Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Stoyan Kostov | -- | 1929 | 2024-01-13 10:40:39 | | | |
| 2 | Camila Xu | Meta information modification | 1929 | 2024-01-15 02:23:03 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kostov, S.; Kornovski, Y.; Watrowski, R.; Slavchev, S.; Ivanova, Y.; Yordanov, A. Internal Iliac Artery Anatomy. Encyclopedia. Available online: https://encyclopedia.pub/entry/53795 (accessed on 07 February 2026).
Kostov S, Kornovski Y, Watrowski R, Slavchev S, Ivanova Y, Yordanov A. Internal Iliac Artery Anatomy. Encyclopedia. Available at: https://encyclopedia.pub/entry/53795. Accessed February 07, 2026.
Kostov, Stoyan, Yavor Kornovski, Rafał Watrowski, Stanislav Slavchev, Yonka Ivanova, Angel Yordanov. "Internal Iliac Artery Anatomy" Encyclopedia, https://encyclopedia.pub/entry/53795 (accessed February 07, 2026).
Kostov, S., Kornovski, Y., Watrowski, R., Slavchev, S., Ivanova, Y., & Yordanov, A. (2024, January 13). Internal Iliac Artery Anatomy. In Encyclopedia. https://encyclopedia.pub/entry/53795
Kostov, Stoyan, et al. "Internal Iliac Artery Anatomy." Encyclopedia. Web. 13 January, 2024.
Copy Citation
The internal iliac artery (IIA), previously referred to the hypogastric artery, is the primary arterial vessel of the pelvis. It supplies the pelvic viscera, pelvic walls, perineum, and the gluteal region. The blood supply to the uterus comes from some of the IIA divisions and their anastomoses
anatomy
obstetrics and gynecology
internal iliac artery ligation
1. Level of the IIA Origin
The IIA originates from the common iliac artery (CIA) anterior to the sacroiliac joint. Generally, the level of the IIA’s origin is situated at the L5–S1 intervertebral disc [1]. A study involving 150 cadavers identified the bifurcation point of the CIA at the level between L5 and S1 in 82% of cases and at the level of L5 in 15% of cases [2]. Another study, including 60 bisected human cadaveric pelvises, demonstrated that the origin of IIA was at the level of the S1 vertebra in 35 cases (58.3%), at the level of L5–S1 in 24 cases (40%), and in 1 case (1.7%), at the level of L5 [3]. Similarly, in a study involving 50 bisected human cadaveric pelvises, the origin of the IIA was observed at the level of the S1 vertebra in 36 cases (72%), at the level of L5–S1 in 12 cases (24%), and at the level of L5 in 2 specimens (4%) [4]. In the study by Sakthivelavan et al. involving 116 pelvic halves from 58 embalmed cadavers, the origin of the IIA was found at the level of the lumbosacral transition in 94 specimens (81%) and above that level in 22 specimens (19%) [5].
2. Level of Termination of IIA Trunks
The IIA runs posteriorly to the superior border of the greater sciatic foramen, where it separates into two divisions—anterior and posterior [6]. Mamatha et al. reported the termination of IIA divisions above the level of the greater sciatic notch in 98% of specimens and below it in 2% [4]. A study by Sakthivelavan et al. showed that the IIA originated at the level of the superior border of the greater sciatic notch in 65.5% of cases, and at various positions between lumbosacral transition and the greater sciatic foramen in 34.5% of cases [5]. Naveen observed the termination of the IIA division above the level of the greater sciatic notch in 100% of specimens [3]. Cases have been reported where the posterior division of IIA is absent, or divisions of IIA arise without dividing into anterior and posterior trunks [5][7].
