Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Milan Toma | -- | 6462 | 2024-01-08 14:17:23 | | | |
| 2 | Wendy Huang | Meta information modification | 6462 | 2024-01-09 12:37:07 | | | | |
| 3 | Wendy Huang | Meta information modification | 6462 | 2024-01-12 12:29:29 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Bekbolatova, M.; Mayer, J.; Ong, C.W.; Toma, M. The Role of Artificial Intelligence in Medicine. Encyclopedia. Available online: https://encyclopedia.pub/entry/53558 (accessed on 27 February 2026).
Bekbolatova M, Mayer J, Ong CW, Toma M. The Role of Artificial Intelligence in Medicine. Encyclopedia. Available at: https://encyclopedia.pub/entry/53558. Accessed February 27, 2026.
Bekbolatova, Molly, Jonathan Mayer, Chi Wei Ong, Milan Toma. "The Role of Artificial Intelligence in Medicine" Encyclopedia, https://encyclopedia.pub/entry/53558 (accessed February 27, 2026).
Bekbolatova, M., Mayer, J., Ong, C.W., & Toma, M. (2024, January 08). The Role of Artificial Intelligence in Medicine. In Encyclopedia. https://encyclopedia.pub/entry/53558
Bekbolatova, Molly, et al. "The Role of Artificial Intelligence in Medicine." Encyclopedia. Web. 08 January, 2024.
Copy Citation
Artificial intelligence (AI) has emerged as a crucial tool in healthcare with the primary aim of improving patient outcomes and optimizing healthcare delivery. By harnessing machine learning algorithms, natural language processing, and computer vision, AI enables the analysis of complex medical data. The integration of AI into healthcare systems aims to support clinicians, personalize patient care, and enhance population health, all while addressing the challenges posed by rising costs and limited resources.
artificial intelligence
medicine
healthcare
administrative tasks
provider burnout
diagnosis
surgeries
medical imaging
pandemics
medical training
1. Introduction
The origins of AI can be traced back to more than 70 years ago, specifically during World War II. It was during this time that mathematician Alan Turing developed The Bombe, an electro-mechanical computer spanning almost 50 square feet in size. A remarkable feat at the time, The Bombe successfully broke the Enigma code, a task previously believed to be impossible even for the most brilliant human mathematicians [1]. This pivotal moment in history ignited further inquiry into the potential of creating machines capable of incorporating external data and processing it using algorithms to produce useful and efficient outcomes for various tasks. In 1950, Alan Turing examined the possibility of creating intelligent computational machines that could imitate human thought processes. He developed a method known as the Turing test to assess whether a machine’s responses can be distinguished from those of a human [2]. If the machine’s answers are indistinguishable from a human’s, it is considered intelligent. Several years later in 1956, John McCarthy coined the term “Artificial Intelligence”, describing it as the computational aspect of achieving goals and capable of being precisely defined for simulation by machines [3].
Since the inception of AI, this field has experienced rapid advancement. Following its successful demonstration in passing the Turing test, AI began to make significant contributions across various industries. One early adopter was the automotive industry, which witnessed an infusion of AI technology starting in the early 1960s. In particular, John Devol and Joseph Engelberger pioneered the development of Unimate, a groundbreaking industrial robot introduced in 1961. Originally designed for die-casting tasks, it later found application in workpiece handling and spot-welding processes involved in car body manufacturing [4]. Subsequently, advancements were made towards creating conversational systems using chatbots powered by AI algorithms. In 1966, Joseph Weizenbaum introduced Eliza, the first chatbot. Eliza could engage in conversations with humans by utilizing pattern matching to generate appropriate responses based on textual inputs [5]. During the same period, Charles A. Rosen created Shakey, a pioneering achievement that enabled an electronic entity capable of executing complex tasks and identifying errors for correction [6]. These significant milestones played a crucial role in shaping AI’s impact across industries and its subsequent expansion into healthcare applications.
In order to fully comprehend the extent of AI’s contribution to the healthcare industry, an examination of the existing state of medical care is necessary. This includes acknowledging any limitations that can potentially be addressed and resolved through the integration of AI. For example, when patients lack sufficient understanding of medical procedures it hinders their ability to provide informed consent. This inadequacy is mainly attributed to time constraints and a lack of personalization. To address this issue, the utilization of an AI-powered chatbot has been found to improve the informed consent process. In a study, patients were randomly assigned to either a conventional informed consent group or an AI-supported chatbot group [7]. The findings indicated that although satisfaction levels were comparable between the two groups, the AI group exhibited significantly higher levels of accurate comprehension regarding the procedure and its associated risks. The subsequent sections present a comprehensive outline of current challenges within healthcare that stand to benefit from advancements in AI technology.
2. Financial Burdens in Healthcare
Excessive spending poses a significant challenge to the US healthcare system. Previous research indicates that unnecessary costs in the range of USD 760 to 935 billion are incurred annually, which represents almost 25% of the country’s total healthcare budget [8]. This substantial economic burden weighs heavily on the overall US economy and is predominantly due to inefficiencies within the current healthcare system. The integration of AI into this framework has emerged as a potential solution, with projected cost savings of nearly USD 150 billion anticipated by 2026 [9]. These extra funds generated through AI implementation could be directed towards addressing existing healthcare concerns, thereby enhancing patient care quality and improving outcomes for patients overall.
Additionally, the application of AI technologies in healthcare can help ease financial burdens in several ways beyond administrative task automation. (a) Improved Diagnosis and Treatment: AI can help improve the accuracy and speed of diagnosis and treatment, which can result in fewer unnecessary tests and procedures, thereby reducing costs. Additionally, predictive analytics can help prevent disease before it occurs, reducing the need for expensive treatments and hospital stays. (b) Telemedicine: AI can support telemedicine platforms in diagnosing patient symptoms remotely. This reduces costs associated with hospital visits and provides a more affordable and accessible option for patients who may not have easy access to a healthcare facility. (c) Drug Discovery: AI can speed up the drug discovery process, which is typically a lengthy and expensive endeavor. By predicting how different drugs will interact with the body, AI can help identify promising drug candidates more quickly, potentially saving significant research and development costs. (d) Personalized Medicine: AI can analyze individual health data to help healthcare providers tailor treatments specifically to the patient’s genetic and health profile, potentially increasing treatment efficacy and reducing the need for expensive trial-and-error drug prescribing. (e) Resource Allocation: AI can aid in predicting patient inflow in hospitals and clinics. This helps in better allocation and utilization of resources, reducing wastage and cost overruns. (f) Predictive Maintenance of Equipment: AI can predict when healthcare equipment needs maintenance. Predictive maintenance can help to avoid sudden equipment failures and the costs associated with them, allowing for budgeting of equipment replacement or repair. (g) Insurance Fraud Detection: AI can be used to identify false insurance claims, which can result in significant cost savings for healthcare providers and insurance companies.
