You're using an outdated browser. Please upgrade to a modern browser for the best experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Stoyan Kostov | -- | 2116 | 2024-01-13 10:37:46 | | | |
| 2 | Fanny Huang | Meta information modification | 2116 | 2024-01-15 10:23:50 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kostov, S.; Kornovski, Y.; Yordanov, A.; Watrowski, R.; Slavchev, S.; Ivanova, Y.; Ganev, T.; Yalçın, H.; Selçuk, I. Anatomy of Pelvic Autonomic Nerve System. Encyclopedia. Available online: https://encyclopedia.pub/entry/53794 (accessed on 25 December 2025).
Kostov S, Kornovski Y, Yordanov A, Watrowski R, Slavchev S, Ivanova Y, et al. Anatomy of Pelvic Autonomic Nerve System. Encyclopedia. Available at: https://encyclopedia.pub/entry/53794. Accessed December 25, 2025.
Kostov, Stoyan, Yavor Kornovski, Angel Yordanov, Rafał Watrowski, Stanislav Slavchev, Yonka Ivanova, Tosho Ganev, Hakan Yalçın, Ilker Selçuk. "Anatomy of Pelvic Autonomic Nerve System" Encyclopedia, https://encyclopedia.pub/entry/53794 (accessed December 25, 2025).
Kostov, S., Kornovski, Y., Yordanov, A., Watrowski, R., Slavchev, S., Ivanova, Y., Ganev, T., Yalçın, H., & Selçuk, I. (2024, January 13). Anatomy of Pelvic Autonomic Nerve System. In Encyclopedia. https://encyclopedia.pub/entry/53794
Kostov, Stoyan, et al. "Anatomy of Pelvic Autonomic Nerve System." Encyclopedia. Web. 13 January, 2024.
Copy Citation
The pelvic autonomic nerve system is a complex network divided into three parts—the sympathetic, parasympathetic, and enteric nervous systems. The enteric nervous system controls the functions of the gastrointestinal tract and is not associated with the autonomic innervation of the pelvis. Therefore, the sympathetic and parasympathetic nerve plexuses innervate the pelvic viscera. The superior hypogastric plexus (SHP), sympathetic trunk, hypogastric nerves (HNs), and most parts of the inferior hypogastric plexus (IHP) contribute to the sympathetic system of the pelvis.
superior hypogastric plexus
inferior hypogastric plexus
hypogastric nerves
1. Introduction
The pelvic autonomic nerve system is a complex network divided into three parts—the sympathetic, parasympathetic, and enteric nervous systems. The enteric nervous system controls the functions of the gastrointestinal tract and is not associated with the autonomic innervation of the pelvis [1]. Therefore, the sympathetic and parasympathetic nerve plexuses innervate the pelvic viscera [2]. The superior hypogastric plexus (SHP), sympathetic trunk, hypogastric nerves (HNs), and most parts of the inferior hypogastric plexus (IHP) contribute to the sympathetic system of the pelvis. In contrast, the pelvic splanchnic nerves (PSNs) (arising from the S2–S4 anterior sacral roots) provide the parasympathetic innervation of the pelvis. The IHP is an intricate plexus, which is formed by the HNs (mainly sympathetic and secondarily parasympathetic innervation), pelvic splanchnic nerves (parasympathetic), and sacral splanchnic nerves (sympathetic innervation from multiple tiny nerve fibers originating from the sacral sympathetic ganglions of the sympathetic trunk) [3][4][5][6][7]. Gynecologic oncologic procedures such as paraaortic (inframesenteric) or presacral lymphadenectomy and radical hysterectomy are often associated with an injury to the sympathetic and parasympathetic branches of the autonomic nervous system [6][7]. Injury to the pelvic autonomic nervous system leads to long-term postoperative complications such as urinary, anorectal, or sexual dysfunction (e.g., reduced vaginal lubrication and libido) [6][8]. Therefore, nerve-sparing procedures have gained increasing recognition in gyneco-oncological surgery [7][9][10][11][12]. Studies have reported that nerve-sparing radical hysterectomy (type C1) is associated with a similar oncological outcome compared to conventional radical hysterectomy (type C2). Moreover, the nerve-sparing procedure is associated with minimized surgical-related pelvic dysfunction [13][14]. Despite recent surgical developments in nerve-sparing radical pelvic surgery (especially radical hysterectomy), the rate of postoperative complications and quality of life remain unsatisfactory [12]. The reason could be the complex anatomy of the IHP and difficulties in the dissection and preservation of the IHP with its branches to the target organs.
2. Anatomical Nomenclature for the Parametrium
Terms such as “superior” versus “inferior”, “anterior” versus “posterior”, and “medial” versus “lateral” will be used. The terms superior and inferior define the anatomical aspect in the surgical supine position.
