Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Robson Amorim | -- | 1244 | 2024-03-07 03:04:26 | | | |
| 2 | Jessie Wu | + 16 word(s) | 1260 | 2024-03-07 04:54:34 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
De Macedo Filho, L.; Figueredo, L.F.; Villegas-Gomez, G.A.; Arthur, M.; Pedraza-Ciro, M.C.; Martins, H.; Kanawati Neto, J.; Hawryluk, G.J.; Amorim, R.L.O. Pathophysiology-Based Traumatic Brain Injury. Encyclopedia. Available online: https://encyclopedia.pub/entry/55945 (accessed on 28 February 2026).
De Macedo Filho L, Figueredo LF, Villegas-Gomez GA, Arthur M, Pedraza-Ciro MC, Martins H, et al. Pathophysiology-Based Traumatic Brain Injury. Encyclopedia. Available at: https://encyclopedia.pub/entry/55945. Accessed February 28, 2026.
De Macedo Filho, Leonardo, Luisa F. Figueredo, Gustavo Adolfo Villegas-Gomez, Matthew Arthur, Maria Camila Pedraza-Ciro, Henrique Martins, Joaquim Kanawati Neto, Gregory J. Hawryluk, Robson Luís Oliveira Amorim. "Pathophysiology-Based Traumatic Brain Injury" Encyclopedia, https://encyclopedia.pub/entry/55945 (accessed February 28, 2026).
De Macedo Filho, L., Figueredo, L.F., Villegas-Gomez, G.A., Arthur, M., Pedraza-Ciro, M.C., Martins, H., Kanawati Neto, J., Hawryluk, G.J., & Amorim, R.L.O. (2024, March 07). Pathophysiology-Based Traumatic Brain Injury. In Encyclopedia. https://encyclopedia.pub/entry/55945
De Macedo Filho, Leonardo, et al. "Pathophysiology-Based Traumatic Brain Injury." Encyclopedia. Web. 07 March, 2024.
Copy Citation
Traumatic brain injury (TBI) is a leading cause of disability and death among children and young adults, with an incidence of approximately 1.7 million per year in the USA, resulting in 52,000 deaths. Survivors of the initial impact must still contend with the consequences of trauma, as not all injury occurs at the time of impact. The primary injury results from forces applied to the head and involve direct structural damage to the brain. This triggers a cascade of events leading to neurological damage that evolves secondary injury. Several external brain insults, both intracranial and systemic, may complicate and worsen the secondary injury.
secondary TBI
traumatic brain injury
brain injuries
physiopathology
1. Spectrum of Traumatic Brain Injury Secondary Injuries
1.1. Mild Traumatic Brain Injury (mTBI)
Mild traumatic brain injury (mTBI), commonly known as concussion, is characterized by a range of subtle yet significant biochemical and cellular changes [1]. These changes primarily include temporary dysfunction in neuronal connectivity and metabolism [2]. Key features often involve minor axonal disruptions, alterations in ion channels leading to ionic fluxes, and imbalances in neurotransmitters [3]. While the structural integrity of the brain may largely remain intact, these molecular and cellular disturbances can result in symptoms such as headache, dizziness, and short-term memory disturbances [3]. Despite the transient nature of these symptoms, a subset of patients might experience prolonged post-concussive syndromes, wherein symptoms persist for weeks or months [3]. This phenomenon underscores the need for a nuanced understanding of mTBI’s secondary effects, particularly in the context of repeated injuries and their cumulative impact [3].
1.2. Severe Traumatic Brain Injury
Severe traumatic brain injury (TBI) is marked by more profound and immediate secondary injuries that can be life-threatening and lead to long-term disabilities. The hallmark of severe TBI includes cerebral edema (swelling of the brain), increased intracranial pressure, and significant axonal injury [4]. These injuries can disrupt the blood-brain barrier, leading to inflammatory responses and oxidative stress, which further exacerbate brain damage. Secondary insults in severe TBI may also encompass hemorrhagic lesions, hypoxia, and ischemia [5], contributing to a complex cascade of neurodegeneration. The consequences of these injuries are often severe, manifesting as long-term cognitive, behavioral, and motor impairments [5]. Management of severe TBI is multifaceted, involving acute medical interventions to stabilize the patient and extensive rehabilitation programs to aid recovery and improve quality of life.