3. Redundant Administrative Tasks
The primary reason for excessive healthcare spending is due to significant allocations towards administrative expenses which encompass various redundant tasks such as reviewing patient records, documenting encounters, and managing medical files [10]. Administrative duties are indispensable in the healthcare system; however, they consume a substantial amount of time and effort that could otherwise be dedicated to providing direct patient care. On average, nurses in the United States spend 25% of their working hours on administrative tasks [11]. While it remains crucial for healthcare professionals to attend to these essential responsibilities, there exists an opportunity to enhance efficiency through the utilization of AI. AI has the potential to automate and streamline healthcare administrative systems, reducing the burden on healthcare providers and optimizing processes [12]. In the emerging era, AI has exhibited a remarkable ability to efficiently carry out administrative functions on par with human capabilities [13]. While it cannot completely supplant the indispensable role of humans in healthcare management, AI presents an opportunity to optimize and streamline these operations, thereby assisting providers in their day-to-day administrative responsibilities. By delegating repetitive organizational tasks to automated systems, valuable time can be liberated for meaningful patient-care interactions. Furthermore, AI can improve accuracy and reduce errors in administrative tasks such as reviewing patient records and managing medical files [14].
4. Provider Burnout
An increasingly prevalent issue in modern healthcare systems is the phenomenon of provider burnout. Studies have found that burnout is a prevalent issue among healthcare professionals, including physicians and other workers in the field [15]. This syndrome can have detrimental effects on mental well-being as well as on the quality and safety of patient care. To mitigate the effects of burnout and improve the overall well-being of healthcare providers, it is crucial to address the contributing factors that lead to burnout, such as excessive workload and burdensome administrative tasks. Provider burnout refers to a chronic stress reaction that arises from emotional exhaustion, mental health decline, and feelings of depersonalization experienced by healthcare professionals due to systemic and organizational factors [16]. According to recent research findings, approximately 25.6% of physicians reported experiencing symptoms associated with burnout [17]. Interestingly, it was discovered that EHR systems played a significant role in contributing to these symptoms, as indicated by 74.5% of survey respondents attributing EHR as the primary cause [17]. Recognizing the critical impact on patient well-being, it becomes essential to acknowledge the importance of maintaining good physical and mental health among healthcare providers who must perform at their utmost capacity to ensure high-quality care delivery. The issue of burnout among healthcare providers remains a persistent challenge for healthcare organizations globally. Efforts are currently underway to address this issue, including the introduction of natural language processing (NLP)-based AI systems [18]. These NLP analytics can generate insights and analyze patient data on a large scale, offering opportunities to optimize electronic health record systems cost-effectively and efficiently [19]. While integrating NLP in EHR requires continued effort and improvement, the potential benefits of increased efficiency and decreased provider burnout serve as strong motivation for further advancements in this area.
5. Diagnosis and Clinical Decision Making
The application of AI in the field of medical diagnosis and treatment is not a new concept. Researchers have been exploring whether AI can accurately suggest clinical diagnoses and recommend optimal treatment plans since the 1970s. The ability to improve the accuracy of clinical diagnoses is seen as an appealing aspect of AI in medicine, as early and precise detection of medical conditions may lead to better patient outcomes by reducing readmission rates, preventing progression to chronic conditions, and improving prognosis with a lower risk for complications. Currently, various subspecialties are showing growing interest in developing advanced AI tools that could assist with clinical problem-solving. These tools can analyze large amounts of medical data, including patient records [20], lab results, and imaging data, to identify patterns and correlations that might not be immediately apparent to human clinicians. Thus, the use of AI in clinical decision-making is based on its ability to analyze a vast amount of patient data and identify patterns that can accurately predict clinical outcomes and recommend appropriate treatments. AI algorithms are capable of examining various types of medical information, including radiographic images, laboratory results, and patient records, to assist healthcare professionals in recognizing abnormal patterns indicative of specific diagnoses. Machine learning, an integral component of AI, plays a crucial role in clinical decision-making by analyzing data to make informed decisions and predictions [21]. Deep learning (DL), a subfield within ML, has demonstrated considerable success in diagnosing heart failure (HF). In light of the significant global burden posed by HF, which affects approximately 26 million individuals worldwide, the achievements of DL hold great importance in the healthcare context [21][22].
The integration of ML in the field of orthopedics has shown promising outcomes, as AI can provide valuable assistance to orthopedic surgeons by analyzing radiographic images, conducting preoperative risk assessments, and aiding in clinical decision-making [23]. Particularly for joint arthroplasty, which is a common elective procedure in orthopedics, AI offers significant advantages over traditional methods. By utilizing advanced vision models, sensors, and feedback mechanisms during robot-assisted arthroplasty surgery with augmented intelligence capabilities, AI technology demonstrates superior performance in achieving precise joint alignment and accurate implant placement tailored to individual patients’ needs. This patient-centered approach sets AI-driven augmentation apart from conventional techniques and establishes it as the future direction for arthroplasty procedures [24].
An interdisciplinary application of ML lies in cancer diagnostics, risk stratification, and prognosis [25][26]. These aspects play a crucial role in comprehending the progression of diseases and determining survival probabilities. In the past, medical professionals heavily relied on their expertise acquired through years of clinical practice to guide the diagnosis and treatment of cancer. However, traditional methods have shown limitations such as clinical errors and higher rates of misdiagnosis. By incorporating ML algorithms into oncology practices, there is potential to mitigate these challenges, as AI algorithms have demonstrated superiority in early cancer detection compared to conventional approaches [27][28]. Furthermore, the integration of AI in oncology has shown promising prospects for enhancing success rates in cancer treatments by tailoring therapies based on individual genetic information and patient-specific data [29].
AI algorithms have the ability to conduct clinical screenings for disease symptoms, allowing for an assessment of the probability prior to a diagnosis being made by a healthcare professional. One notable example of this is seen in the identification of Diabetic Retinopathy (DR), where several AI screening tools have been created and are now available for use in certain countries. In the past, identifying DR relied solely on human clinicians or graders [30]. However, deep learning screening tools can accurately classify individuals with DR at a statistically significant rate of 96.8% [31]. By making these automated screening tools accessible to the public, it becomes possible to initiate an appropriate follow-up plan with a clinician much more quickly, thereby reducing the chances of complications resulting from undiagnosed DR.
Numerous endeavors in the past and present have demonstrated AI’s capacity to excel in clinical decision-making across various healthcare domains. In these instances, AI has successfully matched the vast knowledge and expertise of healthcare practitioners. However, it is crucial to recognize that the application of AI as both a diagnostic and treatment tool remains in its experimental stages and is not yet widely accessible for use within clinical settings. The widespread integration of AI into healthcare systems remains an additional hurdle on the path toward achieving full automation. The widespread integration of AI in clinical decision-making is expected to occur within the next 5–10 years. However, this timeline relies on obtaining approval from governing stakeholders, standardizing system operations, educating current professionals, and securing adequate funding [9]. It is important to note that AI currently does not pose an immediate threat to the job security of healthcare professionals, as their expertise remains crucial for providing the human touch in medicine [9]. The development of advanced clinical AI technology aims to enhance physicians’ diagnostic abilities and offer optimal treatment plans rather than replace them entirely.
