
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Beata Sokołowska | -- | 5570 | 2024-01-31 17:57:20 | | | |
| 2 | Sirius Huang | Meta information modification | 5570 | 2024-02-01 01:59:41 | | |
Video Upload Options
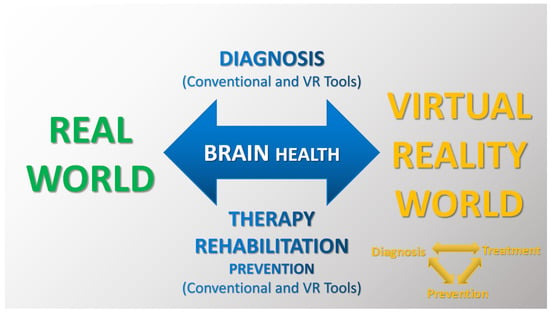
Dynamic technological development and its enormous impact on modern societies are posing new challenges for 21st-century neuroscience. A special place is occupied by technologies based on virtual reality (VR). VR tools have already played a significant role in both basic and clinical neuroscience due to their high accuracy, sensitivity and specificity and, above all, high ecological value. Being in a digital world affects the functioning of the body as a whole and its individual systems. The data obtained so far, both from experimental and modeling studies, as well as (clinical) observations, indicate their great and promising potential, but apart from the benefits, there are also losses and negative consequences for users.
1. Basic Features of Virtual Environments
2. VR Approaches as Novel Beneficial Environments/Tools and Discussion on Their Significance in Neuroscience
2.1. Traditional Versus Virtual Research Approaches
2.2. Basic Benefits of Using Virtual Environments
2.3. Examples of Research Area on the Impact of Virtual Environments on (Brain) Health
| Applications of VEs | Authors | Descriptions of VR Approaches, Basic Results and Conclusions |
|---|---|---|
| Experimental and modeling studies with healthy participants in real and virtual environments (VEs) | Kodithuwakku et al. 2024 [4] |
Researchers investigated the effects of virtual heights, dual-tasking (DT) and training on static postural stability in healthy adults without simulator/motion sickness and acrophobia. The results of modeling VEs showed that static balance deteriorates at higher VR altitudes and during DT and improves with VR training (but excessive visual stimulation reduced cortical response and postural control ability [24]). The authors suggest that VR can be used as a potential tool for ergonomic balance training (e.g., as strategies to prevent falls in workplaces). |
| Benelli et al. 2023 [45] |
Researchers emphasize that there is not yet an effective solution to the problem of cybersickness (CS) and propose an innovative approach for a frequency-dependent reduction in CS in VR via transcranial oscillatory stimulation of the vestibular cortex. The authors indicate that the new approach may be used to treat a variety of vestibular dysfunctions. | |
| Brock et al. 2023 [46] |
The modeling study examined movement kinematic and postural control for visual–motor skills during golf playing in real and VR environments in novice golfers (students). The results showed differences in putter swing between real and virtual reality, as well as between VE with and without haptic information. The authors note the possibility of different motor learning transfers in the conditions tested. | |
| Sokołowska 2021 [19][20] |
The research proposed a novel model-based approach to assessing functional lateralization of the brain and demonstrated highly effective recognition of functional and postural asymmetries using non-immersive VE in healthy adults. | |
| Pain Procedural pain Neuropathic pain Phantom limb pain (PLP) |
Li et al. 2023 [47] |
The research team proposed an interesting project to explore the analgesic effect of VE in healthy adults. The researchers compared the effect of immersive VR and no VR control on pain perception. The authors pointed to the analgesic benefits of VR and concluded that the VR findings support further development of digital healthcare. |
| Phelana et al. 2023 [48] |
The study describes the process of designing, testing and implementing a VR system in a hospital setting. In the experimental phase, the study was conducted on healthy adults, and pain was induced through cold pressor. The effectiveness of the VR system was then tested on burn-injured patients. The results show that prolonging the use of VR after a therapy session can help treat procedural pain more effectively. | |
| Aurucci et al. 2023 [36] |
Researchers proposed novel non-pharmacological interventions, such as transcutaneous electrical nerve stimulation (TENS) to activate peripheral pain relief via neuromodulation and VR to modulate patients’ attention. This is an example of a brain–computer interface enabling personalized multisensory intervention in neuropathic pain (i.e., a comprehensive approach to individualized therapy). The study demonstrates the feasibility of real-time pain detection based on objective neurophysiological signals and the effectiveness of a triggered combination of VR and TENS to significantly reduce neuropathic pain. | |
| Annapureddy et al. 2023 [49] |
Scientists tested a mixed reality system for treating phantom pain, using the immersive Mr. MAPP environment with a novel in-home virtual mirror therapy option. Mirror therapy allows participants to visually see missing limbs using a mirror. The results show that VE can potentially relieve pain and improve function in PLP patients. | |
| Hali et al. 2023 [22] |
Based on the current literature, the authors document that VR therapy has the potential to effectively treat PLP, and they identify additional benefits by adding vibrotactile stimuli to VR therapy. This approach leads to even greater pain reduction compared to VR therapy alone. | |
| Acquired brain injury (ABI) Traumatic brain injury (TBI) Intensive care unit weakness (ICU-AW) |
Bulle-Smid et al. 2023 [50] |
Researchers provide a review of extended reality (XR) environments as particularly promising in rehabilitating people with ABI and promoting professional supervision, faster recovery, shorter hospital stays and lower expenses. The authors suggest that future XR research should focus on developing appropriate XR environments, improving the safety and support for both patients and healthcare professionals. |
| Calabro et al. 2023 [51] |
The results of a study using non-immersive VE in tele-neurorehabilitation of patients with severe ABI (sABI) demonstrate that the VR approach is a suitable alternative and/or complementary tool to improve motor and cognitive function and reduce behavioral changes in sABI patients. In addition, the authors indicate a beneficial effect on alleviating caregivers’ distress and promoting positive aspects of caregiving. | |
| Brassel et al. 2021 [17] |
