Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Guoying Zhou | -- | 2724 | 2024-02-05 11:41:56 | | | |
| 2 | Lindsay Dong | Meta information modification | 2724 | 2024-02-07 02:00:17 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Wang, Y.; Xu, R.; Yan, Y.; He, B.; Miao, C.; Fang, Y.; Wan, H.; Zhou, G. Exosomes-Mediated Signaling Pathway for Organ Ischemia-Reperfusion Injury Treatment. Encyclopedia. Available online: https://encyclopedia.pub/entry/54758 (accessed on 08 February 2026).
Wang Y, Xu R, Yan Y, He B, Miao C, Fang Y, et al. Exosomes-Mediated Signaling Pathway for Organ Ischemia-Reperfusion Injury Treatment. Encyclopedia. Available at: https://encyclopedia.pub/entry/54758. Accessed February 08, 2026.
Wang, Yanying, Ruojiao Xu, Yujia Yan, Binyu He, Chaoyi Miao, Yifeng Fang, Haitong Wan, Guoying Zhou. "Exosomes-Mediated Signaling Pathway for Organ Ischemia-Reperfusion Injury Treatment" Encyclopedia, https://encyclopedia.pub/entry/54758 (accessed February 08, 2026).
Wang, Y., Xu, R., Yan, Y., He, B., Miao, C., Fang, Y., Wan, H., & Zhou, G. (2024, February 05). Exosomes-Mediated Signaling Pathway for Organ Ischemia-Reperfusion Injury Treatment. In Encyclopedia. https://encyclopedia.pub/entry/54758
Wang, Yanying, et al. "Exosomes-Mediated Signaling Pathway for Organ Ischemia-Reperfusion Injury Treatment." Encyclopedia. Web. 05 February, 2024.
Copy Citation
Ischemia reperfusion (I/R) is a common pathological process which occurs mostly in organs like the heart, brain, kidney, and lung. The injury caused by I/R gradually becomes one of the main causes of fatal diseases, which is an urgent clinical problem to be solved. Although great progress has been made in therapeutic methods, including surgical, drug, gene therapy, and transplant therapy for I/R injury, the development of effective methods to cure the injury remains a worldwide challenge.
ischemia-reperfusion
exosomes
signaling pathway
reperfusion injury
1. Introduction
1.1. Overview of Ischemia-Reperfusion Injury
Ischemia-reperfusion (I/R) injury is a pathological process that can occur in many organs of the human body, accompanied by severe cell damage and inflammatory reactions [1]. In recent years, it has become one of the most common causes of disability and death worldwide [2]. There is a lot of evidence that tissue damage is caused not by ischemia itself, but by the sudden resumption of blood supply after a period of ischemia [3]. Organ ischemia-reperfusion injury often occurs in traumatic shock, surgery, organ transplantation, burns, and other blood circulation disorders [4]. The main organs involved in vascular reperfusion injury are the heart, brain, liver, and kidney, and it can also induce systemic inflammation and eventually lead to multiple organ failure [5]. However, not all organs with ischemia will have I/R injury after blood flow recovery, and many factors can affect its occurrence and severity. For example, if the ischemia time is short, or collateral circulation is easy to form after ischemia, there may be no significant reperfusion injury after the restoration of blood supply. Because oxygen readily accepts electrons and forms oxygen free radicals, organs with a high oxygen demand are more prone to reperfusion injury [6]. In addition, appropriately reducing the temperature and pH value of the perfusion solution and reducing the content of Ca2+ and Na+ in the perfusion solution are conducive to alleviating the reperfusion injury [7]. The pathogenesis of organ I/R injury is summarized in Figure 1.
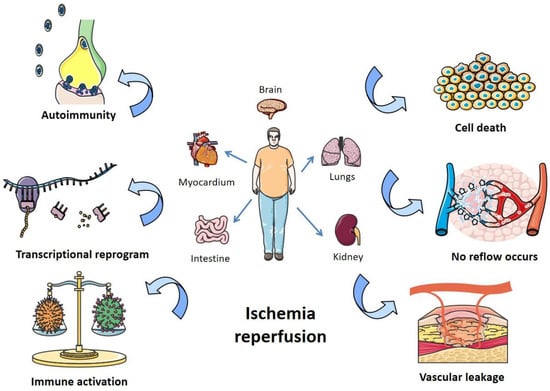
Figure 1. Pathogenesis of organ I/R injury. I/R damages organs like the heart, lungs, kidneys, and intestines, mainly by affecting autoimmunity, transcriptional recoding, immune activation, apoptosis, blocking blood return, and vascular leakage.
1.2. Occurrence and Mechanism of Ischemia-Reperfusion Injury
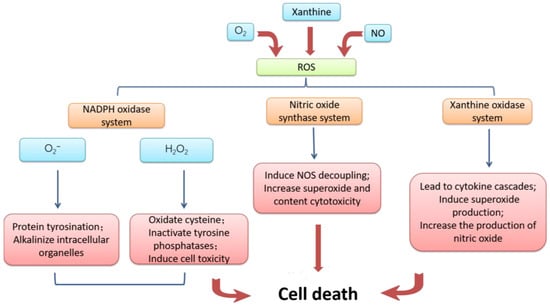
The mechanism of ischemia-reperfusion injury is complex, and the following four aspects are mainly responsible. First of all, the damage to microvessels and parenchymal organs caused by ischemic tissue reperfusion is mainly caused by oxidative stress [8]. Ischemia leads to an inadequate supply of oxygen and nutrients, and cells are unable to produce enough energy. When reperfusion occurs, the sudden supply of oxygen and nutrients increases the degree of oxidative stress within the cell, resulting in the production of excessive reactive oxygen species and other oxidizing substances [9]. The mechanism of cell apoptosis accelerated by massive reactive oxygen is summarized in Figure 2. The synthesis ability of antioxidant enzymes that can scavenge free radicals in ischemic tissue is greatly weakened, and the strong oxidation effect directly damages vascular endothelial cells and tissue cells, thus exacerbating the damage of free radicals to the tissue after I/R [10].