3. Length of IIA
Knowledge of the length of IIA is essential while performing its ligation. According to Gray’s Anatomy, the length of the IIA is approximately 4 cm [8]. The right IIA is frequently longer than the left IIA [2]. Bleich et al. measured the length of the IIA from the CIA bifurcation to the origin of the first posterior division [9]. The authors also measured the length of the IIA together with the cranio-caudal width of the posterior division. Bleich’s measurement has clinical significance, as surgeons can estimate the distance at which the posterior division will be spared. [9]. Generally, the length of the IIA is measured from the CIA bifurcation to the bifurcation into two terminal branches [10][11]. Other authors measured the length of the IIA from its origin to the point of bifurcation of the anterior and posterior divisions [12]. The length of the IIA varies among different populations [12]. Cadaveric studies have reported IIA lengths ranging from 0 to 90 mm (Table 1) [2][3][5][9][10][11][12]. However, except for the study of Bleich et al. [9] (only female cadavers were examined), the majority of studies examined the anatomy of IIA in both sexes [3][5][11][12].
Table 1. Length of IIA in anatomical studies.
| Author | Year | Cadaver Origin | Number of Cadavers or Hemi-Pelvises | Mean Length (cm) (±SD) | Range (cm) |
|---|---|---|---|---|---|
| Adachi [10] | 1928 | Japan | 121 | 44.3 (±1.3) | |
| Shafiroff et al. [2] | 1959 | USA | 150 | 1–3 (21%) 3–5 (60%) 5–7 (13%) |
|
| Fatu et al. [11] | 2006 | Romania | 100 | 4.9 | 2–9 |
| Bleich et al. [9] | 2007 | USA | 54 (right) 54 (left) |
26.8 27 |
0–5.2 0–4.9 |
| Naveen [3] | 2011 | India | 60 (hemi-pelvises) | 3.7 (±4.62) | 1.3–5.4 |
| Sakthivelavan et al. [5] | 2014 | India | 58 | 3.7 | 2.3–7.1 |
| Yuvaraj et al. [12] | 2018 | India | 80 (right) 80 (left) |
3.94 (±0.86) 3.61 (±0.63) |
2.4–5.4 2.7–4.7 |
4. Variability in the Branching Pattern of the IIA
The anterior and posterior divisions of the IIA typically include the following branches: posterior division (superior gluteal artery, iliolumbar artery, and lateral sacral arteries) and anterior division (umbilical artery, superior vesical artery (it could be two or more originating), obturator artery, uterine artery, vaginal artery, middle rectal artery, internal pudendal artery, inferior gluteal artery) [8][13][14][15]. Some editions of anatomical textbooks suggest that in females, the vaginal artery may replace the inferior vesical artery [8]. The 42nd edition of Gray’s Anatomy stated that in females, the vaginal artery sometimes replaces the inferior vesical artery. The latter can originate in close proximity to the origin of the uterine artery, either as a single vaginal artery or multiple vaginal branches [15]. However, it is worth noting that the presence of the inferior vesical artery in the female population exhibits considerable variability in terms of its origin and prevalence. De Treigny et al. reported finding the inferior vesical artery in 47.4% of the examined female cadavers. The artery had different origins, either as a common trunk with the uterine and umbilical artery (33.3%) or emerging directly from the umbilical artery (33.3%), from the uterine artery (22.2%), or from the obturator artery (11.1%). Consequently, the authors concluded that the presence of the inferior vesical artery should not be considered to be confined to the male population alone [16]. Shafiroff reported a 78% prevalence of the inferior vesical artery among 150 specimens (both males and females). The author observed that the artery has many different origins—the umbilical, testicular, internal pudendal, and vaginal arteries [2]. The presence of inferior vesical arteries was reported in another study, which observed the artery flow velocities by Doppler examination in women receiving hormonal replacement therapy [17]. Ercoli et al. also mentioned the presence of inferior vesical arteries in a cadaveric study, which included 30 female cadavers. Authors observed that the inferior vesical and vaginal arteries are part of the tissue that envelops the vesicovaginal ligament, also known as the deep layer of the vesicouterine ligament [18]. Muallem et al. even used the inferior vesical artery as a landmark for the exact anatomical positions of one of the pelvic splanchnic nerves. Moreover, authors believed that the inferior vesical artery plays a very important role in arterial vascularization of the distal ureter [19]. The presence of the inferior vesical artery was mentioned in another study. Authors divided the IIA into visceral divisions and parietal divisions (the iliolumbar, sacral lateral, superior gluteal, inferior gluteal artery, internal pudendal arteries). The aim of the study was to investigate the variability in the origin of the uterine artery among one hundred women, who underwent laparoscopic surgery for uterine fibroids. Authors reported four different types of IIA origin. The study found that the uterine artery, middle rectal artery, and the inferior vesical artery originated from the internal pudendal artery (type 2b) in 24.3% of the investigated patients [20]. Authors reported that the inferior vesical artery, the middle rectal artery, and the uterine artery arose in a common trunk, which originated from a larger-than-usual internal pudendal artery [20].
