Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Meher Oberoi | -- | 3057 | 2024-02-20 20:55:56 | | | |
| 2 | Lindsay Dong | Meta information modification | 3057 | 2024-02-21 02:25:14 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Oberoi, M.; Noor, M.S.; Abdelfatah, E. Surgical Management of Gastroesophageal Junction Adenocarcinoma. Encyclopedia. Available online: https://encyclopedia.pub/entry/55252 (accessed on 08 March 2026).
Oberoi M, Noor MS, Abdelfatah E. Surgical Management of Gastroesophageal Junction Adenocarcinoma. Encyclopedia. Available at: https://encyclopedia.pub/entry/55252. Accessed March 08, 2026.
Oberoi, Meher, Md. Sibat Noor, Eihab Abdelfatah. "Surgical Management of Gastroesophageal Junction Adenocarcinoma" Encyclopedia, https://encyclopedia.pub/entry/55252 (accessed March 08, 2026).
Oberoi, M., Noor, M.S., & Abdelfatah, E. (2024, February 20). Surgical Management of Gastroesophageal Junction Adenocarcinoma. In Encyclopedia. https://encyclopedia.pub/entry/55252
Oberoi, Meher, et al. "Surgical Management of Gastroesophageal Junction Adenocarcinoma." Encyclopedia. Web. 20 February, 2024.
Copy Citation
Gastroesophageal (GE) junction adenocarcinoma is an aggressive malignancy of growing incidence and is associated with public health issues such as obesity and GERD. Management has evolved over the last two decades to incorporate a multidisciplinary approach, including endoscopic intervention, neoadjuvant chemotherapy/chemoradiation, and open or minimally invasive surgical approaches. Surgical approaches include esophagectomy, total gastrectomy, and, more recently, proximal gastrectomy.
gastroesophageal junction cancer
esophagogastric cancer
gastroesophageal cancer
esophageal cancer
gastric cancer
esophagectomy
1. Introduction
Gastroesophageal (GE) junction adenocarcinomas are an aggressive malignancy of growing concern due to their rising incidence in western populations. They are often advanced at the time of diagnosis and have a poor prognosis, with an estimated median 5-year survival of less than 2 years [1][2][3]. Additionally, their association with obesity and Barrett’s esophagus makes them a pertinent public health concern [4][5][6][7]. With several areas of controversy, including their true biologic nature, the anatomic challenges associated with their location at the intersection of two body compartments, and questions of the optimal approach to multidisciplinary and surgical management, GE junction adenocarcinomas are an evolving area of foregut and oncologic surgery.
2. Definition of GE Junction Tumors
Siewert Classification
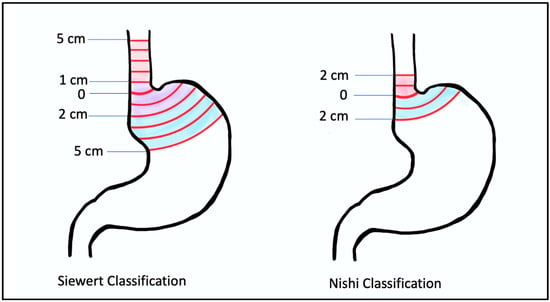
For the purpose of surgical planning, Siewert’s classification system is the most widely followed for GE junction cancers. Siewert et al. originally defined the GE junction topographically at the angle of His where the esophagus joins the cardia and further divided GE junction tumors into three therapeutically relevant types: Type I tumors are located between 5 and 1 cm proximal to the GE junction; type II tumors are located between 1 cm proximal and 2 cm distal to the GE junction; and type III tumors are located between 2 and 5 cm distal to the GE junction [8][9].
While US surgeons fairly uniformly use the Angle of His in concordance with the Siewert classification, there are differences among other specialties in how the GE junction is defined. Gastroenterologists use endoscopic visualization of the proximal extent of the longitudinal gastric folds (different from the squamocolumnar junction or z-line, which lies 3–10 mm proximal to this), and pathologists define it as the most proximal aspect of the gastric folds in an opened surgical specimen. There is no reliable radiographic definition of the GE junction. Additionally, it is important to note that the location of the GE junction may be affected by factors like diaphragmatic movement with respiration, which can cause inter-observer differences, the presence of Barrett’s esophagus, and hiatal hernias, which may change the location of the GE junction [10][11]. Other countries may not use the Siewert system at all. For example, Japan uses the Nishi classification system, which defines GE junction tumors as 2 cm above and below the GE junction (Figure 1).
