Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Aitor Gonzaga | -- | 2340 | 2023-12-28 09:51:10 | | | |
| 2 | Jessie Wu | + 2 word(s) | 2342 | 2023-12-29 02:33:54 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Soria, B.; Escacena, N.; Gonzaga, A.; Soria-Juan, B.; Andreu, E.; Hmadcha, A.; Gutierrez-Vilchez, A.M.; Cahuana, G.; Tejedo, J.R.; De La Cuesta, A.; et al. Complications of Diabetes and Diabetic Foot. Encyclopedia. Available online: https://encyclopedia.pub/entry/53211 (accessed on 07 February 2026).
Soria B, Escacena N, Gonzaga A, Soria-Juan B, Andreu E, Hmadcha A, et al. Complications of Diabetes and Diabetic Foot. Encyclopedia. Available at: https://encyclopedia.pub/entry/53211. Accessed February 07, 2026.
Soria, Bernat, Natalia Escacena, Aitor Gonzaga, Barbara Soria-Juan, Etelvina Andreu, Abdelkrim Hmadcha, Ana Maria Gutierrez-Vilchez, Gladys Cahuana, Juan R. Tejedo, Antonio De La Cuesta, et al. "Complications of Diabetes and Diabetic Foot" Encyclopedia, https://encyclopedia.pub/entry/53211 (accessed February 07, 2026).
Soria, B., Escacena, N., Gonzaga, A., Soria-Juan, B., Andreu, E., Hmadcha, A., Gutierrez-Vilchez, A.M., Cahuana, G., Tejedo, J.R., De La Cuesta, A., Miralles, M., García-Gómez, S., & Hernández-Blasco, L. (2023, December 28). Complications of Diabetes and Diabetic Foot. In Encyclopedia. https://encyclopedia.pub/entry/53211
Soria, Bernat, et al. "Complications of Diabetes and Diabetic Foot." Encyclopedia. Web. 28 December, 2023.
Copy Citation
Globally, a leg is amputated approximately every 30 seconds, with an estimated 85 percent of these amputations being attributed to complications arising from diabetic foot ulcers (DFU), as stated by the American Diabetes Association. Peripheral arterial disease (PAD) is a risk factor resulting in DFU and can, either independently or in conjunction with diabetes, lead to recurring, slow-healing ulcers and amputations.
mesenchymal stromal cells
MSC
diabetic foot
foot ulcer
charcot foot
amputation
1. The Global Burden of Diabetes Mellitus
Diabetes mellitus is a chronic metabolic disease characterized by elevated levels of blood glucose (hyperglycemia). Persistent hyperglycemia can lead to serious damage to the heart, blood vessels, eyes, kidneys, and nerves. The number of people with diabetes in the world rose from 108 million in 1980 to 422 million in 2014. Prevalence has been rising more rapidly in low- and middle-income countries than in high-income countries as shown in Table 1. The 2023 global burden of Diabetes Mellitus is significant, with about 537 million people worldwide having diabetes [1][2].
Table 1. Prevalence of Diabetes Mellitus (DM) in 2021 and projected prevalence for 2030 and 2045 [2]. In USD millions.
| 2021 | 2030 | 2045 | Increase (%) | |
|---|---|---|---|---|
| Global | 537 | 643 | 783 | 46 |
| Europe | 61 | 67 | 69 | 13 |
| North-America & Caribbean | 51 | 57 | 63 | 24 |
| Western Pacific | 206 | 238 | 260 | 27 |
| South & Central America | 32 | 40 | 49 | 50 |
| Africa | 24 | 33 | 55 | 134 |
| Middle East & North Africa | 73 | 95 | 136 | 87 |
| South East Asia | 90 | 113 | 152 | 68 |
From 2000 to 2019, age-standardized mortality rates from diabetes increased 3% yearly increase mostly in lower-middle-income countries (13%) In contrast, the probability of dying from any one of the four main non-communicable diseases (cardiovascular diseases, cancer, chronic respiratory diseases or diabetes) between the ages of 30 and 70 decreased by 22%. Many people with diabetes develop problems with their feet from nerve damage and poor blood flow. This can cause foot ulcers and may lead to amputation. This research deals with innovative treatments for this unmet medical need: ulcers and amputation of the diabetic foot.
Types of Diabetes
-
Type 1 diabetes (previously known as insulin-dependent, juvenile or childhood-onset) is characterized by deficient insulin production and requires daily administration of insulin. Prevalence of type 1 Diabetes Mellitus in 2017 was approximately 9 million people; the majority of them live in high-income countries.