It is well established that the IIA exhibits numerous variations in its branching pattern. Therefore, a thorough understanding of the distribution pattern of this artery is essential for safely performing retroperitoneal surgery [1].
Many authors have proposed various concepts for classifying the terminal divisions of the IIA [11][21][22]. Generally, surgeons use the Adachi classifications system, which has been the standard for many years [4][5][10][11]. Adachi defined the branching of the IIA based on its four major parietal divisions: the umbilical, superior gluteal, inferior gluteal, and internal pudendal arteries (see Figure 1, Figure 2 and Figure 3) [1][10].
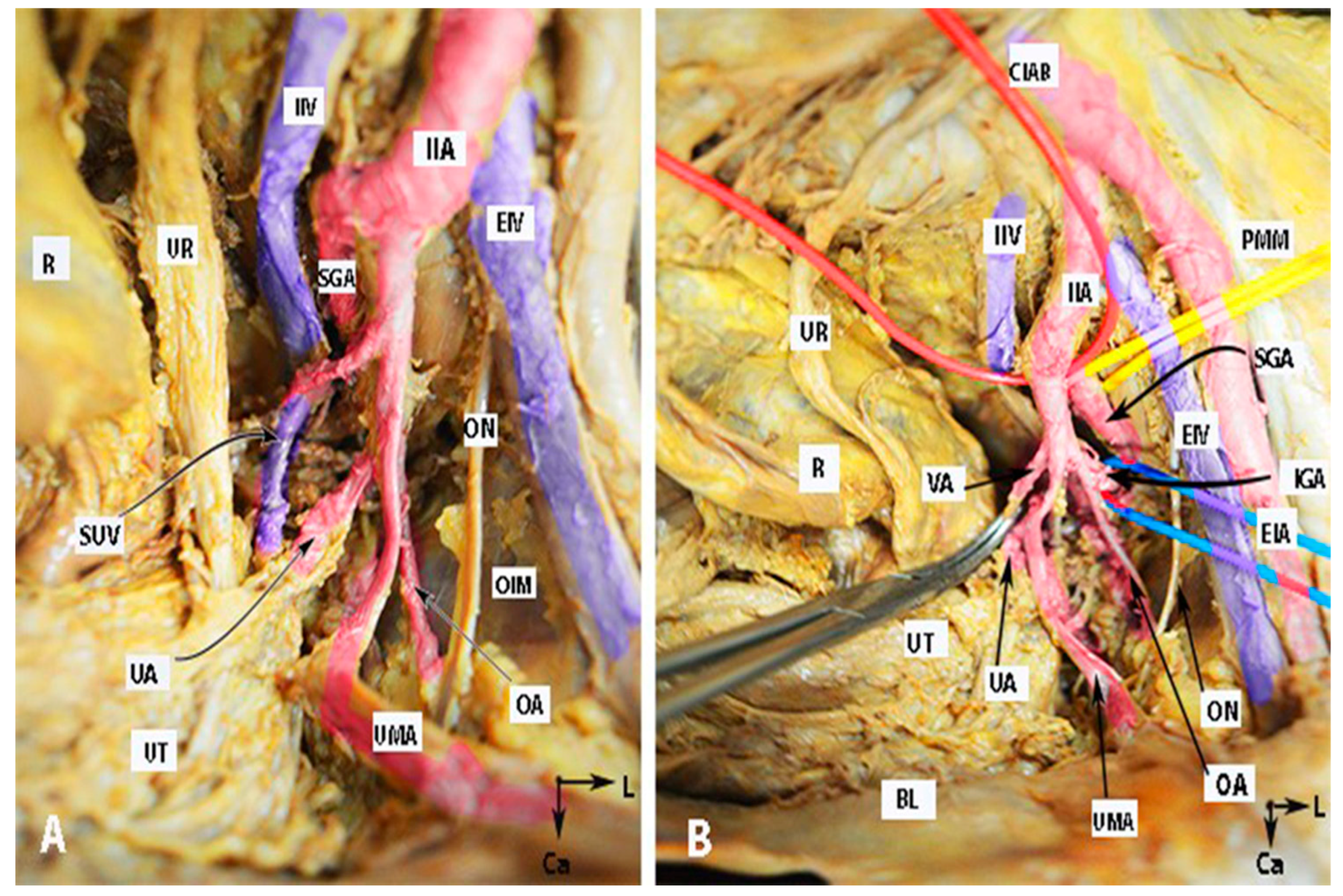
Figure 1. Anatomy of the internal iliac artery ((A,B)—embalmed female cadaver; author’s own material). (A,B) show the left side of the pelvis of the same cadaver. The posterior branch of the IIA has a lateral course (superior gluteal artery) in the pelvic