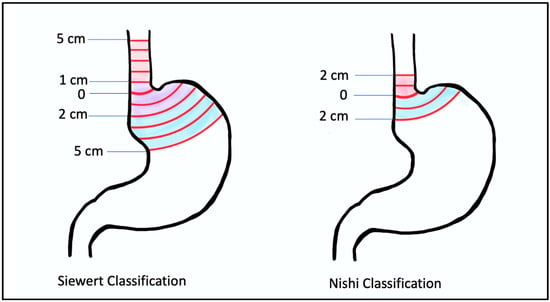
Figure 1. Siewert classification (left) and Nishi classification (right): Siewert classification describes type I tumors as those that lie between 5 cm and 1 cm from the angle of His; type II tumors as those that lie between 1 cm proximal and 2 cm distal from the angle of His; and type III tumors as those that lie between 2 cm and 5 cm distal to the angle of His. The Nishi Classification System is different in that it limits the definition of the GE junction to 2 cm instead of 5 cm proximal and distal to the angle of His.
3. Incidence and Prognosis
Between the 1970s and 1990s, the incidence of GE junction adenocarcinoma in the US increased by almost 2.5-fold, followed by a subsequent plateau since the 1990s [2]. This sharp rise in incidence of GE junction cancers garnered concern and raised questions regarding the contributing factors, one of which may have been the change in classification from “non-specific” to “cardia” cancers before the 1990s. A study in 2004 hypothesized that this improved classification had resulted in the perceived sharp increase in incidence. The authors used the SEER database to evaluate the true incidence of cardia cancers in white males from 1974–1998 and reported a decrease in unspecified gastric cancers from 38 to 14%, with a corresponding unadjusted increase in the incidence of cardia cancers of 77%.
Regardless, the most recent estimate of GE junction cancers comes from a 2018 study that used GLOBOCAN to estimate the global disease burden of esophageal and gastric cancers. The authors found a total of 181,000 cases of cardia gastric cancers in 2018 worldwide, with the majority (75%) occurring in Asian countries and 5% occurring in North America. The authors commented on the increasing incidence in younger populations in otherwise low-incidence countries such as the US and UK [3]. This rising incidence may be attributable to the increasing prevalence of obesity, GERD, and Barrett’s esophagus in the Western world. While H. pylori remains a notable risk factor in distal gastric cancers in Asian countries, it is not associated with GEJ junction cancers in western populations [2][12].
4. Biological Characteristics of GE Junction Cancers
The traditional thinking in regard to the origin of GE junction adenocarcinomas has been that Siewert type I adenocarcinomas, or those just proximal to the GE junction, are esophageal in origin, arising from intestinal metaplasia of the squamous esophageal epithelium, or Barrett’s esophagus. This contradicts the initial description of Barrett’s esophagus as a proximal migration of the stomach epithelium [13]. Cancers at or just distal to the GE junction are thought to be gastric in origin. However, more recently, the very origin of Barrett’s esophagus has come into question.
Despite the evidence suggesting a common gastric origin, there are notable differences in the cancers of the GE junction and those located more distally in the stomach. An association with microsatellite instability, Ebstein-Barr virus infection, Helicobacter pylori infections, and diffuse-type tumor pathology are all more common in non-GE junction or distal gastric cancers, in contrast to a stronger association with obesity, GERD, and Barrett’s esophagus in GE junction cancers [2][14].
5. Early-Stage Disease
Early-stage cancers of the GE junctions, which are limited to the mucosa, well differentiated, small (<2 cm), and without nodal involvement, lymphovascular invasion, or perineural invasion, do not require systemic therapy and are treated with upfront resection. This is due to the low nodal metastatic rate of T1a lesions [15]. This may be achieved via surgical excision or, more preferably, endoscopically, if feasible, via techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD), often in conjunction with ablation [16][17].
6. Resectable Locoregional and Locally Advanced Disease
6.1. Chemoradiation and Chemotherapy
Chemoradiation has been used in the multidisciplinary treatment paradigm of GE junction adenocarcinoma for the past two decades. The CROSS trial, published in 2012, was a landmark study that compared chemoradiation followed by surgery versus surgery alone in esophageal and GE junction cancer and found improved 5-year overall survival with the addition of chemoradiation. However, the degree of benefit was greater in the squamous cell carcinoma group, with pathologic complete response rates of 49% in this group compared to 23% in the adenocarcinoma group, which included GE junction tumors.
