Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Lorcán Mason | -- | 1956 | 2023-12-18 12:22:50 | | | |
| 2 | Rita Xu | Meta information modification | 1956 | 2023-12-19 03:10:05 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Mason, L.; Connolly, J.; Devenney, L.E.; Lacey, K.; O’donovan, J.; Doherty, R. Sleep, Nutrition, and Injury Risk in Adolescent Athletes. Encyclopedia. Available online: https://encyclopedia.pub/entry/52875 (accessed on 07 February 2026).
Mason L, Connolly J, Devenney LE, Lacey K, O’donovan J, Doherty R. Sleep, Nutrition, and Injury Risk in Adolescent Athletes. Encyclopedia. Available at: https://encyclopedia.pub/entry/52875. Accessed February 07, 2026.
Mason, Lorcán, James Connolly, Lydia E. Devenney, Karl Lacey, Jim O’donovan, Rónán Doherty. "Sleep, Nutrition, and Injury Risk in Adolescent Athletes" Encyclopedia, https://encyclopedia.pub/entry/52875 (accessed February 07, 2026).
Mason, L., Connolly, J., Devenney, L.E., Lacey, K., O’donovan, J., & Doherty, R. (2023, December 18). Sleep, Nutrition, and Injury Risk in Adolescent Athletes. In Encyclopedia. https://encyclopedia.pub/entry/52875
Mason, Lorcán, et al. "Sleep, Nutrition, and Injury Risk in Adolescent Athletes." Encyclopedia. Web. 18 December, 2023.
Copy Citation
Sleep is viewed as essential to the recuperation process and is distinguished as an active participant in recovery through its involvement in growth, repair, regeneration, and immunity. Furthermore, the literature has shown that the sleep of athletes impacts elements of athletic performance including both physical and cognitive performance, recovery, injury risk, and mental well-being. For sleep to have a restorative effect on the body, it must meet an individual’s sleep needs whilst also lasting for an adequate duration and being of adequate quality, which is age-dependent.
adolescent
athletes
sleep
nutrition
1. Introduction
Sleep can be defined as a reversible behavioural state of impaired consciousness through a reduction in sensory and motor activity [1][2][3][4][5]. Sleep is regarded as an active regulatory process [6] and facilitates the proper functioning of the brain and cognitive performance while also regulating physiological functions including substrate and energy metabolism [7][8][9], cardiovascular function [10][11], appetite [12], endocrine function [13][14], and immune function [15]. Several facilitating theories for sleep have been hypothesised [5][16], including the regeneration of immune and endocrine function, the nervous system, and metabolic cost of living, and aids in cognitive development and synaptic plasticity [17]. As such, sleep is viewed as essential to the recuperation process [3][18] and is distinguished as an active participant in recovery through its involvement in growth, repair, regeneration, and immunity [5]. Furthermore, the literature has shown that the sleep of athletes impacts elements of athletic performance including both physical and cognitive performance, recovery, injury risk, and mental well-being [4][19][20][21][22][23].
The architecture of sleep is organised into multiple 90-min series of one rapid-eye-movement (REM) and three non-REM sleep phases (N1, N2, and N3) [24][25][26]. Non-REM and REM sleep are distinct in nature and are characterised by brainwave activity, eye movement, cardiac rhythm, muscle tone, breath rate, and arousal thresholds [27][28]. REM sleep facilitates neurological regeneration, learning, memory, and emotional regulation [27][29][30]. Non-REM sleep is a three-phased process whereby the propensity to wake (the arousal threshold) is lowest during the first phase and progressively increases through to the highest point in the final phase (N3) [27][28] and can be characterised by the wave activity of the brain [27][31]. Non-REM sleep functions to support the regeneration of the nervous system, conserve energy, release anabolic hormones that augment protein synthesis to facilitate muscle recovery [32][33], and mobilise free fatty acids for ATP production [34]. For a detailed breakdown of the brainwave characteristics of the sleep cycle, readers should refer to the AASM manual for the scoring of sleep and associated events [25], and the principles and practices of sleep medicine [27].
2. Importance of Sleep Health
Sleep health is defined as an individualised and context-specific multidimensional pattern of sleep and wakefulness that supports physical and mental well-being [35] and is an integral component of not only living a healthy lifestyle [36][37] but also of adaptation and recovery [3][27][32][38][39]. The relationship between sleep and recovery in athletes can be viewed in terms of three key factors that affect restoration processes: 1. sleep duration (total sleep requirements including napping); 2. sleep quality (total sleep absent of sleep disorders, environmental disturbances, or sleep fragmentation); 3. sleep phase (circadian timing of sleep during the light–dark cycle) [39][40]. During adolescence, the psychosocial and societal pressures experienced may result in adverse sleep health and reduced recovery capacity [41][42]. This is due to sleep deficiencies, which have a negative impact on health and are linked to increases in all-cause mortality and disease risk [43]. Sleep deprivation (an insufficient sleep duration compared to the basal level) and disturbances (the inability to initiate and/or maintain the sleep–cycle) are also risk factors for adverse health, recovery, and injury risk in athletic populations [39][40][44][45][46][47][48].
For sleep to have a restorative effect on the body, it must meet an individual’s sleep needs whilst also lasting for an adequate duration and being of adequate quality, which is age-dependent [46]. Sleep needs can be defined as the optimum quantity of sleep required to maintain alertness and function throughout daily living [5]. Sleep duration can be influenced by exogenous and endogenous environmental characteristics, which adds complexity to defining an “optimal” sleep pattern due to high inter-individual differences [49][50][51]. Peripheral tissues contain molecular clocks within each cell that dictate the expression of clock-controlled genes in a period (the required time for a cortical neuron oscillation) or phase (waking time in relation to the light cycle) [49][52]. Processes controlled by circadian rhythms also influence sleep duration; thus, the time at which sleep occurs in the light cycle also has an integral role in sleep duration [50][53][54]. The difference between sleep needs and actual sleep duration is known as sleep debt [5].