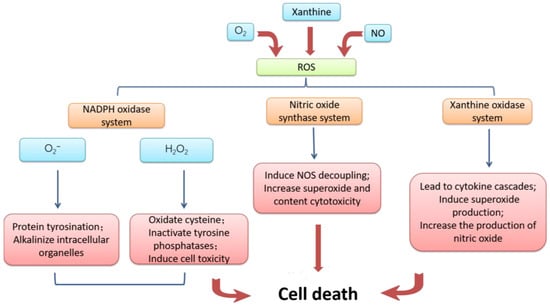
Figure 2. Mechanism of cell damage induced by reactive oxygen species. Excessive accumulation of reactive oxygen caused by I/R and conversion to NADPH oxidase, nitric oxide synthase inhibitor, and xanthine oxidase resulting in cell apoptosis.
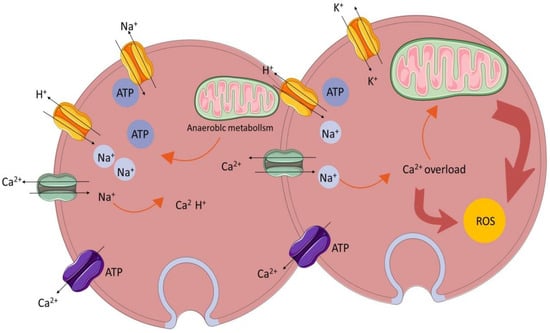
The homeostasis and regulation of the calcium ion concentration in and outside cells are important conditions for maintaining cell function [11]. Calcium overload is the phenomenon of an abnormal intracellular calcium ion concentration leading to structural damage and dysfunction in the functional metabolism [12]. The mechanism of calcium overload is summarized in Figure 3. When I/R injury occurs, the local intracellular calcium ion concentration increases significantly, resulting in the disturbance of calcium ion homeostasis and an insufficient mitochondrial oxidation capacity [13], thus activating phospholipase to damage other organelles or activating calcium-dependent protease activity, as well as increasing the production of oxygen free radicals [14].
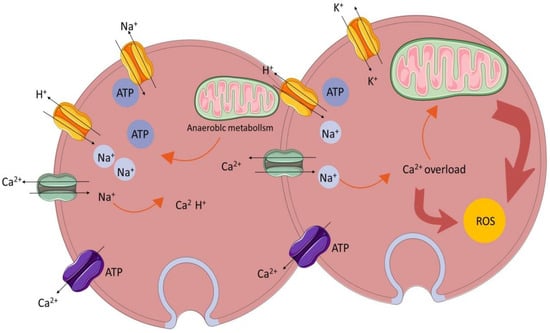
Figure 3. Calcium overload.
In addition, inflammatory responses and immune cell activation also play important roles in the occurrence of ischemia-reperfusion injury [15]. During reperfusion, under the influence of excessive oxidizing substances, immune cells release a large number of inflammatory mediators, causing cell damage in the surrounding tissue [16]. Meanwhile, a large number of free radicals and lysosomal enzymes released by white blood cells make the vascular endothelial cells swell, the microvascular diameter narrow, and permeability increase, meaning that reperfusion blood flow cannot be re-routed [17].
1.3. Current Therapeutic Strategies for Ischemia-Reperfusion Injury
Therefore, reducing inflammation, scavenging free radicals, maintaining calcium homeostasis, and antioxidant therapy are the keys to reducing ischemia-reperfusion injury. In recent years, more and more medical interventions and strategies have been actively applied to minimize I/R injury. However, due to the complex pathologic factors of I/R injury, traditional treatment strategies such as blood pressure control, detumescence, and dehydration are of limited effectiveness [18][19]. Recently, advanced therapies such as ischemic preconditioning, ischemic post-treatment, antioxidant, hypothermia, and stem cell therapy have emerged as potential treatments for I/R injury [20]. Ischemic preconditioning (IPC) is considered as an effective treatment strategy for central nervous system diseases. It causes transient ischemia and the reperfusion of organs or tissues through drugs, intermittent blood flow blockade, and other methods, with the aim of inducing adaptive changes in cells and improving tolerance to subsequent, more severe I/R events [21]. Similar to preconditioning, ischemic posttreatment aims to reduce the harmful effects of reperfusion by activating protective signaling pathways and reducing apoptosis [22]. Several drugs and compounds have shown promise in reducing I/R injury. These include antioxidants (vitamin C), anti-inflammatory agents (corticosteroids), and mitochondrial protectors (CoQ10), which are used to reduce oxidative stress and maintain mitochondrial function [23]. Cooling damaged tissues or organs can slow metabolic processes and reduce oxygen and energy consumption, thus reducing tissue damage. Hypothermia therapy has been shown to be beneficial in reducing I/R injury, especially in the brain and heart [24].