Physical disabilities are increasingly prevalent with advancing age, and rehabilitation plays a crucial role in restoring function and maintaining independence. However, the limited availability and accessibility of rehabilitation services have hindered their clinical impact. While AI has revolutionized several healthcare domains, its potential in rehabilitation remains uncertain. To address this gap, a systematic review of AI-supported physical rehabilitation technology in the clinical setting was conducted in [32]. The authors’ objectives were to assess the availability of AI-supported physical rehabilitation technology, evaluate its clinical effects, and identify barriers and facilitators to implementation. They identified 28 projects encompassing five categories of AI solutions: app-based systems, robotic devices for function replacement or restoration, gaming systems, and wearables. Among these projects, they analyzed five randomized controlled trials that examined outcomes related to physical function, activity, pain, and health-related quality of life. The results revealed inconsistent clinical effects. Implementation barriers included technology literacy, reliability, and user fatigue, whereas enablers encompassed improved access to rehabilitation programs, remote monitoring of progress, reduced manpower requirements, and lower cost. Hence, while the application of AI in physical rehabilitation is a rapidly growing field, there is a need for more rigorous real-world clinical evaluations and post-implementation experiences in order to fully understand its potential and optimize its benefits. Developers and researchers must strive to conduct robust studies to unlock the true potential of AI in enhancing physical rehabilitation outcomes.
The global prevalence of irritable bowel syndrome (IBS) is approximately 4.1%, leading to decreased quality of life and increased healthcare costs. Current guidelines recommend using symptom-based criteria for diagnosing IBS; however, patients often undergo unnecessary medical interventions. To address this issue, the use of AI in medicine presents a promising solution. This research aims to review the applications of AI in IBS. AI has proven useful in colonoscopy by detecting organic lesions, diagnosing them, and objectively evaluating the procedure’s quality. Additionally, AI has been used to study biofilm characteristics in the large bowel and establish a potential correlation with IBS [33]. Furthermore, an AI algorithm has been developed to analyze specific bowel sounds associated with IBS. Smartphone applications based on AI have been created to aid in monitoring IBS symptoms. From a therapeutic perspective, an AI system has been designed to recommend personalized diets based on an individual’s microbiota. In conclusion, the future of IBS diagnosis and treatment could greatly benefit from the integration of AI. The era of big data has necessitated the use of AI models to effectively handle the abundance of clinical data available. These data have become invaluable resources for machine learning, with DL models gaining prominence in analyzing unstructured data. However, traditional ML models continue to hold significant potential to enhance healthcare efficiency, especially for structured data. While ML models have been widely applied in predicting diagnoses and prognoses for various diseases, their adoption in gastroenterology has been relatively limited compared to traditional statistical models or DL approaches [34].
The prospect of patients reporting their symptoms to AI-powered NLP systems, followed by receiving diagnostic and treatment assistance from these AI systems, represents a promising avenue in healthcare. With the utilization of NLP, patients would have the capability to articulate their symptoms in a conversational manner, providing a comprehensive account of their medical condition. The AI systems would then employ advanced algorithms to process and interpret the information shared by the patients to integrate it with pertinent medical data. This amalgamation of patient-reported data and contextual knowledge would enable the AI systems to generate insightful analyses, potentially aiding physicians in arriving at accurate diagnoses and formulating tailored treatment plans. The integration of AI and NLP in this context has the potential to enhance patient outcomes by streamlining healthcare delivery and empowering healthcare providers with AI-facilitated decision support tools, thereby fostering more efficient and personalized medical care [35].
The application of AI in healthcare with potential benefits extending to the field of nutrition assessment has garnered significant attention in recent years. Nutrition assessment plays a pivotal role in healthcare, as it provides crucial insights into an individual’s dietary intake, nutritional status, and overall health. Digital technologies such as mobile applications and wearable devices have emerged as valuable tools in facilitating the collection and analysis of dietary data. These technologies enable individuals to track their food consumption, monitor nutritional content, and receive personalized recommendations. AI algorithms enhance the capabilities of these digital tools by utilizing ML and data analytics techniques to process and interpret vast amounts of nutrition-related data. This allows for more accurate and timely assessment of nutritional status, identification of dietary patterns, and evaluation of health risks associated with inadequate or excessive nutrient intake [36].
6. Surgeries
The expanding application of AI in the healthcare field has brought about significant changes to surgical practices. Surgeons now have access to advanced robotic systems such as Da Vinci that enable less invasive and more independent procedures [37]. Robots are able to perform surgeries on previously inaccessible or delicate areas, such as neural structures, with improved dexterity, speed, and stability. As a result of these advancements, hospital stays have been shortened, recovery times have accelerated, and patient outcomes have been enhanced in terms of morbidity and mortality rates [38]. A recently developed semi-autonomous surgical robot called Smart Tissue Autonomous Robot (STAR) exhibits greater precision and accuracy than experienced surgeons when it comes to incising and suturing soft tissue [39]. Furthermore, studies have indicated that supervised autonomous robot surgery can outperform traditional manual surgery in complex intestinal anastomosis operations, which demand great skillfulness as well as delicacy from surgeons [37][40].
One of the main challenges in traditional surgery is the lack of uniformity caused by variations in surgical experience, training, and skill levels among physicians. However, advancements such as the above-mentioned STAR have addressed this issue by demonstrating the ability to perform surgeries with greater precision and consistency. The STAR system utilizes three-dimensional techniques that result in more consistent suture spacing and improved resection margins compared to manual procedures. Consequently, this reduces the risk of post-surgical complications arising from variability between surgeons’ performances [41]. Moreover, predicting surgical outcomes becomes challenging due to inconsistencies in patient anatomy. Nevertheless, STAR tackles this challenge effectively by adapting to inter-patient anatomical differences and tissue deformability during surgery through real-time data processing and regular updates to the surgical plan [41]. Advancements made on the development of STAR promise not only enhanced surgical outcomes but also increased predictability and standardization within surgeries.
Surgical procedures are widely acknowledged to pose significant risks to the well-being and safety of patients, primarily due to their unpredictable nature and the potential for human error. The integration of AI into surgical practices has been pursued as a means of addressing these concerns and ensuring enhanced levels of safety. Research indicates that robotic surgery boasts a notably lower mortality rate, with 0.097% compared to manual open surgery’s rate of 0.92% per 10,000 surgeries [42]. Thus, by complementing physicians’ expertise with precise robotic assistance, this technology improves surgical accuracy by approximately 6.4% while reducing surgeons’ workload by up to 44% [43].
In addition to its applications in the operating room, AI technology has the potential to enhance healthcare outcomes by streamlining surgical decision-making and management both before and after surgery. As surgery is a significant and often anxiety-provoking event for patients, surgeons need to provide comprehensive support and counseling throughout the entire process. Conversely, surgical interventions necessitate extensive preparation that can be time-consuming; aside from performing procedures, surgeons must analyze various datasets such as patient scans and lab work to develop intricate surgical plans. Fortunately, AI offers a solution by efficiently processing large amounts of patient data within a short timeframe while generating optimal solutions. This allows surgeons more opportunity to engage in meaningful interactions with their patients [44].
A recent literature review analyzed 46 studies on the applications of AI and ML in spinal surgery [45]. The findings revealed that AI/ML models were accurate, with an average overall value of 74.9%. These models performed well in preoperative patient selection, cost prediction, length of stay, functional outcomes, and postoperative mortality prediction. Regression analysis was the most commonly used application, while deep learning/artificial neural networks had the highest sensitivity score of 81.5%. Despite AI/ML’s relatively recent adoption, as shown by 77.5% of studies being published after 2018 (depicted in Figure 1), the results have been encouraging. The increasing prevalence of Big Data and National Registries suggests that the field of spine surgery will gradually adopt and integrate AI/ML into clinical practices, leading to significant improvements in patient care.