3. Sleep Adaptations during Adolescence
The chronotype that defines the expression of individual circadian rhythmicity [55] may similarly shift during adolescence [56][57][58][59][60] due to the greater robustness to increased sleep pressure [61] and environmental factors that increase evening alertness [42]. An individual’s chronotype is mainly dictated by their genetic makeup; however, environmental and societal factors also affect the chronotype [55][62]. Cross-sectional research has evidenced that during adolescence, the distribution of the chronotype shifts toward the evening chronotype, reverting back to the earlier chronotypes post-maturation [56][57][58][59][60]. As sleep needs change over the lifespan, The National Sleep Foundation has published guidelines for age-dependent sleep durations, which includes recommendations for the following: adolescents (8–10 h), adults (7–9 h), and older adults (7–8 h) [46]. The literature has suggested that athletes have increased sleep needs, and thus the general recommendations may not be sufficient for athletic populations [23][63]. Therefore, a more individualised approach accounting for overall sleep health may be more appropriate for addressing sleep needs in individuals including athletes [23][35][63]. To feel rested, the literature has demonstrated that elite athletes need ~8.3 h of sleep [64][65]. Moreover, adolescent athletes achieve, on average, ~6.3 h [47][66][67] of sleep, demonstrating a discrepancy between sleep recommendations and actual sleep achieved [42][68][69]. Sleep–wake cycles also undergo development during adolescence whereby adaptation occurs in sleep regulation during this phase [68]. These adaptations to sleep regulation increase sleep pressure tolerance (reduced adenosine accumulation) [70][71][72] and are driven by the maturation of physiological, psychological, and cognitive functioning along with delays in circadian rhythmicity [73], thus creating an environment for inadequate sleep influenced by external factors associated with adolescence (Figure 1) [41][42][73][74]. This results in ever-decreasing time spent asleep during the ages of 15–18 years, with research reporting a decrease of ~1.5–3 h during this period [70][75][76]. Despite this, an adolescents sleep needs (pressure dissipation) under free living conditions does not appear to alter from the recommended ~9.25 h [42], irrespective of maturation status [77][78][79], thus attributing the decline to environmental factors as opposed to biological factors [73][80].
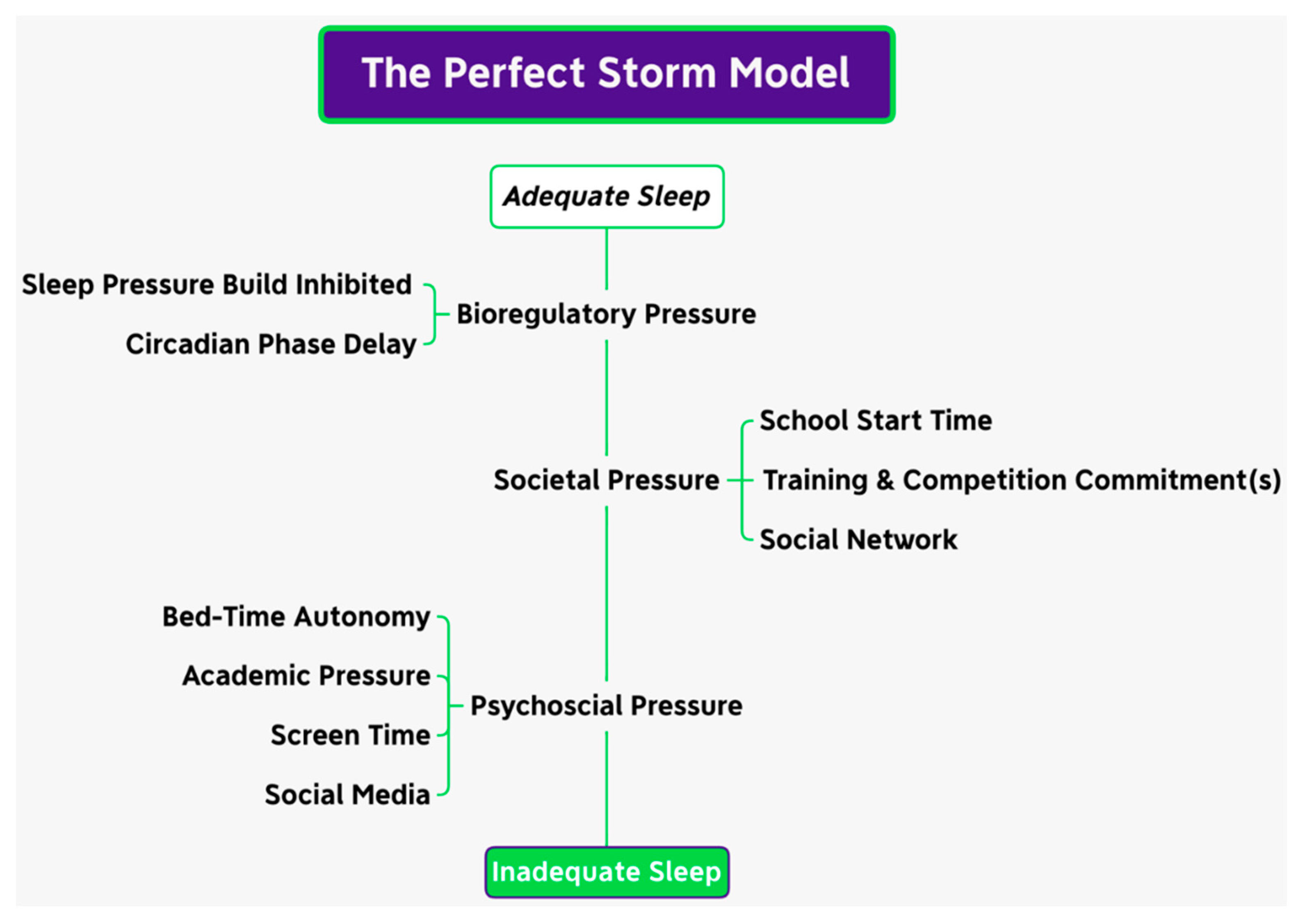
Figure 1. The perfect storm model.
