Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ibrahim Saliba | -- | 1468 | 2024-01-15 11:14:34 | | | |
| 2 | Peter Tang | + 1 word(s) | 1469 | 2024-01-16 02:53:08 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Saliba, I.; Hardy, A.; Wang, W.; Vialle, R.; Feruglio, S. Surgical Treatment of Acute Ankle Injury. Encyclopedia. Available online: https://encyclopedia.pub/entry/53828 (accessed on 28 February 2026).
Saliba I, Hardy A, Wang W, Vialle R, Feruglio S. Surgical Treatment of Acute Ankle Injury. Encyclopedia. Available at: https://encyclopedia.pub/entry/53828. Accessed February 28, 2026.
Saliba, Ibrahim, Alexandre Hardy, Wenzheng Wang, Raphael Vialle, Sylvain Feruglio. "Surgical Treatment of Acute Ankle Injury" Encyclopedia, https://encyclopedia.pub/entry/53828 (accessed February 28, 2026).
Saliba, I., Hardy, A., Wang, W., Vialle, R., & Feruglio, S. (2024, January 15). Surgical Treatment of Acute Ankle Injury. In Encyclopedia. https://encyclopedia.pub/entry/53828
Saliba, Ibrahim, et al. "Surgical Treatment of Acute Ankle Injury." Encyclopedia. Web. 15 January, 2024.
Copy Citation
Ankle sprains are exceedingly common injuries in both athletes and the general population. They account for 10 to 30% of all sports injuries. Although the vast majority of lateral ankle ligament injuries respond successfully to conservative management, the absolute number of those that progress to chronic lateral ankle instability (CLAI) remains considerably important. This condition is characterized by persistent symptoms and may be associated with short-term and long-term complications and functional deficits.
ankle instability
lateral ankle instability
chronic ankle instability
diagnostics
1. Introduction
Ankle sprains are exceedingly common injuries in both athletes and the general population [1][2][3][4]. They account for 10% to 30% of all sports injuries [5]. Inversion-type is the most common mechanism of injury, occurring in 80 to 90% of cases [3][5]. Although the vast majority of lateral ankle ligament injuries respond successfully to conservative management, 10% to 30% of patients may develop chronic lateral ankle instability (CLAI) [1][6]. This condition is characterized by persistent symptoms including pain, feeling of insecurity and a sensation of giving way. Moreover, it may result in short and long-term functional deficits, with risk to other structures requiring surgical correction including osteochondral injuries and peroneal tendons pathology [5][7]. There is a variety of surgical procedures intended to address CLAI, ranging from ligament repair to reconstructions using auto- or allograft tissue in order to replace torn ligaments [2][5][8][9][10]. Currently, there is still a lack of uniform phasing or even individualized protocols for rehabilitation of patients following CLAI surgery regarding weight bearing, Return To Work (RTW) and Return To Sport (RTS) [3][11]. As shown by Clements et al. in their systematic review [11], the postoperative outcomes in most studies are being measured using a variety of objective and subjective functional assessment scores and questionnaires, Range Of Motion (ROM) on physical examination and stress radiographs.
2. Overview of Ankle Lateral Ligamentous Anatomy
As shown in Figure 1, three ligaments compose the lateral ligament complex of the ankle: Anterior TaloFibular Ligament (ATFL), Posterior TaloFibular Ligament (PTFL) and CalcaneoFibular Ligament (CFL) [5][12]. ATFL is formed by superior intra-articular and inferior extra-articular fascicles. The inferior fascicle shares its fibular insertion with the CFL and both are connected together by the arciform fibers. Thus, they are sometimes also referred to as the lateral fibulotalocalcaneal ligament complex [5][13][14].