1.3. Subdural Hematoma (SDH)
Subdural hematoma (SDH) occurs when blood collects between the dura mater and the arachnoid layer of the brain [6]. This accumulation of blood leads to increased intracranial pressure, which can cause significant secondary brain injury [6]. Patients with SDH often experience a progressive decline in consciousness, headache, and hemiparesis [6]. The secondary injuries in SDH can include brain herniation, ischemic injury due to compression of blood vessels, and hypoxic injury from reduced blood flow [7]. The management of SDH focuses on surgical intervention to evacuate the hematoma and relieve pressure, followed by monitoring for potential complications like rebleeding or seizures [7].
1.4. Subarachnoid Hemorrhage (SAH)
Subarachnoid hemorrhage (SAH) involves bleeding into the subarachnoid space, the area between the arachnoid membrane and the pia mater surrounding the brain [8]. This type of hemorrhage is often caused by the rupture of cerebral aneurysms [8]. The primary concern in SAH is the risk of rebleeding and the development of cerebral vasospasm, which can lead to ischemic injury [9]. Secondary injuries in SAH also include hydrocephalus and elevated intracranial pressure [9]. The management of SAH is complex, often requiring nimble balancing of maintaining cerebral perfusion while minimizing the risk of rebleeding and managing vasospasms, often through medication and surgical interventions [9].
1.5. Contusions
Cerebral contusions are essentially bruises on the brain tissue, occurring typically at the site of impact or, in some cases, at a location opposite to the point of impact (coup-contrecoup injury) [10]. These injuries result from the brain striking the inner surface of the skull [11]. Contusions are characterized by localized bleeding and swelling in the brain tissue [10]. The swelling, or edema, can lead to an increase in intracranial pressure, potentially causing a reduction in cerebral blood flow and oxygen supply [12]. In severe cases, this can escalate into a herniation syndrome, where brain tissue is displaced from its normal position [12]. The management of contusions may involve monitoring for changes in neurological status and intracranial pressure, and in some cases, surgical intervention is required to alleviate pressure [12]. Rehabilitation is often necessary to address cognitive and motor deficits resulting from the injury [13].
1.6. Diffuse Axonal Injury (DAI)
Diffuse Axonal Injury is a form of TBI that involves widespread damage to the brain’s white matter [14]. This injury occurs when the brain rapidly shifts inside the skull, typically as a result of high-velocity impacts such as those seen in car accidents or falls from significant heights [14]. The shearing forces during the impact disrupt the axons, leading to a breakdown in neuronal communication [15]. The hallmark of diffuse axonal injury (DAI) is a disruption of the normal signaling and connectivity within the brain, which can lead to a variety of symptoms, ranging from subtle cognitive impairments to prolonged coma [15]. Diagnosis is often challenging due to the microscopic nature of the injury and may require advanced imaging techniques like Diffusion Tensor Imaging (DTI) [16]. The treatment for DAI is largely supportive, focusing on managing symptoms and preventing secondary injuries [16]. Rehabilitation plays a critical role in the recovery process, with a focus on maximizing functional independence and cognitive recovery.
1.7. Penetrating Brain Injuries
Penetrating brain injuries occur when an object, such as a bullet or sharp instrument, breaches the skull and enters the brain tissue [17]. These injuries are particularly severe due to the direct damage to brain tissue and the high risk of infection and inflammation [17]. The trajectory and speed of the penetrating object play a significant role in the extent of the injury. Immediate concerns include bleeding, increased intracranial pressure, and the risk of secondary injuries due to brain swelling and herniation [18]. Surgical intervention is often necessary to remove foreign objects, repair damaged tissue, and reduce intracranial pressure [18]. Antibiotic therapy is critical to prevent or treat infections. Long-term rehabilitation is required to address physical, cognitive, and psychological impacts [19]. Due to the complex nature of these injuries, outcomes can vary widely, with some individuals experiencing significant long-term disabilities.
2. Pathophysiology of Secondary Brain Injury
Secondary traumatic brain injury is the neurological damage that evolves due to the primary injury (Figure 1). Within the first few hours following the injury, a series of events may trigger a cascade of secondary metabolic, inflammatory, and ischemic insults that can exacerbate the primary neuronal injury. These events are associated with the activation of genes that lead to the transcription of proteins and enzymes involved in the release of excitatory amino acids, the production of free radicals and inflammatory cytokines, alterations in ion flux across membranes, upregulation of neuroprotective cascades, and the induction of programmed cell death [20].