4. Growth, Maturation, and Energy Demands in Adolescent Athletes
Adolescence is the transitional life stage where the process of maturation occurs [81]. Maturation signifies the progressive period toward the adult or mature state [82], and is characterised by status (maturity state at the time of observation), timing (biological age at which specific maturational events occur), and tempo (the rate of maturational progression) [82][83][84][85][86]. During the maturation period, approximately 20% of the final adult height is reached and 50% of the predicted adult body weight is achieved with an increase of up to 40% in bone mass [81][87]. The adolescence period is a significant life stage that begins in conjunction with the onset of puberty. Puberty is unique to the individual with a vast range of inter-individual differences in maturation status impacting both physical and psycho-social development [82][84][86]. As evidenced, maturation status influences the development of and improvement in locomotive competencies in both a linear (accrual of strength capabilities) and non-linear (accrual of co-ordinative capabilities) fashion [88], influencing training adaptations in adolescent athletes [88][89][90][91]. Puberty onset is the catalyst of the growth period where the body undergoes meaningful physical and psycho-social adaptations such as alterations to body composition, including the accrual of bone, muscle, and fat mass, metabolic and endocrine system development, the development and maturation of the organ system, the establishment of nutrient storage and partitioning, and the establishment of self-esteem and psychological well-being, all of which affect general health and well-being [81][92][93][94]. Maturation results from the outcome of a multitude of complex processes that are governed by genetics, the endocrine system, environmental constraints, and nutrient intake [86][89][95][96].
5. Differences between Adolescent and Adult Athletes
During adolescence, there are vast inter-individual differences in nutritional needs dependent on factors including maturation status, body composition, physical activity, chronological age, and gender [92][95][96][97][98]. The implementation of correct and individualised nutrition for adolescent athletes not only supports overall health, adaptation, recovery, and athletic performance, but is also necessary for meeting growth and development demands [92][95][96][97][98]. Compared to their adult counterparts, adolescents possess several differences in substrate storage and metabolism, in conjunction with numerous physiological and metabolic alterations associated with maturation that contribute to an individual’s nutrient requirements [96]. Furthermore, nutrient and energy requirements in adolescence are also largely dictated by the interplay between three main factors: (1) current anthropometry, (2) maturation state, rate, and timing, and (3) physical activity and sporting demands [92][96][97]. These energy requirements of an individual are fulfilled by the intake of energy-yielding macro-nutrients, carbohydrates, protein, and fat [96][99][100][101]. The specific energy intake of adolescent athletes should be largely dictated by total daily energy expenditure (TDEE) [96][102][103][104].
Growth and maturation are energy-intensive processes where energy intake influences both the synthesis of new tissue and the deposition of nutrients into the new tissue [92][96][105]. The basal metabolic rate denotes the energy expended to synthesize new tissue during growth; however, energy deposition is difficult to accurately measure [92][96][105][106]. During both peak height velocity (PHV) and peak weight velocity (PWV; weight denotes body mass) periods, energy requirements are in flux and are variable among adolescents of the same chronological age, in particular their basal metabolic rates, which rapidly increases in a stepwise fashion to match their maturation status, timing, and tempo [95][96][107][108]. The thermic effect of activity often makes the largest contribution to energy requirements in adolescent athletes [92][96][107]. The thermic effect of activity is influenced by anthropometry and the duration, intensity, and mode of physical activity, which also contribute to total activity energy expenditure [92][96], resulting in large interindividual variability in energy requirements [92][95][96], creating difficulties in prescribing energy requirement recommendations for adolescent athletes [92][95][96][97]. Persistent low energy availability (LEA) contributes to negative outcomes in growth and development including impaired cellular, organ, and tissue development, reduced bone mineral density, an increased risk of stress fractures, delay and/or regression in sexual maturation, and immune deficiencies [96][109][110]. Thus, it is recommended that if any signs or symptoms of LEA persist in adolescent athletes, energy intake should be increased to prevent detrimental effects on maturation, recovery, and injury risk [96][103][110].