Cell therapy is a new approach to the treatment of ischemia-reperfusion injury, and its effects are constantly being studied and explored. Stem cells can promote the healing of I/R injury by repairing tissue cell damage and stimulating the body’s own cell regeneration, secreting vascular growth factors to improve blood supply and releasing apoptosis inhibitors to reduce the occurrence of apoptosis [25].
1.4. Exosomes Mediate Organ Ischemia-Reperfusion Injury through Different Signaling Pathways
Exosomes are vesicles between 40 nm and 160 nm in diameter that are released into the blood from cells. Exosomes released into cells can participate in immune response, cell migration, cell differentiation, antigen presentation, and other processes [26]. Exosomes play an important role in cell communication, transporting proteins, mRNA, lipids, and other exogenous substances to recipient cells and even crossing the blood–brain barrier (BBB) [27]. On the other hand, exosomes play a compelling role in immune response. Exosomes can induce different signaling pathways through microRNAs (miRNAs) carried by them or ligands existing on the surface to play a role in promoting tissue repair and regeneration, alleviating inflammation, and alleviating organ damage [28]. More and more evidence shows that the bioactive substances carried by exosomes reflect the state of the disease, making them a marker for the diagnosis of hypoxic diseases [29].
The signaling pathway refers to a series of enzymatic reaction pathways that can transmit extracellular molecular signals through the cell membrane to exert effects in cells. Hormones, neurotransmitters, and other extracellular biological signals are perceived by their receptors and transformed into intracellular signals, which are then amplified and regulated by signal cascades, and finally produce a series of comprehensive cellular responses [30]. Once released, exosomes send signals to other cells to mediate intercellular communication in three ways: First, exosome membrane proteins can bind to receptors on their target cell membranes, activating signaling pathways in their target cells. Second, exosome membrane proteins are cleaved by proteases in the extracellular matrix and then bind to receptors on the target cell membrane, thereby activating intracellular signaling pathways. Third, exosomes can directly fuse with target cell membranes to regulate cell signaling through the non-selective release of proteins and miRNAs [31]. There is increasing evidence that exosomes regulate ischemia-reperfusion injury healing in organs through different signaling pathways.
2. The Signaling Pathway of Exosomes in Promoting Organ Ischemia-Reperfusion Injury Recovery
2.1. PI3K/Akt Signaling Pathway
The PI3K/Akt pathway consists of phosphatidylinositol-3-kinase (PI3K) and the serine/threonine kinase Akt (also known as protein kinase B or PKB), activated by receptor tyrosine kinase and cytokine receptors [32]. The pathway can reduce the degree of cell damage and promote cell survival by reducing the expression of inflammatory factors [33]. In addition, PI3K/Akt can activate nitric oxide synthase to push the production and removal of oxygen free radicals in the body into a dynamic equilibrium state [34].
Recent studies have shown that some factors involved in the PI3K/Akt signaling pathway also contribute to the treatment of ischemia-reperfusion injury. It can reduce apoptosis by regulating apoptosis-related proteins and inhibiting the activation of apoptosis pathways. In addition, Akt activation can inhibit inflammatory responses and oxidative stress and reduce cell damage [35]. Chen et al. showed that Danhong Injection can protect the nerves of rats with I/R injury by activating the PI3K/Akt signaling pathway [36]. Moreover, methyleugenol mediates the PI3K/Akt pathway, which acts on injured hepatocytes in vitro and in vivo to promote cell survival and relieve LiRI-induced liver injury and inflammation [37]. Exosomes from different types of cells play an important role in the treatment of ischemia-reperfusion injury in different organs through the PI3K/Akt regulatory pathway.
2.2. NF-κB Signaling Pathway
Nuclear factor kappa-B (NF-κB) protein is an important nuclear transcription factor, which plays an important role in physiological and pathological processes such as inflammation and immunity [38]. In ischemia-reperfusion injury, the role of different signaling pathways may vary depending on specific conditions and tissue types. However, the NF-κB signaling pathway is generally considered to be one of the most important.
As a typical pro-inflammatory signaling pathway, NF-κB is involved in the release of pro-inflammatory cytokines, chemokines, and adhesion molecules [39], and its activation has been widely observed in the pathological processes associated with I/R injury. For instance, physcion protects neuronal cells from I/R damage by reducing oxidative stress and inflammation levels in vitro and in vivo by inhibiting the NF-kB pathway [40]. However, too mild or too severe of an inflammatory response is not conducive to injury recovery [41]. Therefore, binding exosomes to regulate the function of the NF-κB pathway and inhibit or promote inflammatory responses may be a novel approach to ameliorate organ ischemia-reperfusion injury.
2.3. Nrf2 Signaling Pathway
The nuclear factor erythroid 2-related factor 2 (Nrf2) belongs to the Cap-n-Coll family of basic leucine zipper proteins. It is an important transcription factor regulating the cellular oxidative stress response as well as a central regulator of cellular redox homeostasis [42]. The imbalance between free radicals and antioxidants in the body may lead to excessive production of reactive oxygen species (ROS), which, in turn, aggravates cell damage and inflammation in patients with ischemia-reperfusion injury [43]. This pathway can regulate the expression of antioxidant proteins, reduce the damage of reactive oxygen species and electrophilic reagents to cells, and maintain the body’s REDOX homeostasis, which is considered to be the most promising signaling pathway in the clinical improvement of ischemia-reperfusion injury [44].