Researchers indicate that VR is increasingly being used to assess and treat impairment resulting from ABI due to its perceived advantages over conventional methods. In addition, the authors emphasize that there are no tailored options for designing and implementing VR in ABI or TBI rehabilitation. The researchers made some recommendations regarding these issues in this patient population. | |
| Keller et al. 2020 [5] |
Researchers presented that VR-based therapy to regain upper extremity function induces changes in the cortex grey matter in persons with ABI. The researchers proposed an interesting interactivity VR game in which ABI patients with upper limb paresis use an unaffected limb to control a standard input device and a regular computer mouse to control virtual limb movements and tasks in a virtual world. The results showed that the VR rehabilitation program significantly improved motor functions and skills in the affected upper extremities of subjects with ABI. In addition, significant increases in grey matter volume in the motor and premotor regions of the affected hemisphere and correlations of motor skills and volume in non-affected brain regions were observed, pointing out marked changes in structural brain plasticity. | |
| Castelli et al. 2023 [52] |
This is an interesting paper on the role of technology-based rehabilitation in patients with intensive care unit weakness (ICU-AW). The results of the study show that intensive structured rehabilitation is effective in improving motor function, disability and quality of life of patients with severe acquired brain injury and acquired weakness. For example, a combination of non-immersive VR training and focal muscle vibration can result in significant improvements in overall disability and quality of life compared to traditional treatment alone. The researchers recommend VEs in the neurorehabilitation of ICU-AW patients to facilitate the fastest possible neurorepair. | |
| Multiple sclerosis (MS) | Milewska-Jędrzejczak and Głąbiński 2023 [23] |
The research group presents recent findings of brain plasticity induction and its beneficial impact after both traditional physical and VR-based rehabilitation in patients with multiple sclerosis. The basic premise of this approach is that physical rehabilitation and physical activity are known non-pharmacological treatments for MS. |
| Kamm et al. 2023 [53] |
The study presents a new home-based immersive dexterity training program for MS patients based on a VR headset. The study demonstrates good feasibility, usability and patient engagement and satisfaction with this VR training (VRT) program. The results also indicate an improvement in the motor skills of the dominant hand after VRT. | |
| Cortés-Pérez et al. 2021 [54] |
The authors analyze and demonstrate that VR-based therapies are effective in reducing fatigue and have a positive impact on patients’ quality of life. | |
| Leonardi et al. 2021 [55] |
This clinical study on VR-based neurorehabilitation of cognitive dysfunction in people with relapsing/remitting MS showed improvement in mood and visuospatial skills. The researchers suggest that VR can be a motivating and effective tool for cognitive recovery in persons with MS. | |
| Stroke | Bedendo et al. 2024 [56] |
Researchers emphasize that to prevent deterioration of mobility, patients undergoing chronic rehabilitation must perform well-focused and repetitive exercises. In their view, VR appears as an interesting tool that offers the possibility of training and measuring patient performance. The authors proposed and tested an exercise design for the recovery of stroke patients at home, considering standard measures related to usability, immersion, workload and adverse symptoms, and with the involvement of rehabilitation experts. The results suggest the promising potential of VR applications for the future development of home rehabilitation programs. |
| Bargeri et al. 2023 [57] |
Researchers investigate and compare the efficacy and safety of VR rehabilitation for motor upper limb function and activity after stroke in immersive, semi-immersive and non-immersive modes of VR intervention with or without traditional therapy versus conventional therapy alone. The authors recommend the feasibility of using VR technology in clinical practice. | |
| Cinnera et al. 2023 [58] |
The authors explored the use of immersive VR to treat visual perception in unilateral spatial neglect (USN) after a stroke. The results demonstrate not only the potential benefits of VR in treating visual perception impairment in USN, but also that VE motivates patients during the rehabilitation process, improving compliance and interest. | |
| Errante et al. 2022 [59] |
Researchers investigated the effectiveness of a new VR rehabilitative approach with action observation therapy (AOT) based on the discovery of mirror neurons to improve motor function. The study evaluated action observation (AO) added to standard VR (AO + VR) to improve upper limb function in stroke patients, compared to a control treatment consisting of observing naturalistic scenes (CO) without any action content, followed by VR training (CO + VR). The authors suggest that AO + VR therapy could be adjunct to currently available rehabilitation interventions for post-stroke recovery and could be used as part of standard sensorimotor training or in individualized (tele)rehabilitation. | |
| Wiley et al. 2022 [16] |
The review examined the effects of VR therapy on cognition after stroke. The authors indicate that VR therapy (a) is a promising new form of technology that improves patient satisfaction with post-stroke rehabilitation; (b) has the added advantages of providing immediate feedback and a degree of difficulty that can be easily modified (i.e., the user-friendliness of this form of rehabilitation); and (c) has the potential to improve various motor, cognitive and physical deficits after stroke. In summary, VEs can be useful in rehabilitation settings. | |
| Mild cognitive impairment (MCI) | Gómez-Cáceres et al. 2023 [60] |
Researchers analyzed and evaluated the effectiveness of VR-based neuropsychological interventions in improving cognitive functioning in patients with MCI. The authors showed that VEs have a beneficial effect on improving cognitive functioning in patients with MCI, providing a basis for clinical practice recommendations. |
| Yang et al. 2022 [61] |
The results of the study show that VR-based cognitive training and exercise training improve brain health and cognitive and physical function in older adults with MCI. | |
| Liao et al. 2020 [62] |
