
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Peter Schwarzkopf | -- | 2533 | 2024-02-16 10:21:51 | | | |
| 2 | Sirius Huang | Meta information modification | 2533 | 2024-02-17 02:30:35 | | |
Video Upload Options
Brachial plexus blocks at the interscalene level are frequently chosen by physicians and recommended by textbooks for providing regional anesthesia and analgesia to patients scheduled for shoulder surgery. Published data concerning interscalene single-injection or continuous brachial plexus blocks report good analgesic effects. The principle of interscalene catheters is to extend analgesia beyond the duration of the local anesthetic’s effect through continuous infusion, as opposed to a single injection. However, in addition to the recognized beneficial effects of interscalene blocks, whether administered as a single injection or through a catheter, there have been reports of consequences ranging from minor side effects to severe, life-threatening complications.
1. Introduction
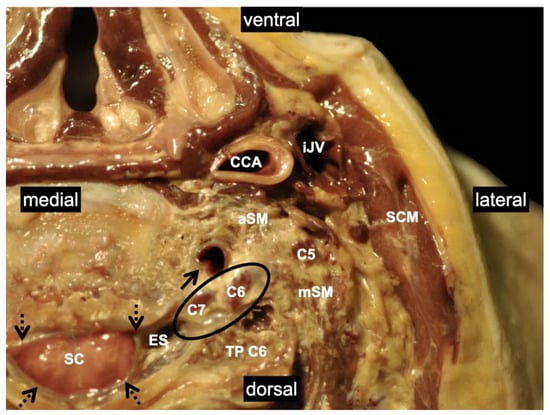
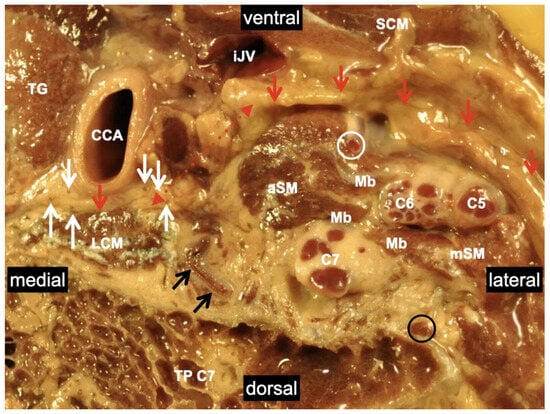
2. Relevant Anatomy for Interscalene Brachial Plexus Blocks
2.1. Innervation and Formation
2.2. Anatomical Variations in the Scalene Gap
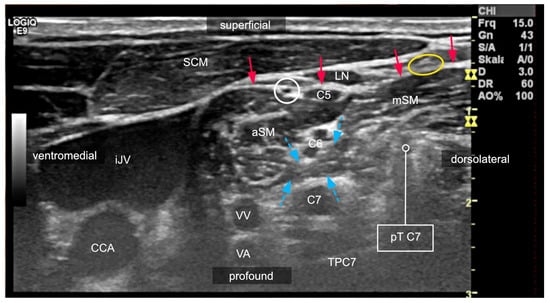
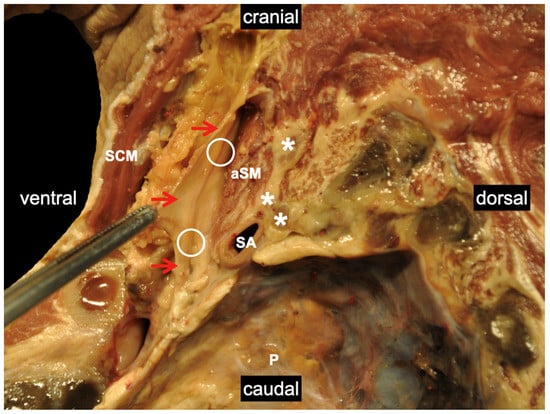
2.3. Variants of the Course of the Ventral Rami
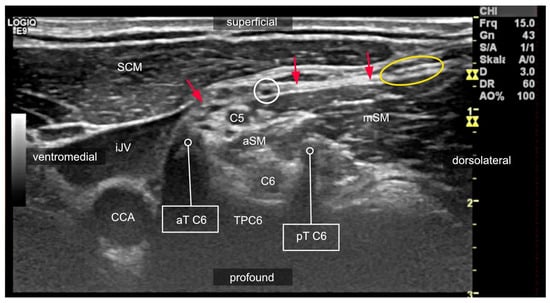
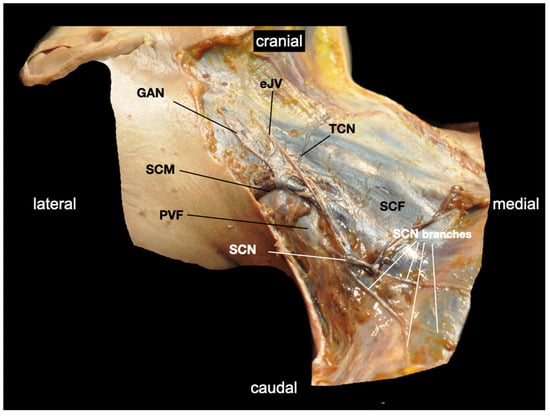
2.4. Compartments of the Lateral Neck and Their Relevance to Side Effects
2.5. Danger Space
2.6. Are Brachial Plexus Blocks Sufficient for Shoulder Surgery?
References
- Ermert, T.; Schnabel, A. Ultrasound in regional anesthesia. Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 2011, 46, 182–187; quiz 188.