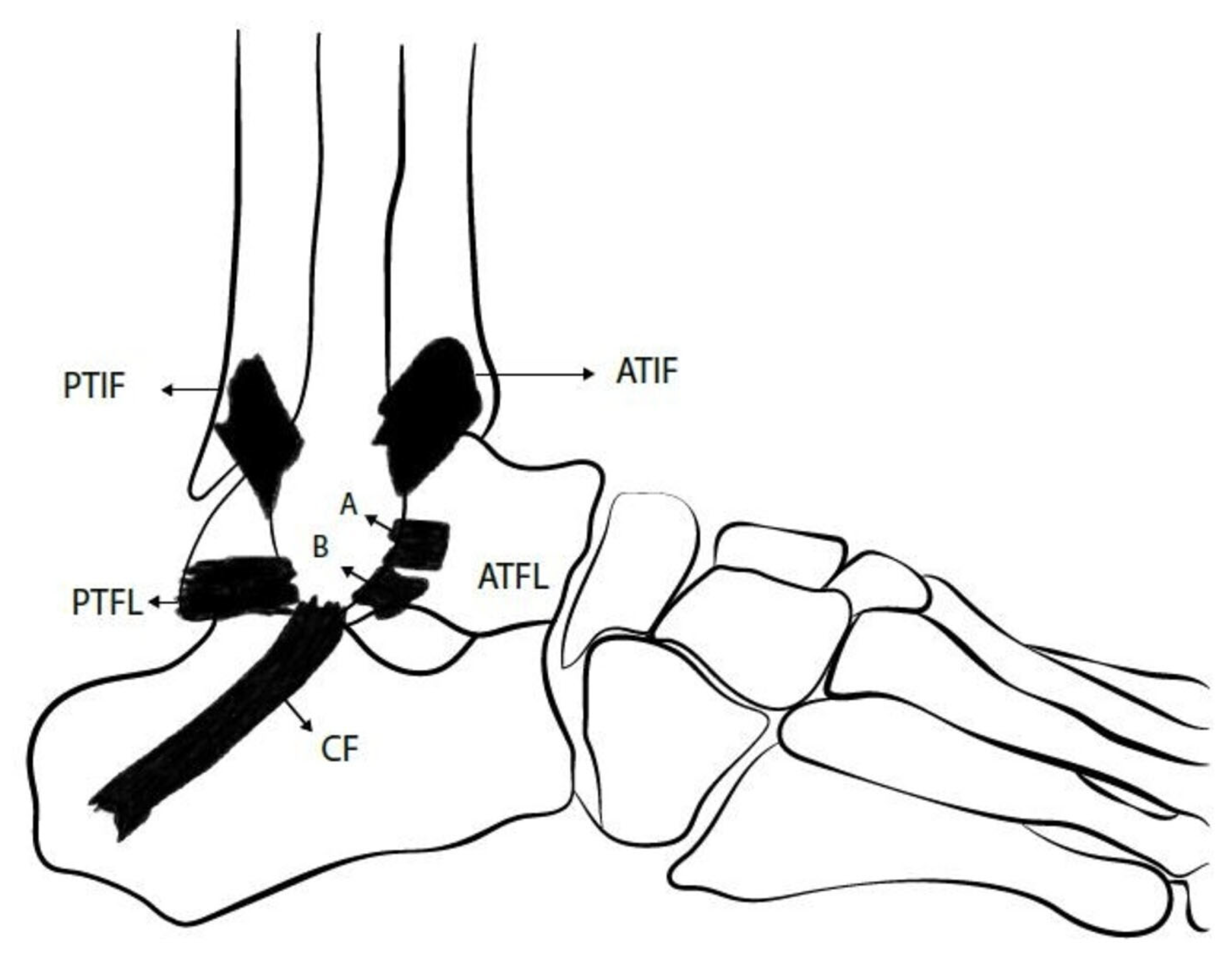
Figure 1. This figure represents the lateral ankle ligament anatomy: superior (A) and inferior (B) bands of Anterior TaloFibular Ligament (ATFL), CalcaneoFibular (CF) ligament and Posterior TaloFibular Ligament (PTFL). ATIF = Anterior inferior TibioFibular ligament; PTIF = Posterior inferior TibioFibular ligament (This figure was created by the researchers to be used here).
Given the aforementioned findings, the ATFL provides restraint to talar translation in the sagittal plane as well as talar rotation in the axial plane, while the CFL controls talar and calcaneal inversion [2]. Moreover, evidence from biomechanical studies shows that CFL contributes to subtalar joint stability, but the talocalcaneal ligaments do not provide stability to the ankle joint [2][15][16]. It was also observed that maximal tensile force of ATFL occurs during ankle plantar flexion while for CFL, the maximal tensile force occurs during ankle dorsiflexion [2][17].
3. Mechanism of Injury
The most common mechanism of acute ankle injury is a combination of inversion (Figure 2) and internal rotation forces associated with a plantar flexed or less frequently dorsiflexed foot [5]. The superior fascicle of ATFL is the weakest structure among the lateral ligaments of the ankle. It is the first ligament to be injured during ankle sprain [5][18][19]. In 65 to 80% of cases, there is an isolated rupture of the ATFL whereas a combined rupture of both ATFL and CFL (Figure 2) happens in around 20% of cases [5][18]. The PTFL is rarely injured during the abovementioned mechanism [19][20].