-
Type 2 diabetes may be due either by insufficient insulin production by the beta cells of the pancreatic islets or by defective action in peripheral tissues (muscle, liver) also called insulin resistance. Combination of both leads to high levels of blood sugar if not treated. Factors that contribute to developing type 2 diabetes include being overweight, not getting enough exercise, and genetics [3].
-
Gestational diabetes, in which there is dysregulated glucose levels is at an increased risk of complications during pregnancy and at delivery. These women and possibly their children are also at increased risk of type 2 diabetes in the future.
-
Monogenic diabetes, directly linked to the mutation of a gene related with the pancreatic beta cell physiology.
2. Economic Burden of Diabetes
Direct costs of diabetes represent approximately 10% of the budget of developed countries [2][4]. The 10 countries or territories with the highest total health expenditure due to diabetes (20–79 years) in 2021 (in USD billion) are shown in Table 2. The projected increase in the global burden of diabetes highlights the need for effective interventions to prevent and manage diabetes and their complications. For example, healthcare costs from patients with peripheral artery disease (PAD) and diabetes have an estimated cost of more than 80 billion USD in the US [5].
Table 2. Direct Cost of Diabetes Mellitus [2].
| Country | Cost (in USD Billion) |
|---|---|
| United States of America | 379.5 |
| China | 165.3 |
| Brazil | 42.9 |
| Germany | 41.3 |
| Japan | 35.6 |
| United Kingdom | 23.4 |
| France | 22.7 |
| Mexico | 19.9 |
| Spain | 15.5 |
| Italy | 14.7 |
3. Complications of Diabetes
Diabetes can cause a range of complications that affect various parts of the body (Figure 1). In fact, although Acute Metabolic complications are more related with type 1 diabetes, the rest are present in both in type 1 and type 2 diabetes. Both the economic cost and death risk depend on complications. Chronic complications may be classified as: microvascular (retinopathy, nephropathy and