However, concomitant with these results, the MAGIC trial published its findings in 2006 demonstrating significant survival benefit with a joint pre(three cycles)- and post(three cycles)- operative chemotherapy regimen of Cisplatin, Fluorouracil, and Epirubicin (ECF) when compared with surgery alone; 5-year overall survival was 36% in the perioperative chemo group vs. 23% in the surgery alone group, p = 0.009 [18]. The MAGIC trial included only adenocarcinomas, 11.2% of which were classified as esophagogastric junction tumors, as well as 14.8% lower esophageal and 74% gastric tumors, and it is unclear how many of those gastric or lower esophageal tumors would have fallen into the Siewert classification of GE junction tumors.
The MAGIC trial did not specifically comment on rates of R0 resection but did report tumor shrinkage in the chemotherapy group (3 cm vs. 5 cm, p < 0.001), downstaging with a higher proportion of T1-T2 tumors (51.7% vs. 36.8%, p = 0.002), and less advanced nodal disease (84.4% vs. 70.5%, p = 0.01) in the chemotherapy group [18]. The CROSS trial found higher rates of R0 resection in the chemoradiation group when compared with upfront surgery (92% vs. 69%, p < 0.001) [19]. Both trials found no difference in the rates of postoperative complications and 30-day mortality when compared with surgery alone. The FLOT trial reported higher rates of R0 resection in the FLOT group (85% vs. 778%, p = 0.0162) and also found no difference in postoperative complications or 30-day mortality when comparing the FLOT regimen with ECF/ECX [20].
6.2. Immunotherapy
Immunotherapy has been incorporated into the management of GE junction adenocarcinoma. The CheckMate 577 trial randomized patients with stage II or III esophageal or GE junction cancer who had undergone chemoradiation followed by R0 resection and had residual pathological disease on the resection specimen to receive adjuvant PD-1 checkpoint inhibition with nivolumab vs. placebo. They found that patients who received Nivolumab had a median disease-free survival of 22.4 months, compared to 11.0 months (p < 0.001). The study concluded that the risk of distant recurrence or death was 26% lower with Nivolumab than with placebo [21].
7. Tailored Therapy for HER-2-Positive GE Junction Adenocarcinoma
There is promising data for the use of trastuzumab in HER2-positive gastric and GE junction cancers. The ToGa trial reported a significant survival advantage (13.8 months vs. 11.1 months, p = 0.0046) with the addition of Traztuzumab to the capecitabine/cisplatin/FU regimen in patients with HER-2-positive gastric and GE junction cancers [22]. The HER-FLOT trial evaluated patients with HER2-positive gastric and GE junction cancers staged cT2 or higher and/or cN+ without distant metastases and reported a pathologic complete response rate of 21.4% in patients who received trastuzumab in addition to the FLOT regimen [23]. However, Phase III RTOG 1010, which compared CROSS vs. CROSS + Trastuzumab, found no additional benefit in pathologic response or disease-free survival [24]. Thus far, this suggests that there is an advantage when adding Trastuzumab to chemotherapy but not when added to chemoradiation; however, more long-term data are needed.
8. Surgery
8.1. Transhiatal Esophagectomy
This operation utilizes abdominal incisions and a neck incision for a transcervical anastomosis. The stomach is mobilized, and the gastric conduit is created while preserving the right gastroepiploic artery. The left gastric artery and vein are identified and divided at their origin to perform a lymphadenectomy. A penrose drain is placed around the GE junction for caudal retraction of the stomach and lower esophagus. The nodal tissue in the lower mediastinum is then dissected under direct visualization. The distal 5–10 cm of mediastinal esophagus is also dissected first with an electrosurgical device and then bluntly with tactile guidance from a bougie placed in the esophagus if performed open. Using minimally invasive or robotic approaches can often achieve visualization higher up into the mediastinum. In the neck, an incision is created, dividing the omohyoid muscle while identifying and preserving the left recurrent laryngeal nerve. The dissection is carried down to the prevertebral fascia and esophagus, until the surgeon is able to pass the index finger between the prevertebral fascia and esophagus and subsequently dissect the cervical esophagus off the trachea.