The term “parametrium”, which refers to the fatty lymphoid tissue around the uterus (including the uterine body and cervix), defines three parametria—lateral, ventral, and dorsal parametria [15].
The lateral parametrium consists of the parauterine tissue (above the ureter) and paracervix tissue (below the ureter). The parauterine tissue, also known as the “uterine pedicle”, contains the uterine artery and the superficial uterine vein with the fatty lymphoid tissue. The paracervix (below the ureter) is separated by the vaginal vein (a synonym of the deep uterine vein) into a cranial part (pars vasculosa) and a caudal part (pars nervosa). The pars vasculosa may contain the branches of the internal iliac system (vaginal artery and inferior vesical artery) in addition to the vaginal or uterine vein. In contrast, the pars nervosa contains pelvic splanchnic nerves and the posteroinferior part of the IHP [7][15].
The dorsal parametrium consists of the uterosacral ligament; its superior (cranial) part is called the rectouterine ligament, and the inferior (caudal) part is called the rectovaginal ligament [4][11][15].
The ventral parametrium includes the vesicouterine ligament (VUL), which is medial and superior (anterior) to the distal ureter, and the vesicovaginal ligament (VVL), which is lateral and inferior (posterior) to the distal ureter. The term “vesicouterine ligament posterior leaf” can also be used as a synonym for the VVL [15].
The mesoureter is a mesentery-like structure containing fatty tissue, the HN, and the posterior part of the IHP. The mesoureter is located inferior (posterior in classical anatomical position) to the ureter and defines the lateral part of the dorsal parametrium [15]. The term “ureterohypogastric fascia” can also be used as a synonym for the mesoureter [11].
The paravaginal veins contribute to the structure of the VVL. They have been termed “inferior vesical veins” or “middle and inferior vesical veins” by different authors [4]. Researchers prefer the term “paravaginal veins”. The vaginal vein (VV) is equal to the deep uterine vein, which drains the vaginal and vesical venous plexuses as a single tributary [4][9][11][15].
The paracolpium is described as a distinct fatty lymphoid anatomical structure adjacent to the vagina and inferior to the distal ureter. The VVL lies at the superolateral part of the paracolpium, close to the bladder, and the VVL is intertwined with the paracolpium. The VVL-paracolpium border contains the paravaginal veins and the bladder nerve branches (BNBs) of the IHP. The paravaginal veins lie parallel to the paracolpium and drains into the vaginal vein [4][5][15].
3. Anatomy of Pelvic Autonomic Nerve System (Hypogastric Plexus)
3.1. Superior Hypogastric Plexus
The SHP is a retroperitoneal structure, formed caudal to the level of the inferior mesenteric artery origin and located slightly to the left of the midline. The SHP lies anterior to the aortic bifurcation and the left common iliac vein at the level of the sacral promontory/fifth lumbar vertebra body, between the left and right common iliac arteries [2][5]. Generally, the lower part of the SHP is located posterior to the sigmoid mesocolon at the right part of the superior rectal artery [5]. In 60% of cases, the SHP terminates at the sacral promontory, whereas in 40% of patients, it ends above the distal portion of the S1 vertebra body [6]. Variations in the morphology (condensation of nerves and shape) of the SHP are often encountered: a plexiform structure, two distinct nerves, a thick single nerve, a broadened band-like nerve trunk, etc. [1][2][16][17]. A dissection of the SHP from the posterior parietal peritoneum and loose connective tissue is usually straightforward [5]. The SHP is derived from two lateral roots and one median root. The median root of the SHP is the direct caudal continuation of the preaortic plexus (superior, intermesenteric, and inferior mesenteric plexuses) [2]. The lateral roots of the SHP are sympathetic and parasympathetic. The sympathetic root represents the lumbar splanchnic nerves, L3-4, which run through the lumbar ganglia of the sympathetic trunk on both sides. Interestingly, the parasympathetic pelvic splanchnic nerves (PSNs) also contribute to the formation of the SHP. These nerves have a cranial direction from the IHP via both the left and right hypogastric nerves [5]. In addition, the median root of the SHP, as the caudal continuation of the preaortic plexus, also contains sympathetic and parasympathetic fibers [2][5][16][17].
