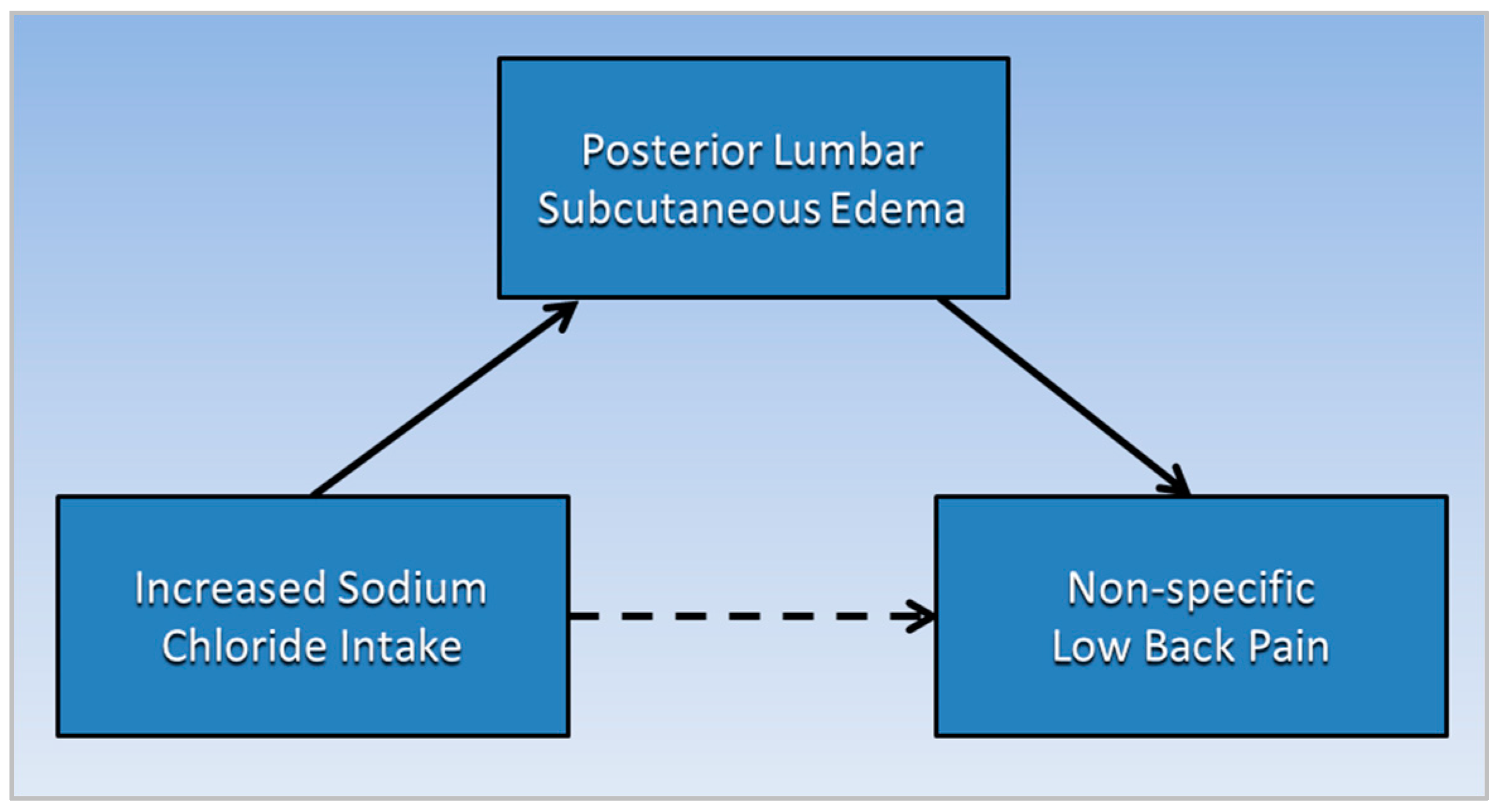
Figure 1. Posterior lumbar subcutaneous edema potentially mediates the association of increased sodium chloride intake with non-specific low back pain.
4. Salt Transitively Links Low Back Pain and Comorbid Conditions
Additional evidence that excessive sodium chloride intake is a potential mediator or causative factor in nonspecific LBP is implied in numerous associations of LBP with comorbid conditions mediated by salt, including migraine headache, hypertension, cardiovascular disease, venous thromboembolism, liver disease, respiratory disorders, chronic kidney disease, pregnancy complications, and multiple sclerosis.