8.2. Ivor–Lewis Esophagectomy
This operation utilizes abdominal and thoracic incisions for a transthoracic anastomosis. The stomach is mobilized while preserving the right gastroepiploic artery. The left gastric pedicle is divided at its origin. The phrenoesophageal membrane is divided, and the right crus may be divided if necessary as well. The conduit is created by dividing the stomach along the lesser curvature, starting proximally to the right gastric artery and ending in between the cardia and the fundus. A pyloric drainage procedure may be performed, such as a pyloromyotomy, pyloroplasty, or botox injection; however, recent studies have questioned the utility of this [25][26].The patient is repositioned, and through a thoracic incision, the thoracic esophagus is mobilized and transected, and a lymphadenectomy of the paraoesophageal, inferior pulmonary ligament, and subcarinal lymph nodes is performed. The conduit is then pulled into the chest, and an esophagogastric anastomosis is performed.
8.3. McKeown Esophagectomy
This operation combines the Ivor–Lewis and transhiatal approaches and utilizes abdominal, thoracic, and neck incisions. The thoracic portion of the operation is completed first in the left lateral decubitus position. The patient is then repositioned to the supine position for the creation of the gastric conduit, and the anastomosis is performed in the neck [27].
8.4. Minimally Invasive Approaches
Esophagectomies are increasingly being performed with minimally invasive approaches, either robotically or laparoscopically/thoracoscopically. The TIME trial was a multicenter, randomized controlled trial that showed significantly lower pulmonary infection rates (12% vs. 34%, p = 0.005), decreased length of stay, decreased postoperative pain, and improved quality of life at 6 weeks with MIE compared to open esophagectomy [28]. MIE was performed via laparoscopy and thoracoscopy with the patient in the prone position.
8.5. Ivor–Lewis vs. Transhiatal Esophagectomy
The advantages of the Ivor–Lewis approach result from improved transthoracic visualization, which allows for extensive lymph node dissection and a higher lymph node yield [29]. While older studies reported higher rates of pulmonary complications with transthoracic approaches [30], recent studies that are more representative of the modern era with minimally invasive surgery and improved perioperative care have shown results varying from no difference to actually fewer pulmonary complications with transthoracic esophagectomy when compared with transhiatal approaches [29][31].
8.6. Technique for Total Gastrectomy
Total gastrectomy is often performed for Siewert III and possibly Siewert II tumors. In this technique, the greater omentum is separated from the transverse mesocolon, the lesser sac is entered, and the plane is extended proximally and distally. A complete omentectomy may be performed. The right gastroepiploic artery is then identified and divided at its origin from the gastroduodenal artery. The infrapyloric nodal tissue is mobilized with the specimen. The greater curvature of the stomach is further dissected with careful division of the short gastric vessels up to the phrenoesophageal ligament. The lesser curvature is then mobilized. The right gastric artery is identified and divided at its origin from the common hepatic artery. The duodenum is then circumferentially dissected distal to the pylorus and divided. The specimen is reflected anteriorly, and the left gastric artery is identified and divided, taking all nodal tissue. The distal esophagus is mobilized and divided, and reconstruction is performed with a Roux-en-Y esophagojejunostomy [32]. NCCN guidelines recommend the removal of at least 16 lymph nodes with a complete D2 lymph node dissection when performing total gastrectomy for gastric cancer [33]. This involves the removal of perigastric nodal tissue as well as nodal tissue along the named celiac axis vessels, i.e., the left gastric, common hepatic, celiac, and splenic arteries. D2 lymphadenectomy has been shown to have a survival benefit in Eastern studies, but these results have not been replicated in Western trials [34].
8.7. Esophagectomy versus Total Gastrectomy
In Siewert II tumors, clinical practice is variable between esophagectomy, gastrectomy, and, more recently, proximal gastrectomy. Regardless of the approach, an R0 resection is considered an independent predictor of long-term survival [9]. Additionally, a few studies have noted improved survival with a wider margin [35][36]. With this in mind, total gastrectomy poses certain challenges as it is difficult to achieve a proximal margin of more than 3–4 cm on the esophagus.
9. Proximal Gastrectomy
9.1. Rationale
As discussed above, there is variability in the surgical approach chosen for Siewert 2 and 3 GE junction adenocarcinomas, especially Siewert 2. For tumors in the same location, some surgeons will choose to perform esophagectomy, while others choose to perform total gastrectomy (TG). These have traditionally been seen as the two surgical options; however, there is increased interest in and utilization of proximal gastrectomy (PG) as an additional option.