2.4. PTEN Signaling Pathway
Phosphatase and Tensin Homolog deleted on Chromosome 10 (PTEN) is a tumor suppressor with growth and survival regulatory functions. In recent years, it has been found that PTEN can participate in cell proliferation, energy metabolism, and other cellular activities as a metabolic regulator [45]. PTEN can inhibit the activation of downstream proteins of the PI3K pathway by reducing the level of phosphatidylinositol 3-phosphate (PIP3) in cells. It plays an important role in inhibiting many biological processes such as inflammation and apoptosis caused by I/R injury [46]. Studies have shown that mitochondria play an important role between the PTEN signaling pathway and I/R injury. The increase in mitochondrial autophagy mediated by PTEN-induced enzymes can reduce I/R injury and induce an inflammatory response to a certain extent, providing a new idea for the treatment of organ ischemia-reperfusion injury [47]. A variety of miRNAs carried by different exosomes derived from various stem cells can target the expression of the PTEN signaling pathway, which provides a variety of methods for the treatment of organ ischemia-reperfusion injury.
2.5. Wnt Signaling Pathway
The wingless/Integrated (Wnt) signaling pathway is highly conserved in invertebrates and vertebrates [48]. It plays a vital role in cell growth, proliferation, differentiation, and homeostasis [49]. The Wnt signaling pathway is a complex regulatory system that consists of three branches: the classical Wnt signaling pathway, the Wnt/planar cell polarity (PCP) pathway, and the Wnt/Ca2+ pathway. Among them, the classical Wnt signaling pathway activated by β-catenin is most closely related to the treatment of ischemia-reperfusion injury [50]. Lithium has been shown to alleviate BBB destruction after cerebral I/R in mice by up-regulating endothelial Wnt/β-catenin signaling [51]. Clearly, this pathway plays a significant role in the inhibition of apoptosis, which is involved in the regulation of protein levels, cell migration, and other processes closely related to the treatment of organ I/R injury [52].
2.6. MAPK Signaling Pathway
Mitogen-activated protein kinase (MAPK) is a group of serine/threonine protein kinases that can be activated by different extracellular stimulation. It is involved in many biological processes such as apoptosis, hormone signal transduction, and the regulation of inflammatory factors [53]. It has been confirmed that MAPK genes can be divided into three major subfamilies, namely extracellular-signal-regulated kinases (ERKs), the p38 MAPKs, and Jun N-terminal kinases (JNKs) [54].
The MAPK pathway is involved in a variety of biological processes, such as protecting nerve cells and inhibiting inflammatory response, which is of great significance for ameliorating brain I/R injury [55]. Huang et al. found that curcumin can inhibit the MAPK/p38 pathway, effectively reduce NLR family pyrin domain containing 1 (NLRP1)-dependent neuronal pyroptosis, and thus play a neuroprotective role in cerebral I/R injury [56]. In addition, studies have shown that the inflammation of ischemia-reperfusion injury can be alleviated by reducing the expression levels of phosphorylated p38, ERK, and JNK [57].
2.7. Toll-Like Receptor-Mediated Signaling Pathway
Toll-like receptors (TLRs) are well known for their general effects in non-specific immunity. Initially, TLRs were discovered in developmental studies, and as research progressed, TLRS were known to regulate cellular communication and signaling in synapses [58]. Expressed TLRs can be released by host cells and activate various intracellular pathways, leading to the production of pro-inflammatory cytokines and the expression of costimulatory molecules, so as to prevent pathogen invasion and damage to the human body [59].
The Toll-like receptor-mediated signaling pathway has been identified as one of the signaling pathways involved in the inflammatory response in ischemia-reperfusion injury [60]. In the treatment of I/R injury, various active substances carried by exosomes from various cell sources can be combined with TLR to alleviate I/R injury. TLR2 has been reported to promote the release of interleukin-10 from macrophages to regulate the levels of inflammatory cytokines in I/R injury [61]. Furthermore, TLR9, as a key receptor for unmethylated CpG motifs in mitochondrial DNA, regulates the occurrence of inflammatory responses [62]. Blocking the TLR-mediated signaling pathway can improve myocardial I/R injury and reduce infarct size, which may be a new target for the treatment of organ ischemia-reperfusion injury [63].
2.8. AMPK Signaling Pathway
AMPK (Adenosine 5′-monophosphate activated protein kinase) is a key molecule in the regulation of biological energy metabolism. It is expressed in a variety of metabolically related organs and can be activated by various types of stimulation, including cell movement, hormones, and substances that affect cell metabolism [64]. The AMPK pathway is a pleiotropic signaling pathway involved in many processes, such as regulating lipid metabolism and glucose metabolism, maintaining mitochondrial function stability, and cell energy homeostasis [65]. In addition, it positively regulates intracellular ATP supply, reduces energy consumption, and enhances autophagy, which is considered to be a key therapeutic target for the treatment of organ ischemia-reperfusion injury [66].