neuropathy) and macrovascular (infarction, stroke, peripheral artery disease). Complications are heterogeneous, but un-fortunately, it has not been fully characterized the ethnic, genetic and lifestyle linked to specific complications. hospitalizations, and mortality among diabetic patients and contribute significantly to the high costs of diabetes care (Table 2).
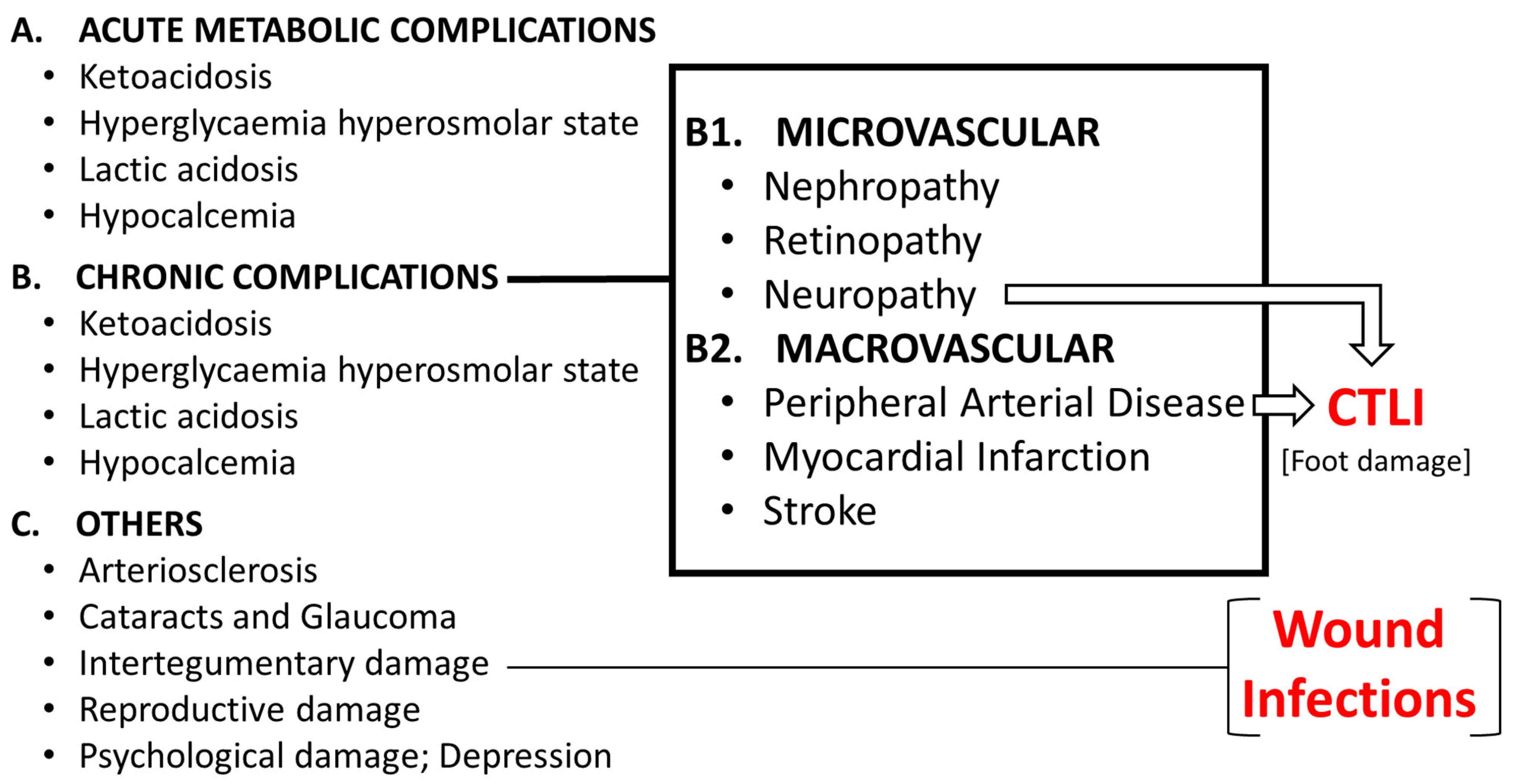
Figure 1. Complications of Diabetes Mellitus. CTLI: Chronic Life Threatening Limb Ischemia (No-Option Chronic Limb Ischemia).
Some of the chronic complications of diabetes include nerve damage (diabetic neuropathy), chronic kidney disease (diabetic nephropathy), eye problems (diabetic retinopathy), foot problems, heart attack, stroke, skin problems, digestive problems, sexual dysfunction, oral and dental problems, etc. These complications can be serious and can lead to amputation, blindness, heart disease, and kidney failure if left untreated. However, with proper management of blood glucose and conventional treatments, many of these complications can be prevented or delayed. This research deals with innovative therapies to treat some of these complications related with PAD, critical limb ischemia (CLI), ulcers and amputations, in fact an unmet medical need.
About 20% of people with diabetes will develop PAD which remains to be a serious public health problem. Estimated prevalence of PAD in 2019 was 113,443,017 people with an annual incidence of 10,504,092 [6] and 11% of people with PAD may end with Chronic Life Threatening Limb Ischemia (CTLI).
Figure 2 summarizes the prevalence and distribution of patients with CTLI (chronic threatening limb ischemia, and CLI with no option of revascularization). Although these figures mostly depend on differences in prevention, evolution and ethnicity. Since there is an estimation of 537 million people with diabetes [2] the risk of CTLI may reach a prevalence of approximately 2.95 million people all over the world (diabetes has a 20% risk of PAD, PAD a 11% risk of CLI and 25% CLI are considered non revascularizable or CTLI).