6. Nutrition Knowledge of Adolescents
As established within the literature, adequate nutrition is paramount for performance, recovery, and adaptation to training, along with optimising the maturation process during adolescence [96][103][111]; thus, sufficient nutritional knowledge is required to optimise dietary behaviours to support these processes and inform eating habits [112][113][114][115][116][117]. In the absence of sufficient nutritional knowledge, nutritional intake may be compromised due to poor food selection and decreased dietary quality [118]. This may negatively impact the training–recovery cycle in athletes and adolescent growth and development [112][113][115][116][117][119][120][121][122]. It has been reported that athletic populations fail to meet the recommended nutritional requirements to support training demands [116][118]; however, with regards to the level of nutrition knowledge, a weak positive relationship (r = >0.26) exists between the level of one’s nutrition knowledge and their energy balance and dietary quality [113][118][121][122]. Due to the multiple assessment tools utilised in nutrition knowledge research including the Abridged-Nutrition for Sport Knowledge Questionnaire (A-NSKQ), General and Sports Nutrition Knowledge Questionnaire (GeSNK), Nutrition Knowledge Questionnaire for Athletes (NKQA), Nutrition for Sport Knowledge Questionnaire (NSKQ), Nutrition Knowledge for Young and Adult Athletes (NUKYA), and Platform to Evaluate Athlete Knowledge of Sports Nutrition Questionnaire (PEAKS-NQ) [116], research is difficult to infer. Despite this, research suggests that that the mean correct scores for general (GNK) and sport (SNK) nutrition knowledge in adult athletes are between 40.2 ± 12.4% and 70 ± 9% [118]. Moreover, research in adolescent athletes suggests that mean nutrition knowledge ranges between 43.8 ± 11.4% and 48.85 ± 12.7% [115][123][124], which is lower than that of their elder counterparts (overall NK% = 55.1 ± 10.7%) [118], therefore highlighting the importance of increasing the level of nutritional knowledge in adolescent athletes to support maturation, recovery, and injury risk.
References
- Shapiro, C.M. Sleep and the Athlete. Br. J. Sports Med. 1981, 15, 51–55.
- Allada, R.; Siegel, J.M. Unearthing the Phylogenetic Roots of Sleep. Curr. Biol. 2008, 18, R670–R679.
- Halson, S.L. Sleep and the Elite Athlete. Sports Sci. Exch. 2013, 26, 1–4.
- Fullagar, H.H.K.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise. Sports Med. 2015, 45, 161–186.
- Chokroverty, S. (Ed.) Overview of Normal Sleep. In Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects; Springer: New York, NY, USA, 2017; pp. 5–27. ISBN 978-1-4939-6578-6.
- Hobson, J.A. Sleep Is of the Brain, by the Brain and for the Brain. Nature 2005, 437, 1254–1256.
- VanHelder, T.; Symons, J.D.; Radomski, M.W. Effects of Sleep Deprivation and Exercise on Glucose Tolerance. Aviat. Space Environ. Med. 1993, 64, 487–492.
- Penev, P.D. Sleep Deprivation and Energy Metabolism: To Sleep, Perchance to Eat? Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 374–381.
- Chua, E.C.-P.; Shui, G.; Cazenave-Gassiot, A.; Wenk, M.R.; Gooley, J.J. Changes in Plasma Lipids during Exposure to Total Sleep Deprivation. Sleep 2015, 38, 1683–1691.
- Trinder, J.; Waloszek, J.; Woods, M.J.; Jordan, A.S. Sleep and Cardiovascular Regulation. Pflüg. Arch. Eur. J. Physiol. 2012, 463, 161–168.
- Vaara, J.; Kyröläinen, H.; Koivu, M.; Tulppo, M.; Finni, T. The Effect of 60-h Sleep Deprivation on Cardiovascular Regulation and Body Temperature. Eur. J. Appl. Physiol. 2009, 105, 439–444.
- Spiegel, K.; Tasali, E.; Penev, P.; Cauter, E.V. Brief Communication: Sleep Curtailment in Healthy Young Men Is Associated with Decreased Leptin Levels, Elevated Ghrelin Levels, and Increased Hunger and Appetite. Ann. Intern. Med. 2004, 141, 846–850.
- Scheer, F.A.J.L.; Hilton, M.F.; Mantzoros, C.S.; Shea, S.A. Adverse Metabolic and Cardiovascular Consequences of Circadian Misalignment. Proc. Natl. Acad. Sci. USA 2009, 106, 4453–4458.
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of Sleep Debt on Metabolic and Endocrine Function. Lancet 1999, 354, 1435–1439.
- Santos, R.V.T.; Tufik, S.; De Mello, M.T. Exercise, Sleep and Cytokines: Is There a Relation? Sleep Med. Rev. 2007, 11, 231–239.
- Frank, M.G.; Benington, J.H. The Role of Sleep in Memory Consolidation and Brain Plasticity: Dream or Reality? Neuroscientist 2006, 12, 477–488.
- Morrison, M.; Halson, S.L.; Weakley, J.; Hawley, J.A. Sleep, Circadian Biology and Skeletal Muscle Interactions: Implications for Metabolic Health. Sleep Med. Rev. 2022, 66, 101700.
- Adam, K.; Oswald, I. Sleep Is for Tissue Restoration. J. R. Coll. Physicians 1977, 11, 376.
- Malhotra, R.K. Sleep, Recovery, and Performance in Sports. Neurol. Clin. 2017, 35, 547–557.
- Kölling, S.; Duffield, R.; Erlacher, D.; Venter, R.; Halson, S.L. Sleep-Related Issues for Recovery and Performance in Athletes. Int. J. Sports Physiol. Perform. 2019, 14, 144–148.
- Charest, J.; Grandner, M.A. Sleep and Athletic Performance: Impacts on Physical Performance, Mental Performance, Injury Risk and Recovery, and Mental Health. Sleep Med. Clin. 2020, 15, 41–57.
- Doherty, R.; Madigan, S.M.; Nevill, A.; Warrington, G.; Ellis, J.G. The Sleep and Recovery Practices of Athletes. Nutrients 2021, 13, 1330.
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J.; et al. Sleep and the Athlete: Narrative Review and 2021 Expert Consensus Recommendations. Br. J. Sports Med. 2021, 55, 356–368.