The research team presented the potential of VR-based physical and cognitive training designed as an intervention for cognition and brain activation in elderly patients with MCI. The authors also analyzed whether a VR program designed around functional tasks can improve the instrumental activities of daily living (IADL) of these patients. The results showed that in both training programs without and with VR, there were improvements in executive function and verbal memory (immediate recall). But only in VR were there significant improvements in global cognition, verbal memory and IADL. In the authors’ opinion, VR training can be implemented for older adults with MCI. | |
| Mancuso et al. 2020 [63] |
The authors present the greater benefits/better effects of using VR with non-invasive brain stimulation, VR-NIBS, in the cognitive rehabilitation of patients with MCI and Alzheimer’s dementia. | |
| Cassani et al. 2020 [38] |
Based on the current literature, the authors demonstrated the benefits of the VR-NIBS combination for five therapeutic applications, namely neuropathic pain, cerebral palsy, stroke, multiple sclerosis, and post-traumatic stress disorder (PTSD) and phobias. | |
| VR exposure therapy (VRET) for posttraumatic stress disorders (PTSDs) and specific phobias | Siehl et al. 2023 [64] |
The study found that PTSD patients differ in brain activation from control subjects in regions such as the hippocampus, amygdala and ventromedial prefrontal cortex in processing unpredictable and predictable contexts. The researchers suggest that (a) deficient encoding of more complex configurations may lead to a preponderance of cue-based predictions in PTSD and (b) exposure-based therapies need to focus on improving the predictability of contextual processing and reducing enhanced cue reactivity. |
| Binder et al. 2022 [65] |
Researchers developed a fully automated experimental procedure using immersive VR involving behavioral search, forced-choice and an approaching task with varying degrees of freedom and stimulus relevance. In this study, scientists examined the sensitivity and feasibility of these tasks to assess avoidance behavior in patients with specific phobias. The results show the beneficial effects of immersive VR on specific phobias. In addition, the authors conclude that the behavioral tasks are well suited for assessing avoidance behavior in participants with phobias and provide detailed insights into the avoidance process. | |
| Alvarez-Perez et al. 2021 [66] |
Researchers emphasize that cognitive-behavioral therapy (CBT) with exposure is the treatment of choice for specific phobias. VR exposure therapy (VRET) has been shown to benefit the treatment and prevention of specific phobias by addressing the therapeutic limitations of exposure to real images. Neuroimaging studies on specific phobias demonstrate various changes in brain activation through CBT with VR exposure. | |
| Hinze et al. 2021 [67] |
The review presents current and future applications of innovative digital technologies in the effective diagnosis and cognitive-behavioral psychotherapy of spider phobia (arachnophobia). | |
| Other areas of application of VEs for Parkinson’s disease (PD), attention-deficit hyperactivity disorder (ADHD), schizophrenia spectrum disorders (SSDs) or autism spectrum disorders (ASDs), depressive disorders | Alavian et al. 2024 [68] Kaplan et et al. 2024 [69] Baugher et al. 2023 [70] |
Scientists emphasize that relatively few studies using innovative technologies are conducted in groups of patients with Parkinson’s disease. Not only VEs but also robotic (assistive) technologies are used in rehabilitation and evaluation of its (beneficial) effects. Patients’ family members/guardians are also involved in the research. This is crucial for such patients who require advanced care provided by the patient’s environment. The incidence of Parkinson’s disease, like that of other progressive neurodegenerative diseases, will increase as the world’s population ages. High hopes are being placed on the development of digital environments and tools, such as MR and AI. |
| Goharinejad et al. 2022 [71] Coleman et al. 2019 [72] |
The use of VR, AR and MR technologies in attention-deficit hyperactivity disorder (ADHD) has increased in recent years. ADHD is a neurodevelopmental disorder characterized by problems with concentration, excessive physical activity and impulsivity. The findings show that innovative technologies are promising tools to improve the diagnosis and management of ADHD. | |
| Holopainen et al. 2023 [73] Aubin et al. 2018 [74] |
Studies to date using VR technology in various symptom domains of schizophrenia spectrum disorders (SSDs) point to completely new possibilities for effective SSD treatment. Researchers indicate that (a) VEs still require more research and validation and (b) there are currently few studies examining the latest technology in the treatment of SSDs. | |
| Zhang et al. 2022 [75] De Luca 2021 [76] |
The number of studies using VR-based technology for individuals with ASD has increased over the last decade. De Luca’s team proposed a novel training program in a VE, documenting improved outcomes and changes in frontoparietal network connectivity after VR rehabilitation training. The current research indicates that (a) VEs are promising and efficacious for the assessment and treatment of ASD and have been found to be acceptable by persons with ASD. Researchers also emphasize that VEs provide fully interactive simulations of real-world settings and social situations that are particularly suitable for cognitive and performance training, including social skills and interaction. | |
| Yan et al. 2024 [77] Baghaei et al. 2021 [78] |
Research indicates that non-pharmacological innovations in (personalized) treatment plans/approaches for depressive disorders also include new VR-based strategies that may be effective in supporting the treatment of patients with depression. |
3. Being in VR and Discussing the Impact of Technical Aspects and Adverse Symptoms on (Brain) Health
3.1. VR Equipment for Non-Immersion, Partial Immersion and Full Immersion
3.2. VR and Adverse Symptoms such as Cybersickness
3.3. VR and the Development of Validation and Standardization Procedures
3.4. Summary
References
- Ali, S.G.; Wang, X.; Li, P.; Jung, Y.; Bi, L.; Kim, J.; Chen, Y.; Feng, D.D.; Magnenat Thalmann, N.; Wang, J.; et al. A systematic review: Virtual-reality-based techniques for human exercises and health improvement. Front. Public Health 2023, 11, 1143947.