sidewall. The middle rectal artery and iliolumbar artery were cut during dissection. EIA—external iliac artery; IIA—internal iliac artery; EIV—external iliac vein; ON—obturator nerve; OIM—obturator internus muscle; SGA—superior gluteal artery; IGA—inferior gluteal artery; UR—ureter; SUV—superficial uterine vein; OA—obturator artery; UMA—umbilical artery; UA—uterine artery; UT—uterus; PMM—psoas major muscle; IIV—internal iliac vein; VA—vaginal artery; CIAB—common iliac artery bifurcation; BL—bladder; R—rectum; CA—caudal; L—left.
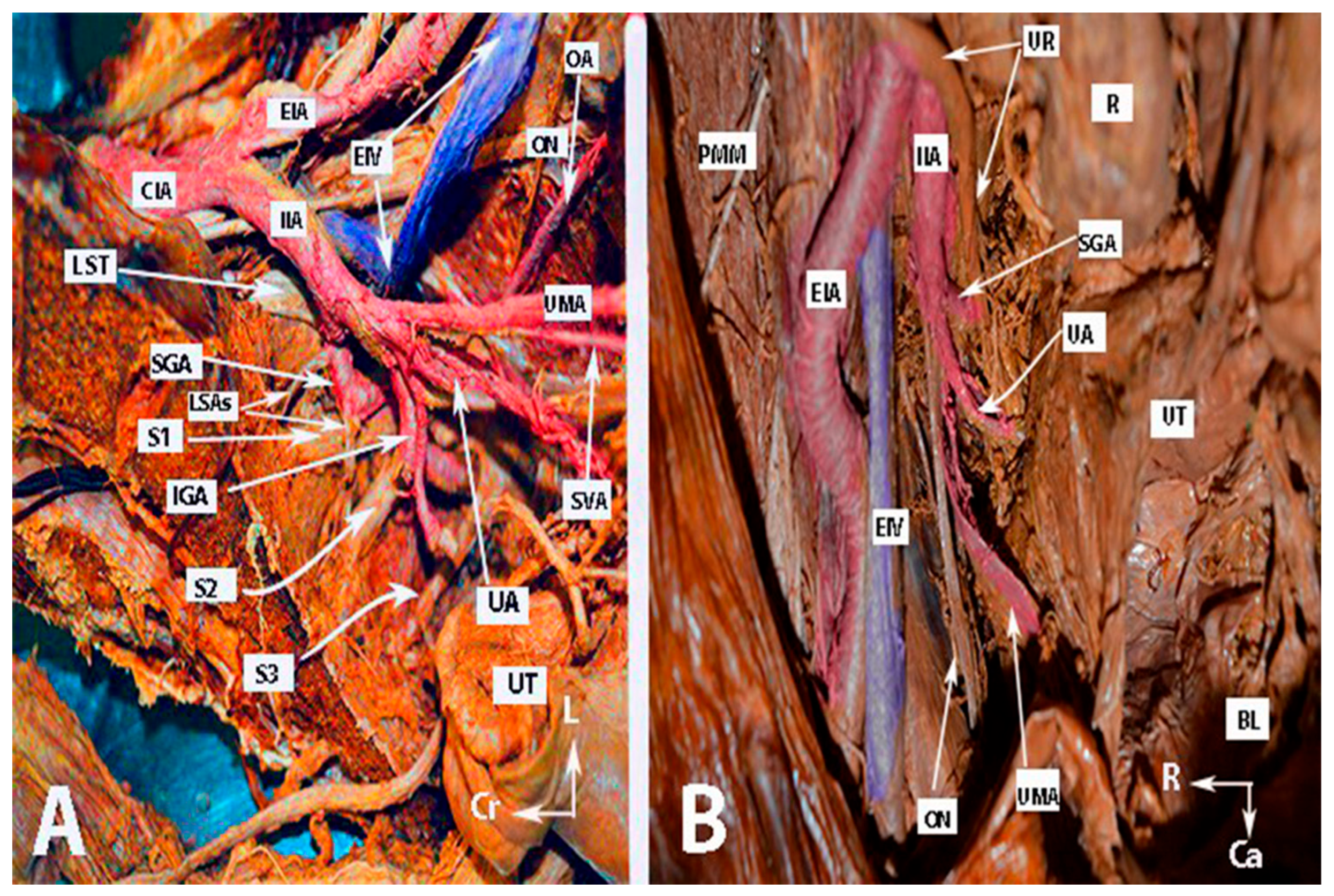
Figure 2. Anatomy of the internal iliac artery ((A,B)—embalmed female cadavers; author’s own material). (A,B) show the left and right pelvic sidewall in two different female cadavers. The posterior branch of the internal iliac artery (superior gluteal artery) has a medial course in both figures. (A)—The sacral plexus and its relation to the divisions of the internal iliac artery are clearly highlighted. The superior gluteal artery runs between the lumbosacral trunk and the anterior ramus of the first sacral nerve and leaves the pelvis through the suprapiriform foramen. The inferior gluteal artery is located between the anterior rami of the second and third sacral nerves and leaves the pelvis through the infrapiriform foramen. (B)—The course of the uterine artery ventral to the ureter can be clearly seen. EIA—external iliac artery; IIA—internal iliac artery; EIV—external iliac vein; ON—obturator nerve; SGA—superior gluteal artery; IGA—inferior gluteal artery; UR—ureter; SUV—superficial uterine vein; SVA—superior vesical artery; LSAs—lateral sacral arteries; OA—obturator artery; UMA—umbilical artery; UA—uterine artery; PMM—psoas major muscle; IIV—internal iliac vein; VA—vaginal artery; CIAB—common iliac artery bifurcation; BL—bladder; UT—uterus; R—rectum; LST—lumbosacral trunk; S1, S2, S3—anterior rami of the sacral spinal nerves; Ca—caudal; L—left; Cr—cranial.
