
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alexandra Pons-Riverola | -- | 2291 | 2023-12-29 10:36:37 | | | |
| 2 | Lindsay Dong | Meta information modification | 2291 | 2024-01-02 01:31:18 | | |
Video Upload Options
Modern cancer therapies have achieved a remarkable improvement in overall survival and patients’ quality of life. However, cardiovascular toxicities are still a major concern. A specific Cardio-Oncology unit is key to offering patients with cancer the best approaches to treatment while minimizing adverse cardiac effects. Moreover, this area of medicine requires a large expertise and has limited trials on which to base decision-making. The development of structured Cardio-Oncology programs leads to better patient care and generates scientific evidence that may impact patient’s survival outcomes.
1. Introduction
2. Organization of a Cardio-Oncology Unit
2.1. Objective of the Cardio-Oncology Unit
2.2. Components of Cardio-Oncology Team
2.3. Cardio-Oncology Programs
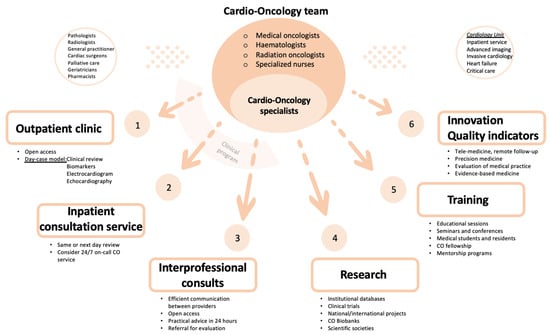
2.3.1. Clinical Program
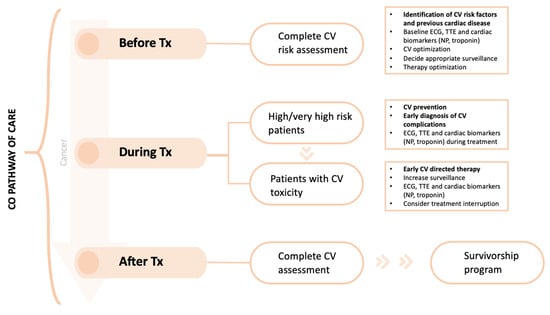
The CO outpatient clinic is the main activity in a CO program. Most CO consultations should be organized as a face-to-face day-case model, which reduces the number of visits to the hospital and avoids treatment delay. The aim of a day-case model is to provide clinical assessment, non-invasive investigations (blood tests with cardiac biomarkers, electrocardiogram and echocardiography) and multidisciplinary discussion on the same day. Invasive cardiac investigations, if appropriate, can be delivered in collaboration with the cardiology department (advanced cardiac imaging and interventional procedures). The virtual outpatient clinic, using a telephone call or videoconferencing, is an option to connect with patients without in person appointment, e.g., to monitor vital signs or to share test results. A CO program can be established taking advantage of existing resources, such as a specialized nursing staff and a heart failure program, thereby patients who develop significant cardiotoxicity could be transferred to HF Unit for a more specific management [12].
2.3.2. Research Program
2.3.3. Training Program
2.3.4. Innovation in Cardio-Oncology
2.3.5. Quality Indicators
2.4. Pathway of Care
3. Conclusions
References
- Koene, R.J.; Prizment, A.E.; Blaes, A.; Konety, S.H. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation 2016, 133, 1104–1114.
- Ameri, P.; Canepa, M.; Anker, M.S.; Belenkov, Y.; Bergler-Klein, J.; Cohen-Solal, A.; Farmakis, D.; López-Fernández, T.; Lainscak, M.; Pudil, R.; et al. Cancer diagnosis in patients with heart failure: Epidemiology, clinical implications and gaps in knowledge. Eur. J. Heart Fail. 2018, 20, 879–887.
- Banke, A.; Schou, M.; Videbaek, L.; Møller, J.E.; Torp-Pedersen, C.; Gustafsson, F.; Dahl, J.S.; Kober, L.; Hildebrandt, P.R.; Gislason, G.H. Incidence of cancer in patients with chronic heart failure: A long-term follow-up study. Eur. J. Heart Fail. 2016, 18, 260–266.