3.2. Hypogastric Nerves
The hypogastric nerves (HNs) are paired nerves representing the direct caudolateral continuation of the SHP. Their origin (at the level of or above the sacral promontory) and morphology (either a distinct bundle of nerve fibers or a network of multiple thin nerve fibers) vary among the human population [1][6][7]. After originating from the SHP, the HNs run anterolateral to the presacral fascia and medial to the internal iliac vascular system. The HNs attach to the presacral fascia through the lateral ligaments of the rectum. After descending into the pelvis, the HNs pass approximately 5–20 mm infero-medially to the ureter and laterally to the rectovaginal ligament to enter the IHP [1][6][7][8]. The presence of an accessory hypogastric nerve is also possible [6]. The HN lies as a part of the mesoureter/ureterohypogastric fascia lateral to the dorsal parametrium (uterosacral ligament) [1][7][8]. Some authors suggested that the HN contains only sympathetic fibers [1]. However, the HNs contain mainly sympathetic fibers (descending from the SHP), but also a few parasympathetic fibers (ascending nerve branches from the pelvic splanchnic nerves and IHP) [1][5][8].
The inferior mesenteric plexus, superior hypogastric plexus, and hypogastric nerves are shown in Figure 1, Figure 2, Figure 3 and Figure 4.
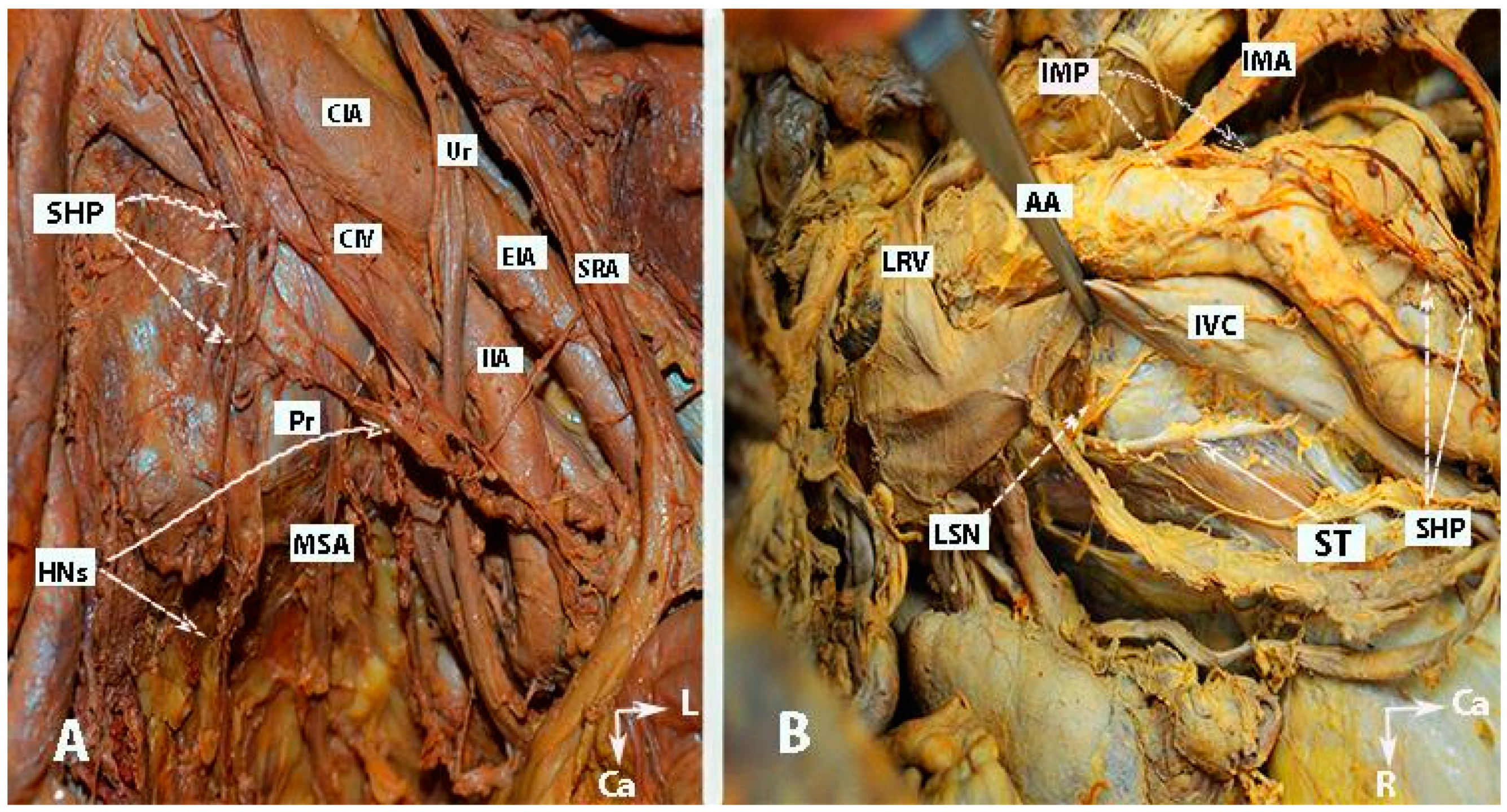
Figure 1. Inferior mesenteric plexus, superior hypogastric plexus, and hypogastric nerves (embalmed cadavers; authors’ own material). The superior hypogastric plexus has a plexiform structure on both figures. (A) Superior hypogastric plexus and hypogastric nerves are shown. (B) Lumbar splanchnic nerves (L3) and sympathetic trunk could be identified. SHP—superior hypogastric plexus; HNs—hypogastric nerves; Pr—promontory; CIA—common iliac artery; Ur—ureter; CIV—common iliac vein; EIA—external iliac artery; IIA—internal iliac artery; SRA—superior rectal artery; MSA—median sacral artery; IMP—inferior mesenteric plexus; IMA—inferior mesenteric artery; LRV—left renal vein; LSN—lumbar splanchnic nerve (L3); ST—sympathetic trunk; IVC—inferior vena cava; Ca—caudal; L—left.