- McCarley, R.W. Neurobiology of REM and NREM Sleep. Sleep Med. 2007, 8, 302–330.
- Berry, R.B.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Marcus, C.; Vaughn, B.V. The AASM Manual for the Scoring of Sleep and Associated Events. Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Darien, IL, USA, 2012; Volume 176, p. 2012.
- Halson, S.L.; Juliff, L.E. Sleep, Sport, and the Brain. Prog. Brain Res. 2017, 234, 13–31.
- Carskadon, M.A.; Dement, W.C. Chapter 2—Normal Human Sleep: An Overview. In Principles and Practice of Sleep Medicine, 4th ed.; Kryger, M.H., Roth, T., Dement, W.C., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2005; pp. 13–23. ISBN 978-0-7216-0797-9.
- Irwin, M.R.; Opp, M.R. Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2017, 42, 129–155.
- Siegel, J.M. Clues to the Functions of Mammalian Sleep. Nature 2005, 437, 1264–1271.
- Stickgold, R. Sleep-Dependent Memory Consolidation. Nature 2005, 437, 1272–1278.
- Sriraam, N.; Padma Shri, T.K.; Maheshwari, U. Recognition of Wake-Sleep Stage 1 Multichannel Eeg Patterns Using Spectral Entropy Features for Drowsiness Detection. Australas. Phys. Eng. Sci. Med. 2016, 39, 797–806.
- Venter, R.E. Role of Sleep in Performance and Recovery of Athletes: A Review Article. S. Afr. J. Res. Sport Phys. Educ. Recreat. 2012, 34, 167–184.
- Kraemer, W.J.; Ratamess, N.A.; Hymer, W.C.; Nindl, B.C.; Fragala, M.S. Growth Hormone(s), Testosterone, Insulin-Like Growth Factors, and Cortisol: Roles and Integration for Cellular Development and Growth with Exercise. Front. Endocrinol. 2020, 11, 33.
- Sassin, J.F.; Parker, D.C.; Mace, J.W.; Gotlin, R.W.; Johnson, L.C.; Rossman, L.G. Human Growth Hormone Release: Relation to Slow-Wave Sleep and Sleep-Waking Cycles. Science 1969, 165, 513–515.
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17.
- Matricciani, L.; Bin, Y.S.; Lallukka, T.; Kronholm, E.; Wake, M.; Paquet, C.; Dumuid, D.; Olds, T. Rethinking the Sleep-Health Link. Sleep Health 2018, 4, 339–348.
- Benítez, I.; Roure, N.; Pinilla, L.; Sapiña-Beltran, E.; Buysse, D.J.; Barbé, F.; de Batlle, J. Validation of the Satisfaction, Alertness, Timing, Efficiency and Duration (SATED) Questionnaire for Sleep Health Measurement. Ann. Am. Thorac. Soc. 2020, 17, 338–343.
- Halson, S.L. Nutrition, Sleep and Recovery. Eur. J. Sport Sci. 2008, 8, 119–126.
- Samuels, C. Sleep, Recovery, and Performance: The New Frontier in High-Performance Athletics. Neurol. Clin. 2008, 26, 169–180.
- Samuels, C.; James, L.; Lawson, D.; Meeuwisse, W. The Athlete Sleep Screening Questionnaire: A New Tool for Assessing and Managing Sleep in Elite Athletes. Br. J. Sports Med. 2016, 50, 418–422.
- Carskadon, M.A. Sleep in Adolescents: The Perfect Storm. Pediatr. Clin. N. Am. 2011, 58, 637–647.
- Crowley, S.J.; Wolfson, A.R.; Tarokh, L.; Carskadon, M.A. An Update on Adolescent Sleep: New Evidence Informing the Perfect Storm Model. J. Adolesc. 2018, 67, 55–65.
- Ong, J.L.; Lo, J.C.; Gooley, J.J.; Chee, M.W.L. EEG Changes Accompanying Successive Cycles of Sleep Restriction with and without Naps in Adolescents. Sleep 2017, 40, zsx030.
- Skein, M.; Duffield, R.; Minett, G.M.; Snape, A.; Murphy, A. The Effect of Overnight Sleep Deprivation after Competitive Rugby League Matches on Postmatch Physiological and Perceptual Recovery. Int. J. Sports Physiol. Perform. 2013, 8, 556–564.
- Milewski, M.D.; Skaggs, D.L.; Bishop, G.A.; Pace, J.L.; Ibrahim, D.A.; Wren, T.A.L.; Barzdukas, A. Chronic Lack of Sleep Is Associated with Increased Sports Injuries in Adolescent Athletes. J. Pediatr. Orthop. 2014, 34, 129–133.
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s Sleep Time Duration Recommendations: Methodology and Results Summary. Sleep Health 2015, 1, 40–43.
- Copenhaver, E.A.; Diamond, A.B. The Value of Sleep on Athletic Performance, Injury, and Recovery in the Young Athlete. Pediatr. Ann. 2017, 46, e106–e111.
- Coel, R.A.; Pujalte, G.G.A.; Applewhite, A.I.; Zaslow, T.; Cooper, G.; Ton, A.N.; Benjamin, H.J. Sleep and the Young Athlete. Sports Health 2023, 15, 537–546.
- Koronowski, K.B.; Sassone-Corsi, P. Communicating Clocks Shape Circadian Homeostasis. Science 2021, 371, eabd0951.
- Kryger, M.H.; Roth, T.; Dement, W.C. (Eds.) Principles and Practice of Sleep Medicine, 6th ed.; Elsevier: Philadelphia, PA, USA, 2017; ISBN 978-0-323-24288-2.