7. Medical Imaging
The introduction of X-ray imaging over 120 years ago revolutionized the way healthcare providers diagnose and treat patients [46]. Since then, advancements in imaging technologies have greatly enhanced the medical field by providing a detailed visualization of vital patient anatomy that is not perceptible to the human eye alone. Despite these innovations, modern imaging technology continues to rely on high-quality images and skilled practitioners to accurately interpret and identify potential ailments [47]. An important development occurred approximately 50 years ago when AI capabilities expanded beyond data analysis and problem-solving to include image recognition and interpretation with a lower error rate compared to radiologists [48][49]. However, it is crucial to dispel public apprehension, as AI does not aim to replace the expertise of radiology professionals with robotic systems; rather, it complements their skills within this discipline. The integration of AI in radiology has gained significant attention, and is expected to enhance the diagnostic process by supplementing radiologists with AI algorithms. This approach aims to streamline operations, reduce redundancy, and improve accuracy in image interpretation [50]. During the COVID-19 pandemic, AI proved invaluable in detecting asymptomatic individuals infected with SARS-CoV-2 on CT scans, allowing radiologists to confidently rule out the disease [51][52]. The use of AI visual recognition tools has played a crucial role in preventing transmission through false negative results. As shown in Figure 1, there has been a noticeable surge of interest among researchers studying the applications of AI technology to medical imaging in recent years [53].
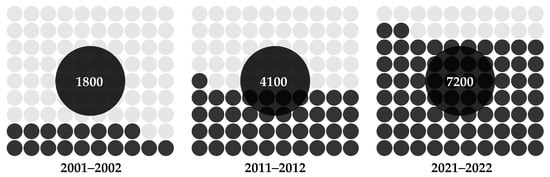
Figure 1. Trends in the number of PubMed-indexed publications on AI in medical imaging.
AI plays a vital role in automating echocardiographic analysis, aiding in the diagnosis of cardiovascular diseases. A recent literature review discussed AI algorithms used in various stages of analysis, including image acquisition, view classification, cardiac chamber segmentation, and quantification of cardiac structure and function [54][55]. The researchers found that such AI models demonstrate high accuracy in comparison to human experts. The same research explored the potential benefits and limitations of AI in healthcare, such as the need for larger datasets and to address algorithm biases to allow for wider clinical adoption.
Endoscopic ultrasound (EUS) has emerged as a widely utilized diagnostic tool for digestive diseases. With the gradual recognition of AI in healthcare, its superiority in the field of EUS has become increasingly evident. Research findings demonstrate that EUS-AI exhibits superiority, or at least equivalence, to conventional methods of diagnosis, prognosis, and quality control for subepithelial lesions, early esophageal cancer, early gastric cancer, and various pancreatic diseases, including pancreatic cystic lesions, autoimmune pancreatitis, and pancreatic cancer [56]. The implementation of EUS-AI has opened up new avenues for individualized precision medicine while introducing innovative approaches to diagnosing and treating digestive diseases.
8. AI’s Role in Pandemics
The COVID-19 pandemic has underscored the potential of AI in effectively addressing healthcare challenges. It spurred the adoption and integration of AI technologies into medical practices, showcasing their ability to facilitate rapid response, accurate diagnosis, efficient treatment, and extensive research endeavors [57]. The increased application of AI in healthcare is evident through the noticeable surge in academic publications. Importantly, this rise coincided with the onset of the COVID-19 pandemic. Throughout this crisis period, various applications of AI played a crucial role in diverse aspects such as pandemic response management, patient care enhancement, and innovative research initiatives. One of the key areas where AI can be utilized during pandemics is in the management of pandemic responses [58]. AI has proved instrumental in disease cluster identification, monitoring patients, determining mortality risk, disease diagnosis and management, contact tracing through geotagging, resource allocation, and data management. The following sections offer an elaboration on these key areas.
8.1. Diagnosis and Screening
In recent years, significant progress has been made in the development of AI-powered diagnostic tools designed to support healthcare professionals in identifying cases of COVID-19 using medical images. These advanced tools utilize convolutional neural networks (CNNs) to carefully examine chest X-rays and CT scans for potential indications of the virus within lung tissue. By analyzing large datasets containing both infected and non-infected images, these AI algorithms are trained to detect subtle patterns that could suggest the presence of COVID-19. This valuable assistance enables radiologists and clinicians to make faster and more precise diagnoses, particularly in regions where PCR testing (i.e., Polymerase Chain Reaction testing, the “gold standard” for COVID-19 tests) may be limited or subject to delays. The ability of AI systems to swiftly process medical images plays a pivotal role in facilitating early detection and treatment plans, ultimately influencing patient outcomes positively and helping to mitigate the spread of the virus [59]. Moreover, AI technology has proven to be beneficial in predicting the progression of COVID-19 cases. By analyzing patterns in symptoms and clinical data, AI algorithms can generate predictive models that help healthcare professionals anticipate how a patient’s condition may develop over time. These predictions guide medical professionals in making informed decisions regarding the appropriate course of treatment and allocation of resources.
8.2. Drug Discovery and Vaccine Development
The integration of AI has significantly transformed the field of drug discovery. By utilizing AI algorithms, scientists are now able to simulate and predict the interactions between potential drugs and viral proteins. This is achieved through molecular docking, a technique that assesses how a drug molecule binds to its target protein. In addition to molecular docking, AI-enhanced molecular dynamics simulations provide valuable insights into the behavior of drug–protein complexes over time. These simulations aid researchers in selecting promising candidates for further testing by offering detailed information on their stability and efficacy. Moreover, AI models have been instrumental in vaccine development [60]. Through advanced prediction techniques, these models can accurately define viral protein structures and analyze potential epitopes that can trigger immune responses. By leveraging such predictions, researchers can design vaccines with greater precision that efficiently elicit strong and protective immune reactions against targeted pathogens. Consequently, this approach has substantially reduced the time required for developing viable vaccine candidates compared to traditional methods. AI has revolutionized the field of drug discovery by enabling researchers to accurately predict drug–protein interactions and efficiently design lead compounds [61]. Furthermore, AI has improved the process of drug development by automating various tasks and reducing the cost and time associated with preclinical and clinical trials.
8.3. Epidemiological Forecasting
AI-powered epidemiological models incorporate intricate data streams for predicting the transmission of the virus. These models analyze factors such as infection rates, hospitalization rates, population density, and human mobility. Machine learning algorithms play a role in refining these models by adapting them to real-world data. By simulating different scenarios based on varying intervention strategies, these models offer policymakers valuable insights into the potential consequences of their actions. Consequently, they aid in resource allocation decisions, inform the implementation of public health measures, and help to mitigate stress on healthcare systems during periods of high demand. AI-powered epidemiological models have become invaluable tools in predicting the transmission of viruses, including COVID-19. Furthermore, AI-based techniques can be utilized to track and monitor the spread of viruses at different scales, ranging from individual to population levels [62].