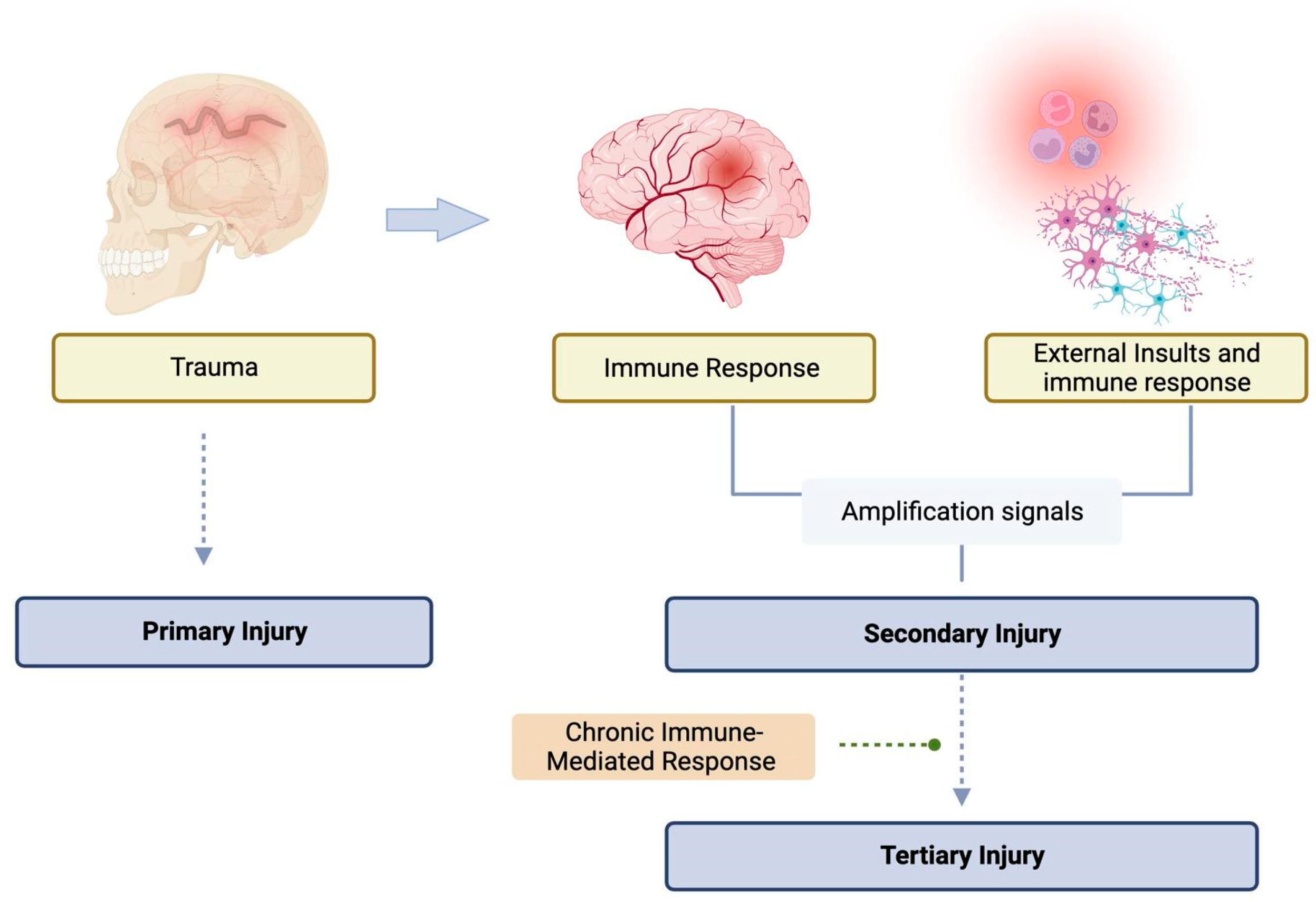
Figure 1. Schematic view of the primary, secondary, and tertiary injuries after TBI. Solid arrows indicate an association, and dashed arrows indicate the following stage (leads to).
Alterations in cellular metabolism and signaling pathways (Figure 2) can lead to the depletion of energy reserves. As a result, neuronal cells may no longer be able to maintain depolarization of their membranes, causing alterations in ion fluxes and osmotic swelling of the cells. Therefore, following TBI, it is crucial to recognize, prevent, and treat secondary injury to ensure neuronal survival.