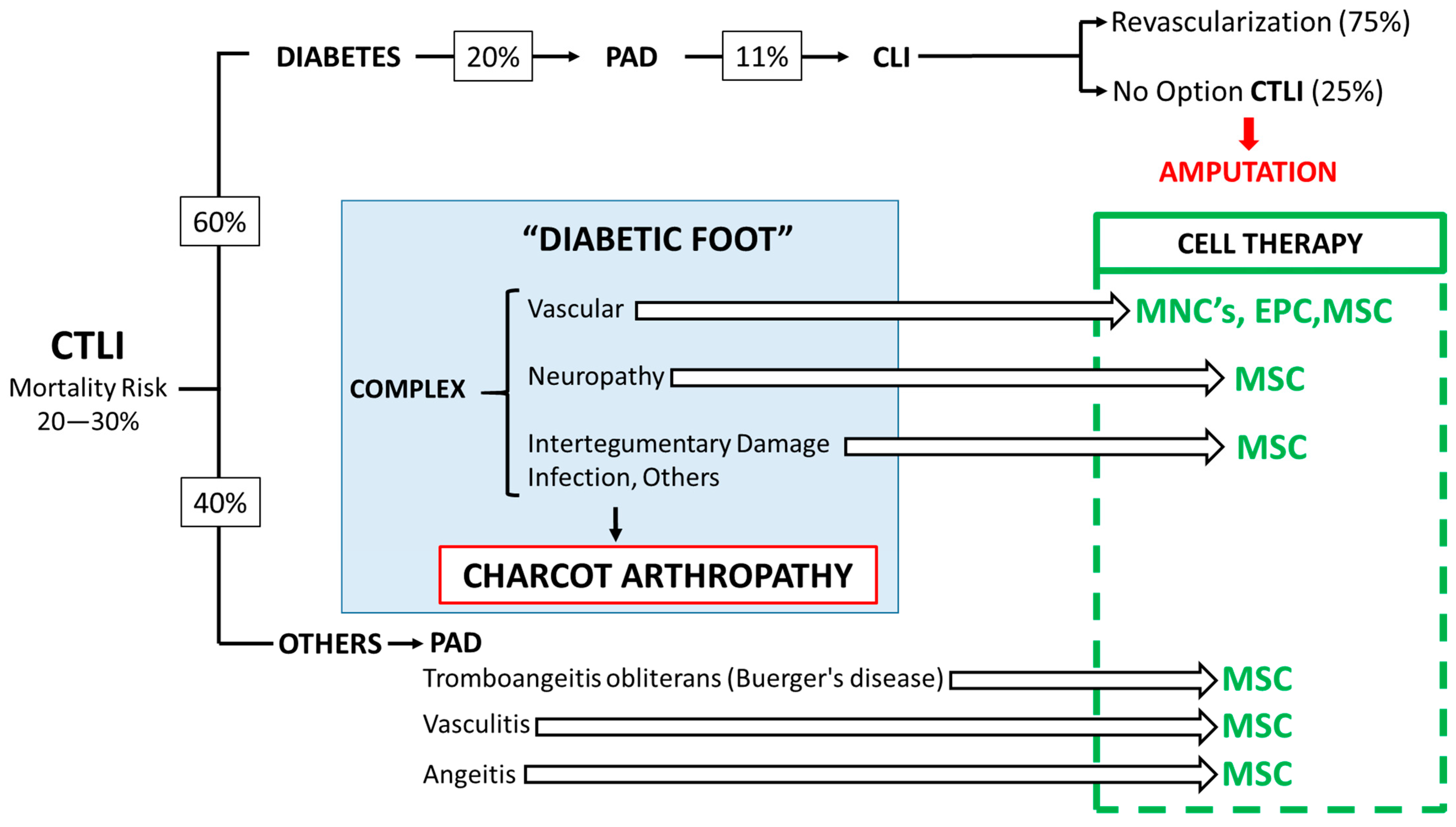
Figure 2. Prevalence and distribution of patients with CTLI. Proposed ATMP treatment depending on the complex nature of the diabetic foot. MNC: Mononuclear Cells, EPC: Endothelial Progenitor Cells, MSC: Mesenchymal Stromal Cells.
Since a high percentage of PAD patients develop CLI and 25% of CLI has no option for Revascularization (chronic threatening limb ischemia, CTLI), the risk for ulcers, amputation and mortality increases substantially. Furthermore, the mortality risk associated with CTLI ranges between 20% and 30%. Then, there is an obvious need to develop novel therapeutic strategies focused in ameliorate limb perfusion and neuropathy together with a decrease in the concomitant inflammatory process. Ulcer healing will be a consequence. However, when Charcot arthropathy and infections appears researchers can only expect a limited response. Although researchers do not have yet an advanced therapy medicinal product (ATMP) approved by regulatory agencies (FDA, EMA, etc.) to treat CTLI and prevent amputation, the amount of results in pilot, Phase I and Phase II studies strongly suggest that a proper segmentation of CTLI patients and the selection of worth primary and secondary endpoints in the Phase III trials will help to establish the profile for Cell Therapy of CTLI. The right side of the Figure 2 summarizes the ATMP cell therapy options.
1.3.1. The Diabetic Foot
Diabetic foot a complex complication in which PAD, neuropathy, arteriosclerosis and intertegumentary damage are related, with a “personal mix” that differs from one to another patient. Diabetes is a significant risk factor for developing CTLI due to PAD. Patients with diabetes concomitant to CLI represent a sub-group at particular risk. CLI appears when a severe obstruction of the arteries markedly reduces blood flow to the extremities and progress to the point of severe pain and even skin ulcers or sores. Unfortunately, vessels affected in diabetic patients are distal, small diameter and profusely distributed making nonviable surgical revascularization. Furthermore, diabetes is associated with decreased limb survival in patients with CLI.