AMPK activation reduces oxidant-induced injury in I/R Injury by promoting autophagy, inhibiting apoptosis, and up-regulating the antioxidant enzyme system [67]. HBMSC-derived exosomes decrease caspase 1 and interleukin-1β levels and increase the number of autophagosomes and autolysosomes by activating the AMPK pathway. At the same time, the pyrodeath process mediated by leucine-rich NLRP3 inflammasome is weakened, thereby protecting PC12 cells from ischemia-reperfusion injury [68].
2.9. Cross-Talk between Different Signaling Pathways
In addition to treating organ I/R damage through the above exosome-mediated signaling pathways, exosomes can also act on I/R damage by regulating the cross-talk between different signaling pathways.
References
- Liu, Y.; Li, L.; Wang, Z.; Zhang, J.; Zhou, Z. Myocardial ischemia-reperfusion injury; Molecular mechanisms and prevention. Microvasc. Res. 2023, 149, 104565.
- Shi, Y.J.; Sun, L.L.; Ji, X.; Shi, R.; Xu, F.; Gu, J.H. Neuroprotective effects of oleanolic acid against cerebral ischemia-reperfusion injury in mice. Exp. Neurol. 2021, 343, 113785.
- Zheng, T.; Jiang, T.; Huang, Z.; Ma, H.; Wang, M. Role of traditional Chinese medicine monomers in cerebral ischemia/reperfusion injury: A review of the mechanism. Front. Pharmacol. 2023, 14, 1220862.
- Fan, L.; Zhou, L. AG490 protects cerebral ischemia/reperfusion injury via inhibiting the JAK2/3 signaling pathway. Brain Behav. 2021, 11, e01911.
- Ikhlas, M.; Atherton, N.S. Vascular Reperfusion Injury. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022.
- Fan, Z.; Cai, L.; Wang, S.; Wang, J.; Chen, B. Baicalin Prevents Myocardial Ischemia/Reperfusion Injury Through Inhibiting ACSL4 Mediated Ferroptosis. Front. Pharmacol. 2021, 12, 628988.
- Jiménez-Castro, M.B.; Cornide-Petronio, M.E.; Gracia-Sancho, J.; Peralta, C. Inflammasome-Mediated Inflammation in Liver Ischemia-Reperfusion Injury. Cells 2019, 8, 1131.
- Algoet, M.; Janssens, S.; Himmelreich, U.; Gsell, W.; Pusovnik, M.; Van den Eynde, J.; Oosterlinck, W. Myocardial ischemia-reperfusion injury and the influence of inflammation. Trends Cardiovasc. Med. 2023, 33, 357–366.
- Nørgård, M.; Svenningsen, P. Acute Kidney Injury by Ischemia/Reperfusion and Extracellular Vesicles. Int. J. Mol. Sci. 2023, 24, 15312.
- Tao, H.; Dong, L.; Shan, X.; Li, L.; Chen, H. MicroRNA-32-3p facilitates cerebral ischemia/reperfusion injury through inhibiting Cab39/AMPK. Int. Immunopharmacol. 2023, 121, 110504.
- Wang, R.; Wang, M.; Zhou, J.; Dai, Z.; Sun, G.; Sun, X. Calenduloside E suppresses calcium overload by promoting the interaction between L-type calcium channels and Bcl2-associated athanogene 3 to alleviate myocardial ischemia/reperfusion injury. J. Adv. Res. 2021, 34, 173–186.
- Ye, J.; Wang, R.; Wang, M.; Fu, J.; Zhang, Q.; Sun, G.; Sun, X. Hydroxysafflor Yellow A Ameliorates Myocardial Ischemia/Reperfusion Injury by Suppressing Calcium Overload and Apoptosis. Oxidative Med. Cell. Longev. 2021, 2021, 6643615.
- Zheng, X.; Li, J.; Fan, Q.; Zhao, X.; Chen, K. Dexmedetomidine alleviates myocardial ischemia/reperfusion-induced injury and Ca(2+) overload via the microRNA-346-3p/CaMKIId axis. Int. J. Cardiol. 2021, 338, 185–195.
- Tu, C.C.; Wan, B.Y.; Zeng, Y. STIM2 knockdown protects against ischemia/reperfusion injury through reducing mitochondrial calcium overload and preserving mitochondrial function. Life Sci. 2020, 247, 116560.
- Li, S.; Chen, J.; Liu, M.; Chen, Y.; Wu, Y.; Li, Q.; Ma, T.; Gao, J.; Xia, Y.; Fan, M.; et al. Protective effect of HINT2 on mitochondrial function via repressing MCU complex activation attenuates cardiac microvascular ischemia-reperfusion injury. Basic. Res. Cardiol. 2021, 116, 65.
- Francisco, J.; Del Re, D.P. Inflammation in Myocardial Ischemia/Reperfusion Injury: Underlying Mechanisms and Therapeutic Potential. Antioxidants 2023, 12, 1944.
- Franke, M.; Bieber, M.; Kraft, P.; Weber, A.N.R.; Stoll, G.; Schuhmann, M.K. The NLRP3 inflammasome drives inflammation in ischemia/reperfusion injury after transient middle cerebral artery occlusion in mice. Brain Behav. Immun. 2021, 92, 223–233.
- Necsoiu, C.; Jordan, B.S.; Choi, J.H.; Moon, J.J.; Espinoza, M.D.; Gremmer, B.J.; Batchinsky, A.I.; Cancio, L.C. Mitigating Ischemia-Reperfusion Injury Using a Bilobed Partial REBOA Catheter: Controlled Lower-Body Hypotension. Shock 2021, 55, 396–406.