- Riva, C.G. Special Topics in Information Technology; Springer Nature: Cham, Switzerland, 2023.
- Hamad, A.; Jia, B. How Virtual Reality Technology Has Changed Our Lives: An Overview of the Current and Potential Applications and Limitations. Int. J. Environ. Res. Public Health 2022, 19, 11278.
- Kodithuwakku Arachchige, S.N.K.; Chander, H.; Shojaei, A.; Knight, A.C.; Brown, C.; Freeman, H.R.; Burch, V.R.F.; Chen, C.C. Effects of virtual heights, dual-tasking, and training on static postural stability. Appl. Ergon. 2024, 114, 104145.
- Keller, J.; Štětkářová, I.; Macri, V.; Kühn, S.; Pětioký, J.; Gualeni, S.; Simmons, C.D.; Arthanat, S.; Zilber, P. Virtual reality-based treatment for regaining upper extremity function induces cortex grey matter changes in persons with acquired brain injury. J. Neuroeng. Rehabil. 2020, 17, 127.
- Milgram, P.; Takemura, H.; Utsumi, A.; Kishino, F. Augmented Reality: A class of displays on the reality-virtuality continuum. In Telemanipulator and Telepresence Technologies; Proc. SPIE 2351; SPIE: Bellingham, WA, USA, 1994; Volume 2351, pp. 282–292.
- Skarbez, R.; Smith, M.; Whitton, M.C. Revisiting Milgram and Kishino’s Reality-Virtuality Continuum. Front. Virtual Real. 2021, 2, 647997.
- Buhusi, C.V.; Oprisan, S.A.; Buhusi, M. The future of integrative neuroscience: The big questions. Front. Integr. Neurosci. 2023, 17, 1113238.
- Mauri, M.; Rancati, G.; Riva, G.; Gaggioli, A. Comparing the effects of immersive and non-immersive real estate experience on behavioral intentions. Comput. Hum. Behav. 2024, 150, 107996.
- Leong, S.C.; Tang, Y.M.; Toh, F.M.; Fong, K.N.K. Examining the effectiveness of virtual, augmented, and mixed reality (VAMR) therapy for upper limb recovery and activities of daily living in stroke patients: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2022, 19, 93.
- Cavedoni, S.; Cipresso, P.; Mancuso, V.; Bruni, F.; Pedroli, E. Virtual reality for the assessment and rehabilitation of neglect: Where are we now? A 6-year review update. Virtual Real. 2022, 30, 1–42.
- Msika, E.F.; Ehrlé, N.; Gaston-Bellegarde, A.; Orriols, E.; Piolino, P.; Narme, P. Using a Computer-Based Virtual Environment to Assess Social Cognition in Aging: An Exploratory Study of the REALSoCog Task. Front. Psychol. 2022, 13, 882165.
- Ribas, M.O.; Micai, M.; Caruso, A.; Fulceri, F.; Fazio, M.; Scattoni, M.L. Technologies to support the diagnosis and/or treatment of neurodevelopmental disorders: A systematic review. Neurosci. Biobehav. Rev. 2023, 145, 105021.
- Allain, P.; Foloppe, D.A.; Besnard, J.; Yamaguchi, T.; Etcharry-Bouyx, F.; Le Gall, D.; Nolin, R.P. Detecting everyday action deficits in Alzheimer’s disease using a nonimmersive virtual reality kitchen. J. Int. Neuropsychol. Soc. 2014, 20, 468–477.
- Liu, Q.; Song, H.; Yan, M.; Ding, Y.; Wang, Y.; Chen, L.; Yin, H. Virtual reality technology in the detection of mild cognitive impairment: A systematic review and meta-analysis. Ageing Res. Rev. 2023, 87, 101889.
- Wiley, E.; Khattab, S.; Tang, A. Examining the effect of virtual reality therapy on cognition post-stroke: A systematic review and meta-analysis. Disabil. Rehabil. Assist. Technol. 2022, 17, 50–60.
- Brassel, S.; Power, E.; Campbell, A.; Brunner, M.; Togher, L. Recommendations for the Design and Implementation of Virtual Reality for Acquired Brain Injury Rehabilitation: Systematic Review. J. Med. Internet Res. 2021, 23, e26344.