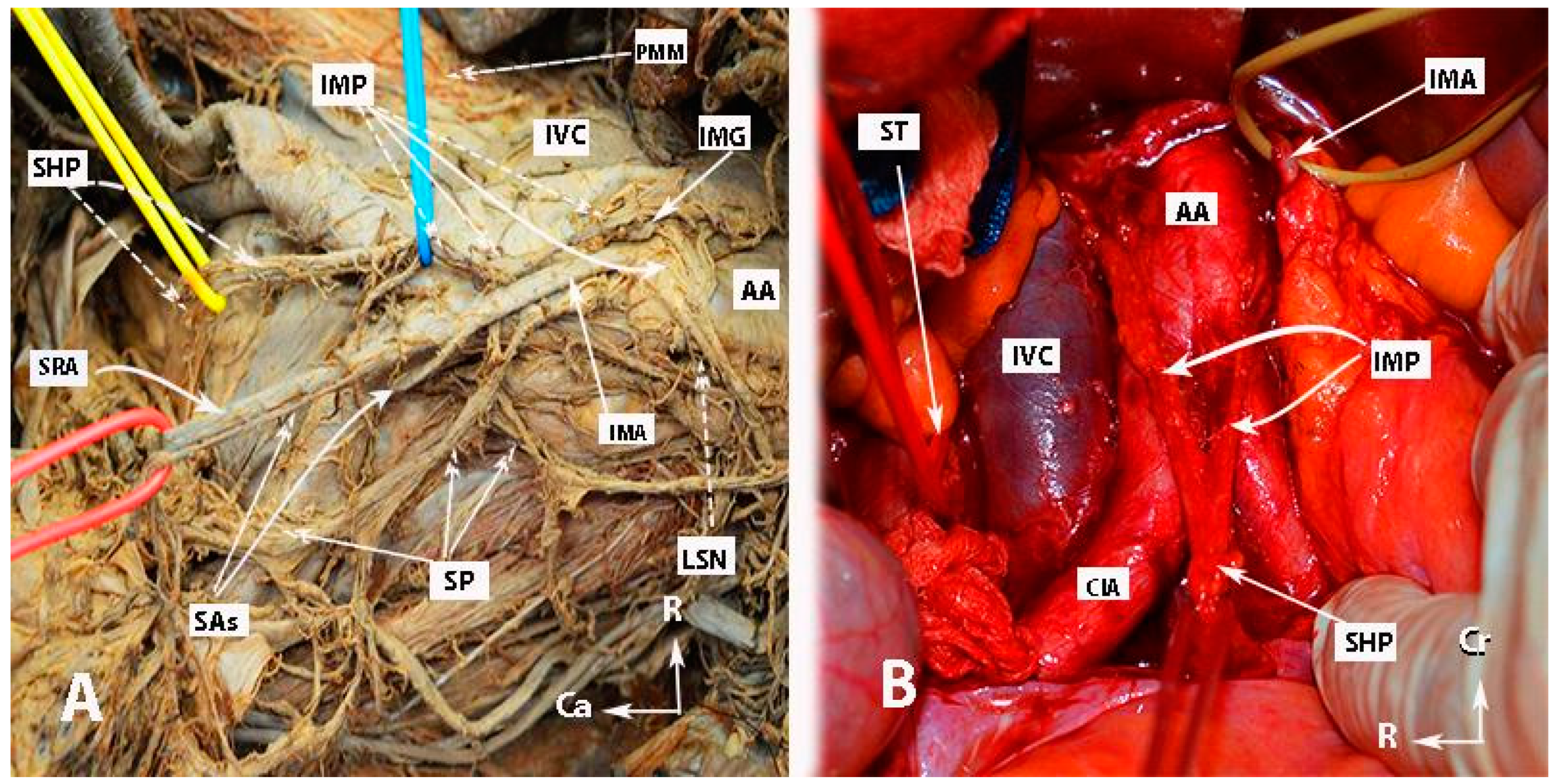
Figure 2. Inferior mesenteric plexus, superior hypogastric plexus, and hypogastric nerves (authors’ own material). (A) Embalmed cadaver; (B) open surgery. The superior hypogastric plexus has the morphology of a broadened band-like nerve trunk in both figures. SHP—superior hypogastric plexus; IMP—inferior mesenteric plexus; PMM—psoas major muscle; IVC—inferior vena cava; AA—abdominal aorta; IMG—inferior mesenteric ganglion; IMA—inferior mesenteric artery; LSN—lumbar splanchnic nerve (L3); SRA—superior rectal artery; SP—sigmoid plexus; Sas—sigmoid arteries; ST—sympathetic trunk marked with vessel loop; CIA—common iliac artery; Ca—caudal; R—right; Cr—cranial.