Figure 2. This figure shows a combined rupture of both Anterior TaloFibular Ligament (ATFL) and CalcaneoFibular Ligament (CFL) during an inversion-type lateral ankle sprain. This is found in about 20% of patients with lateral ankle instability (This figure was created by the researchers to be used here).
4. Diagnosis
Given that the purpose of this research is to focus on the improvement of the postoperative management, the different aspects that should be addressed by anamnesis [7][21] and the clinical tests [5][7][21] that should be carried out in order to rule out other associated injuries with lateral ligamentous ruptures including osteochondral lesions, bone fractures and peroneal tendons lesions, will not be detailed in this research. Special tests are usually used to help surgeons diagnose ankle instability. Typically, Anterior Drawer (AD) and Talar Tilt (TT) tests are used to assess the integrity of ATFL and CFL, respectively [2][5][7][21]. However, Van Dijk et al. considered that the AD test may not be accurate because it applies isolated sagittal translation without taking into account the rotational laxity [22]. Phisitkul et al. described AnteroLateral Drawer (ALD) testing in which the foot is allowed to internally rotate while translating it anteriorly, and they showed that ALD is a more accurate test than AD in detecting ATFL inefficiency [23]. Frey et al. compared Magnetic Resonance Imaging (MRI) results with physical examination findings and found that grade II lesions were most often underestimated by clinicians with an accuracy of only 25% in diagnosing those lesions [24]. To clarify, a grade I injury involves ligament stretching with minimal swelling, grade II indicates a partial macroscopic tear, while grade III signifies a complete rupture of the ligaments [24]. Some authors have proposed delaying the physical examination in acute settings to improve the accuracy of testing [22].
5. Imaging
Classically, three imaging modalities have been used to help diagnose CLAI: stress radiographs, MRI and UltraSonography (US) [2]. While stress radiographs have been proposed as an objective tool to visualize the subjective findings of AD and TT tests, with established threshold values including 10 mm anterior translation of talus for AD testing, and 10° tilt for TT testing [25]. When performing comparative radiographs between the injured and the normal sides, a side-to-side difference of at least 5 mm for AD or at least 5° for TT is required to support the diagnosis of lateral ankle instability [2][25]. In 1993, Peyre and Rodineau showed that auto-varus active stress radiographs may provide better results compared with passive testing realized manually or using a stress device [26]. However, the variety of measurement methods make the results difficult to exploit and until today the main limitation of stress radiographs remains their low sensitivity, which is around 57% [2][5][7][21][26].
MRI is sensitive for identification of ligament defects and ruptures, but its static nature prevents its ability to assess ligament function [2][5][27]. In their retrospective study, Jolman et al. compared the MRI findings of 112 patients operated for CLAI with those of 75 patients referred for other pathologies. The authors identified a high sensitivity but a relatively low specificity (53.3%) and concluded that MRI can be useful to identify associated extra and intra-articular lesions that can be associated with CLAI rather than being a primary tool to help establish the diagnosis of CLAI [27].
Ultrasonography (US) has showed substantial accuracy with high sensitivity and specificity in detecting ATFL and CFL defects [2][5][28]. Dynamic US can be performed using stress maneuvers in order to assess lateral ankle stability in real time. Although favorable outcomes are being observed in some studies, further clinical and biomechanical studies are still necessary before validating it as a diagnostic tool for CLAI. Finally, useful data cannot be obtained with US unless it is performed by a skilled operator.
6. Surgical Treatment
The surgical treatment of CLAI includes a number of procedures ranging from simple repair of the injured ligaments to reconstruction techniques. They can all be performed as open procedures or arthroscopically, and they can all be classified either as anatomic or non-anatomic techniques. Broström first described an anatomic open repair technique in 1966, consisting of tightening the ruptured lateral ligaments to the fibula [29]. Several modifications have been described subsequently, including the Gould et al. procedure that comprised an additional step, which is an augmentation of the repair using the inferior extensors retinaculum [30], then the Karlsson et al. modification that consisted of performing a shortening of the ligaments when they are elongated rather than disrupted [31]. The augmentation using non-absorbable suture-tape have been also advocated by some authors [5][32]. Non-anatomic reconstruction techniques involving tenodesis and including Chrisman-Snook, Evans and Watson-Jones procedures were initially introduced to replace the direct repair for cases with severely injured ligaments. However, they have been associated with many complications, including decreased ROM, recurrent lateral ankle instability and osteoarthritis. It was also shown that non-anatomic reconstruction may compromise the normal joint biomechanics [2][5][33]. Anatomic reconstruction procedures involve direct reconstruction of the ATFL and CFL using either autografts (Figure 3), allografts or synthetic ligaments. They have showed positive results and superior outcomes compared with non-anatomic reconstruction [2][5][34]. Nowadays, arthroscopically assisted and all-arthroscopic procedures are increasingly used for performing both repair and reconstruction with favorable outcomes in clinical studies. To the researchers' knowledge, we are still lacking high-level biomechanical evidence directly comparing arthroscopic versus open lateral ankle instability surgical techniques.