- Qian, J.; McDonough, D.J.; Gao, Z. The Effectiveness of Virtual Reality Exercise on Individual’s Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4133.
- Sokołowska, B. A Novel Perspective for Examining and Comparing Real and Virtual Test Tasks Performed by the Dominant and Non-Dominant Hand in Healthy Adults. Symmetry 2021, 13, 1810.
- Sokołowska, B. A novel virtual reality approach for functional lateralization in healthy adults. Brain Res. 2021, 1766, 147537.
- Sokołowska, B.; Sokołowska, E. An Example of the Assessment of Human Laterality Using Virtual reality. Int. J. Innov. Res. Comput. Commun. Eng. 2019, 7, 3555–3562.
- Hali, K.; Manzo, M.A.; Koucheki, R.; Wunder, J.S.; Jenkinson, R.J.; Mayo, A.L.; Ferguson, P.C.; Lex, J.R. Use of virtual reality for the management of phantom limb pain: A systematic review. Disabil. Rehabil. 2023, 1–8.
- Milewska-Jędrzejczak, M.; Głąbiński, A. The Influence of Conventional and Innovative Rehabilitation Methods on Brain Plasticity Induction in Patients with Multiple Sclerosis. J. Clin. Med. 2023, 12, 1880.
- Zhou, Z.; Chen, X.; Li, Y.; Chen, S.; Zhang, S.; Wu, Y.; Shi, X.; Ren, M.; Shan, C. Effects of integrated action and sensory observation therapy based on mirror neuron and embodied cognition theory on upper limb sensorimotor function in chronic stroke: A study protocol for a randomised controlled trial. BMJ Open 2023, 13, e069126.
- Kourtesis, P.; Kouklari, E.C.; Roussos, P.; Mantas, V.; Papanikolaou, K.; Skaloumbakas, C.; Pehlivanidis, A. Virtual Reality Training of Social Skills in Adults with Autism Spectrum Disorder: An Examination of Acceptability, Usability, User Experience, Social Skills, and Executive Functions. Behav. Sci. 2023, 13, 336.
- Kourtesis, P.; MacPherson, S.E. How immersive virtual reality methods may meet the criteria of the National Academy of Neuropsychology and American Academy of Clinical Neuropsychology: A software review of the Virtual Reality Everyday Assessment Lab (VR-EAL). CHB Rep. 2021, 4, 100151.
- Bonini, L.; Rotunno, C.; Arcuri, E.; Gallese, V. Mirror neurons 30 years later: Implications and applications. Trends Cogn. Sci. 2022, 26, 767–781.
- di Pellegrino, G.; Fadiga, L.; Fogassi, L.; Gallese, V.; Rizzolatti, G. Understanding motor events: A neurophysiological study. Exp. Brain Res. 1992, 91, 176–180.
- Rizzolatti, G.; Fadiga, L.; Gallese, V.; Fogassi, L. Premotor cortex and the recognition of motor actions. Brain Res. Cogn. Brain Res. 1996, 3, 131–141.
- Gallese, V.; Fadiga, L.; Fogassi, L.; Rizzolatti, G. Action recognition in the premotor cortex. Brain 1996, 119 Pt 2, 593–609.
- Thompson, E.L.; Bird, G.; Catmur, C. Mirror neuron brain regions contribute to identifying actions, but not intentions. Hum. Brain Mapp. 2022, 43, 4901–4913.
- Zhou, X.; Stehr, D.A.; Pyles, J.; Grossman, E.D. Configuration of the action observation network depends on the goals of the observer. Neuropsychologia 2023, 191, 108704.
- Plata-Bello, J.; Privato, N.; Modroño, C.; Pérez-Martín, Y.; Borges, Á.; González-Mora, J.L. Empathy Modulates the Activity of the Sensorimotor Mirror Neuron System during Pain Observation. Behav. Sci. 2023, 13, 947.
- Miyamoto, Y.; Uchitomi, H.; Miyake, Y. Effects of avatar shape and motion on mirror neuron system activity. Front. Hum. Neurosci. 2023, 17, 1173185.
- Gunduz, M.E.; Bucak, B.; Keser, Z. Advances in Stroke Neurorehabilitation. J. Clin. Med. 2023, 12, 6734.
- Aurucci, G.V.; Preatoni, G.; Damiani, A.; Raspopovic, S. Brain-Computer Interface to Deliver Individualized Multisensory Intervention for Neuropathic Pain. Neurotherapeutics 2023, 20, 1316–1329.
- Ansado, J.; Chasen, C.; Bouchard, S.; Northoff, G. How brain imaging provides predictive biomarkers for therapeutic success in the context of virtual reality cognitive training. Neurosci. Biobehav. Rev. 2021, 120, 583–594.
- Cassani, R.; Novak, G.S.; Falk, T.H.; Oliveira, A.A. Virtual reality and non-invasive brain stimulation for rehabilitation applications: A systematic review. J. Neuroeng. Rehabil. 2020, 17, 147.
- Minissi, M.E.; Gómez-Zaragozá, L.; Marín-Morales, J.; Mantovani, F.; Sirera, M.; Abad, L.; Cervera-Torres, S.; Gómez-García, S.; Chicchi Giglioli, I.A.; Alcañiz, M. The whole-body motor skills of children with autism spectrum disorder taking goal-directed actions in virtual reality. Front. Psychol. 2023, 14, 1140731.