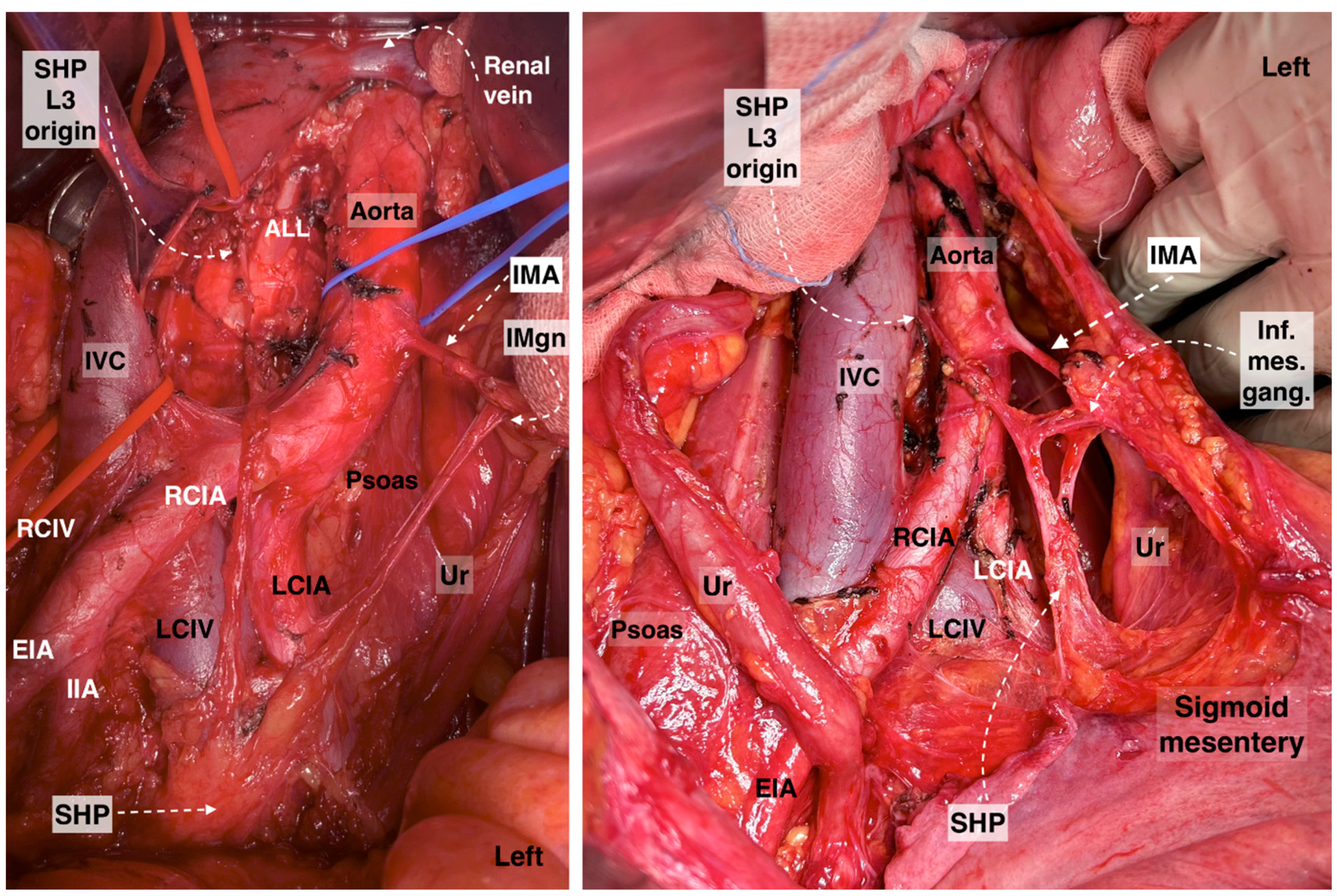
Figure 3. Superior hypogastric plexus, originating from the L3 paravertebral plexus and communicating nerve fibers with the inferior mesenteric ganglion. The caudal extension of the nerve fibers from the thoracic splanchnic nerves was excised during paraaortic lymph node dissection (surgical dissection by author IS) (L: lumbar; IVC: inferior vena cava; RCIA: right common iliac artery; RCIV: right common iliac vein; LCIA: left common iliac artery; LCIV: left common iliac vein; EIA: external iliac artery; IIA: internal iliac artery; IMA: inferior mesenteric artery; ALL: anterior longitudinal ligament; SHP: superior hypogastric plexus; Imgn: inferior mesenteric ganglion; Ur: ureter).