8.4. Remote Monitoring and Telehealth
AI-enabled remote monitoring tools have emerged as a valuable solution for facilitating patient care from the comfort of home. Through the use of wearable devices, vital signs and symptoms can be continuously tracked to generate streams of data. These extensive datasets are then subjected to AI algorithms that accurately identify any deviations from baseline levels, allowing healthcare providers to promptly address potential declines in patients’ conditions. Additionally, telehealth platforms employ sophisticated chatbots driven by AI capabilities that aid patients in conducting symptom assessments, providing them with relevant information and determining the urgency required for medical attention. By leveraging these advanced systems, healthcare professionals can effectively enhance patient care while simultaneously mitigating unnecessary face-to-face interactions, an especially crucial measure during times such as widespread pandemics [63].
8.5. Data Analysis and Decision Support
The COVID-19 pandemic resulted in a significant influx of data, ranging from the number of cases to hospitalizations to genomic sequences. AI systems have played a crucial role in analyzing these datasets to uncover patterns that contribute to decision-making processes. Machine learning algorithms specifically help to identify risk factors correlated with severe outcomes and demographic trends regarding infections and to evaluate the effectiveness of interventions. The insights derived from these analyses can assist public health officials and policymakers in making well-informed choices, effectively allocate resources, and tailor interventions to cater to specific populations [64].
8.6. Natural Language Processing
Natural language processing techniques facilitate the comprehension and interpretation of human language by AI. In light of the COVID-19 pandemic, NLP tools empowered by AI are capable of systematically sifting through an expansive repertoire of scientific literature to extract significant insights. By summarizing research discoveries and identifying emerging patterns, these advanced tools assist researchers in promptly accessing pertinent information [65]. Furthermore, NLP drives the development of chatbots that deliver precise information to the general public, effectively addressing concerns and countering false or misleading narratives [66].
8.7. Contact Tracing
AI-powered contact tracing applications utilize smartphone technologies such as Bluetooth to monitor and record interactions among individuals. Advanced algorithms powered by machine learning assess the likelihood of disease transmission by considering factors such as proximity, duration, and contextual information [67]. To uphold privacy standards, these apps employ decentralized data storage and cryptographic techniques that safeguard sensitive data from unauthorized access. Through the implementation of AI technology, public health agencies can effectively trace potential infection routes, control outbreaks, and promptly notify individuals who may be at risk [68]. However, it is important to address privacy concerns that arise with the use of AI-powered contact tracing applications. One way to address privacy concerns in AI-powered contact tracing applications is by incorporating privacy-by-design principles [69]. Privacy-by-design principles ensure that privacy is considered at every stage of the design and development process of AI-powered contact tracing applications. By incorporating privacy-by-design principles, contact tracing apps can prioritize user privacy and data protection [70]. Additionally, contact tracing apps can adopt a decentralized approach to data storage. This means that personal data are stored locally on users’ smartphones rather than being collected and stored centrally. This approach enhances privacy, as it minimizes the risk of unauthorized access to sensitive information. Furthermore, adopting an opt-in system for contact tracing apps can help to address privacy concerns. Adopting an opt-in system for contact tracing apps means that users have the choice to voluntarily participate in the app’s functionality. This empowers individuals to make informed decisions about their privacy and control the collection and use of their personal data. Overall, the use of AI-powered contact tracing applications presents significant benefits for public health agencies in controlling disease transmission. However, the collection of personal data and potential surveillance associated with these apps continue to raise valid privacy concerns.
8.8. Patient Triage and Resource Allocation
AI-driven triage systems utilize advanced algorithms to assess patient information such as medical history, symptoms, and laboratory findings in order to anticipate the probability of severe illness [71]. These machine learning models detect early signs of complications, allowing healthcare professionals to prioritize individuals requiring urgent care. In situations where resources are scarce, AI technologies facilitate the efficient allocation of resources by considering predicted patient outcomes; this ensures optimal utilization of critical supplies like ventilators. In addition to patient triage, AI-based systems play a crucial role in resource allocation within hospitals and on a larger scale. By accurately predicting disease severity and patient outcomes, AI-driven triage systems aid in clinical decision-making as well as in the planning and allocation of resources across hospital systems and at the state/country level [72]. Moreover, the use of AI in patient triage and resource allocation becomes particularly vital during pandemics. During the COVID-19 pandemic, AI algorithms demonstrated their effectiveness in predicting patient outcomes and identifying individuals at high risk for severe illness. These AI-powered systems consider a wide range of factors, including pre-existing conditions, laboratory results, and in-hospital data.
9. Medical Training
The effectiveness of medical education is closely linked to a doctor’s ability to provide proper care for their patients while minimizing the risk of irreversible errors or harm. As a result, physicians undergo extensive training over several years to acquire a well-rounded set of skills encompassing cognitive, psychomotor, and affective domains. In the past, medical education primarily emphasized the retention of large volumes of complex information for long periods. However, this task has become increasingly challenging in light of the vast amount of new knowledge being generated daily, which surpasses human capacity [73]. The rapid advancement of AI in the medical field has demonstrated the ability to effectively store, analyze, and retrieve medical data, saving clinicians valuable time and energy in patient management and treatment. This integration of cutting-edge technology necessitates a reformation in the education of future healthcare providers in order to align with these recent advancements, particularly the incorporation of AI into medical practice.
One benefit of incorporating AI into medical education is its ability to enhance the efficiency of learning and studying. This in turn reduces the workload for students and provides them with more opportunities to improve their fundamental clinical skills [74]. In an increasingly demanding healthcare industry, it is crucial for medical professionals to have proficient information recall and analysis abilities as well as to possess effective communication skills, manual dexterity in performing clinical tasks, cultural sensitivity, and empathy toward patients. The integration of AI technologies offers a valuable educational resource that streamlines the didactic components of medical training. Consequently, this allows students to prioritize developing their clinical expertise and interpersonal competencies while promoting a compassionate approach within the field of medicine [75]. Additionally, AI in medical education can facilitate the acquisition of practical skills through real-world use of technologies [76]. This can be achieved by incorporating AI-based tools such as intelligent tutoring systems that simulate interactive scenarios for students to practice their clinical decision-making and problem-solving skills
The integration of AI in medical training offers the potential for a more personalized educational experience tailored to meet the individual needs of students, thereby enhancing their overall performance [77]. The utilization of AI has proven effective in analyzing students’ progress and identifying specific areas where knowledge gaps exist. This enables immediate and customized feedback, empowering students to learn at a pace that suits their abilities and preferences [77]. Additionally, AI-powered tools can provide valuable resources for medical education, such as computer-based models, virtual reality simulations, and personalized learning platforms [78]. These resources allow students to experience real-world scenarios in a safe and controlled environment, enabling them to develop practical skills and apply theoretical knowledge.
The incorporation of AI-based virtual reality simulations in medical education can offer significant benefits by providing a safer learning environment for students to refine their clinical skills before entering real-world patient care. This approach allows for practice in common scenarios such as suturing or conducting physical examinations while enabling preparation for rare yet potentially impactful catastrophic events. For example, research has demonstrated the feasibility of simulating Operating Rooms using AI technology, which proved effective in analyzing healthcare professionals’ response to such emergencies and delivering appropriate training on how to handle these unique situations safely and effectively [79]. Furthermore, AI-driven virtual reality simulations have the potential to revolutionize radiology education [80]. With the integration of AI intelligence, radiology simulations in virtual environments can reproduce real-world scenarios and provide learners with immersive, interactive, and realistic training experiences that closely mimic clinical practice.