- Pinarello, C.; Elmers, J.; Inojosa, H.; Beste, C.; Ziemssen, T. Management of multiple sclerosis fatigue in the digital age: From assessment to treatment. Front. Neurosci. 2023, 17, 1231321.
- Sattin, D.; Parma, C.; Lunetta, C.; Zulueta, A.; Lanzone, J.; Giani, L.; Vassallo, M.; Picozzi, M.; Parati, E.A. An Overview of the Body Schema and Body Image: Theoretical Models, Methodological Settings and Pitfalls for Rehabilitation of Persons with Neurological Disorders. Brain Sci. 2023, 13, 1410.
- Jacob, D.; Unnsteinsdóttir Kristensen, I.S.; Aubonnet, R.; Recenti, M.; Donisi, L.; Ricciardi, C.; Svansson, H.Á.R.; Agnarsdóttir, S.; Colacino, A.; Jónsdóttir, M.K.; et al. Towards defining biomarkers to evaluate concussions using virtual reality and a moving platform (BioVRSea). Sci. Rep. 2022, 12, 8996.
- Cavedoni, S.; Chirico, A.; Pedroli, E.; Cipresso, P.; Riva, G. Digital Biomarkers for the Early Detection of Mild Cognitive Impairment: Artificial Intelligence Meets Virtual Reality. Front. Hum. Neurosci. 2020, 14, 245.
- Nishimoto, R.; Fujiwara, S.; Kutoku, Y.; Ogata, T.; Mihara, M. Effect of dual-task interaction combining postural and visual perturbations on cortical activity and postural control ability. Neuroimage 2023, 280, 120352.
- Benelli, A.; Neri, F.; Cinti, A.; Pasqualetti, P.; Romanella, S.M.; Giannotta, A.; De Monte, D.; Mandalà, M.; Smeralda, C.; Prattichizzo, D.; et al. Frequency-Dependent Reduction of Cybersickness in Virtual Reality by Transcranial Oscillatory Stimulation of the Vestibular Cortex. Neurotherapeutics 2023, 20, 1796–1807.
- Brock, K.; Vine, S.J.; Ross, J.M.; Trevarthen, M.; Harris, D.J. Movement kinematic and postural control differences when performing a visuomotor skill in real and virtual environments. Exp. Brain Res. 2023, 241, 1797–1810.
- Li, J.; Yang, H.; Xiao, Y.; Liu, X.; Ma, B.; Ma, K.; Hu, L.; Lu, X. The analgesic effects and neural oscillatory mechanisms of virtual reality scenes based on distraction and mindfulness strategies in human volunteers. Br. J. Anaesth. 2023, 131, 1082–1092.
- Phelan, I.; Furness, P.J.; Matsangidou, M.; Babiker, N.T.; Fehily, O.; Thompson, A.; Carrion-Plaza, A.; Lindley, S.A. Designing effective virtual reality environments for pain management in burn-injured patients. Virtual Real. 2023, 27, 201–215.
- Annapureddy, D.; Annaswamy, T.M.; Raval, G.; Chung, Y.Y.; Prabhakaran, B. A novel mixed reality system to manage phantom pain in-home: Results of a pilot clinical trial. Front. Pain Res. 2023, 4, 1183954.
- Bulle-Smid, L.; Keuning, W.; Van Den Heuvel, R.; Hakvoort, G.; Verhoeven, F.; Daniels, R.; Hettinga, M. The Use of Extended Reality in Rehabilitation for Patients with Acquired Brain Injury: A Scoping Review. Stud. Health Technol. Inform. 2023, 306, 583–590.
- Calabrò, R.S.; Bonanno, M.; Torregrossa, W.; Cacciante, L.; Celesti, A.; Rifici, C.; Tonin, P.; De Luca, R.; Quartarone, A. Benefits of Telerehabilitation for Patients With Severe Acquired Brain Injury: Promising Results From a Multicenter Randomized Controlled Trial Using Nonimmersive Virtual Reality. J. Med. Internet Res. 2023, 25, e45458.
- Castelli, L.; Iacovelli, C.; Fusco, A.; Amoruso, V.; Cuccagna, C.; Loreti, C.; Giovannini, S.; Padua, L. The Role of Technological Rehabilitation in Patients with Intensive Care Unit Weakness: A Randomized Controlled Pilot Study. J. Clin. Med. 2023, 12, 2612.
- Kamm, C.P.; Blättler, R.; Kueng, R.; Vanbellingen, T. Feasibility and usability of a new home-based immersive virtual reality headset-based dexterity training in multiple sclerosis. Mult. Scler. Relat. Disord. 2023, 71, 104525.
- Cortés-Pérez, I.; Sánchez-Alcalá, M.; Nieto-Escámez, F.A.; Castellote-Caballero, Y.; Obrero-Gaitán, E.; Osuna-Pérez, M.C. Virtual Reality-Based Therapy Improves Fatigue, Impact, and Quality of Life in Patients with Multiple Sclerosis. A Systematic Review with a Meta-Analysis. Sensors 2021, 21, 7389.
- Leonardi, S.; Maggio, M.G.; Russo, M.; Bramanti, A.; Arcadi, F.A.; Naro, A.; Calabrò, R.S.; De Luca, R. Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation. Clin. Neurol. Neurosurg. 2021, 208, 106828.