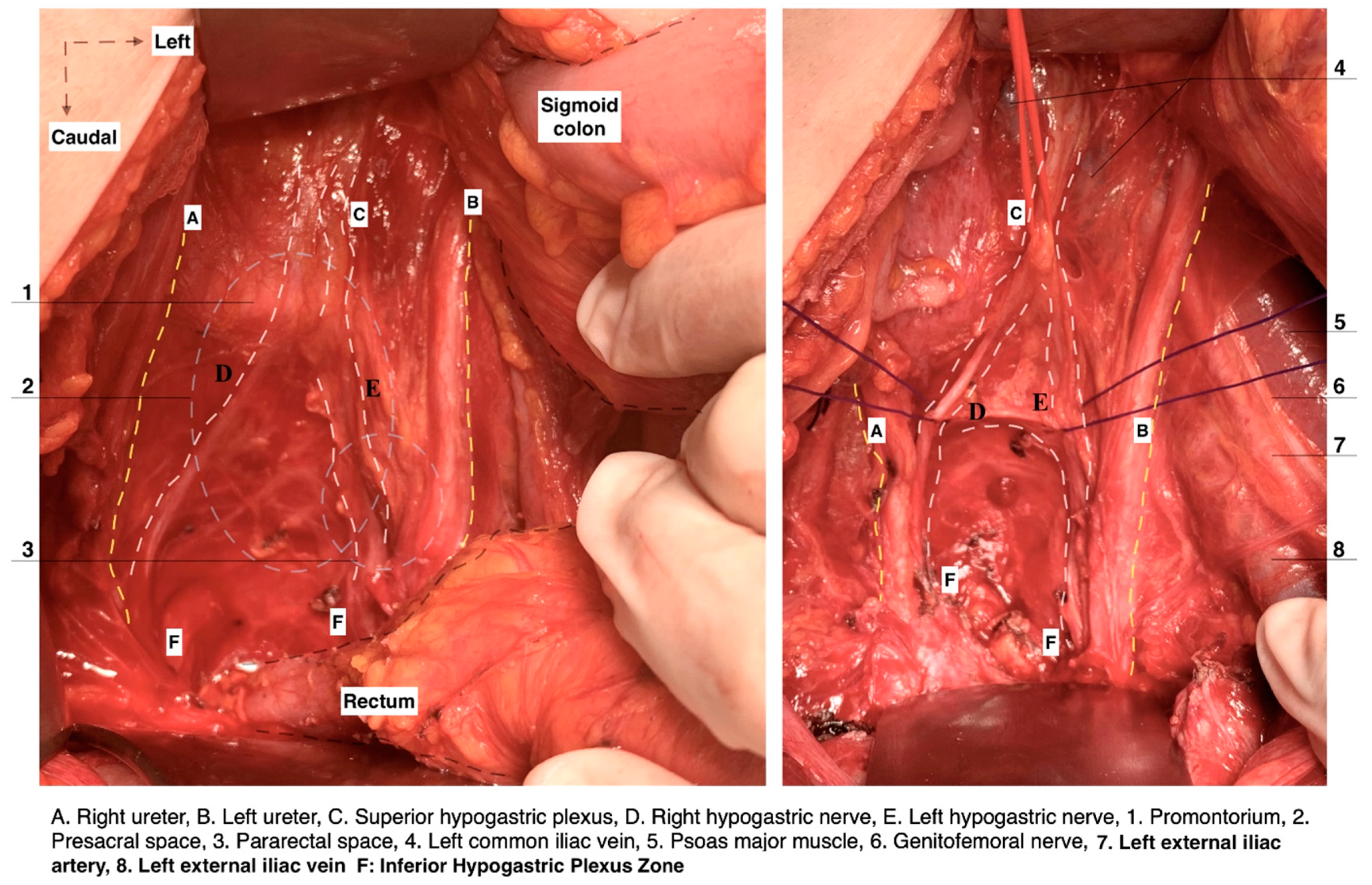
Figure 4. Superior hypogastric plexus lies anterior to the left common iliac vein and is divided into the right and left hypogastric nerves at the retrorectal plane. The hypogastric nerve runs approximately 2 cm posterior to the ureter (surgical dissection by author IS).