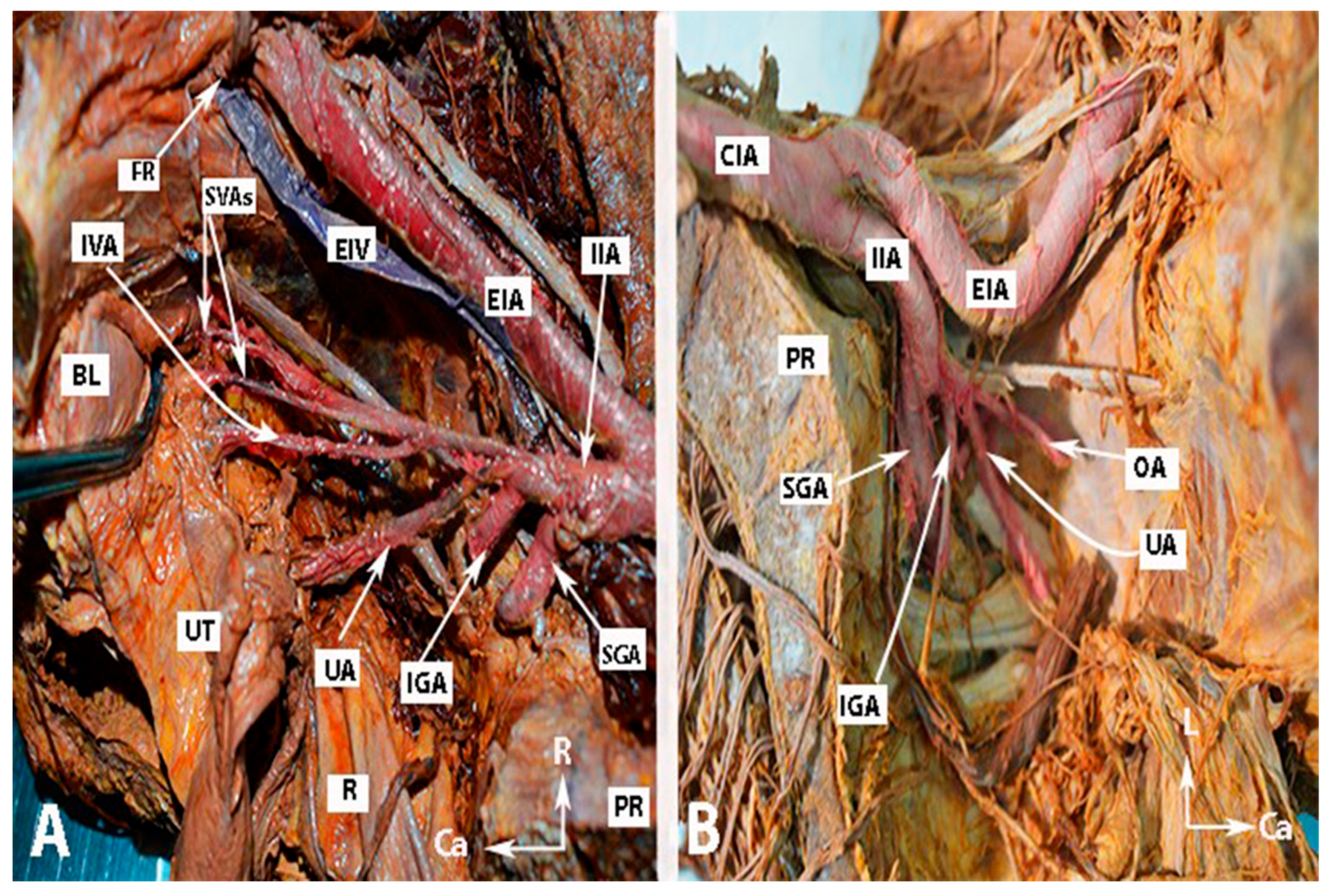
Figure 3. Anatomy of the internal iliac artery of (A,B) embalmed female cadavers; author’s own material. (A,B) show the right and left pelvic sidewalls in two different female cadavers. A—Presence of the inferior vesical artery in a female. B—Anomalous shape and course of the internal and external iliac arteries. The internal iliac artery follows a direct caudal course. EIA—external iliac artery; EIV—external iliac vein; IIA—internal iliac artery; FR—femoral ring; IVA—inferior vesical artery; SVAs—superior vesical arteries; IGA—inferior gluteal artery; SGA—superior gluteal artery; UA—uterine artery; OA—obturator artery; PR—promontory; UT—uterus; R—rectum; BL—bladder; R—right; Ca—caudal; L—left.