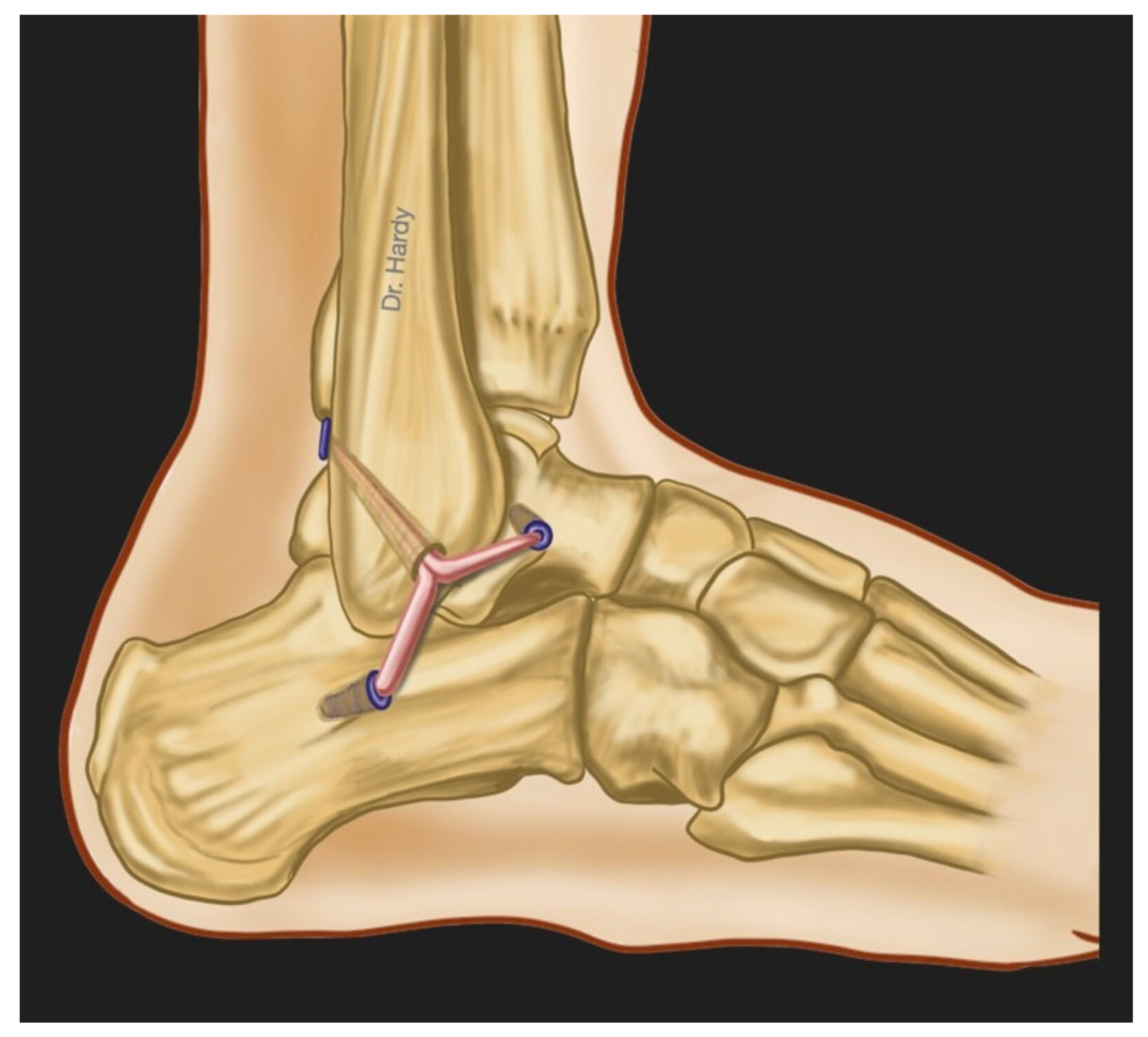
Figure 3. This figure represents the anatomic surgical reconstruction of the lateral ankle ligaments using an autograft: the gracilis tendon harvested from the patient’s knee (This figure was created by the researchers to be used here).