- Lassi, G.; Tucci, V. Genomic Imprinting and the Control of Sleep in Mammals. Curr. Opin. Behav. Sci. 2019, 25, 77–82.
- Kurien, P.; Ptáček, L.J.; Fu, Y.-H. Chapter 11—The Genetic Regulation of Human Sleep-Wake Rhythms and Patterns. In Handbook of Behavioral Neuroscience; Dringenberg, H.C., Ed.; Handbook of Sleep Research; Elsevier: Amsterdam, The Netherlands, 2019; Volume 30, pp. 169–180.
- Borbély, A.A. A Two Process Model of Sleep Regulation. Hum. Neurobiol. 1982, 1, 195–204.
- Borbély, A.A.; Daan, S.; Wirz-Justice, A.; Deboer, T. The Two-Process Model of Sleep Regulation: A Reappraisal. J. Sleep Res. 2016, 25, 131–143.
- Rosenthal, L.; Day, R.; Gerhardstein, R.; Meixner, R.; Roth, T.; Guido, P.; Fortier, J. Sleepiness/Alertness among Healthy Evening and Morning Type Individuals. Sleep Med. 2001, 2, 243–248.
- Karan, M.; Bai, S.; Almeida, D.M.; Irwin, M.R.; McCreath, H.; Fuligni, A.J. Sleep-Wake Timings in Adolescence: Chronotype Development and Associations with Adjustment. J. Youth Adolesc. 2021, 50, 628–640.
- Kuula, L.; Pesonen, A.-K.; Merikanto, I.; Gradisar, M.; Lahti, J.; Heinonen, K.; Kajantie, E.; Räikkönen, K. Development of Late Circadian Preference: Sleep Timing From Childhood to Late Adolescence. J. Pediatr. 2018, 194, 182–189.e1.
- Hagenauer, M.H.; Lee, T.M. The Neuroendocrine Control of the Circadian System: Adolescent Chronotype. Front. Neuroendocrinol. 2012, 33, 211–229.
- Fischer, D.; Lombardi, D.A.; Marucci-Wellman, H.; Roenneberg, T. Chronotypes in the US—Influence of Age and Sex. PLoS ONE 2017, 12, e0178782.
- Carskadon, M.A.; Vieira, C.; Acebo, C. Association between Puberty and Delayed Phase Preference. Sleep 1993, 16, 258–262.
- Jenni, O.G.; Achermann, P.; Carskadon, M.A. Homeostatic Sleep Regulation in Adolescents. Sleep 2005, 28, 1446–1454.
- Vitale, J.A.; Weydahl, A. Chronotype, Physical Activity, and Sport Performance: A Systematic Review. Sports Med. 2017, 47, 1859–1868.
- Halson, S.L. Sleep Monitoring in Athletes: Motivation, Methods, Miscalculations and Why It Matters. Sports Med. 2019, 49, 1487–1497.
- Sargent, C.; Lastella, M.; Halson, S.L.; Roach, G.D. How Much Sleep Does an Elite Athlete Need? Int. J. Sports Physiol. Perform. 2021, 16, 1746–1757.
- Cunha, L.A.; Costa, J.A.; Marques, E.A.; Brito, J.; Lastella, M.; Figueiredo, P. The Impact of Sleep Interventions on Athletic Performance: A Systematic Review. Sports Med. Open 2023, 9, 58.
- Lo, H.; Leung, J.; Chau, K.Y.; Lam, M.H.S.; Lee, K.Y.; Ho, A. Factors Affecting Sleep Quality among Adolescent Athletes. Sports Nutr. Ther. 2017, 2, 2.
- Patel, A.R.; Hsu, A.; Perez, I.A.; Wren, T.A.L.; Edison, B.R. Assessing the Effects of Sleep on Neurocognitive Performance and Injury Rate in Adolescent Athletes Using Actigraphy. Res. Sports Med. 2020, 28, 498–506.
- Tarokh, L.; Short, M.; Crowley, S.J.; Fontanellaz-Castiglione, C.E.G.; Carskadon, M.A. Sleep and Circadian Rhythms in Adolescence. Curr. Sleep Med. Rep. 2019, 5, 181–192.
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786.
- Crowley, S.J.; Reen, E.V.; LeBourgeois, M.K.; Acebo, C.; Tarokh, L.; Seifer, R.; Barker, D.H.; Carskadon, M.A. A Longitudinal Assessment of Sleep Timing, Circadian Phase, and Phase Angle of Entrainment across Human Adolescence. PLoS ONE 2014, 9, e112199.
- Skeldon, A.C.; Derks, G.; Dijk, D.-J. Modelling Changes in Sleep Timing and Duration across the Lifespan: Changes in Circadian Rhythmicity or Sleep Homeostasis? Sleep Med. Rev. 2016, 28, 96–107.
- Deboer, T. Sleep Homeostasis and the Circadian Clock: Do the Circadian Pacemaker and the Sleep Homeostat Influence Each Other’s Functioning? Neurobiol. Sleep Circadian Rhythms 2018, 5, 68–77.
- Tarokh, L.; Saletin, J.M.; Carskadon, M.A. Sleep in Adolescence: Physiology, Cognition and Mental Health. Neurosci. Biobehav. Rev. 2016, 70, 182–188.
- Carskadon, M.A. Sleep and Circadian Rhythms in Children and Adolescents: Relevance for Athletic Performance of Young People. Clin. Sports Med. 2005, 24, 319–328.
- Wheaton, A.G. Sleep Duration and Injury-Related Risk Behaviors Among High School Students—United States, 2007–2013. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 337–341.