The Adachi classification system includes the following types:
Type 1: The superior gluteal artery (SGA) originates separately from the IIA, while the inferior gluteal (IGA) and internal pudendal artery (IPA) share a common trunk. Subtypes 1a and 1b depend on whether the bifurcation of the IGA and IPA occur within or below the pelvis, respectively.
Type 2: The IPA originates independently from the IIA, while the SGA and the IGA share a common trunk. Subtypes 2a and 2b represent whether the bifurcation of the SGA and IGA arise within or below the pelvis, respectively.
Type 3: The SGA, IGA, and IPA originate independently from the IIA, with the IPA being the terminal branch.
Type 4: The SGA, IGA, and IPA have a common trunk. Classification in subtypes 4a and 4b depends on whether the SGA or IPA is the initial vessel emerging from the common trunk. For instance, in 4a, the SGA is the initial vessel coming from the common trunk before bifurcating into the other two divisions—the SGA and IGA. In type 4b, the IPA is the first to come from the common trunk, which then splits into the SGA and IGA.
Type 5: The IGA originates independently from the IIA, while the SGA and IGA share a common trunk [10].
Surgeons should also be familiar with the anatomy of the internal iliac vein (IIV), which follows a similar course to its arterial counterpart, ascending posteromedially to the IIA. The IIV drains into the ipsilateral external iliac vein [8].
For visual reference, the anatomy of the IIA and some anatomical differences are illustrated in Figure 1, Figure 2 and Figure 3. The iliolumbar artery and middle rectal artery are not shown in the figures.
References
- Tubbs, R.S.; Shoja, M.M.; Loukas, M. Bergman’s Comprehensive Encyclopedia of Human Anatomic Variation; John Wiley & Sons: Hoboken, NJ, USA, 2016; pp. 669–673, 884–889.
- Shafiroff, B.G.P.; Grillo, E.B.; Baron, H. Bilateral ligation of the hypogastric arteries. Am. J. Surg. 1959, 98, 34–40.
- Naveen, N.S. Morphological Analysis of the Human Internal Iliac Artery in South Indian Population. Online J. Health Allied. Sci. 2011, 10, 1–4.
- Mamatha, H.; Hemalatha, B.; Vinodini, P.; Souza, A.S.; Suhani, S. Anatomical Study on the Variations in the Branching Pattern of Internal Iliac Artery. Indian J. Surg. 2015, 77 (Suppl. S2), 248–252.
- Sakthivelavan, S.; Aristotle, S.; Sivanandan, A.; Sendiladibban, S.; Felicia Jebakani, C. Variability in the branching pattern of the internal iliac artery in Indian population and its clinical importance. Anat. Res. Int. 2014, 2014, 597103.
- Selçuk, İ.; Yassa, M.; Tatar, İ.; Huri, E. Anatomic structure of the internal iliac artery and its educative dissection for peripartum and pelvic hemorrhage. Turk. J. Obstet. Gynecol. 2018, 15, 126–129.
- Field, K.; Ryan, M.J.; A Saadeh, F.; Kamran, W.; Brennan, V.; Gillham, C.; Gleeson, N. Selective arterial embolisation for intractable vaginal haemorrhage in genital tract malignancies. Eur. J. Gynaecol. Oncol. 2016, 37, 736–740.