Tumors of the distal stomach are treated with subtotal distal gastrectomy, where the distal 50–60% of the stomach is resected along with appropriate lymphadenectomy and an anastomosis created to the proximal stomach. This is preferred to total gastrectomy due to less weight loss and better functional outcomes with equivalent oncologic outcomes [37][38][39].
9.2. Oncologic Concerns
The first and most important question is whether PG is an oncologically equivalent approach compared to TG for type 2/3 GE junction cancers. In regard to the extent of lymphadenectomy during resection, one study has quantified positivity rates across each lymph node station. A prospective nationwide Japanese study assessed rates of lymph node metastases at abdominal and mediastinal lymph node stations for cancers at the GE junction to determine rates of nodal metastatic disease at each lymph node station [40].
9.3. PG Reconstruction Techniques and Outcomes
While these studies have supported the rationale that PG is at least oncologically equivalent to TG, another concern is functional outcomes and complications. TG has been associated with greater postoperative weight loss as a percentage of body weight (15–20%) than distal subtotal gastrectomy (5–10%) [38]. This is important not only for quality of life but also oncologic outcomes, as studies have shown that greater postoperative weight loss is associated with decreased compliance with adjuvant chemotherapy [41] and early recurrence [42]. Therefore, if PG can be similarly shown to decrease postoperative weight loss and improve quality of life for GE junction cancers compared to TG, then it would support its use in appropriately selected patients.
9.4. Esophagogastric Anastomosis
PG with direct anastomosis between the distal stomach and esophagus (esophagogastrostomy) is the fastest and most straightforward anastomotic technique, with preservation of the normal route of enteral contents through the esophagus, stomach, and into the duodenum. However, the initial experience with this technique had significant functional limitations. PG with esophagogastrostomy is associated with high rates of severe gastroesophageal reflux and resultant reflux esophagitis [43][44][45][46] due to the loss of the lower esophageal sphincter, impaired gastric emptying function of the distal stomach, and preservation of the pylorus.
9.5. Jejunal Interposition and Double Tract Reconstruction
Alternative reconstructions of the esophagogastric anastomosis have been developed. The two most commonly utilized and reported are jejunal interposition and double-tract reconstruction. Both of these reconstructions utilize the jejunum as a conduit between the esophagus and distal gastric remnant.
Jejunal interposition (JI), first described in 1955 by Merendino et al., involves transecting the proximal jejunum about 20–30 cm distal to the ligament of Treitz while maintaining its mesentery and vascular supply. An esophagojejunal anastomosis is then performed, and 10–15 cm distally, a gastrojejunal anastomosis is performed. The jejunum distal to the gastrojejunal anastomosis is transected, and a jejunojejunal anastomosis is then performed to restore continuity of the GI tract [47][48].
9.6. Comparison of PG to TG Outcomes
Multiple studies have compared functional, nutritional, and quality of life outcomes between PG and TG. A randomized controlled trial comparing JI, DTR, and TG found decreased reflux esophagitis rates and improved nutritional parameters in the JI and DTR groups compared to TG in terms of hemoglobin, serum protein, serum albumin, vitamin B12, and weight loss up to 18 months postoperatively [48].
10. Conclusions
GE junction adenocarcinoma is a growing public health concern around the world, with a direct correlation to increasing rates of obesity and GERD. The anatomic location and biological characteristics of these tumors present unique management challenges. Advancements have been made with the incorporation of neoadjuvant therapy and improvements in surgical techniques, including minimally invasive surgery.
References
- Then, E.O.; Lopez, M.; Saleem, S.; Gayam, V.; Sunkara, T.; Culliford, A.; Gaduputi, V. Esophageal Cancer: An Updated Surveillance Epidemiology and End Results Database Analysis. World J. Oncol. 2020, 11, 55–64.
- Buas, M.F.; Vaughan, T.L. Epidemiology and risk factors for gastroesophageal junction tumors: Understanding the rising incidence of this disease. Semin. Radiat. Oncol. 2013, 23, 3–9.
- Arnold, M.; Ferlay, J.; van Berge Henegouwen, M.I.; Soerjomataram, I. Global burden of oesophageal and gastric cancer by histology and subsite in 2018. Gut 2020, 69, 1564–1571.