Figure 3 also depicts the concomitant process and tentative biomarkers. A decrease in endothelial progenitor cells (EPC) with reduction on oxygen availability (as measured by transcutaneous oxygen pressure-TcPO2) and ischemic pain is accompanied by an increase in inflammation and the appearance of ulcers.
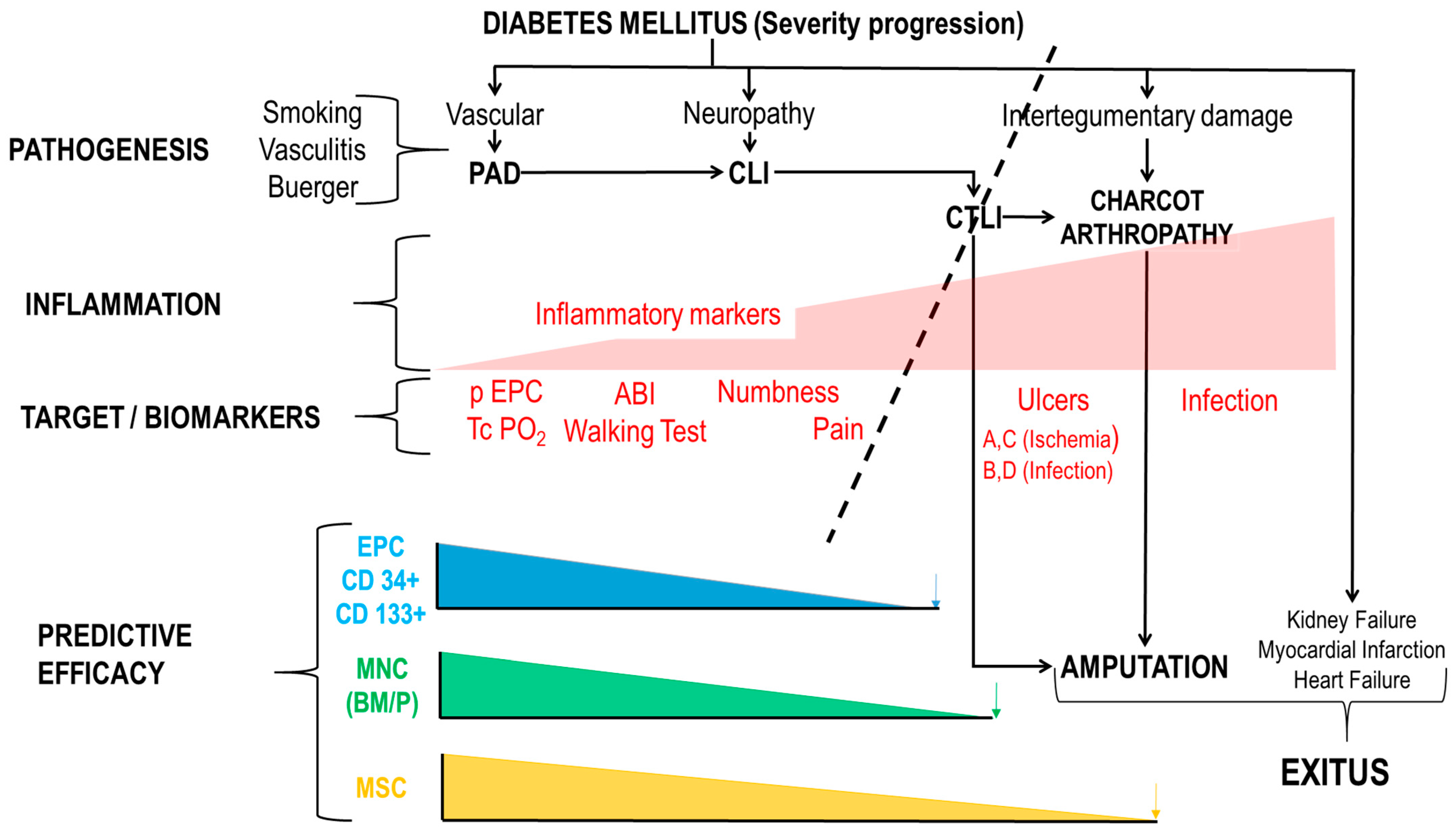
Figure 3. Pathogenesis, target biomarkers and predictive efficacy of AMTPs. PAD: Peripheral Artery Disease. CLI: Critical Limb Ischemia. CTLI: Chronic Life-threatening Limb Ischemia. ABI: Ankle Brachial Index. EPC; Endothelial Progenitor Cells. ABCD; University of Texas Staging System for Diabetic Foot Ulcers. Blue, Green and Orange arrows mean that at that point, outcome is amputation.