- Gray, H.; Standring, S.; Hrold Ellis, H.; Berkovitz, B. Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th ed.; Elsevier Churchill Livingstone Edinburgh: New York, NY, USA, 2005.
- Bleich, A.T.; Rahn, D.D.; Wieslander, C.K.; Wai, C.Y.; Roshanravan, S.M.; Corton, M.M. Posterior division of the internal iliac artery: Anatomic variations and clinical applications. Am. J. Obstet. Gynecol. 2007, 197, 658.e1–658.e5.
- Adachi, B. Das arteriensystem der Japaner. Band 1928, 9, 1926–1927.
- Fătu, C.; Puişoru, M.; Fătu, I.C. Morphometry of the internal iliac artery in different ethnic groups. Ann. Anat. 2006, 188, 541–546.
- Yuvaraj, M.F.; Balaji, T.; Rajila, R.H.S.; Vaithianathan, G.; Aruna, S.; Balaji, K. Study on Variations in the Origin and Branching Pattern of Internal Iliac Artery in Cadavers. Biomed Pharmacol. J. 2018, 11, 2201–2207.
- Papp, Z.; Tóth-Pál, E.; Papp, C.; Sziller, I.; Gávai, M.; Silhavy, M.; Hupuczi, P. Hypogastric artery ligation for intractable pelvic hemorrhage. Int. J. Gynaecol. Obstet. 2006, 92, 27–31.
- B-Lynch, C.; Keith, L.G.; Campbell, W.B. Internal iliac (hypogastric) artery ligation. In A Textbook of Postpartum Hemorrhage A Comprehensive Guide to Evaluation, Management and Surgical Intervention, 1st ed.; B-Lynch, C., Keith, L.G., Lalonde, A.B., Karosmi, M., Eds.; Sapiens Publishing: London, UK, 2006; pp. 299–307.
- Standring, S. Gray’s Anatomy, 42nd ed.; The Anatomical Basis of Clinical Practice; Elsevier: Amsterdam, The Netherlands, 2020; Chapter 71; pp. 1248–1249.
- de Treigny, O.M.; Roumiguie, M.; Deudon, R.; de Bonnecaze, G.; Carfagna, L.; Chaynes, P.; Rimailho, J.; Chantalat, E. Anatomical study of the inferior vesical artery: Is it specific to the male sex? Surg. Radiol. Anat. 2017, 39, 961–965.
- Bekavac, I.; Kupesic, S.; Mihaljevic, D.; Kurjak, A. Vascular impedance of uterine, inferior vesicle, and ophthalmic arteries in postmenopausal women receiving hormonal replacement therapy: Comparative Doppler study. Croat Med. J. 2000, 41, 235–239.
- Ercoli, A.; Delmas, V.; Fanfani, F.; Gadonneix, P.; Ceccaroni, M.; Fagotti, A.; Mancuso, S.; Scambia, G. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: A dissection-based comparative study. Am. J. Obstet. Gynecol. 2005, 193, 1565–1573.
- Muallem, M.Z.; Armbrust, R.; Neymeyer, J.; Miranda, A.; Muallem, J. Nerve Sparing Radical Hysterectomy: Short-Term Oncologic, Surgical, and Functional Outcomes. Cancers 2020, 12, 483.
- Holub, Z.; Lukac, J.; Kliment, L.; Urbanek, S. Variability of the origin of the uterine artery: Laparoscopic surgical observation. J. Obstet. Gynaecol. Res. 2005, 31, 158–163.
- Khan, R.; Naidoo, N.; Lazarus, L. Unique vascular patterns of the internal iliac artery and its clinical import in pelvic surgery. Transl. Res. Anat. 2021, 25, 100151.
- Mohammadbaigi, H.; Darvishi, M.; Moayeri, A. Variations of anterior and posterior division of internal iliac artery: A systematic review and clinical implications. Biomed Res. Ther. 2019, 6, 3189–3206.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revisions:
2 times
(View History)
Update Date:
15 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