- Ryan, A.M.; Duong, M.; Healy, L.; Ryan, S.A.; Parekh, N.; Reynolds, J.V.; Power, D.G. Obesity, metabolic syndrome and esophageal adenocarcinoma: Epidemiology, etiology and new targets. Cancer Epidemiol. 2011, 35, 309–319.
- Du, X.; Hidayat, K.; Shi, B.-M. Abdominal obesity and gastroesophageal cancer risk: Systematic review and meta-analysis of prospective studies. Biosci. Rep. 2017, 37, BSR20160474.
- Falk, G.W. Barrett’s esophagus. Gastroenterology 2002, 122, 1569–1591.
- Cameron, A.J.; Lomboy, C.T.; Pera, M.; Carpenter, H.A. Adenocarcinoma of the esophagogastric junction and Barrett’s esophagus. Gastroenterology 1995, 109, 1541–1546.
- Siewert, J.R.; Hölscher, A.H.; Becker, K.; Gössner, W. Cardia cancer: Attempt at a therapeutically relevant classification. Chirurg 1987, 58, 25–32.
- Rüdiger Siewert, J.; Feith, M.; Werner, M.; Stein, H.J. Adenocarcinoma of the esophagogastric junction: Results of surgical therapy based on anatomical/topographic classification in 1002 consecutive patients. Ann. Surg. 2000, 232, 353–361.
- Grotenhuis, B.A.; Wijnhoven, B.P.L.; Poley, J.W.; Hermans, J.J.; Biermann, K.; Spaander, M.C.W.; Bruno, M.J.; Tilanus, H.W.; van Lanschot, J.J.B. Preoperative assessment of tumor location and station-specific lymph node status in patients with adenocarcinoma of the gastroesophageal junction. World J. Surg. 2013, 37, 147–155.
- Reeh, M.; Mina, S.; Bockhorn, M.; Kutup, A.; Nentwich, M.F.; Marx, A.; Sauter, G.; Rösch, T.; Izbicki, J.R.; Bogoevski, D. Staging and outcome depending on surgical treatment in adenocarcinomas of the oesophagogastric junction. Br. J. Surg. 2012, 99, 1406–1414.
- Manabe, N.; Matsueda, K.; Haruma, K. Epidemiological Review of Gastroesophageal Junction Adenocarcinoma in Asian Countries. Digestion 2022, 103, 29–36.
- Barrett, N.R. Chronic peptic ulcer of the oesophagus and “oesophagitis”. Br. J. Surg. 1950, 38, 175–182.
- Quante, M.; Bhagat, G.; Abrams, J.A.; Marache, F.; Good, P.; Lee, M.D.; Lee, Y.; Friedman, R.; Asfaha, S.; Dubeykovskaya, Z.; et al. Bile acid and inflammation activate gastric cardia stem cells in a mouse model of Barrett-like metaplasia. Cancer Cell 2012, 21, 36–51.
- Gotoda, T.; Yanagisawa, A.; Sasako, M.; Ono, H.; Nakanishi, Y.; Shimoda, T.; Kato, Y. Incidence of lymph node metastasis from early gastric cancer: Estimation with a large number of cases at two large centers. Gastric Cancer 2000, 3, 219–225.
- Ajani, J.A.; D’amico, T.A.; Bentrem, D.J.; Cooke, D.; Corvera, C.; Das, P.; Enzinger, P.C.; Enzler, T.; Farjah, F.; Gerdes, H.; et al. Esophageal and Esophagogastric Junction Cancers, Version 2.2023, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 393–422.
- Yamada, M.; Oda, I.; Nonaka, S.; Suzuki, H.; Yoshinaga, S.; Taniguchi, H.; Sekine, S.; Kushima, R.; Saito, Y.; Gotoda, T. Long-term outcome of endoscopic resection of superficial adenocarcinoma of the esophagogastric junction. Endoscopy 2013, 45, 992–996.
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006, 355, 11–20.
- van Hagen, P.; Hulshof, M.C.C.M.; Van Lanschot, J.J.B.; Steyerberg, E.W.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; Richel, D.J.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N. Engl. J. Med. 2012, 366, 2074–2084.