References
- Drakos, M.; Hansen, O.; Kukadia, S. Ankle Instability. Foot Ankle Clin. 2022, 27, 371–384.
- Chang, S.H.; Morris, B.L.; Saengsin, J.; Tourné, Y.; Guillo, S.; Guss, D.; DiGiovanni, C.W. Diagnosis and Treatment of Chronic Lateral Ankle Instability: Review of Our Biomechanical Evidence. J. Am. Acad. Orthop. Surg. 2021, 29, 3–16.
- Hunt, K.J.; Fuld, R.S.; Sutphin, B.S.; Pereira, H.; D’Hooghe, P. Return to sport following lateral ankle ligament repair is under-reported: A systematic review. J. ISAKOS Jt. Disord. Orthop. Sports Med. 2017, 2, 234–240.
- Vopat, M.L.; Tarakemeh, A.; Morris, B.; Hassan, M.; Garvin, P.; Zackula, R.; Mullen, S.; Schroeppel, P.; Vopat, B.G. Early versus Delayed Mobilization Post-Operative Protocols for Primary Lateral Ankle Ligament Repair: A Systematic Review and Meta-analysis. Foot Ankle Orthop. 2019, 4, 2473011419S0007.
- Machado, M.; Amado, P.; Babulal, J. Ankle instability—Review and new trends. J. Orthop. Trauma Rehabil. 2021, 28, 221049172110355.
- Bestwick-Stevenson, T.; Wyatt, L.A.; Palmer, D.; Ching, A.; Kerslake, R.; Coffey, F.; Batt, M.E.; Scammell, B.E. Incidence and risk factors for poor ankle functional recovery, and the development and progression of posttraumatic ankle osteoarthritis after significant ankle ligament injury (SALI): The SALI cohort study protocol. BMC Musculoskelet. Disord. 2021, 22, 362.
- Tourné, Y.; Besse, J.-L.; Mabit, C. Chronic ankle instability. Which tests to assess the lesions? Which therapeutic options? Orthop. Traumatol. Surg. Res. 2010, 96, 433–446.
- Dromzée, E.; Granger, B.; Rousseau, R.; Steltzlen, C.; Stolz, H.; Khiami, F. Long-Term Results for Treatment of Chronic Ankle Instability with Fibular Periosteum Ligamentoplasty and Extensor Retinaculum Flap. J. Foot Ankle Surg. 2019, 58, 674–678.
- Cho, B.-K.; Kim, Y.-M.; Shon, H.-C.; Park, K.-J.; Cha, J.-K.; Ha, Y.-W. A Ligament Reattachment Technique for High-Demand Athletes with Chronic Ankle Instability. J. Foot Ankle Surg. 2015, 54, 7–12.
- Porter, D.A.; Kamman, K.A. Chronic Lateral Ankle Instability. Foot Ankle Clin. 2018, 23, 539–554.
- Clements, A.D.; Belilos, E.B.; Keeling, L.; Kelly, M.; Casscells, N. Postoperative Rehabilitation of Chronic Lateral Ankle Instability: A Systematic Review. Sports Med. Arthrosc. Rev. 2021, 29, 146–152.
- Schroeder, J.; Barzilay, Y.; Hasharoni, A.; Kaplan, L. Long-term outcome of surgical correction of congenital kyphosis in patients with myelomeningocele (MMC) with segmental spino-pelvic fixation. Evid. Based Spine-Care J. 2011, 2, 17–22.
- Vega, J.; Malagelada, F.; Céspedes, M.-C.M.; Dalmau-Pastor, M. The lateral fibulotalocalcaneal ligament complex: An ankle stabilizing isometric structure. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 8–17.
- Umans, H.; Cerezal, L.; Linklater, J.; Fritz, J. Postoperative MRI of the Ankle and Foot. Magn. Reson. Imaging Clin. North Am. 2022, 30, 733–755.
- Brantigan, J.; Pedegana, L.; Lippert, F. Instability of the subtalar joint. Diagnosis by stress tomography in three cases. Minerva Anestesiol. 1977, 59, 321–324.
- Tochigi, Y.; Amendola, A.; Rudert, M.J.; Baer, T.E.; Brown, T.D.; Hillis, S.L.; Saltzman, C.L. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004, 25, 588–596.