- Charles, E.J.; Tian, Y.; Zhang, A.; Wu, D.; Mehaffey, J.H.; Gigliotti, J.C.; Klibanov, A.L.; Kron, I.L.; Yang, Z. Pulsed ultrasound attenuates the hyperglycemic exacerbation of myocardial ischemia-reperfusion injury. J. Thorac. Cardiovasc. Surg. 2021, 161, e297–e306.
- Li, X.; Ou, W.; Xie, M.; Yang, J.; Li, Q.; Li, T. Nanomedicine-Based Therapeutics for Myocardial Ischemic/Reperfusion Injury. Adv. Healthc. Mater. 2023, 12, e2300161.
- Liu, J.; Gu, Y.; Guo, M.; Ji, X. Neuroprotective effects and mechanisms of ischemic/hypoxic preconditioning on neurological diseases. CNS Neurosci. Ther. 2021, 27, 869–882.
- Lou, J.; Wang, X.; Zhang, H.; Yu, G.; Ding, J.; Zhu, X.; Li, Y.; Wu, Y.; Xu, H.; Xu, H.; et al. Inhibition of PLA2G4E/cPLA2 promotes survival of random skin flaps by alleviating Lysosomal membrane permeabilization-Induced necroptosis. Autophagy 2022, 18, 1841–1863.
- Mu, J.; Li, C.; Shi, Y.; Liu, G.; Zou, J.; Zhang, D.Y.; Jiang, C.; Wang, X.; He, L.; Huang, P.; et al. Protective effect of platinum nano-antioxidant and nitric oxide against hepatic ischemia-reperfusion injury. Nat. Commun. 2022, 13, 2513.
- Eskla, K.L.; Vellama, H.; Tarve, L.; Eichelmann, H.; Jagomäe, T.; Porosk, R.; Oja, V.; Rämma, H.; Peet, N.; Laisk, A.; et al. Hypothermia Alleviates Reductive Stress, a Root Cause of Ischemia Reperfusion Injury. Int. J. Mol. Sci. 2022, 23, 10108.
- Ziegler, M.; Haigh, K.; Nguyen, T.; Wang, X.; Lim, B.; Yap, M.L.; Eddy, E.M.; Haigh, J.J.; Peter, K. The pulmonary microvasculature entraps induced vascular progenitor cells (iVPCs) systemically delivered after cardiac ischemia-reperfusion injury: Indication for preservation of heart function via paracrine effects beyond engraftment. Microcirculation 2019, 26, e12493.
- Hade, M.D.; Suire, C.N.; Suo, Z. Mesenchymal Stem Cell-Derived Exosomes: Applications in Regenerative Medicine. Cells 2021, 10, 1959.
- Liang, Y.; Duan, L.; Lu, J.; Xia, J. Engineering exosomes for targeted drug delivery. Theranostics 2021, 11, 3183–3195.
- Gao, L.; Qiu, F.; Cao, H.; Li, H.; Dai, G.; Ma, T.; Gong, Y.; Luo, W.; Zhu, D.; Qiu, Z.; et al. Therapeutic delivery of microRNA-125a-5p oligonucleotides improves recovery from myocardial ischemia/reperfusion injury in mice and swine. Theranostics 2023, 13, 685–703.
- Chang, C.; Cai, R.P.; Su, Y.M.; Wu, Q.; Su, Q. Mesenchymal Stem Cell-Derived Exosomal Noncoding RNAs as Alternative Treatments for Myocardial Ischemia-Reperfusion Injury: Current Status and Future Perspectives. J. Cardiovasc. Transl. Res. 2023, 16, 1085–1098.
- Xin, P.; Xu, X.; Deng, C.; Liu, S.; Wang, Y.; Zhou, X.; Ma, H.; Wei, D.; Sun, S. The role of JAK/STAT signaling pathway and its inhibitors in diseases. Int. Immunopharmacol. 2020, 80, 106210.
- Liu, X.; Wang, L.; Ma, C.; Wang, G.; Zhang, Y.; Sun, S. Exosomes derived from platelet-rich plasma present a novel potential in alleviating knee osteoarthritis by promoting proliferation and inhibiting apoptosis of chondrocyte via Wnt/β-catenin signaling pathway. J. Orthop. Surg. Res. 2019, 14, 470.
- Xu, F.; Na, L.; Li, Y.; Chen, L. Roles of the PI3K/AKT/mTOR signalling pathways in neurodegenerative diseases and tumours. Cell Biosci. 2020, 10, 54.
- Glaviano, A.; Foo, A.S.C.; Lam, H.Y.; Yap, K.C.H.; Jacot, W.; Jones, R.H.; Eng, H.; Nair, M.G.; Makvandi, P.; Geoerger, B.; et al. PI3K/AKT/mTOR signaling transduction pathway and targeted therapies in cancer. Mol. Cancer 2023, 22, 138.
- Deng, R.M.; Zhou, J. The role of PI3K/AKT signaling pathway in myocardial ischemia-reperfusion injury. Int. Immunopharmacol. 2023, 123, 110714.
- Ruan, C.; Guo, H.; Gao, J.; Wang, Y.; Liu, Z.; Yan, J.; Li, X.; Lv, H. Neuroprotective effects of metformin on cerebral ischemia-reperfusion injury by regulating PI3K/Akt pathway. Brain Behav. 2021, 11, e2335.