The incorporation of AI in the field of medicine is yet to be fully realized, resulting in a knowledge and skills gap among clinicians regarding its application in their day-to-day practice. This lack of familiarity with AI hinders clinicians from harnessing its numerous benefits within the medical sector. This is not due to a lack of interest in becoming proficient at utilizing AI on their part; rather, it can be attributed to the limited availability of educational resources for both students and practicing clinicians. A recent experimental study that introduced an AI course specifically designed for fourth year medical students demonstrated promising outcomes, as evidenced by an average score of 97% achieved by the participants [81]. These findings validate the effectiveness of online modules focusing on AI and emphasize the pressing need for additional educational opportunities within current medical training programs. The integration of AI into medical practice requires a thorough understanding of its potential benefits and limitations. This prompts medical educators to teach the best practices of AI as a tool while understanding its limitations [82]. To bridge the knowledge gap and enhance the understanding of AI among medical professionals, medical educators need to develop standardized AI content and incorporate it into medical training pathways [83]. This approach will ensure that medical students and clinicians are equipped with the necessary knowledge and skills to effectively utilize AI in their practice.
References
- Haenlein, M.; Kaplan, A. A Brief History of Artificial Intelligence: On the Past, Present, and Future of Artificial Intelligence. Calif. Manag. Rev. 2019, 61, 5–14.
- Li, L.; Zheng, N.N.; Wang, F.Y. On the Crossroad of Artificial Intelligence: A Revisit to Alan Turing and Norbert Wiener. IEEE Trans. Cybern. 2019, 49, 3618–3626.
- Monett, D.; Lewis, C.W.P.; Thórisson, K.R.; Bach, J.; Baldassarre, G.; Granato, G.; Berkeley, I.S.N.; Chollet, F.; Crosby, M.; Shevlin, H.; et al. Special Issue “On Defining Artificial Intelligence”—Commentaries and Author’s Response. J. Artif. Gen. Intell. 2020, 11, 1–100.
- Gasparetto, A.; Scalera, L. From the Unimate to the Delta Robot: The Early Decades of Industrial Robotics. In Explorations in the History and Heritage of Machines and Mechanisms; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 284–295.
- Shum, H.; He, X.; Li, D. From Eliza to XiaoIce: Challenges and opportunities with social chatbots. Front. Inf. Technol. Electron. Eng. 2018, 19, 10–26.
- Kuipers, B.; Feigenbaum, E.A.; Hart, P.E.; Nilsson, N.J. Shakey: From Conception to History. AI Mag. 2017, 38, 88–103.
- Aydin, F.; Yildirim, O.T.; Aydin, A.H.; Murat, B.; Basaran, C.H. Comparison of artificial intelligence-assisted informed consent obtained before coronary angiography with the conventional method: Medical competence and ethical assessment. Digit. Health 2023, 9, 20552076231218141.
- Shrank, W.H.; Rogstad, T.L.; Parekh, N. Waste in the US Health Care System. JAMA 2019, 322, 1501.
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Elsevier: Amsterdam, The Netherlands, 2020; pp. 25–60.
- Erickson, S.M.; Rockwern, B.; Koltov, M.; McLean, R.M. Putting Patients First by Reducing Administrative Tasks in Health Care: A Position Paper of the American College of Physicians. Ann. Intern. Med. 2017, 166, 659.
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98.
- Kaneda, Y.; Takita, M.; Hamaki, T.; Ozaki, A.; Tanimoto, T. ChatGPT’s Potential in Enhancing Physician Efficiency: A Japanese Case Study. Cureus 2023, 15, e48235.
- TerKonda, S.P.; TerKonda, A.A.; Sacks, J.M.; Kinney, B.M.; Gurtner, G.C.; Nachbar, J.M.; Reddy, S.K.; Jeffers, L.L. Artificial Intelligence: Singularity Approaches. Plast. Reconstr. Surg. 2023; publish ahead of print.
- Alzahrani, A.S.; Gay, V.; Alturki, R.; AlGhamdi, M.J. Towards Understanding the Usability Attributes of AI-Enabled eHealth Mobile Applications. J. Healthc. Eng. 2021, 2021, 5313027.
- Țăranu, S.M.; Ștefăniu, R.; Ștefan Rotaru, T.; Turcu, A.M.; Pîslaru, A.I.; Sandu, I.A.; Herghelegiu, A.M.; Prada, G.I.; Alexa, I.D.; Ilie, A.C. Factors Associated with Burnout in Medical Staff: A Look Back at the Role of the COVID-19 Pandemic. Healthcare 2023, 11, 2533.
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529.
- Tajirian, T.; Stergiopoulos, V.; Strudwick, G.; Sequeira, L.; Sanches, M.; Kemp, J.; Ramamoorthi, K.; Zhang, T.; Jankowicz, D. The Influence of Electronic Health Record Use on Physician Burnout: Cross-Sectional Survey. J. Med. Internet Res. 2020, 22, e19274.
- Yu, P.; Xu, H.; Hu, X.; Deng, C. Leveraging Generative AI and Large Language Models: A Comprehensive Roadmap for Healthcare Integration. Healthcare 2023, 11, 2776.
- Suryanarayanan, P.; Epstein, E.A.; Malvankar, A.; Lewis, B.L.; DeGenaro, L.; Liang, J.J.; Tsou, C.H.; Pathak, D. Timely and efficient AI insights on EHR: System design. AMIA Annu. Symp. Proc. 2020, 2020, 1180–1189.
- Sim, J.-a.; Huang, X.; Horan, M.R.; Stewart, C.M.; Robison, L.L.; Hudson, M.M.; Baker, J.N.; Huang, I.-C. Natural language processing with machine learning methods to analyze unstructured patient-reported outcomes derived from electronic health records: A systematic review. Artif. Intell. Med. 2023, 146, 102701.
- Yasmin, F.; Shah, S.M.I.; Naeem, A.; Shujauddin, S.M.; Jabeen, A.; Kazmi, S.; Siddiqui, S.A.; Kumar, P.; Salman, S.; Hassan, S.A.; et al. Artificial intelligence in the diagnosis and detection of heart failure: The past, present, and future. Rev. Cardiovasc. Med. 2021, 22, 1095.
- Toma, M.; Singh-Gryzbon, S.; Frankini, E.; Wei, Z.A.; Yoganathan, A.P. Clinical Impact of Computational Heart Valve Models. Materials 2022, 15, 3302.
- Myers, T.G.; Ramkumar, P.N.; Ricciardi, B.F.; Urish, K.L.; Kipper, J.; Ketonis, C. Artificial Intelligence and Orthopaedics. J. Bone Jt. Surg. 2020, 102, 830–840.
- Bagaria, V.; Tiwari, A. Augmented Intelligence in Joint Replacement Surgery: How can artificial intelligence (AI) bridge the gap between the man and the machine? Arthroplasty 2022, 4, 4.
- Cellina, M.; Cè, M.; Khenkina, N.; Sinichich, P.; Cervelli, M.; Poggi, V.; Boemi, S.; Ierardi, A.M.; Carrafiello, G. Artificial Intelligence in the Era of Precision Oncological Imaging. Technol. Cancer Res. Treat. 2022, 21, 153303382211417.