- Al-Batran, S.-E.; Homann, N.; Pauligk, C.; Goetze, T.O.; Meiler, J.; Kasper, S.; Kopp, H.-G.; Mayer, F.; Haag, G.M.; Luley, K.; et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): A randomised, phase 2/3 trial. Lancet 2019, 393, 1948–1957.
- Kelly, R.J.; Ajani, J.A.; Kuzdzal, J.; Zander, T.; Van Cutsem, E.; Piessen, G.; Mendez, G.; Feliciano, J.; Motoyama, S.; Lièvre, A.; et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N. Engl. J. Med. 2021, 384, 1191–1203.
- Bang, Y.-J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010, 376, 687–697.
- Hofheinz, R.D.; Hegewisch-Becker, S.; Kunzmann, V.; Thuss-Patience, P.; Fuchs, M.; Homann, N.; Graeven, U.; Schulte, N.; Merx, K.; Pohl, M.; et al. Trastuzumab in combination with 5-fluorouracil, leucovorin, oxaliplatin and docetaxel as perioperative treatment for patients with human epidermal growth factor receptor 2-positive locally advanced esophagogastric adenocarcinoma: A phase II trial of the Arbeitsgemeinschaft Internistische Onkologie Gastric Cancer Study Group. Int. J. Cancer 2021, 149, 1322–1331.
- Safran, H.P.; Winter, K.; Ilson, D.H.; Wigle, D.; DiPetrillo, T.; Haddock, M.G.; Hong, T.S.; Leichman, L.P.; Rajdev, L.; Resnick, M.; et al. Trastuzumab with trimodality treatment for oesophageal adenocarcinoma with HER2 overexpression (NRG Oncology/RTOG 1010): A multicentre, randomised, phase 3 trial. Lancet Oncol. 2022, 23, 259–269.
- Loo, J.H.; Ng, A.D.R.; Chan, K.S.; Oo, A.M. Outcomes of Intraoperative Pyloric Drainage on Delayed Gastric Emptying Following Esophagectomy: A Systematic Review and Meta-analysis. J. Gastrointest. Surg. 2023, 27, 823–835.
- Nevins, E.J.; Maleyko, I.; Brown, S.T.R.; Nazeer, M.N.M.; Sangheli, A.; Phillips, A.W. Are intra-operative gastric drainage procedures necessary in esophagectomy: A systematic review and meta-analysis. Langenbecks Arch. Surg. 2022, 407, 3287–3295.
- McKeown, K.C. Total three-stage oesophagectomy for cancer of the oesophagus. Br. J. Surg. 1976, 63, 259–262.
- Biere, S.S.A.Y.; Van Berge Henegouwen, M.I.; Maas, K.W.; Bonavina, L.; Rosman, C.; Garcia, J.R.; Gisbertz, S.S.; Klinkenbijl, J.H.G.; Hollmann, M.W.; de Lange, E.S.; et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: A multicentre, open-label, randomised controlled trial. Lancet 2012, 379, 1887–1892.
- Takahashi, C.; Shridhar, R.; Huston, J.; Blinn, P.; Maramara, T.; Meredith, K. Comparative outcomes of transthoracic versus transhiatal esophagectomy. Surgery 2021, 170, 263–270.
- Bolton, J.S.; Sardi, A.; Bowen, J.C.; Ellis, J.K. Transhiatal and transthoracic esophagectomy: A comparative study. J. Surg. Oncol. 1992, 51, 249–253.
- Chu, K.M.; Law, S.Y.; Fok, M.; Wong, J. A prospective randomized comparison of transhiatal and transthoracic resection for lower-third esophageal carcinoma. Am. J. Surg. 1997, 174, 320–324.
- Hawn, M.T. Operative Techniques in Surgery, 2nd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2023.
- Ajani, J.A.; D'Amico, T.A.; Bentrem, D.J.; Chao, J.; Cooke, D.; Corvera, C.; Das, P.; Enzinger, P.C.; Enzler, T.; Fanta, P.; et al. Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 167–192.
- Seevaratnam, R.; Bocicariu, A.; Cardoso, R.; Mahar, A.; Kiss, A.; Helyer, L.; Law, C.; Coburn, N. A meta-analysis of D1 versus D2 lymph node dissection. Gastric Cancer 2012, 15 (Suppl. 1), S60–S69.