- Feng, C.; Wan, H.; Zhang, Y.; Yu, L.; Shao, C.; He, Y.; Wan, H.; Jin, W. Neuroprotective Effect of Danhong Injection on Cerebral Ischemia-Reperfusion Injury in Rats by Activation of the PI3K-Akt Pathway. Front. Pharmacol. 2020, 11, 298.
- Wang, M.; Zhang, J.; Zhang, J.; Sun, K.; Li, Q.; Kuang, B.; Wang, M.M.Z.; Hou, S.; Gong, N. Methyl eugenol attenuates liver ischemia reperfusion injury via activating PI3K/Akt signaling. Int. Immunopharmacol. 2021, 99, 108023.
- Oh, A.; Pardo, M.; Rodriguez, A.; Yu, C.; Nguyen, L.; Liang, O.; Chorzalska, A.; Dubielecka, P.M. NF-κB signaling in neoplastic transition from epithelial to mesenchymal phenotype. Cell Commun. Signal. CCS 2023, 21, 291.
- Dong, P.; Liu, K.; Han, H. The Role of NF-κB in Myocardial Ischemia/Reperfusion Injury. Curr. Protein Pept. Sci. 2022, 23, 535–547.
- Dong, X.; Wang, L.; Song, G.; Cai, X.; Wang, W.; Chen, J.; Wang, G. Physcion Protects Rats Against Cerebral Ischemia-Reperfusion Injury via Inhibition of TLR4/NF-kB Signaling Pathway. Drug Des. Dev. Ther. 2021, 15, 277–287.
- Li, M.; Hou, Q.; Zhong, L.; Zhao, Y.; Fu, X. Macrophage Related Chronic Inflammation in Non-Healing Wounds. Front. Immunol. 2021, 12, 681710.
- Lin, L.; Wu, Q.; Lu, F.; Lei, J.; Zhou, Y.; Liu, Y.; Zhu, N.; Yu, Y.; Ning, Z.; She, T.; et al. Nrf2 signaling pathway: Current status and potential therapeutic targetable role in human cancers. Front. Oncol. 2023, 13, 1184079.
- Li, B.; Wang, Y.; Jiang, X.; Du, H.; Shi, Y.; Xiu, M.; Liu, Y.; He, J. Natural products targeting Nrf2/ARE signaling pathway in the treatment of inflammatory bowel disease. Biomed. Pharmacother. 2023, 164, 114950.
- Ucar, B.I.; Ucar, G.; Saha, S.; Buttari, B.; Profumo, E.; Saso, L. Pharmacological Protection against Ischemia-Reperfusion Injury by Regulating the Nrf2-Keap1-ARE Signaling Pathway. Antioxidants 2021, 10, 823.
- Cui, X.; Liu, X.; Kong, P.; Du, T.; Li, T.; Yang, G.; Zhang, W.; Jing, X.; Wang, W. PTEN inhibitor VO-OHpic protects endplate chondrocytes against apoptosis and calcification via activating Nrf-2 signaling pathway. Aging 2023, 15, 2275–2292.
- Jiang, T.Y.; Shi, Y.Y.; Cui, X.W.; Pan, Y.F.; Lin, Y.K.; Feng, X.F.; Ding, Z.W.; Yang, C.; Tan, Y.X.; Dong, L.W.; et al. PTEN Deficiency Facilitates Exosome Secretion and Metastasis in Cholangiocarcinoma by Impairing TFEB-mediated Lysosome Biogenesis. Gastroenterology 2023, 164, 424–438.
- Xu, Y.; Tang, Y.; Lu, J.; Zhang, W.; Zhu, Y.; Zhang, S.; Ma, G.; Jiang, P.; Zhang, W. PINK1-mediated mitophagy protects against hepatic ischemia/reperfusion injury by restraining NLRP3 inflammasome activation. Free Radic. Biol. Med. 2020, 160, 871–886.
- Xu, X.; Zhang, M.; Xu, F.; Jiang, S. Wnt signaling in breast cancer: Biological mechanisms, challenges and opportunities. Mol. Cancer 2020, 19, 165.
- Ma, Q.; Yu, J.; Zhang, X.; Wu, X.; Deng, G. Wnt/β-catenin signaling pathway-a versatile player in apoptosis and autophagy. Biochimie 2023, 211, 57–67.
- Liu, J.; Xiao, Q.; Xiao, J.; Niu, C.; Li, Y.; Zhang, X.; Zhou, Z.; Shu, G.; Yin, G. Wnt/β-catenin signalling: Function, biological mechanisms, and therapeutic opportunities. Signal Transduct. Target. Ther. 2022, 7, 3.
- Ji, Y.B.; Gao, Q.; Tan, X.X.; Huang, X.W.; Ma, Y.Z.; Fang, C.; Wang, S.N.; Qiu, L.H.; Cheng, Y.X.; Guo, F.Y.; et al. Lithium alleviates blood-brain barrier breakdown after cerebral ischemia and reperfusion by upregulating endothelial Wnt/β-catenin signaling in mice. Neuropharmacology 2021, 186, 108474.
- Zhao, H.; Ming, T.; Tang, S.; Ren, S.; Yang, H.; Liu, M.; Tao, Q.; Xu, H. Wnt signaling in colorectal cancer: Pathogenic role and therapeutic target. Mol. Cancer 2022, 21, 144.