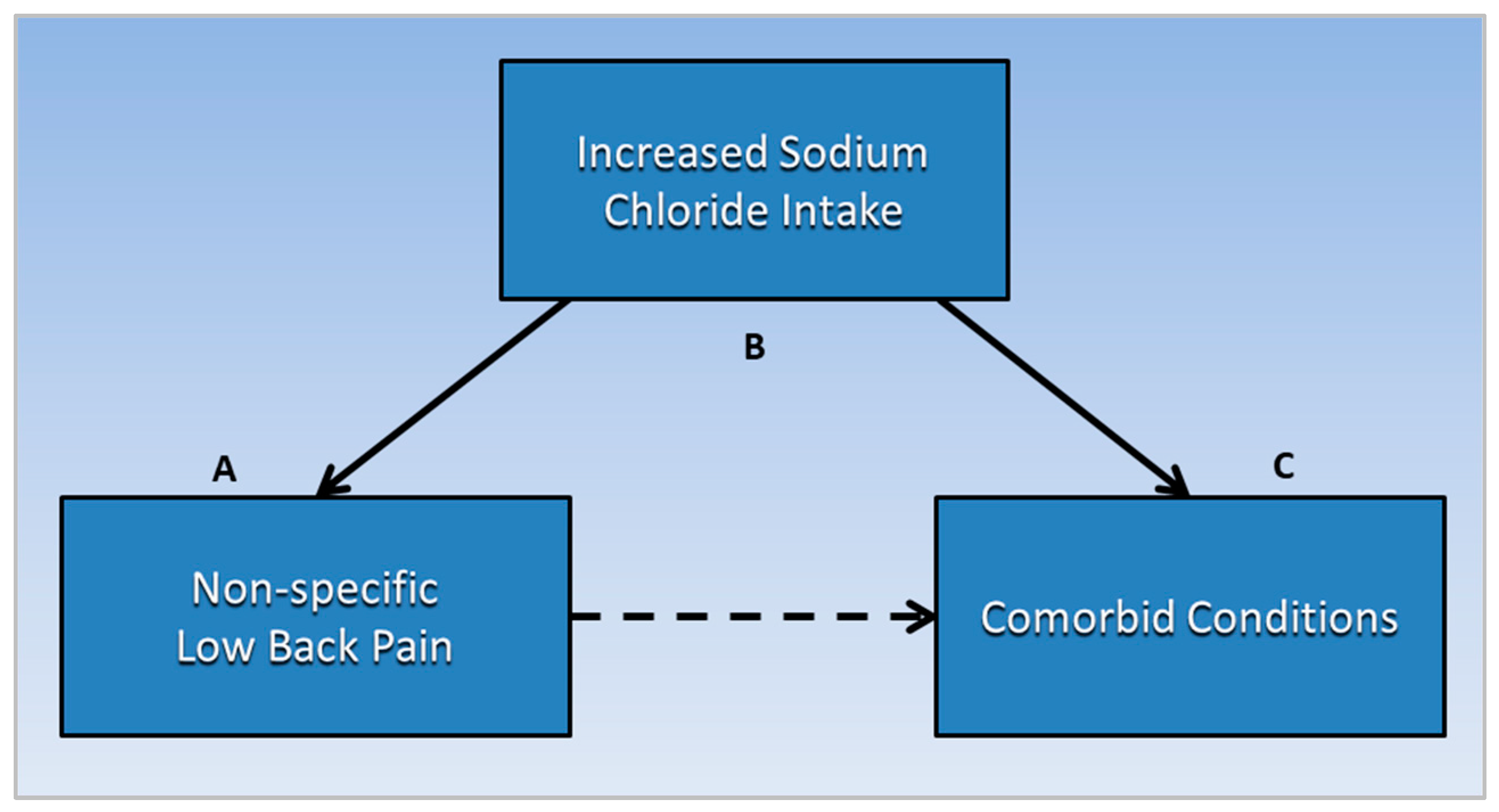
Analysis of research findings in this section uses a transitive inference method, inferring that salt is a common causative factor related to both non-specific LBP and comorbid conditions that are also associated with salt intake. Transitive inference is a technique used in literature-based discovery (LBD) to synthesize new knowledge from disjointed knowledge domains [26]. If concepts A and C from separate knowledge domains are each associated with concept B, a novel association is inferred between A and C through B. This technique is useful for exploring new insights and directions for future research in a new area.
As shown in Figure 2, the following subsections describe evidence transitively linking non-specific LBP (A) with specific comorbid conditions (C), through the common mediating factor of increased salt intake (B). Future studies should investigate prevalence of PLSE in conditions comorbid with non-specific LBP.