3.3. Pelvic Splanchnic Nerves
The PSNs arise from the anterior rami of the sacral roots 2-3-4 (S2–S4) and supply parasympathetic innervation to the pelvic structures via the IHP. As mentioned above, some PSN fibers have an ascending course and pass directly into the HNs and SHP [5][6][7]. Most PSNs have a caudomedial course from the pelvic sidewall at the posterior aspect of the internal iliac vein and cross the pelvic floor to enter into the IHP (3–4 cm lateral and 2–4 cm inferior to the Douglas pouch). In some cases, there is a strict conjunction between the middle rectal vessels and the PSNs [5][6][7]. However, the middle rectal artery is not always present, or it may share the same root with the vaginal and/or inferior vesical artery. The PSNs lie medial to the vesical vessels and run inferior to the vaginal vein (deep uterine vein) to join the IHP at the deep part of the lateral parametrium, also known as the paracervix [4][5][8]. The pathway of the bladder nerve branches of the IHP is thoroughly described during dissection.
3.4. Inferior Hypogastric Plexus
The IHP is also known as the pelvic plexus or pelvic ganglion. It is a bilateral network of nerves, which lies in a sagittal plane slightly anterolateral to the mesorectum, lateral to the vagina and rectum, and posterolateral to the base of the bladder. The IHP can be dissected close to the parietal pelvic fascia [1][3][5][6][7]. The superior part of the IHP is located just below the lateral margin of the rectouterine/rectovaginal ligament within the leaves of the broad ligament retroperitoneally. The inferior part of the plexus is more condensed compared to the superior part [1]. The length (15–40 mm) and thickness (10–30 mm) of the IHP vary in medical literature [1][3][6][7][18][19][20][21]. The IHP can be found along the posterior aspect of the internal iliac artery and vein. Visceral branches related to the internal iliac artery and vein cross the plexus without a direct connection [6][20]. The shape of the plexus has been described as either triangular, quadrangular, or cross-shaped [1][19][20][21]. Mauroy et al. characterized the IHP as a triangle-shaped structure with a posterior base and an antero-inferior top, as well as three edges and angles of the IHP. However, this description seems somewhat speculative [20]. Traditionally, the anatomical description of the IHP has delineated two main plexuses, which are the anterior, comprising the vesical and uterovaginal plexuses, and the postero-medial, rectal plexus [5][6]. However, other authors categorize the IHP into three distinct plexuses: anterior (vesical), intermediate (uterovaginal), and posterior (rectal) [3]. Fuji et al. offered a different view, describing the IHP as being formed by a cross-shaped nerve bundle, with the lateral part being the PSN (S2–S4), medial (uterovaginal plexus), posterior (hypogastric nerve), and anterior bladder nerve branches (BNBs) [21]. In gynecologic-oncological surgery, special attention is paid to the PSNs and the BNBs, since the uterovaginal plexus is transected during uterine removal. On the other hand, the rectal plexus can easily be preserved.
References
- Gässler, J.P.F. Topography of the Ureter and Hypogastric Nerve in Relation to the Mesorectal Fascia and Inferior Hypogastric Plexus. Ph.D. Thesis, Medizinischen Universität Graz, Graz, Austria, 2019.
- Eid, S.; Iwanaga, J.; Chapman, J.R.; Oskouian, R.J.; Loukas, M.; Tubbs, R.S. The Superior Hypogastric Plexus and its Surgical Implications During Spine Surgery: A Review. World Neurosurg. 2018, 120, 143–152.
- Goidescu, O.C.; Dogaru, I.A.; Badea, T.G.; Enyedi, M.; Enciu, O.; Gheoca Mutu, D.E.; Filipoiu, F.M. The distribution of the inferior hypogastric plexus in female pelvis. J. Med. Life 2022, 15, 784–791.
- Sekiyama, K.; Fujii, S.; Mandai, M. Anatomical location of the surgically identifiable bladder branch of the inferior hypogastric plexus for nerve-sparing radical hysterectomy. Gynecol. Oncol. Rep. 2023, 46, 101152.
- Gray, H.; Standring, S.; Hrold Ellis, H.; Berkovitz, B. Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 41st ed.; Elsevier Churchill Livingstone Edinburgh: New York, NY, USA, 2015; pp. 1036–1038.
- Aurore, V.; Röthlisberger, R.; Boemke, N.; Hlushchuk, R.; Bangerter, H.; Bergmann, M.; Imboden, S.; Mueller, M.D.; Eppler, E.; Djonov, V. Anatomy of the female pelvic nerves: A macroscopic study of the hypogastric plexus and their relations and variations. J. Anat. 2020, 237, 487–494.