- Yang, C.-K.; Kim, J.K.; Patel, S.R.; Lee, J.-H. Age-Related Changes in Sleep/Wake Patterns among Korean Teenagers. Pediatrics 2005, 115, 250–256.
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-Analysis of Quantitative Sleep Parameters From Childhood to Old Age in Healthy Individuals: Developing Normative Sleep Values Across the Human Lifespan. Sleep 2004, 27, 1255–1273.
- Mary, A.C.; Harvey, K.; Duke, P.; Thomas, F.A.; Iris, F.L.; William, C.D. Pubertal Changes in Daytime Sleepiness. Sleep 1980, 2, 453–460.
- Chaput, J.-P.; Dutil, C.; Sampasa-Kanyinga, H. Sleeping Hours: What Is the Ideal Number and How Does Age Impact This? Nat. Sci. Sleep 2018, 10, 421–430.
- Kelley, P.; Lockley, S.W.; Foster, R.G.; Kelley, J. Synchronizing Education to Adolescent Biology: ‘Let Teens Sleep, Start School Later’. Learn. Media Technol. 2015, 40, 210–226.
- Norris, S.A.; Frongillo, E.A.; Black, M.M.; Dong, Y.; Fall, C.; Lampl, M.; Liese, A.D.; Naguib, M.; Prentice, A.; Rochat, T.; et al. Nutrition in Adolescent Growth and Development. Lancet 2022, 399, 172–184.
- Cumming, S.P.; Lloyd, R.S.; Oliver, J.L.; Eisenmann, J.C.; Malina, R.M. Bio-Banding in Sport: Applications to Competition, Talent Identification, and Strength and Conditioning of Youth Athletes. Strength Cond. J. 2017, 39, 34–47.
- Bergeron, M.F.; Mountjoy, M.; Armstrong, N.; Chia, M.; Côté, J.; Emery, C.A.; Faigenbaum, A.; Hall, G.; Kriemler, S.; Léglise, M. International Olympic Committee Consensus Statement on Youth Athletic Development. Br. J. Sports Med. 2015, 49, 843–851.
- Malina, R.M.; Bouchard, C.; Bar-Or, O. Growth, Maturation, and Physical Activity; Human Kinetics: Champaign, IL, USA, 2004; ISBN 0-88011-882-2.
- Armstrong, N.; Van Mechelen, W. Oxford Textbook of Children’s Sport and Exercise Medicine; Oxford University Press: Oxford, UK, 2017; ISBN 0-19-875767-0.
- Malina, R.M.; Rogol, A.D.; Cumming, S.P.; Coelho e Silva, M.J.; Figueiredo, A.J. Biological Maturation of Youth Athletes: Assessment and Implications. Br. J. Sports Med. 2015, 49, 852–859.
- Baxter-Jones, A.D.; Faulkner, R.A.; Forwood, M.R.; Mirwald, R.L.; Bailey, D.A. Bone Mineral Accrual from 8 to 30 Years of Age: An Estimation of Peak Bone Mass. J. Bone Miner. Res. 2011, 26, 1729–1739.
- Rodriguez-Negro, J.; Llodio, I.; Castillo, D.; Romaratezabala, E.; Yanci, J. Changes in Selected Locomotor Skills of Young Runners after One Athletic Season: Influence of Sex and Age. Int. J. Sports Sci. Coach. 2021, 16, 1152–1161.
- Malina, R.M.; Rogol, A.D. Sport Training and the Growth and Pubertal Maturation of Young Athletes. Pediatr. Endocrinol. Rev. PER 2011, 9, 441–455.
- McBurnie, A.; Dos’Santos, T.; Johnson, D.; Leng, E. Training Management of the Elite Adolescent Soccer Player throughout Maturation. Sports 2021, 9, 170.
- Jayanthi, N.; Schley, S.; Cumming, S.P.; Myer, G.D.; Saffel, H.; Hartwig, T.; Gabbett, T.J. Developmental Training Model for the Sport Specialized Youth Athlete: A Dynamic Strategy for Individualizing Load-Response During Maturation. Sports Health 2022, 14, 142–153.
- Desbrow, B. Youth Athlete Development and Nutrition. Sports Med. 2021, 51, 3–12.
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A Foundation for Future Health. Lancet 2012, 379, 1630–1640.
- Meeus, W. Adolescent Psychosocial Development: A Review of Longitudinal Models and Research. Dev. Psychol. 2016, 52, 1969–1993.
- Hannon, M.P.; Parker, L.J.F.; Carney, D.J.; Mckeown, J.; Speakman, J.R.; Hambly, C.; Drust, B.; Unnithan, V.B.; Close, G.L.; Morton, J.P. Energy Requirements of Male Academy Soccer Players from the English Premier League. Med. Sci. Sports Exerc. 2021, 53, 200–210.
- Hannon, M.P.; Close, G.L.; Morton, J.P. Energy and Macronutrient Considerations for Young Athletes. Strength Cond. J. 2020, 42, 109–119.
- Berg, E.K. Performance Nutrition for the Adolescent Athlete: A Realistic Approach. Clin. J. Sport Med. 2019, 29, 345–352.
- Aerenhouts, D.; Deriemaeker, P.; Hebbelinck, M.; Clarys, P. Energy and Macronutrient Intake in Adolescent Sprint Athletes: A Follow-up Study. J. Sports Sci. 2011, 29, 73–82.
- Jeukendrup, A.; Gleeson, M. Sport Nutrition; Human Kinetics: Champaign, IL, USA, 2018; ISBN 1-4925-2903-6.