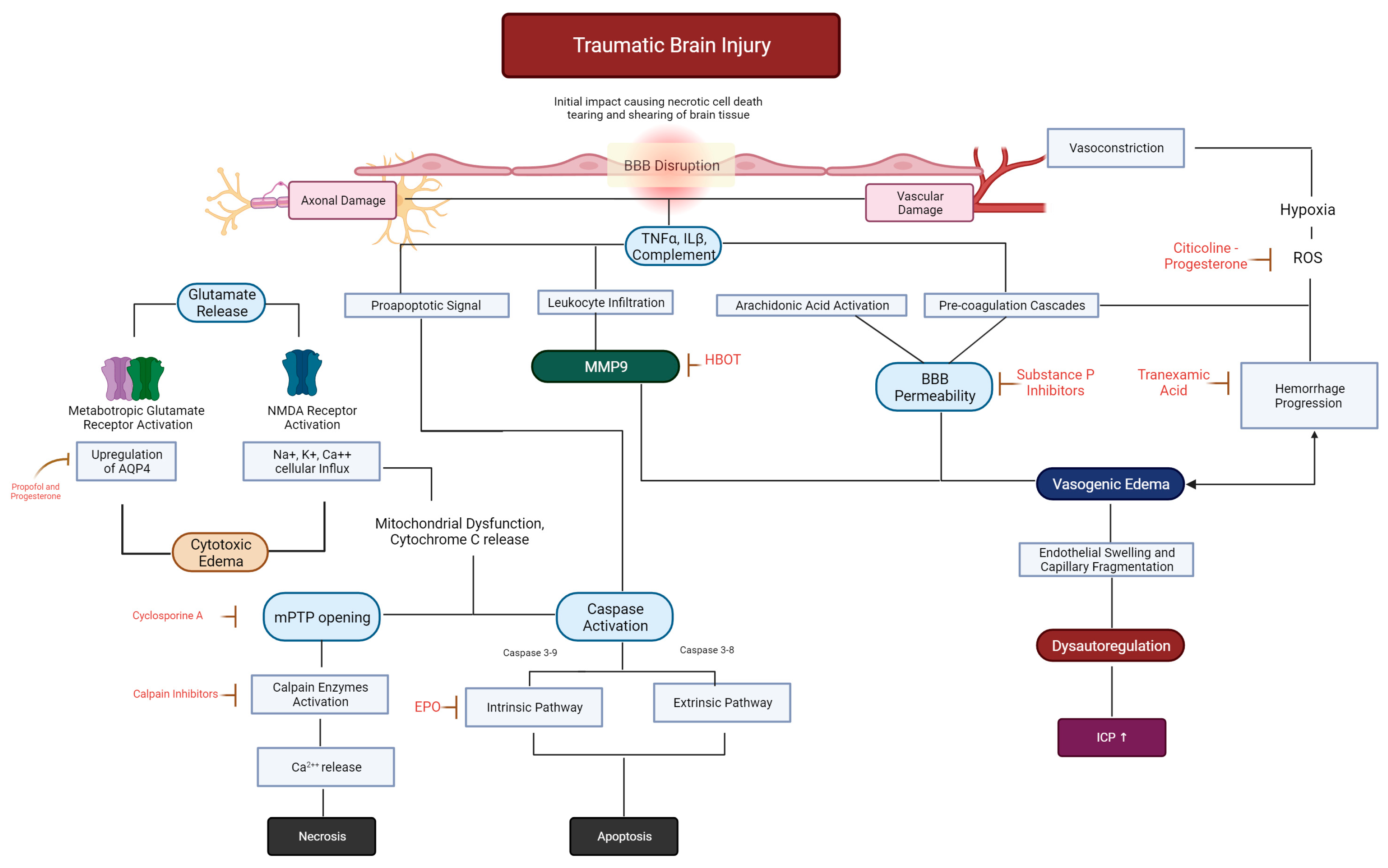
Figure 2. Schematic evolution of the major mechanisms involved in the secondary injury of TBI. The sequence of events can occur simultaneously and interact to exacerbate injury and initiate neuronal and vascular repair. Potential drugs are placed in red-doted arrows directed to their leading site of action. Black solid lines indicate association, while red continuous indicate an inhibitor of the pathway.
References
- Romeu-Mejia, R.; Giza, C.C.; Goldman, J.T. Concussion Pathophysiology and Injury Biomechanics. Curr. Rev. Musculoskelet. Med. 2019, 12, 105–116.
- Langlois, J.A.; Rutland-Brown, W.; Wald, M.M. The Epidemiology and Impact of Traumatic Brain Injury: A brief overview. J. Head Trauma Rehabil. 2006, 21, 375–378.