- Ma, Y.; Nicolet, J. Specificity models in MAPK cascade signaling. FEBS Open Bio 2023, 13, 1177–1192.
- Qi, X.M.; Chen, G. p38γ MAPK Inflammatory and Metabolic Signaling in Physiology and Disease. Cells 2023, 12, 1674.
- Xu, D.; Kong, T.; Shao, Z.; Liu, M.; Zhang, R.; Zhang, S.; Kong, Q.; Chen, J.; Cheng, B.; Wang, C. Orexin-A alleviates astrocytic apoptosis and inflammation via inhibiting OX1R-mediated NF-κB and MAPK signaling pathways in cerebral ischemia/reperfusion injury. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166230.
- Huang, L.; Li, X.; Liu, Y.; Liang, X.; Ye, H.; Yang, C.; Hua, L.; Zhang, X. Curcumin Alleviates Cerebral Ischemia-reperfusion Injury by Inhibiting NLRP1-dependent Neuronal Pyroptosis. Curr. Neurovasc Res. 2021, 18, 189–196.
- Zhou, Q.L.; Teng, F.; Zhang, Y.S.; Sun, Q.; Cao, Y.X.; Meng, G.W. FPR1 gene silencing suppresses cardiomyocyte apoptosis and ventricular remodeling in rats with ischemia/reperfusion injury through the inhibition of MAPK signaling pathway. Exp. Cell Res. 2018, 370, 506–518.
- Zhang, Y.; Wu, J.; Dong, E.; Wang, Z.; Xiao, H. Toll-like receptors in cardiac hypertrophy. Front. Cardiovasc. Med. 2023, 10, 1143583.
- Zhang, Y.; Liu, J.; Wang, C.; Liu, J.; Lu, W. Toll-Like Receptors Gene Polymorphisms in Autoimmune Disease. Front. Immunol. 2021, 12, 672346.
- Chu, Y.T.; Liao, M.T.; Tsai, K.W.; Lu, K.C.; Hu, W.C. Interplay of Chemokines Receptors, Toll-like Receptors, and Host Immunological Pathways. Biomedicines 2023, 11, 2384.
- Hu, J.; Deng, F.; Zhao, B.; Lin, Z.; Sun, Q.; Yang, X.; Wu, M.; Qiu, S.; Chen, Y.; Yan, Z.; et al. Lactobacillus murinus alleviate intestinal ischemia/reperfusion injury through promoting the release of interleukin-10 from M2 macrophages via Toll-like receptor 2 signaling. Microbiome 2022, 10, 38.
- Kitazume-Taneike, R.; Taneike, M.; Omiya, S.; Misaka, T.; Nishida, K.; Yamaguchi, O.; Akira, S.; Shattock, M.J.; Sakata, Y.; Otsu, K. Ablation of Toll-like receptor 9 attenuates myocardial ischemia/reperfusion injury in mice. Biochem. Biophys. Res. Commun. 2019, 515, 442–447.
- Guo, L.L.; Guo, M.L.; Yao, J.; Weng, Y.Q.; Zhang, X.Z. MicroRNA-421 improves ischemia/reperfusion injury via regulation toll-like receptor 4 pathway. J. Int. Med. Res. 2020, 48, 300060519871863.
- Zhang, T.; Xu, D.; Trefts, E.; Lv, M.; Inuzuka, H.; Song, G.; Liu, M.; Lu, J.; Liu, J.; Chu, C.; et al. Metabolic orchestration of cell death by AMPK-mediated phosphorylation of RIPK1. Science 2023, 380, 1372–1380.
- Lu, Y.; Zhang, C.; Chen, J.; Zou, Q.; Li, B.; Wei, H.; Chang, M.P.; Liao, X.; Hu, C. Hypothermia preconditioning improves cardiac contractility after cardiopulmonary resuscitation through AMPK-activated mitophagy. Exp. Biol. Med. 2022, 247, 1277–1286.
- Zuurbier, C.J.; Bertrand, L.; Beauloye, C.R.; Andreadou, I.; Ruiz-Meana, M.; Jespersen, N.R.; Kula-Alwar, D.; Prag, H.A.; Eric Botker, H.; Dambrova, M.; et al. Cardiac metabolism as a driver and therapeutic target of myocardial infarction. J. Cell. Mol. Med. 2020, 24, 5937–5954.
- Liu, H.; Wu, X.; Luo, J.; Zhao, L.; Li, X.; Guo, H.; Bai, H.; Cui, W.; Guo, W.; Feng, D.; et al. Adiponectin peptide alleviates oxidative stress and NLRP3 inflammasome activation after cerebral ischemia-reperfusion injury by regulating AMPK/GSK-3β. Exp. Neurol. 2020, 329, 113302.
- Zeng, Q.; Zhou, Y.; Liang, D.; He, H.; Liu, X.; Zhu, R.; Zhang, M.; Luo, X.; Wang, Y.; Huang, G. Exosomes Secreted From Bone Marrow Mesenchymal Stem Cells Attenuate Oxygen-Glucose Deprivation/Reoxygenation-Induced Pyroptosis in PC12 Cells by Promoting AMPK-Dependent Autophagic Flux. Front. Cell Neurosci. 2020, 14, 182.
More
Information
Subjects:
Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
525
Revisions:
2 times
(View History)
Update Date:
07 Feb 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