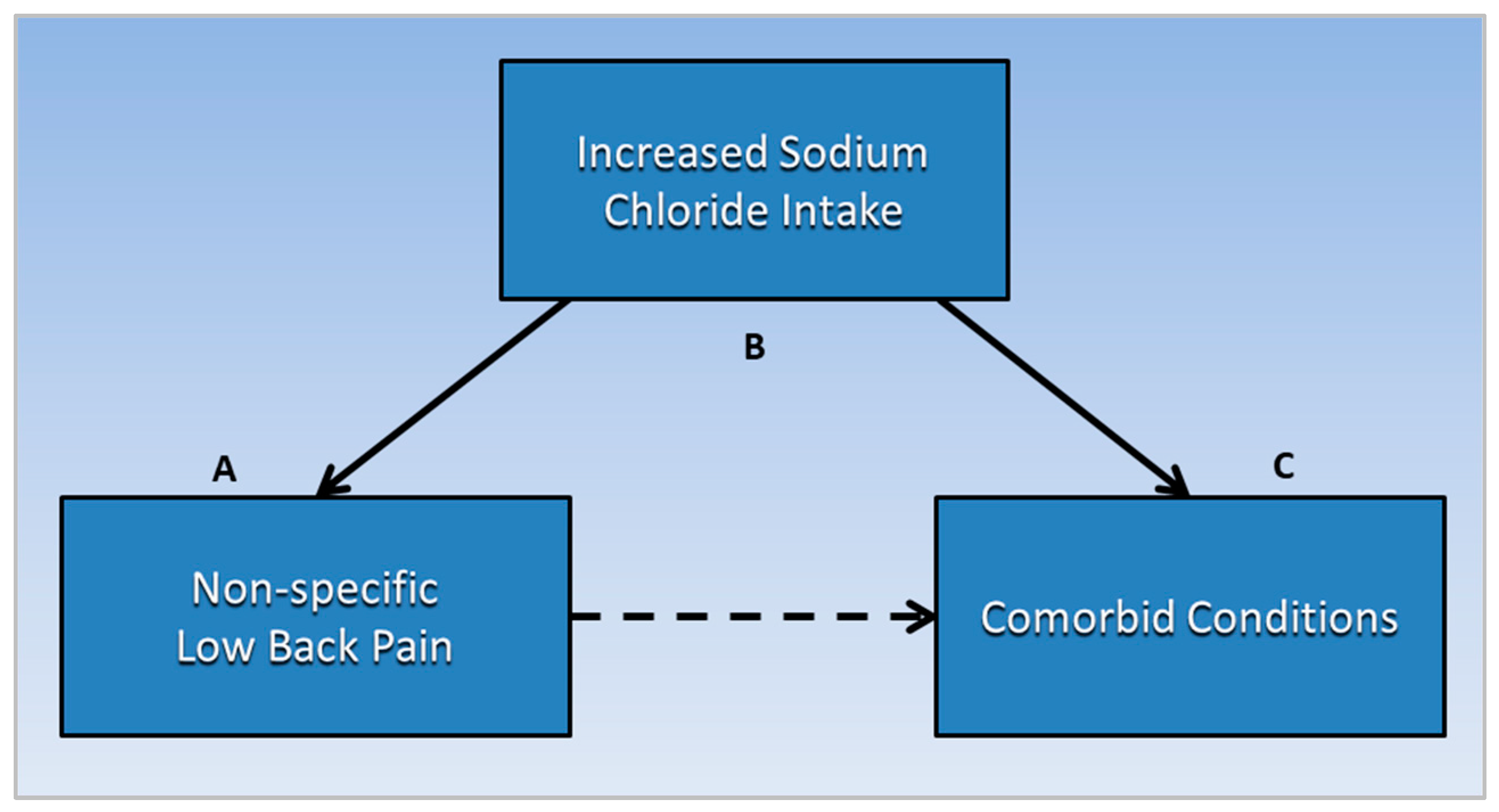
Figure 2. Non-specific low back pain (A) is transitively linked to comorbid conditions (C) through the common mediating factor of increased sodium chloride intake (B). Future studies should investigate prevalence of posterior lumbar subcutaneous edema in conditions comorbid with non-specific low back pain.
References
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858.
- Kim, L.H.; Vail, D.; Azad, T.D.; Bentley, J.P.; Zhang, Y.; Ho, A.L.; Fatemi, P.; Feng, A.; Varshneya, K.; Desai, M.; et al. Expenditures and Health Care Utilization Among Adults With Newly Diagnosed Low Back and Lower Extremity Pain. JAMA Netw. Open 2019, 2, e193676.
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367.
- Koch, C.; Hänsel, F. Non-specific Low Back Pain and Postural Control During Quiet Standing—A Systematic Review. Front. Psychol. 2019, 10, 586.
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747.