- Gaus, P.; Kutz, P.; Bachtler, J.A.; Lindner, R.; Saur, P. Cave: Interscalene catheters. Anaesthesist 2017, 66, 961–968.
- Liu, S.S.; Gordon, M.A.; Shaw, P.M.; Wilfred, S.; Shetty, T.; Yadeau, J.T. A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth. Analg. 2010, 111, 617–623.
- Riazi, S.; Carmichael, N.; Awad, I.; Holtby, R.M.; McCartney, C.J. Effect of local anaesthetic volume (20 vs. 5 mL) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br. J. Anaesth. 2008, 101, 549–556.
- Stundner, O.; Meissnitzer, M.; Brummett, C.M.; Moser, S.; Forstner, R.; Koköfer, A.; Danninger, T.; Gerner, P.; Kirchmair, L.; Fritsch, G. Comparison of tissue distribution, phrenic nerve involvement, and epidural spread in standard- vs. low-volume ultrasound-guided interscalene plexus block using contrast magnetic resonance imaging: A randomized, controlled trial. Br. J. Anaesth. 2016, 116, 405–412.
- Lee, J.H.; Cho, S.H.; Kim, S.H.; Chae, W.S.; Jin, H.C.; Lee, J.S.; Kim, Y.I. Ropivacaine for ultrasound-guided interscalene block: 5 mL provides similar analgesia but less phrenic nerve paralysis than 10 mL. Can. J. Anaesth. 2011, 58, 1001–1006.
- Thackeray, E.M.; Swenson, J.D.; Gertsch, M.C.; Phillips, K.M.; Steele, J.W.; Burks, R.T.; Tashjian, R.Z.; Greis, P.E. Diaphragm function after interscalene brachial plexus block: A double-blind, randomized comparison of 0.25% and 0.125% bupivacaine. J. Shoulder Elb. Surg. 2013, 22, 381–386.
- Wong, A.K.; Keeney, L.G.; Chen, L.; Williams, R.; Liu, J.; Elkassabany, N.M. Effect of Local Anesthetic Concentration (0.2% vs. 0.1% Ropivacaine) on Pulmonary Function, and Analgesia After Ultrasound-Guided Interscalene Brachial Plexus Block: A Randomized Controlled Study. Pain Med. 2016, 17, 2397–2403.
- Palhais, N.; Brull, R.; Kern, C.; Jacot-Guillarmod, A.; Charmoy, A.; Farron, A.; Albrecht, E. Extrafascial injection for interscalene brachial plexus block reduces respiratory complications compared with a conventional intrafascial injection: A randomized, controlled, double-blind trial. Br. J. Anaesth. 2016, 116, 531–537.
- Renes, S.H.; van Geffen, G.J.; Rettig, H.C.; Gielen, M.J.; Scheffer, G.J. Minimum effective volume of local anesthetic for shoulder analgesia by ultrasound-guided block at root C7 with assessment of pulmonary function. Reg. Anesth. Pain Med. 2010, 35, 529–534.
- Siegenthaler, A.; Moriggl, B.; Mlekusch, S.; Schliessbach, J.; Haug, M.; Curatolo, M.; Eichenberger, U. Ultrasound-guided suprascapular nerve block, description of a novel supraclavicular approach. Reg. Anesth. Pain Med. 2012, 37, 325–328.
- Burckett-St Laurent, D.; Chan, V.; Chin, K.J. Refining the ultrasound-guided interscalene brachial plexus block: The superior trunk approach. Can. J. Anaesth. 2014, 61, 1098–1102.
- Karmakar, M.K.; Sala-Blanch, X.; Songthamwat, B.; Tsui, B.C. Benefits of the costoclavicular space for ultrasound-guided infraclavicular brachial plexus block: Description of a costoclavicular approach. Reg. Anesth. Pain Med. 2015, 40, 287–288.
- Tran, D.Q.; Layera, S.; Bravo, D.; Cristi-Sánchez, I.; Bermúdez, L.; Aliste, J. Diaphragm-sparing nerve blocks should spare the diaphragm. Reg. Anesth. Pain Med. 2020, 45, 752–753.
- Hussain, N.; Goldar, G.; Ragina, N.; Banfield, L.; Laffey, J.G.; Abdallah, F.W. Suprascapular and Interscalene Nerve Block for Shoulder Surgery: A Systematic Review and Meta-analysis. Anesthesiology 2017, 127, 998–1013.