- Moliner, P.; Lupón, J.; de Antonio, M.; Domingo, M.; Santiago-Vacas, E.; Zamora, E.; Cediel, G.; Santesmases, J.; Díez-Quevedo, C.; Isabel, M.; et al. Trends in modes of death in heart failure over the last two decades: Less sudden death but cancer deaths on the rise. Eur. J. Heart Fail. 2019, 21, 1259–1266.
- Nhola, L.F.; Villarraga, H.R. Fundamentos de las unidades de cardio-oncología. Rev. Española Cardiol. 2017, 70, 583–589.
- Ammon, M.; Arenja, N.; Leibundgut, G.; Buechel, R.R.; Kuster, G.M.; Kaufmann, B.A.; Pfister, O. Cardiovascular management of cancer patients with chemotherapy-associated left ventricular systolic dysfunction in real-world clinical practice. J. Card. Fail. 2013, 19, 629–634.
- Parent, S.; Pituskin, E.; Paterson, D.I. The Cardio-oncology Program: A Multidisciplinary Approach to the Care of Cancer Patients With Cardiovascular Disease. Can. J. Cardiol. 2016, 32, 847–851.
- Pareek, N.; Cevallos, J.; Moliner, P.; Shah, M.; Tan, L.L.; Chambers, V.; Baksi, A.J.; Khattar, R.S.; Sharma, R.; Rosen, S.D.; et al. Activity and outcomes of a cardio-oncology service in the United Kingdom-a five-year experience. Eur. J. Heart Fail. 2018, 20, 1721–1731.
- Lancellotti, P.; Suter, T.M.; López-Fernández, T.; Galderisi, M.; Lyon, A.R.; Van der Meer, P.; Cohen, A.; Zamorano, J.L.; Jerusalem, G.; Moonen, M.; et al. Cardio-Oncology Services: Rationale, organization, and implementation. Eur. Heart J. 2019, 40, 1756–1763.
- Barros-Gomes, S.; Herrmann, J.; Mulvagh, S.L.; Lerman, A.; Lin, G.; Villarraga, H.R. Rationale for setting up a cardio-oncology unit: Our experience at Mayo Clinic. Cardiooncology 2016, 2, 5.
- Arjun KGhosh Charlotte Manisty Simon Woldman Tom Crake Mark Westwood, J.M.W. Setting up cardio-oncology services. Br. J. Cardiol. 2017, 24, 1.
- Snipelisky, D.; Park, J.Y.; Lerman, A.; Mulvagh, S.; Lin, G.; Pereira, N.; Rodríguez-Porcel, M.; Villarraga, H.R.; Herrmann, J. How to Develop a Cardio-Oncology Clinic. Heart Fail. Clin. 2017, 13, 347–359.
- Okwuosa, T.M.; Barac, A. Burgeoning Cardio-Oncology Programs: Challenges and Opportunities for Early Career Cardiologists/Faculty Directors. J. Am. Coll. Cardiol. 2015, 66, 1193–1197.
- Sadler, D.; Chaulagain, C.; Alvarado, B.; Cubeddu, R.; Stone, E.; Samuel, T.; Bastos, B.; Grossman, D.; Fu, C.L.; Alley, E.; et al. Practical and cost-effective model to build and sustain a cardio-oncology program. Cardiooncology 2020, 6, 9.
- Brown, S.-A.; Rhee, J.-W.; Guha, A.; Rao, V.U. Innovation in Precision Cardio-Oncology during the Coronavirus Pandemic and Into a Post-pandemic World. Front. Cardiovasc. Med. 2020, 7, 145.
- Aktaa, S.; Batra, G.; Wallentin, L.; Baigent, C.; Erlinge, D.; James, S.; Ludman, P.; Maggioni, A.P.; Price, S.; Weston, C.; et al. European Society of Cardiology methodology for the development of quality indicators for the quantification of cardiovascular care and outcomes. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 4–13.
- Lyon, A.R.; López-Fernández, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Córdoba, R.; Cosyns, B.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J 2022, 43, 4229–4361.
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726.
- Zamorano, J.L.; Lancellotti, P.; Rodriguez Muñoz, D.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.; Lyon, A.R.; et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2768–2801.