- Ozeki, S.; Yasuda, K.; Kaneda, K.; Yamakoshi, K.; Yamanoi, T. Simultaneous strain measurement with determination of a zero strain reference for the medial and lateral ligaments of the ankle. Foot Ankle Int. 2002, 23, 825–832.
- Hintermann, B.; Boss, A.; Schäfer, D. Arthroscopic Findings in Patients with Chronic Ankle Instability. Am. J. Sports Med. 2002, 30, 402–409.
- Vega, J.; Allmendinger, J.; Malagelada, F.; Guelfi, M.; Dalmau-Pastor, M. Combined arthroscopic all-inside repair of lateral and medial ankle ligaments is an effective treatment for rotational ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 132–140.
- Vega, J.; Peña, F.; Golanó, P. Minor or occult ankle instability as a cause of anterolateral pain after ankle sprain. Knee Surg. Sports Traumatol. Arthrosc. 2014, 24, 1116–1123.
- Guillo, S.; Bauer, T.; Lee, J.; Takao, M.; Kong, S.; Stone, J.; Mangone, P.; Molloy, A.; Perera, A.; Pearce, C.; et al. Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop. Traumatol. Surg. Res. 2013, 99, S411–S419.
- van Dijk, C.N.; Lim, L.S.L.; Bossuyt, P.M.M.; Marti, R.K. Physical examination is sufficient for the diagnosis of sprained ankles. J. Bone Jt. Surg. 1996, 78, 958–962.
- Phisitkul, P.; Chaichankul, C.; Sripongsai, R.; Prasitdamrong, I.; Tengtrakulcharoen, P.; Suarchawaratana, S. Accuracy of Anterolateral Drawer Test in Lateral Ankle Instability: A Cadaveric Study. Foot Ankle Int. 2009, 30, 690–695.
- Frey, C.; Bell, J.; Teresi, L.; Kerr, R.; Feder, K. A Comparison of MRI and Clinical Examination of Acute Lateral Ankle Sprains. Foot Ankle Int. 1996, 17, 533–537.
- Hoffman, E.; Paller, D.; Koruprolu, S.; Drakos, M.; Behrens, S.B.; Crisco, J.J.; DiGiovanni, C.W. Accuracy of Plain Radiographs Versus 3D Analysis of Ankle Stress Test. Foot Ankle Int. 2011, 32, 994–999.
- Peyre, M.; Rodineau, J. L’auto Varus: Une Technique D’exploration des Instabilités Externes de Cheville; 3e Journées d’imagerie ostéo-articulaire de la Pitié Salpêtrière: Paris, France, 1993.
- Jolman, S.; Robbins, J.; Lewis, L.; Wilkes, M.; Ryan, P. Comparison of Magnetic Resonance Imaging and Stress Radiographs in the Evaluation of Chronic Lateral Ankle Instability. Foot Ankle Int. 2017, 38, 397–404.
- Alshalawi, S.; Galhoum, A.E.; Alrashidi, Y.; Wiewiorski, M.; Herrera, M.; Barg, A.; Valderrabano, V. Medial Ankle Instability. Foot Ankle Clin. 2018, 23, 639–657.
- Broström, L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand 1966, 132, 551–565.
- Gould, N.; Seligson, D.; Gassman, J. Early and Late Repair of Lateral Ligament of the Ankle. Foot Ankle 1980, 1, 84–89.
- Karlsson, J.; Bergsten, T.; Lansinger, O.; Peterson, L. Surgical treatment of chronic lateral instability of the ankle joint. Am. J. Sports Med. 1989, 17, 268–274.
- Viens, N.A.; Wijdicks, C.A.; Campbell, K.J.; LaPrade, R.F.; Clanton, T.O. Anterior Talofibular Ligament Ruptures, Part 1. Am. J. Sports Med. 2014, 42, 405–411.
- Hunt, K.J.; Pereira, H.; Kelley, J.; Anderson, N.; Fuld, R.; Baldini, T.; Kumparatana, P.; D’hooghe, P. The Role of Calcaneofibular Ligament Injury in Ankle Instability: Implications for Surgical Management. Am. J. Sports Med. 2019, 47, 431–437.
- Camacho, L.D.; Roward, Z.T.; Deng, Y.; Latt, L.D. Surgical Management of Lateral Ankle Instability in Athletes. J. Athl. Train. 2019, 54, 639–649.
More
Information
Subjects:
Health Care Sciences & Services; Rehabilitation
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
2 times
(View History)
Update Date:
16 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