- Nöske, E.; Stolzer, M.; Racher, M.; Baumann, H.; Lehmann, K.J.; Henrich, M. Central neurological complication of an interscalene plexus catheter. Anaesthesist 2021, 70, 937–941.
- Spitzer, D.; Wenger, K.J.; Neef, V.; Divé, I.; Schaller-Paule, M.A.; Jahnke, K.; Kell, C.; Foerch, C.; Burger, M.C. Local Anesthetic-Induced Central Nervous System Toxicity during Interscalene Brachial Plexus Block: A Case Series Study of Three Patients. J. Clin. Med. 2021, 10, 1013.
- Benumof, J.L. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology 2000, 93, 1541–1544.
- Walter, M.; Rogalla, P.; Spies, C.; Kox, W.J.; Volk, T. Intrathecal misplacement of an interscalene plexus catheter. Anaesthesist 2005, 54, 215–219.
- Frasca, D.; Clevenot, D.; Jeanny, A.; Laksiri, L.; Petitpas, F.; Debaene, B. Total spinal anesthesia after interscalenic plexus block. Ann. Fr. Anesth. Reanim. 2007, 26, 994–998.
- Gaus, P.; Heb, B.; Tanyay, Z.; Müller-Breitenlohner, H. Epidural malpositioning of an interscalene plexus catheter. Anaesthesist 2011, 60, 850–853.
- Hohner, M.; von Knobelsdorff, G.; Andresen-Streichert, H.; Püschel, K.; Schulz, F. Tödlicher Ausgang einer Katheterfehllage bei Plexusanästhesie. Rechtsmedizin 2013, 23, 38–43.
- Tuominen, M.K.; Pere, P.; Rosenberg, P.H. Unintentional arterial catheterization and bupivacaine toxicity associated with continuous interscalene brachial plexus block. Anesthesiology 1991, 75, 356–358.
- Yanovski, B.; Gaitini, L.; Volodarski, D.; Ben-David, B. Catastrophic complication of an interscalene catheter for continuous peripheral nerve block analgesia. Anaesthesia 2012, 67, 1166–1169.
- Marhofer, D.; Marhofer, P.; Triffterer, L.; Leonhardt, M.; Weber, M.; Zeitlinger, M. Dislocation rates of perineural catheters: A volunteer study. Br. J. Anaesth. 2013, 111, 800–806.
- Maecken, T.; Lohr, D.; Zahn, P.K.; Litz, R.J. Sonographic comparison of two different peripheral nerve catheters for continuous interscalene nerve blocks. EJA 2017, 34 (Suppl. S55), 89.
- Grodinsky, M.; Holyoke, E.A. The fasciae and fascial spaces of the head, neck and adjacent regions. Am. J. Anat. 1938, 63, 367–408.
- Feigl, G.C.; Pixner, T. Combination of variations of the interscalene gap as a pitfall for ultrasound-guided brachial plexus block. Reg. Anesth. Pain Med. 2011, 36, 523–524.
- Feigl, G.C.; Dreu, M. Important structures to be known for a safe ultrasound-guided supraclavicular plexus block. Reg. Anesth. Pain Med. 2010, 35, 317–318.
- Feigl, G.C.; Pixner, T. The cleidoatlanticus muscle: A potential pitfall for the practice of ultrasound guided interscalene brachial plexus block. Surg. Radiol. Anat. 2011, 33, 823–825.
- Hafferl, A. Lehrbuch der Topographischen Anatomie, 3rd ed.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 1969.
- Harry, W.G.; Bennett, J.D.; Guha, S.C. Scalene muscles and the brachial plexus: Anatomical variations and their clinical significance. Clin. Anat. 1997, 10, 250–252.
- Weiglein, A.H.; Moriggl, B.; Schalk, C.; Künzel, K.H.; Müller, U. Arteries in the posterior cervical triangle in man. Clin. Anat. 2005, 18, 553–557.
- Feigl, G.; Hammer, G.P.; Litz, R.; Kachlik, D. The intercarotid or alar fascia, other cervical fascias, and their adjacent spaces—A plea for clarification of cervical fascia and spaces terminology. J. Anat. 2020, 237, 197–207.
- Hafferl, A. (Ed.) Die Anatomie der Pleurakuppel; Springer Verlag GmbH: Berlin/Heidelberg, Germany, 1939.
- Gerbershagen, H.J.; Aduckathil, S.; van Wijck, A.J.; Peelen, L.M.; Kalkman, C.J.; Meissner, W. Pain intensity on the first day after surgery: A prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013, 118, 934–944.
- Aszmann, O.C.; Dellon, A.L.; Birely, B.T.; McFarland, E.G. Innervation of the human shoulder joint and its implications for surgery. Clin. Orthop. Relat. Res. 1996, 330, 202–207.
- Gardner, E. The innervation of the shoulder joint. Anat. Rec. 1948, 102, 1–18.