- Kea, B.; Fu, R.; Lowe, R.A.; Sun, B.C. Interpreting the National Hospital Ambulatory Medical Care Survey: United States Emergency Department Opioid Prescribing, 2006–2010. Acad. Emerg. Med. 2016, 23, 159–165.
- Deyo, R.A.; Von Korff, M.; Duhrkoop, D. Opioids for low back pain. BMJ 2015, 350, g6380.
- Perera, R.S.; Chen, L.; Hart, D.J.; Spector, T.D.; Arden, N.K.; Ferreira, M.L.; Radojčić, M.R. Effects of body weight and fat mass on back pain—direct mechanical or indirect through inflammatory and metabolic parameters? Semin. Arthritis Rheum. 2022, 52, 151935.
- Mortazavi, J.; Zebardast, J.; Mirzashahi, B. Low Back Pain in Athletes. Asian J. Sports Med. 2015, 6, e24718.
- Zick, S.M.; Murphy, S.L.; Colacino, J. Association of chronic spinal pain with diet quality. Pain Rep. 2020, 5, e837.
- Schwarz-Nemec, U.; Friedrich, K.M.; Arnoldner, M.A.; Schwarz, F.K.; Weber, M.; Trattnig, S.; Grohs, J.G.; Nemec, S.F. When an incidental MRI finding becomes a clinical issue: Posterior lumbar subcutaneous edema in degenerative, inflammatory, and infectious conditions of the lumbar spine. Wien. Klin. Wochenschr. 2020, 132, 27–34.
- Lakadamyali, H.; Tarhan, N.C.; Ergun, T.; Cakir, B.; Agildere, A.M. STIR sequence for depiction of degenerative changes in posterior stabilizing elements in patients with lower back pain. Am. J. Roentgenol. 2008, 191, 973–979.
- Brazier, Y. Everything You Need to Know about Edema. Available online: https://www.medicalnewstoday.com/articles/159111#_noHeaderPrefixedContent (accessed on 21 April 2022).
- Besharat, S.; Grol-Prokopczyk, H.; Gao, S.; Feng, C.; Akwaa, F.; Gewandter, J.S. Peripheral edema: A common and persistent health problem for older Americans. PLoS ONE 2021, 16, e0260742.
- Delitto, A.; George, S.Z.; Van Dillen, L.; Whitman, J.M.; Sowa, G.; Shekelle, P.; Denninger, T.R.; Godges, J.J. Low back pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2012, 42, A1–A57.
- Stanton, T.R.; Moseley, G.L.; Wong, A.Y.L.; Kawchuk, G.N. Feeling stiffness in the back: A protective perceptual inference in chronic back pain. Sci. Rep. 2017, 7, 9681.
- U.S. News Best Hospitals. Available online: https://health.usnews.com/best-hospitals (accessed on 22 June 2022).
- MFMER. Sodium Chloride (Oral Route) Side Effects. Mayo Foundation for Medical Education and Research. Available online: https://www.mayoclinic.org/drugs-supplements/sodium-chloride-oral-route/side-effects/drg-20122545 (accessed on 23 June 2022).
- Sodium Chloride (Injection Route) Side Effects. Available online: https://www.mayoclinic.org/drugs-supplements/sodium-chloride-injection-route/side-effects/drg-20068846 (accessed on 2 May 2022).
- Cirino, E. Hypervolemia (Fluid Overload). Available online: https://www.healthline.com/health/hypervolemia (accessed on 22 April 2022).
- Oppelaar, J.J.; Vogt, L. Body Fluid-Independent Effects of Dietary Salt Consumption in Chronic Kidney Disease. Nutrients 2019, 11, 2779.
- NHLBI. Implementing Recommendat Ions for Dietary Salt Reduction: Where Are We? Where Are We Going? How Do We Get There?: A Summary of an NHLBI Workshop; National Institutes of Health, National Heart, Lung, and Blood Institute: Bethesda, MA, USA, 1996.
- Salt Reduction. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 22 April 2022).
- Bertino, M.; Beauchamp, G.K.; Engelman, K. Long-term reduction in dietary sodium alters the taste of salt. Am. J. Clin. Nutr. 1982, 36, 1134–1144.
- Imai, K.; Keele, L.; Tingley, D.; Yamamoto, T. Unpacking the Black Box of Causality: Learning about Causal Mechanisms from Experimental and Observational Studies. Am. Political Sci. Rev. 2011, 105, 765–789.
- Thilakaratne, M.; Falkner, K.; Atapattu, T. A systematic review on literature-based discovery workflow. PeerJ Comput. Sci. 2019, 5, e235.
More
Information
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.8K
Revisions:
2 times
(View History)
Update Date:
14 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