- Ercoli, A.; Delmas, V.; Gadonneix, P.; Fanfani, F.; Villet, R.; Paparella, P.; Mancuso, S.; Scambia, G. Classical and nerve-sparing radical hysterectomy: An evaluation of the risk of injury to the autonomous pelvic nerves. Surg. Radiol. Anat. 2003, 25, 200–206.
- Alkatout, I.; Wedel, T.; Pape, J.; Possover, M.; Dhanawat, J. Review: Pelvic nerves - from anatomy and physiology to clinical applications. Transl. Neurosci. 2021, 12, 362–378.
- Muallem, M.Z.; Armbrust, R.; Neymeyer, J.; Miranda, A.; Muallem, J. Nerve Sparing Radical Hysterectomy: Short-Term Oncologic, Surgical, and Functional Outcomes. Cancers 2020, 12, 483.
- Ercoli, A.; Cosma, S.; Riboni, F.; Campagna, G.; Petruzzelli, P.; Surico, D.; Danese, S.; Scambia, G.; Benedetto, C. Laparoscopic Nerve-Preserving Sacropexy. J. Minim. Invasive Gynecol. 2017, 24, 1075–1077.
- Yabuki, Y. Twenty-first century radical hysterectomy—Journey from descriptive to practical anatomy. Gynecol. Oncol. Rep. 2020, 34, 100623.
- Derks, M.; Van Der Velden, J.; Frijstein, M.M.; Vermeer, W.M.; Stiggelbout, A.M.; Roovers, J.P.W.; De Kroon, C.D.; Ter Kuile, M.M.; Kenter, G.G. Long-term pelvic floor function and quality of life after radical surgery for cervical cancer: A multicenter comparison between different techniques for radical hysterectomy with pelvic lymphadenectomy. Int. J. Gynecol. Cancer 2016, 26, 1538–1543.
- Roh, J.-W.; Lee, D.O.; Suh, D.H.; Lim, M.C.; Seo, S.-S.; Chung, J.; Lee, S.; Park, S.-Y. Efficacy and oncologic safety of nerve-sparing radical hysterectomy for cervical cancer: A randomized controlled trial. J. Gynecol. Oncol. 2015, 26, 90–99.
- Lee, S.H.; Bae, J.W.; Han, M.; Cho, Y.J.; Park, J.; Oh, S.R.; Kim, S.J.; Choe, S.Y.; Yun, J.H.; Lee, Y. Efficacy of nerve-sparing radical hysterectomy vs. conventional radical hysterectomy in early-stage cervical cancer: A systematic review and meta-analysis. Mol. Clin. Oncol. 2020, 12, 160–168.
- Cibula, D.; Abu-Rustum, N.R.; Benedetti-Panici, P.; Köhler, C.; Raspagliesi, F.; Querleu, D.; Morrow, C.P. New classification system of radical hysterectomy: Emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol. Oncol. 2011, 122, 264–268.
- Paraskevas, G.; Tsitsopoulos, P.; Papaziogas, B.; Natsis, K.; Martoglou, S.; Stoltidou, A.; Kitsoulis, P. Variability in superior hypogastric plexus morphology and its clinical applications: A cadaveric study. Surg. Radiol. Anat. 2008, 30, 481–488.
- Kim, H.; Nam, Y.S.; Lee, U.Y.; Kim, I.B.; Kim, Y.S. Anatomy of the superior hypogastric plexus and its application in nerve-sparing paraaortic lymphadenectomy. Folia Morphol. 2021, 80, 70–75.
- Sakuragi, N.; Kaneuchi, M. Nerve-Sparing Radical Hysterectomy Using the Okabayashi-Kobayashi Method. Surg. J. 2021, 7 (Suppl. S2), S48–S56.
- Bertrand, M.M.; Alsaid, B.; Droupy, S.; Benoit, G.; Prudhomme, M. Optimal plane for nerve sparing total mesorectal excision, immunohistological study and 3D reconstruction: An embryological study. Color. Dis. 2013, 15, 1521–1528.
- Mauroy, B.; Demondion, X.; Bizet, B.; Claret, A.; Mestdagh, P.; Hurt, C. The female inferior hypogastric (=pelvic) plexus: Anatomical and radiological description of the plexus and its afferences—Applications to pelvic surgery. Surg. Radiol. Anat. 2006, 29, 55–66.
- Fujii, S.; Takakura, K.; Matsumura, N.; Higuchi, T.; Yura, S.; Mandai, M.; Baba, T.; Yoshioka, S. Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol. Oncol. 2007, 107, 4–13.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.6K
Revisions:
2 times
(View History)
Update Date:
15 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