CLI characterized by ischemic rest pain, ulcers, or gangrene is the end-stage of PAD, usually associated with a significant risk of affected limb loss and a high risk for cardiovascular events. No-option CLI or CTLI [7][8][9], is an independent risk factor for major amputation in diabetic patients. The annual incidence is approximately 500–1000 new cases per million in industrialized countries [7][10][11]. Then, there are between 0.6 million and 1.36 million people with CTLI per year. According to the World Bank 17% of the world population live in industrialized countries. To note that by 2030, China, Thailand, Mexico and Turkey with join the developed countries, then it is expected that it will be 50% of the world population by 2050. Tobacco, diabetes and age are independent risk factors. Critical threatening limb ischemia grasps for different pathologies: such as Buerger disease, thromboangeitis obliterans and others, but diabetes is in the origin of more than 60% of CTLI. In conclusion, healthcare systems are facing a costly high prevalence threatening situation.
Diabetes is the leading nontraumatic cause of lower limb amputations [12][13]. As a result, neuropathy injuries in their feet and ankles are more frequent and more severe than people without diabetes. Wounds and skin infections heal poorly in persons with diabetes. Endovascular intervention and bypass surgery are the current treatment options [11][14][15][16][17]. However, approximately 20–30% of CLI patients are not eligible for revascularization, or this procedure has failed.
1.3.2. The Complex Nature of the Diabetic Foot
Atherosclerosis in distal arteries in combination with diabetic neuropathy can lead to CLI (Figure 1). The distal nature of the arterial narrowing in CLI is less amenable to revascularization. CLI is the advanced stage of PAD, which results from a progressive thickening of an artery’s lining (caused by atherosclerosis) and narrowing of the vessel, which reduces blood flow to the limbs. Patients with diabetes are more likely than other patients to have distal disease that is less amenable to bypass grafting. Limb salvage after bypass is better for insulin and non-insulin diabetics, compared to the endovascular approach.
The pathogenesis of CLI is complex and involves atherosclerosis, peripheral arterial disease, and other vascular risk factors (Figure 3).
1.3.3. Arthropathy of Charcot
Charcot arthropathy (CA), also known as Charcot foot and Charcot neuroarthropathy, affects the bones, joints, and soft tissues in the feet and ankles, caused by an inability to sense injuries, which can result in significant deformities. Diabetes is the main risk factor of CA, but not the only one. Leprosy, syphilis, poliomyelitis, chronic alcoholism, or syringomyelia among other conditions, may also end with CA. It occurs most commonly in patients who have peripheral neuropathy, or loss of sensation, in the foot and ankle, which can be caused by diabetes.
CA results in progressive destruction of bone and soft tissues at weight bearing joints. The neurovascular theory suggests that CA is caused by a combination of vascular and neuropathic factors. The earliest signs of Charcot are mild pain and discomfort, swelling of the foot, redness and warmth that may be confused with and infections and which can occur without an obvious injury.
Hyperglycemia, decreased blood supply and neuropathy that impairs sensation in the feet and makes it difficult to heal wounds, together with pressure and inability to sense injuries ends with minor undetected lesions, deformities and ulcers. Non-surgical conservative treatments (Immobilization, protective footwear, activity changes) are used in the first phases however surgical treatment are necessary with the progression of the disease including debridement of ulcers, exostectomy, deformity corrections, arthrodesis and amputation for severe cases.
One of the key issues is diabetic wounds, particularly leg ulcers and diabetic ulcers. Diabetes slows the healing process by affecting each stage of wound healing, including homeostasis, inflammation, proliferation, and remodeling. This has a long-term detrimental impact on morbidity and mortality as well as quality of life. Diabetic wounds display a long-lasting inflammatory phase together with a delay in the development of mature granulation tissue and a decrease in the tensile strength of the wound. This could be as a result of the ischemia-causing vascular damage [18][19]. In severe cases of CA, it may not be possible to save part or all of the foot resulting in minor or major amputations.
Prevention of CA and new treatments for this unmet medical need, such as new ATMPs, to avoid amputation are needed. Given the complexity of Diabetic Foot, the results of cell therapy published so far are difficult to compare.