- Barbour, A.P.; Rizk, N.P.; Gonen, M.; Tang, L.; Bains, M.S.; Rusch, V.W.; Coit, D.G.; Brennan, M.F. Adenocarcinoma of the gastroesophageal junction: Influence of esophageal resection margin and operative approach on outcome. Ann. Surg. 2007, 246, 1–8.
- Johansson, J.; Djerf, P.; Öberg, S.; Zilling, T.; von Holstein, C.S.; Johnsson, F.; Walther, B. Two different surgical approaches in the treatment of adenocarcinoma at the gastroesophageal junction. World J. Surg. 2008, 32, 1013–1020.
- Bozzetti, F.; Marubini, E.; Bonfanti, G.; Miceli, R.; Piano, C.; Gennari, L. Subtotal versus total gastrectomy for gastric cancer: Five-year survival rates in a multicenter randomized Italian trial. Italian Gastrointestinal Tumor Study Group. Ann. Surg. 1999, 230, 170–178.
- Davis, J.L.; Selby, L.V.; Chou, J.F.; Schattner, M.; Ilson, D.H.; Capanu, M.; Brennan, M.F.; Coit, D.G.; Strong, V.E. Patterns and Predictors of Weight Loss After Gastrectomy for Cancer. Ann. Surg. Oncol. 2016, 23, 1639–1645.
- Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2021 (6th edition). Gastric Cancer 2023, 26, 1–25.
- Kurokawa, Y.; Takeuchi, H.; Doki, Y.; Mine, S.; Terashima, M.; Yasuda, T.; Yoshida, K.; Daiko, H.; Sakuramoto, S.; Yoshikawa, T.; et al. Mapping of Lymph Node Metastasis From Esophagogastric Junction Tumors: A Prospective Nationwide Multicenter Study. Ann. Surg. 2021, 274, 120–127.
- Aoyama, T.; Yoshikawa, T.; Shirai, J.; Hayashi, T.; Yamada, T.; Tsuchida, K.; Hasegawa, S.; Cho, H.; Yukawa, N.; Oshima, T.; et al. Body weight loss after surgery is an independent risk factor for continuation of S-1 adjuvant chemotherapy for gastric cancer. Ann. Surg. Oncol. 2013, 20, 2000–2006.
- Lee, S.E.; Lee, J.H.; Ryu, K.W.; Nam, B.; Kim, C.G.; Park, S.R.; Kook, M.-C.; Kim, Y.-W. Changing pattern of postoperative body weight and its association with recurrence and survival after curative resection for gastric cancer. Hepatogastroenterology 2012, 59, 430–435.
- Hsu, C.P.; Chen, C.Y.; Hsieh, Y.H.; Hsia, J.Y.; Shai, S.E.; Kao, C.H. Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am. J. Gastroenterol. 1997, 92, 1347–1350.
- Tokunaga, M.; Ohyama, S.; Hiki, N.; Hoshino, E.; Nunobe, S.; Fukunaga, T.; Seto, Y.; Yamaguchi, T. Endoscopic evaluation of reflux esophagitis after proximal gastrectomy: Comparison between esophagogastric anastomosis and jejunal interposition. World J. Surg. 2008, 32, 1473–1477.
- Nunobe, S.; Ida, S. Current status of proximal gastrectomy for gastric and esophagogastric junctional cancer: A review. Ann. Gastroenterol. Surg. 2020, 4, 498–504.
- Mochiki, E.; Fukuchi, M.; Ogata, K.; Ohno, T.; Ishida, H.; Kuwano, H. Postoperative functional evaluation of gastric tube after laparoscopic proximal gastrectomy for gastric cancer. Anticancer Res. 2014, 34, 4293–4298.
- Merendino, K.A.; Dillard, D.H. The concept of sphincter substitution by an interposed jejunal segment for anatomic and physiologic abnormalities at the esophagogastric junction; with special reference to reflux esophagitis, cardiospasm and esophageal varices. Ann. Surg. 1955, 142, 486–506.
- Li, Z.; Dong, J.; Huang, Q.; Zhang, W.; Tao, K. Comparison of three digestive tract reconstruction methods for the treatment of Siewert II and III adenocarcinoma of esophagogastric junction: A prospective, randomized controlled study. World J. Surg. Oncol. 2019, 17, 209.
More
Information
Subjects:
Surgery; Gastroenterology & Hepatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
527
Revisions:
2 times
(View History)
Update Date:
21 Feb 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