- Girgis, F.; Pace, J.; Sweet, J.; Miller, J.P. Hippocampal Neurophysiologic Changes after Mild Traumatic Brain Injury and Potential Neuromodulation Treatment Approaches. Front. Syst. Neurosci. 2016, 10, 8.
- Maas, A.I.R.; Stocchetti, N.; Bullock, R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008, 7, 728–741.
- Galgano, M.; Toshkezi, G.; Qiu, X.; Russell, T.; Chin, L.; Zhao, L.-R. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplant. 2017, 26, 1118–1130.
- Aromatario, M.; Torsello, A.; D’errico, S.; Bertozzi, G.; Sessa, F.; Cipolloni, L.; Baldari, B. Traumatic Epidural and Subdural Hematoma: Epidemiology, Outcome, and Dating. Medicina 2021, 57, 125.
- Shin, D.-S.; Hwang, S.-C. Neurocritical Management of Traumatic Acute Subdural Hematomas. Korean J. Neurotrauma 2020, 16, 113–125.
- Griswold, D.P.; Fernandez, L.L.; Rubiano, A.M. Traumatic Subarachnoid Hemorrhage: A Scoping Review. J. Neurotrauma 2022, 39, 35–48.
- Vinciguerra, L.; Bösel, J. Noninvasive Neuromonitoring: Current Utility in Subarachnoid Hemorrhage, Traumatic Brain Injury, and Stroke. Neurocritical Care 2017, 27, 122–140.
- Adatia, K.; Newcombe, V.F.J.; Menon, D.K. Contusion Progression Following Traumatic Brain Injury: A Review of Clinical and Radiological Predictors, and Influence on Outcome. Neurocritical Care 2021, 34, 312–324.
- Sturiale, C.L.; De Bonis, P.; Rigante, L.; Calandrelli, R.; D’Arrigo, S.; Pompucci, A.; Mangiola, A.; D’Apolito, G.; Colosimo, C.; Anile, C. Do traumatic brain contusions increase in size after decompressive craniectomy? J. Neurotrauma 2012, 29, 2723–2726.
- Simard, J.M.; Kilbourne, M.; Tsymbalyuk, O.; Tosun, C.; Caridi, J.; Ivanova, S.; Keledjian, K.; Bochicchio, G.; Gerzanich, V. Key role of sulfonylurea receptor 1 in progressive secondary hemorrhage after brain contusion. J. Neurotrauma 2009, 26, 2257–2267.
- Kurland, D.; Hong, C.; Aarabi, B.; Gerzanich, V.; Simard, J.M. Hemorrhagic progression of a contusion after traumatic brain injury: A review. J. Neurotrauma 2012, 29, 19–31.
- Smith, D.H.; Meaney, D.F.; Shull, W.H. Diffuse Axonal Injury in Head Trauma. J. Head Trauma Rehabil. 2003, 18, 307–316.
- Humble, S.S.; Wilson, L.D.; Wang, L.; Long, D.A.; Smith, M.A.; Siktberg, J.C.; Mirhoseini, M.F.; Bhatia, A.; Pruthi, S.; Day, M.A.; et al. Prognosis of diffuse axonal injury with traumatic brain injury. J. Trauma Inj. Infect. Crit. Care Surg. 2018, 85, 155–159.
- Johnson, V.E.; Stewart, W.; Smith, D.H. Axonal pathology in traumatic brain injury. Exp. Neurol. 2013, 246, 35–43.
- Takahashi, C.E.; Virmani, D.; Chung, D.Y.; Ong, C.; Cervantes-Arslanian, A.M. Blunt and Penetrating Severe Traumatic Brain Injury. Neurol. Clin. 2021, 39, 443–469.
- Fathalla, H.; Ashry, A.; El-Fiki, A. Managing military penetrating brain injuries in the war zone: Lessons learned. Neurosurg. Focus 2018, 45, E6.
- Solumsmoen, S.; Lilja-Cyron, A.; Buch, K.F.; Kelsen, J. Traumatic penetrating brain injury. Ugeskr Laeger 2018, 180, V03180201.
- Raghupathi, R. Cell Death Mechanisms Following Traumatic Brain Injury. Brain Pathol. 2004, 14, 215–222.
More
Information
Subjects:
Neurosciences
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
5.0K
Entry Collection:
Neurodegeneration
Revisions:
2 times
(View History)
Update Date:
07 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