- Frascarelli, C.; Bonizzi, G.; Musico, C.R.; Mane, E.; Cassi, C.; Guerini Rocco, E.; Farina, A.; Scarpa, A.; Lawlor, R.; Reggiani Bonetti, L.; et al. Revolutionizing Cancer Research: The Impact of Artificial Intelligence in Digital Biobanking. J. Pers. Med. 2023, 13, 1390.
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges. Cancer Lett. 2020, 471, 61–71.
- Froń, A.; Semianiuk, A.; Lazuk, U.; Ptaszkowski, K.; Siennicka, A.; Lemiński, A.; Krajewski, W.; Szydełko, T.; Małkiewicz, B. Artificial Intelligence in Urooncology: What We Have and What We Expect. Cancers 2023, 15, 4282.
- Bhinder, B.; Gilvary, C.; Madhukar, N.S.; Elemento, O. Artificial Intelligence in Cancer Research and Precision Medicine. Cancer Discov. 2021, 11, 900–915.
- Grzybowski, A.; Brona, P.; Lim, G.; Ruamviboonsuk, P.; Tan, G.S.W.; Abramoff, M.; Ting, D.S.W. Artificial intelligence for diabetic retinopathy screening: A review. Eye 2019, 34, 451–460.
- Ting, D.S.W.; Pasquale, L.R.; Peng, L.; Campbell, J.P.; Lee, A.Y.; Raman, R.; Tan, G.S.W.; Schmetterer, L.; Keane, P.A.; Wong, T.Y. Artificial intelligence and deep learning in ophthalmology. Br. J. Ophthalmol. 2018, 103, 167–175.
- Sumner, J.; Lim, H.W.; Chong, L.S.; Bundele, A.; Mukhopadhyay, A.; Kayambu, G. Artificial intelligence in physical rehabilitation: A systematic review. Artif. Intell. Med. 2023, 146, 102693.
- Vulpoi, R.A.; Luca, M.; Ciobanu, A.; Olteanu, A.; Bărboi, O.; Iov, D.E.; Nichita, L.; Ciortescu, I.; Cijevschi Prelipcean, C.; Ștefănescu, G.; et al. The Potential Use of Artificial Intelligence in Irritable Bowel Syndrome Management. Diagnostics 2023, 13, 3336.
- Kim, H.J.; Gong, E.J.; Bang, C.S. Application of Machine Learning Based on Structured Medical Data in Gastroenterology. Biomimetics 2023, 8, 512.
- Gala, D.; Makaryus, A.N. The Utility of Language Models in Cardiology: A Narrative Review of the Benefits and Concerns of ChatGPT-4. Int. J. Environ. Res. Public Health 2023, 20, 6438.
- Salinari, A.; Machì, M.; Armas Diaz, Y.; Cianciosi, D.; Qi, Z.; Yang, B.; Ferreiro Cotorruelo, M.S.; Villar, S.G.; Dzul Lopez, L.A.; Battino, M.; et al. The Application of Digital Technologies and Artificial Intelligence in Healthcare: An Overview on Nutrition Assessment. Diseases 2023, 11, 97.
- Minamimura, K.; Hara, K.; Matsumoto, S.; Yasuda, T.; Arai, H.; Kakinuma, D.; Ohshiro, Y.; Kawano, Y.; Watanabe, M.; Suzuki, H.; et al. Current Status of Robotic Gastrointestinal Surgery. J. Nippon Med. Sch. 2023, 90, 308–315.
- Ahmed, S.I.; Javed, G.; Mubeen, B.; Bareeqa, S.B.; Rasheed, H.; Rehman, A.; Phulpoto, M.M.; Samar, S.S.; Aziz, K. Robotics in neurosurgery: A literature review. J. Pak. Med. Assoc. 2018, 68, 258–263.
- Opfermann, J.D.; Leonard, S.; Decker, R.S.; Uebele, N.A.; Bayne, C.E.; Joshi, A.S.; Krieger, A. Semi-autonomous electrosurgery for tumor resection using a multi-degree of freedom electrosurgical tool and visual servoing. In Proceedings of the 2017 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Vancouver, BC, Canada, 24–28 September 2017.
- Shademan, A.; Decker, R.S.; Opfermann, J.D.; Leonard, S.; Krieger, A.; Kim, P.C.W. Supervised autonomous robotic soft tissue surgery. Sci. Transl. Med. 2016, 8, 337ra64.
- Kam, M.; Saeidi, H.; Wei, S.; Opfermann, J.D.; Leonard, S.; Hsieh, M.H.; Kang, J.U.; Krieger, A. Semi-autonomous Robotic Anastomoses of Vaginal Cuffs Using Marker Enhanced 3D Imaging and Path Planning. In Lecture Notes in Computer Science; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; pp. 65–73.
- Salman, M.; Bell, T.; Martin, J.; Bhuva, K.; Grim, R.; Ahuja, V. Use, Cost, Complications, and Mortality of Robotic versus Nonrobotic General Surgery Procedures Based on a Nationwide Database. Am. Surg. 2013, 79, 553–560.
- Saeidi, H.; Opfermann, J.D.; Kam, M.; Raghunathan, S.; Leonard, S.; Krieger, A. A Confidence-Based Shared Control Strategy for the Smart Tissue Autonomous Robot (STAR). In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018.
- Gumbs, A.A.; Perretta, S.; d’Allemagne, B.; Chouillard, E. What is Artificial Intelligence Surgery? Artif. Intell. Surg. 2021, 1, 1–10.
- Tragaris, T.; Benetos, I.S.; Vlamis, J.; Pneumaticos, S. Machine Learning Applications in Spine Surgery. Cureus 2023, 15, e48078.
- Bradley, W.G. History of Medical Imaging. Proc. Am. Philos. Soc. 2008, 152, 349–361.
- Giger, M.L. Machine Learning in Medical Imaging. J. Am. Coll. Radiol. 2018, 15, 512–520.
- Currie, G.M. Intelligent Imaging: Artificial Intelligence Augmented Nuclear Medicine. J. Nucl. Med. Technol. 2019, 47, 217–222.
- Tang, X. The role of artificial intelligence in medical imaging research. BJR|Open 2020, 2, 20190031.
- Liew, C. The future of radiology augmented with Artificial Intelligence: A strategy for success. Eur. J. Radiol. 2018, 102, 152–156.
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial intelligence in the diagnosis of COVID-19: Challenges and perspectives. Int. J. Biol. Sci. 2021, 17, 1581–1587.
- Shukla, A.; Ramdasani, U.; Vinzuda, G.; Obaidat, M.S.; Tanwar, S.; Kumar, N. BCovX: Blockchain-based COVID Diagnosis Scheme using Chest X-ray for Isolated Location. In Proceedings of the ICC 2021—IEEE International Conference on Communications, Montreal, QC, Canada, 14–23 June 2021.
- Najjar, R. Redefining Radiology: A Review of Artificial Intelligence Integration in Medical Imaging. Diagnostics 2023, 13, 2760.
- Qayyum, S.N. A comprehensive review of applications of Artificial Intelligence in Echocardiography. Curr. Probl. Cardiol. 2023, 49, 102250.