- Benardot, D. Advanced Sports Nutrition, 3rd ed.; Human Kinetics: Champaign, IL, USA, 2021; ISBN 978-1-4925-9311-9.
- Spano, M.A.; Kruskall, L.J.; Thomas, D.T. Nutrition for Sport, Exercise, and Health; Human Kinetics: Champaign, IL, USA, 2018; ISBN 978-1-4504-1487-6.
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568.
- Hannon, M.P.; Unnithan, V.; Morton, J.P.; Close, G.L. Nutritional Strategies to Support Young Athletes. In Strength and Conditioning for Young Athletes; Routledge: Oxford, UK, 2019; pp. 300–335.
- Pontzer, H.; Yamada, Y.; Sagayama, H.; Ainslie, P.N.; Andersen, L.F.; Anderson, L.J.; Arab, L.; Baddou, I.; Bedu-Addo, K.; Blaak, E.E. Daily Energy Expenditure through the Human Life Course. Science 2021, 373, 808–812.
- Torun, B. Energy Requirements of Children and Adolescents. Public Health Nutr. 2005, 8, 968–993.
- World Health Organization. Measuring Change in Nutritional Status; World Health Organization: Geneva, Switzerland, 1982; ISBN 92-4-154166-0.
- Silva, A.M.; Santos, D.A.; Matias, C.N.; Minderico, C.S.; Schoeller, D.A.; Sardinha, L.B. Total Energy Expenditure Assessment in Elite Junior Basketball Players: A Validation Study Using Doubly Labeled Water. J. Strength Cond. Res. 2013, 27, 1920–1927.
- Hannon, M.P.; Carney, D.J.; Floyd, S.; Parker, L.J.F.; McKeown, J.; Drust, B.; Unnithan, V.B.; Close, G.L.; Morton, J.P. Cross-Sectional Comparison of Body Composition and Resting Metabolic Rate in Premier League Academy Soccer Players: Implications for Growth and Maturation. J. Sports Sci. 2020, 38, 1326–1334.
- Loucks, A.B.; Kiens, B.; Wright, H.H. Energy Availability in Athletes. J. Sports Sci. 2011, 29, S7–S15.
- Mountjoy, M.; Sundgot-Borgen, J.K.; Burke, L.M.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.K.; Meyer, N.L.; et al. IOC Consensus Statement on Relative Energy Deficiency in Sport (RED-S): 2018 Update. Br. J. Sports Med. 2018, 52, 687–697.
- Kudret Saribay, A.; Kirbaş, Ş. Determination of Nutrition Knowledge of Adolescents Engaged in Sports. Univers. J. Educ. Res. 2019, 7, 40–47.
- Smith, J.W.; Holmes, M.E.; McAllister, M.J. Nutritional Considerations for Performance in Young Athletes. J. Sports Med. 2015, 2015, e734649.
- Spronk, I.; Heaney, S.E.; Prvan, T.; O’Connor, H.T. Relationship between General Nutrition Knowledge and Dietary Quality in Elite Athletes. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 243–251.
- Noll, M.; de Mendonça, C.R.; de Souza Rosa, L.P.; Silveira, E.A. Determinants of Eating Patterns and Nutrient Intake among Adolescent Athletes: A Systematic Review. Nutr. J. 2017, 16, 46.
- Bird, S.P.; Rushton, B.D. Nutritional Knowledge of Youth Academy Athletes. BMC Nutr. 2020, 6, 35.
- Tam, R.; Gifford, J.A.; Beck, K.L. Recent Developments in the Assessment of Nutrition Knowledge in Athletes. Curr. Nutr. Rep. 2022, 11, 241–252.
- Vázquez-Espino, K.; Rodas-Font, G.; Farran-Codina, A. Sport Nutrition Knowledge, Attitudes, Sources of Information, and Dietary Habits of Sport-Team Athletes. Nutrients 2022, 14, 1345.
- Janiczak, A.; Devlin, B.L.; Forsyth, A.; Trakman, G.L. A Systematic Review Update of Athletes’ Nutrition Knowledge and Association with Dietary Intake. Br. J. Nutr. 2022, 128, 1156–1169.
- Wardle, J.; Parmenter, K.; Waller, J. Nutrition Knowledge and Food Intake. Appetite 2000, 34, 269–275.
- Wansink, B.; Westgren, R.E.; Cheney, M.M. Hierarchy of Nutritional Knowledge That Relates to the Consumption of a Functional Food. Nutrition 2005, 21, 264–268.
- Heaney, S.; O’Connor, H.; Michael, S.; Gifford, J.; Naughton, G. Nutrition Knowledge in Athletes: A Systematic Review. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 248–261.
- Spronk, I.; Kullen, C.; Burdon, C.; O’Connor, H. Relationship between Nutrition Knowledge and Dietary Intake. Br. J. Nutr. 2014, 111, 1713–1726.
- Rosi, A.; Ferraris, C.; Guglielmetti, M.; Meroni, E.; Charron, M.; Menta, R.; Manini, F.; Di Gioia, V.; Martini, D.; Erba, D. Validation of a General and Sports Nutrition Knowledge Questionnaire in Italian Early Adolescents. Nutrients 2020, 12, 3121.
- Foo, W.L.; Faghy, M.A.; Sparks, A.; Newbury, J.W.; Gough, L.A. The Effects of a Nutrition Education Intervention on Sports Nutrition Knowledge during a Competitive Season in Highly Trained Adolescent Swimmers. Nutrients 2021, 13, 2713.
More
Information
Subjects:
Sport Sciences
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
19 Dec 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