1.3.4. Treatment of Critical Ischemia of the Limb
Conventional Medical Care
Percutaneous transluminal angioplasty (PTA) has become the first line treatment. However, despite the high success rate of PTA, clinical restenosis still represents a huge problem, reaching around 70% at 1-year follow-up [20][21], even more, since in the obstructive pattern is more distal and disperse is quite difficult to succeed with PTA then is considered as no-option CTLI [22][23]. No-option CTLI drives to non-healing ulcers, failure of surgical approaches with a high risk of major amputation, and mortality [24].
Advanced Therapies: Clinical Trials with ATMP to Treat the Diabetic Foot
In 2001, the EMA (European Medicines Agency) defined Advanced Therapy Medicinal Products (ATMPs)/Advanced Therapies as medicines for human use including Somatic Cell Therapy, Gene Therapy, Tissue Engineering and Combined Advanced Therapies. The legal definitions of Cellular and Gene Therapies can be found in Directive 2001/83/EC amended by Directive Commission 2008/12/EC. Definitions of Tissue Engineering and Combined Advanced Therapies can be found in Regulation (EC) No 1394/2007 [25]. Shown in Figure 2 and Figure 3 are the tentative ATMPs that have been use so far and the expected effects bases in their mechanism of action.
Photodynamic Therapies
Typically, the conventional approach for managing diabetic foot ulcers (DFU) involves several key steps, including debridement (cleaning and removal of dead tissue), enhancing blood circulation, maintaining a moist wound environment, and effectively controlling infections [26]. Nevertheless, traditional topical treatments for DFU are expensive and often demonstrate limited effectiveness, especially when faced with multidrug-resistant bacteria, therefore photodynamic therapy (PDT) could stand as a promising approach for addressing infections in the treatment and recovery of DFU. This method entails the application of light-sensitive compounds on the affected area, followed by exposure to either laser (light amplification by stimulated emission of radiation) or LED (light emitting diode) light. When combined with tissue oxygen, this process triggers the generation of reactive oxygen species, leading to a potent local cytotoxic effect that effectively contests the infection in the affected area [27].
References
- IHME. I.f.H.M.a.E. In Global Burden of Disease Study 2019; Global Burden of Disease Collaborative Network: Washington, DC, USA, 2019.
- Magliano, D.J.; Boyko, E.J. IDF Diabetes Atlas; IDF Diabetes Atlas 10th Edition Scientific Committee: Brussels, Belgium, 2021.
- Romero-Gómez, M.; Zelber-Sagi, S.; Martín, F.; Bugianesi, E.; Soria, B. Nutrition could prevent or promote non-alcoholic fatty liver disease: An opportunity for intervention. BMJ (Clin. Res. Ed.) 2023, 383, e075179.
- Crespo, C.; Brosa, M.; Soria-Juan, A.; Lopez-Alba, A.; López-Martínez, N.; Soria, B. Costes directos de la diabetes mellitus y de sus complicaciones en España (Estudio SECCAID: Spain estimated cost Ciberdem-Cabimer in Diabetes). Av. Diabetol. 2013, 29, 182–189.
- Barnes, J.A.; Eid, M.A.; Creager, M.A.; Goodney, P.P. Epidemiology and Risk of Amputation in Patients With Diabetes Mellitus and Peripheral Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1808–1817.
- Lin, J.; Chen, Y.; Jiang, N.; Li, Z.; Xu, S. Burden of Peripheral Artery Disease and Its Attributable Risk Factors in 204 Countries and Territories from 1990 to 2019. Front. Cardiovasc. Med. 2022, 9, 868370.
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.B.; Suresh, K.R.; Murad, M.H.; et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2019, 58, S1–S109.
- Prompers, L.; Huijberts, M.; Apelqvist, J.; Jude, E.; Piaggesi, A.; Bakker, K.; Edmonds, M.; Holstein, P.; Jirkovska, A.; Mauricio, D.; et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007, 50, 18–25.
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis (†). Ann. Med. 2017, 49, 106–116.
- Hart, O.; Xue, N.; Davis-Havill, B.; Pottier, M.; Prakash, M.; Reimann, S.A.; King, J.; Xu, W.; Khashram, M. The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period. J. Clin. Med. 2022, 11, 3303.
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.; Bell, K.; Caporusso, J.; Durand-Zaleski, I.; Komori, K.; et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2007, 33 (Suppl. S1), S5–S67.
- Boulton, A.J. The diabetic foot: Grand overview, epidemiology and pathogenesis. Diabetes/Metab. Res. Rev. 2008, 24 (Suppl. S1), S3–S6.