- Ledzinski, L.; Grzesk, G. Artificial Intelligence Technologies in Cardiology. J. Cardiovasc. Dev. Dis. 2023, 10, 202.
- Huang, J.; Fan, X.; Liu, W. Applications and Prospects of Artificial Intelligence-Assisted Endoscopic Ultrasound in Digestive System Diseases. Diagnostics 2023, 13, 2815.
- M., S.; Chattu, V.K. A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health. Big Data Cogn. Comput. 2021, 5, 41.
- Lauri, C.; Shimpo, F.; Sokołowski, M.M. Artificial intelligence and robotics on the frontlines of the pandemic response: The regulatory models for technology adoption and the development of resilient organisations in smart cities. J. Ambient. Intell. Humaniz. Comput. 2023, 2023, 1–12.
- Mi, D.; Li, Y.; Zhang, K.; Huang, C.; Shan, W.; Zhang, J. Exploring intelligent hospital management mode based on artificial intelligence. Front. Public Health 2023, 11.
- Pun, F.W.; Ozerov, I.V.; Zhavoronkov, A. AI-powered therapeutic target discovery. Trends Pharmacol. Sci. 2023, 44, 561–572.
- Fountzilas, E.; Tsimberidou, A.M.; Vo, H.H.; Kurzrock, R. Clinical trial design in the era of precision medicine. Genome Med. 2022, 14, 101.
- Shakibfar, S.; Nyberg, F.; Li, H.; Zhao, J.; Nordeng, H.M.E.; Sandve, G.K.F.; Pavlovic, M.; Hajiebrahimi, M.; Andersen, M.; Sessa, M. Artificial intelligence-driven prediction of COVID-19-related hospitalization and death: A systematic review. Front. Public Health 2023, 11, 1183725.
- Tan, T.F.; Thirunavukarasu, A.J.; Jin, L.; Lim, J.; Poh, S.; Teo, Z.L.; Ang, M.; Chan, R.V.P.; Ong, J.; Turner, A.; et al. Artificial intelligence and digital health in global eye health: Opportunities and challenges. Lancet Glob. Health 2023, 11, e1432–e1443.
- Datta, D.; Dalmida, S.G.; Martinez, L.; Newman, D.; Hashemi, J.; Khoshgoftaar, T.M.; Shorten, C.; Sareli, C.; Eckardt, P. Using machine learning to identify patient characteristics to predict mortality of in-patients with COVID-19 in south Florida. Front. Digit. Health 2023, 5, 1193467.
- Lösch, L.; Zuiderent-Jerak, T.; Kunneman, F.; Syurina, E.; Bongers, M.; Stein, M.L.; Chan, M.; Willems, W.; Timen, A. Capturing Emerging Experiential Knowledge for Vaccination Guidelines Through Natural Language Processing: A Proof-of-Concept Study (Preprint). J. Med. Internet Res. 2022, 25, e44461.
- Zhang, P.; Kamel Boulos, M.N. Generative AI in Medicine and Healthcare: Promises, Opportunities and Challenges. Future Internet 2023, 15, 286.
- Hong, S.J.; Cho, H. The role of uncertainty and affect in decision-making on the adoption of AI-based contact-tracing technology during the COVID-19 pandemic. Digit. Health 2023, 9, 205520762311698.
- Pasquale, D.K.; Welsh, W.; Olson, A.; Yacoub, M.; Moody, J.; Gomez, B.A.B.; Bentley-Edwards, K.L.; McCall, J.; Solis-Guzman, M.L.; Dunn, J.P.; et al. Scalable Strategies to Increase Efficiency and Augment Public Health Activities during Epidemic Peaks. J. Public Health Manag. Pract. 2023; publish ahead of print.
- Maras, M.H.; Miranda, M.D.; Wandt, A.S. The use of COVID-19 contact tracing app data as evidence of a crime. Sci. Justice 2023, 63, 158–163.
- Barth, S.; Ionita, D.; Hartel, P. Understanding Online Privacy—A Systematic Review of Privacy Visualizations and Privacy by Design Guidelines. ACM Comput. Surv. 2022, 55, 1–37.
- Charkoftaki, G.; Aalizadeh, R.; Santos-Neto, A.; Tan, W.Y.; Davidson, E.A.; Nikolopoulou, V.; Wang, Y.; Thompson, B.; Furnary, T.; Chen, Y.; et al. An AI-powered patient triage platform for future viral outbreaks using COVID-19 as a disease model. Hum. Genom. 2023, 17, 80.
- Hao, B.; Hu, Y.; Sotudian, S.; Zad, Z.; Adams, W.G.; Assoumou, S.A.; Hsu, H.; Mishuris, R.G.; Paschalidis, I.C. Development and validation of predictive models for COVID-19 outcomes in a safety-net hospital population. J. Am. Med. Inform. Assoc. 2022, 29, 1253–1262.
- Wartman, S.A.; Combs, C.D. Reimagining Medical Education in the Age of AI. AMA J. Ethics 2019, 21, 146–152.
- Han, E.R.; Yeo, S.; Kim, M.J.; Lee, Y.H.; Park, K.H.; Roh, H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: An integrative review. BMC Med. Educ. 2019, 19, 460.
- Buabbas, A.J.; Miskin, B.; Alnaqi, A.A.; Ayed, A.K.; Shehab, A.A.; Syed-Abdul, S.; Uddin, M. Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education. Healthcare 2023, 11, 1298.
- Dobey, B.C. Educating Medical Providers in the Era of Artificial Intelligence. J. Physician Assist. Educ. 2023, 34, 168–170.
- Chan, K.S.; Zary, N. Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Med. Educ. 2019, 5, e13930.
- Lum, Z.C. Can Artificial Intelligence Pass the American Board of Orthopaedic Surgery Examination? Orthopaedic Residents versus ChatGPT. Clin. Orthop. Relat. Res. 2023, 481, 1623–1630.
- Qi, D.; Ryason, A.; Milef, N.; Alfred, S.; Abu-Nuwar, M.R.; Kappus, M.; De, S.; Jones, D.B. Virtual reality operating room with AI guidance: Design and validation of a fire scenario. Surg. Endosc. 2020, 35, 779–786.
- Mese, I. The Impact of Artificial Intelligence on Radiology Education in the Wake of Coronavirus Disease 2019. Korean J. Radiol. 2023, 24, 478.
- Krive, J.; Isola, M.; Chang, L.; Patel, T.; Anderson, M.; Sreedhar, R. Grounded in reality: Artificial intelligence in medical education. JAMIA Open 2023, 6, ooad037.
- Wood, E.A.; Ange, B.L.; Miller, D.D. Are We Ready to Integrate Artificial Intelligence Literacy into Medical School Curriculum: Students and Faculty Survey. J. Med. Educ. Curric. Dev. 2021, 8, 238212052110240.
- Aylward, B.S.; Abbas, H.; Taraman, S.; Salomon, C.; Gal-Szabo, D.; Kraft, C.; Ehwerhemuepha, L.; Chang, A.; Wall, D.P. An Introduction to Artificial Intelligence in Developmental and Behavioral Pediatrics. J. Dev. Behav. Pediatr. 2022, 44, e126–e134.
More
Information
Subjects:
Medicine, Research & Experimental
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
915
Revisions:
3 times
(View History)
Update Date:
12 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