- Bedendo, V.; Aruanno, B.; Dozio, N.; Covarrubias, M.; Ferrise, F. Exploiting Virtual Reality to Design Exercises for the Recovery of Stroke Patients at Home. Comput. Aided Des. Appl. 2024, 21, 463–473.
- Bargeri, S.; Scalea, S.; Agosta, F.; Banfi, G.; Corbetta, D.; Filippi, M.; Sarasso, E.; Turolla, A.; Castellini, G.; Gianola, S. Effectiveness and safety of virtual reality rehabilitation after stroke: An overview of systematic reviews. EClinicalMedicine 2023, 64, 102220.
- Martino Cinnera, A.; Bisirri, A.; Chioccia, I.; Leone, E.; Ciancarelli, I.; Iosa, M.; Morone, G.; Verna, V. Exploring the Potential of Immersive Virtual Reality in the Treatment of Unilateral Spatial Neglect Due to Stroke: A Comprehensive Systematic Review. Brain Sci. 2022, 12, 1589.
- Errante, A.; Saviola, D.; Cantoni, M.; Iannuzzelli, K.; Ziccarelli, S.; Togni, F.; Simonini, M.; Malchiodi, C.; Bertoni, D.; Inzaghi, M.G.; et al. Effectiveness of action observation therapy based on virtual reality technology in the motor rehabilitation of paretic stroke patients: A randomized clinical trial. BMC Neurol. 2022, 22, 109.
- Gómez-Cáceres, B.; Cano-López, I.; Aliño, M.; Puig-Perez, S. Effectiveness of virtual reality-based neuropsychological interventions in improving cognitive functioning in patients with mild cognitive impairment: A systematic review and meta-analysis. Clin. Neuropsychol. 2023, 37, 1337–1370.
- Yang, J.G.; Thapa, N.; Park, H.J.; Bae, S.; Park, K.W.; Park, J.H.; Park, H. Virtual Reality and Exercise Training Enhance Brain, Cognitive, and Physical Health in Older Adults with Mild Cognitive Impairment. Int. J. Environ. Res. Public Health 2022, 19, 13300.
- Liao, Y.Y.; Tseng, H.Y.; Lin, Y.J.; Wang, C.J.; Hsu, W.C. Using virtual reality-based training to improve cognitive function, instrumental activities of daily living and neural efficiency in older adults with mild cognitive impairment. Eur. J. Phys. Rehabil. Med. 2020, 56, 47–57.
- Mancuso, V.; Stramba-Badiale, C.; Cavedoni, S.; Pedroli, E.; Cipresso, P.; Riva, G. Virtual Reality Meets Non-invasive Brain Stimulation: Integrating Two Methods for Cognitive Rehabilitation of Mild Cognitive Impairment. Front. Neurol. 2020, 11, 566731.
- Siehl, S.; Wicking, M.; Pohlack, S.; Winkelmann, T.; Zidda, F.; Steiger-White, F.; Nees, F.; Flor, H. Altered frontolimbic activity during virtual reality-based contextual fear learning in patients with posttraumatic stress disorder. Psychol. Med. 2023, 53, 6345–6355.
- Binder, F.P.; Pöhlchen, D.; Zwanzger, P.; Spoormaker, V.I. Facing Your Fear in Immersive Virtual Reality: Avoidance Behavior in Specific Phobia. Front. Behav. Neurosci. 2022, 16, 827673.
- Álvarez-Pérez, Y.; Rivero, F.; Herrero, M.; Viña, C.; Fumero, A.; Betancort, M.; Peñate, W. Changes in Brain Activation through Cognitive-Behavioral Therapy with Exposure to Virtual Reality: A Neuroimaging Study of Specific Phobia. J. Clin. Med. 2021, 10, 3505.
- Hinze, J.; Röder, A.; Menzie, N.; Müller, U.; Domschke, K.; Riemenschneider, M.; Noll-Hussong, M. Spider Phobia: Neural Networks Informing Diagnosis and (Virtual/Augmented Reality-Based) Cognitive Behavioral Psychotherapy-A Narrative Review. Front. Psychiatry 2021, 12, 704174.
- Alavian, S.; Taghizade, G.; Mahdizade, H.; Behzadipour, S. A computerized assessment tool for the upper extremities motor performance in individuals with Parkinson’s disease. Biomed. Signal Process. Control 2024, 87, 105547.
- Kaplan, A.; Barkan-Slater, S.; Zlotnik, Y.; Levy-Tzedeket, S. Robotic technology for Parkinson’s disease: Needs, attitudes and concerns of individuals with Parkinson’s disease and their family members. A focus group study. Int. J. Hum.-Comput. Stud. 2024, 181, 103148.
- Baugher, B.; Szewczyk, N.; Liao, J. Augmented reality cueing for freezing of gait: Reviewing an emerging therapy. Parkinsonism Relat. Disord. 2023, 116, 105834.
- Goharinejad, S.; Goharinejad, S.; Hajesmaeel-Gohari, S.; Bahaadinbeigy, K. The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: An overview of relevant studies. BMC Psychiatry 2022, 22, 4.
- Coleman, B.; Marion, S.; Rizzo, A.; Turnbull, J.; Nolty, A. Virtual Reality Assessment of Classroom—Related Attention: An Ecologically Relevant Approach to Evaluating the Effectiveness of Working Memory Training. Front. Psychol. 2019, 10, 1851.