- Lipsky, B.A.; Berendt, A.R.; Deery, H.G.; Embil, J.M.; Joseph, W.S.; Karchmer, A.W.; LeFrock, J.L.; Lew, D.P.; Mader, J.T.; Norden, C.; et al. Diagnosis and treatment of diabetic foot infections. Plast. Reconstr. Surg. 2006, 117, 212s–238s.
- Fadini, G.P.; Agostini, C.; Avogaro, A. Autologous stem cell therapy for peripheral arterial disease meta-analysis and systematic review of the literature. Atherosclerosis 2010, 209, 10–17.
- Nehler, M.R.; Peyton, B.D. Is revascularization and limb salvage always the treatment for critical limb ischemia? J. Cardiovasc. Surg. 2004, 45, 177–184.
- Sprengers, R.W.; Moll, F.L.; Verhaar, M.C. Stem cell therapy in PAD. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2010, 39 (Suppl. S1), S38–S43.
- Watelet, J.; Soury, P.; Menard, J.F.; Plissonnier, D.; Peillon, C.; Lestrat, J.P.; Testart, J. Femoropopliteal bypass: In situ or reversed vein grafts? Ten-year results of a randomized prospective study. Ann. Vasc. Surg. 1997, 11, 510–519.
- Alavi, A.; Sibbald, R.G.; Mayer, D.; Goodman, L.; Botros, M.; Armstrong, D.G.; Woo, K.; Boeni, T.; Ayello, E.A.; Kirsner, R.S. Diabetic foot ulcers: Part I. Pathophysiology and prevention. J. Am. Acad. Dermatol. 2014, 70, 1-e1.
- Galkowska, H.; Wojewodzka, U.; Olszewski, W.L. Chemokines, cytokines, and growth factors in keratinocytes and dermal endothelial cells in the margin of chronic diabetic foot ulcers. Wound Repair Regen. Off. Publ. Wound Heal. Soc. Eur. Tissue Repair Soc. 2006, 14, 558–565.
- Faglia, E.; Clerici, G.; Clerissi, J.; Gabrielli, L.; Losa, S.; Mantero, M.; Caminiti, M.; Curci, V.; Quarantiello, A.; Lupattelli, T.; et al. Long-term prognosis of diabetic patients with critical limb ischemia: A population-based cohort study. Diabetes Care 2009, 32, 822–827.
- Ferraresi, R.; Mauri, G.; Losurdo, F.; Troisi, N.; Brancaccio, D.; Caravaggi, C.; Neri, L. BAD transmission and SAD distribution: A new scenario for critical limb ischemia. J. Cardiovasc. Surg. 2018, 59, 655–664.
- Hata, Y.; Iida, O.; Takahara, M.; Asai, M.; Masuda, M.; Okamoto, S.; Ishihara, T.; Nanto, K.; Kanda, T.; Tsujimura, T.; et al. Infrapopliteal Anatomic Severity and Delayed Wound Healing in Patients With Chronic Limb-Threatening Ischemia in the Era of the Global Limb Anatomic Staging System. J. Endovasc. Ther. Off. J. Int. Soc. Endovasc. Spec. 2020, 27, 641–646.
- Uccioli, L.; Meloni, M.; Izzo, V.; Giurato, L.; Merolla, S.; Gandini, R. Critical limb ischemia: Current challenges and future prospects. Vasc. Health Risk Manag. 2018, 14, 63–74.
- Ferraresi, R.; Centola, M.; Ferlini, M.; Da Ros, R.; Caravaggi, C.; Assaloni, R.; Sganzaroli, A.; Pomidossi, G.; Bonanomi, C.; Danzi, G.B. Long-term outcomes after angioplasty of isolated, below-the-knee arteries in diabetic patients with critical limb ischaemia. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2009, 37, 336–342.
- Gálvez, P.; Clares, B.; Hmadcha, A.; Ruiz, A.; Soria, B. Development of a cell-based medicinal product: Regulatory structures in the European Union. Br. Med. Bull. 2013, 105, 85–105.
- Everett, E.; Mathioudakis, N. Update on management of diabetic foot ulcers. Ann. N. Y. Acad. Sci. 2018, 1411, 153–165.
- Pantò, F.; Adamo, L.; Giordano, C.; Licciardello, C. Efficacy and safety of photodynamic therapy with RLP068 for diabetic foot ulcers: A review of the literature and clinical experience. Drugs Context 2020, 9.
More
Information
Subjects:
Peripheral Vascular Disease
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
668
Revisions:
2 times
(View History)
Update Date:
29 Dec 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