- Holopainen, R.; Tiihonen, J.; Lähteenvuo, M. Efficacy of immersive extended reality (XR) interventions on different symptom domains of schizophrenia spectrum disorders. A systematic review. Front. Psychiatry 2023, 14, 1208287.
- Aubin, G.; Béliveau, M.F.; Klinger, E. An exploration of the ecological validity of the Virtual Action Planning-Supermarket (VAP-S) with people with schizophrenia. Neuropsychol. Rehabil. 2018, 28, 689–708.
- Zhang, M.; Ding, H.; Naumceska, M.; Zhang, Y. Virtual Reality Technology as an Educational and Intervention Tool for Children with Autism Spectrum Disorder: Current Perspectives and Future Directions. Behav. Sci. 2022, 12, 138.
- De Luca, R.; Naro, A.; Colucci, P.V.; Pranio, F.; Tardiolo, G.; Billeri, L.; Le Cause, M.; De Domenico, C.; Portaro, S.; Rao, G.; et al. Improvement of brain functional connectivity in autism spectrum disorder: An exploratory study on the potential use of virtual reality. J. Neural Transm. 2021, 128, 371–380.
- Yan, S.; Shen, S.; Lu, Q.; Zhong, S.; Lv, S.; Lai, S.; Luo, Y.; Ran, H.; Duan, M.; Song, K.; et al. Virtual reality working memory training improves cognitive performance of acute and remitted patients with major depressive disorder. J. Affect. Disord. 2024, 344, 267–276.
- Baghaei, N.; Chitale, V.; Hlasnik, A.; Stemmet, L.; Liang, H.N.; Porter, R. Virtual Reality for Supporting the Treatment of Depression and Anxiety: Scoping Review. JMIR Ment. Health 2021, 8, e29681.
- Suh, A.; Prophet, J. The state of immersive technology research: A literature analysis. Comput. Hum. Behav. 2018, 86, 77–90.
- Vrigkas, M.; Nikou, C. A virtual reality 3D game: A comparison between an immersive virtual reality application and a desktop experience. In Proceedings of the 1st Workshop on 3D Computer Vision and Photogrammetry, Held in Conjunction with IEEE International Conference on Image Processing (ICIP’23), Kuala Lumpur, Malaisia, 8–11 October 2023; pp. 1–5.
- Sokołowska, B. Impact of Virtual Reality Cognitive and Motor Exercises on Brain Health. Int. J. Environ. Res. Public Health 2023, 20, 4150.
- Martirosov, S.; Bureš, M.; Zítka, T. Cyber sickness in low-immersive, semi-immersive, and fully immersive virtual reality. Virtual Real. 2022, 26, 15–32.
- Stanney, K.; Lawson, B.D.; Rokers, B.; Dennison, M.; Fidopiastis, C.; Stoffregen, T.; Weech, S.; Fulvio, J.M. Identifying Causes of and Solutions for Cybersickness in Immersive Technology: Reformulation of a Research and Development Agenda. Int. J. Hum. Comput. Interact. 2020, 36, 1783–1803.
- Kourtesis, P.; Linnell, J.; Amir, R.; Argelaguet, F.; MacPherson, S.E. Cybersickness in Virtual Reality Questionnaire (CSQ-VR): A Validation and Comparison against SSQ and VRSQ. Virtual Worlds 2023, 2, 16–35.
- Laessoe, U.; Abrahamsen, S.; Zepernick, S.; Raunsbaek, A.; Stensen, C. Motion sickness and cybersickness-Sensory mismatch. Physiol. Behav. 2023, 258, 114015.
- Kim, H.K.; Park, J.; Choi, Y.; Choe, M. Virtual reality sickness questionnaire (VRSQ): Motion sickness measurement index in a virtual reality environment. Appl. Ergon. 2018, 69, 66–73.
- Wenk, N.; Penalver-Andres, J.; Buetler, K.A.; Nef, T.; Müri, R.M.; Marchal-Crespo, L. Effect of immersive visualization technologies on cognitive load, motivation, usability, and embodiment. Virtual Real. 2023, 27, 307–331.
- Seki, R.; Shimomura, Y.; Asakawa, N.; Wada, H. Development of Orientation and Mobility Training System for Visually Impaired Children Using VR. Stud. Health Technol. Inform. 2023, 306, 527–534.
- Rahaman, T. Into the Metaverse—Perspectives on a New Reality. Med. Ref. Serv. Q. 2022, 41, 330–337.
- Kaddoura, S.; Al Husseiny, F. The rising trend of Metaverse in education: Challenges, opportunities, and ethical considerations. PeerJ Comput. Sci. 2023, 9, e1252.
- Segkouli, S.; Giakoumis, D.; Votis, K.; Triantafyllidis, A.; Paliokas, I.; Tzovaras, D. Smart Workplaces for older adults: Coping ‘ethically’ with technology pervasiveness. Univers. Access Inf. Soc. 2023, 22, 37–49.
- Paquin, V.; Ferrari, M.; Sekhon, H.; Rej, S. Time to Think “Meta”: A Critical Viewpoint on the Risks and Benefits of Virtual Worlds for Mental Health. JMIR Serious Games 2023, 11, e43388.
- Parsons, T.D. Ethical Challenges of Using Virtual Environments in the Assessment and Treatment of Psychopathological Disorders. J. Clin. Med. 2021, 10, 378.




