Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Noemi Fico | -- | 2602 | 2023-12-12 11:03:12 | | | |
| 2 | Camila Xu | Meta information modification | 2602 | 2023-12-13 02:22:21 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Fico, N.; Grezia, G.D.; Cuccurullo, V.; Salvia, A.A.H.; Iacomino, A.; Sciarra, A.; La Forgia, D.; Gatta, G. Breast Imaging Physics in Mammography (Part II). Encyclopedia. Available online: https://encyclopedia.pub/entry/52616 (accessed on 11 March 2026).
Fico N, Grezia GD, Cuccurullo V, Salvia AAH, Iacomino A, Sciarra A, et al. Breast Imaging Physics in Mammography (Part II). Encyclopedia. Available at: https://encyclopedia.pub/entry/52616. Accessed March 11, 2026.
Fico, Noemi, Graziella Di Grezia, Vincenzo Cuccurullo, Antonio Alessandro Helliot Salvia, Aniello Iacomino, Antonella Sciarra, Daniele La Forgia, Gianluca Gatta. "Breast Imaging Physics in Mammography (Part II)" Encyclopedia, https://encyclopedia.pub/entry/52616 (accessed March 11, 2026).
Fico, N., Grezia, G.D., Cuccurullo, V., Salvia, A.A.H., Iacomino, A., Sciarra, A., La Forgia, D., & Gatta, G. (2023, December 12). Breast Imaging Physics in Mammography (Part II). In Encyclopedia. https://encyclopedia.pub/entry/52616
Fico, Noemi, et al. "Breast Imaging Physics in Mammography (Part II)." Encyclopedia. Web. 12 December, 2023.
Copy Citation
Mammography is the gold standard for breast cancer diagnosis, as it is low cost, low administered radiation dose, and high sensitivity.
breast imaging
medical physics
mammography
1. Introduction
In Italy, breast cancer is the most frequently diagnosed neoplasm [1], and thanks to screening, mortality rates are lowered [2] since prevention, like early diagnosis, allows for more effective treatment [3]. With the increase in the number of screenings, there has been an increase in the incidence of breast cancer, probably due to more extensive diagnostic investigations [4][5][6][7].
Mammography is the gold standard for breast cancer diagnosis [8], as it is low cost, low administered radiation dose [9], and high sensitivity [10]. However, in previous work [11], there are also critical issues that are sometimes overcome [12], either by the use of higher performance machines or by more in-depth investigation techniques [13].
In order to make more effective diagnoses, quality images are required, and in difficult cases such as high densities, a more in-depth examination may be necessary [14][15][16][17][18][19].
2. Breast Tomosynthesis
Breast Digital Tomosynthesis is a technique used both as a screening tool for early breast cancer detection and a diagnostic tool for evaluating anomalies detected during clinical examination or mammography [20].
Breast Digital Tomosynthesis (DBT) is achieved using a tube that generates a beam of photons, with information related to the differential attenuation of X-rays as they pass through various structures that make up the patient’s area of interest [21].
The patient is in an anatomical position (standing with hands against the tube), parallel to the tube, and the breast is perpendicular to the generated beam. The breast is compressed to ensure even distribution and to prevent motion during image acquisition, which could generate artifacts [22][23][24].
The tube acquires an initial static image of the breast to obtain an initial overview and provide an understanding of the breast’s characteristics. Subsequently, images at discrete angles are acquired by rotating around the breast for a total of N. The acquisition is not along the circumference but at discrete angles, enhancing the ability to detect details and hidden structures [25][26].
Individual two-dimensional (2D) sections are reconstructed, resulting in a pseudo-three-dimensional image that provides a detailed view of breast structures. The acquired images are then reconstructed, pre-processed, and the DBT is finally obtained [27][28].
The patient’s position varies with each acquisition, and Breast Digital Tomosynthesis can be performed in various modes, providing different views. In the Mediolateral Oblique (MLO) projection, the patient stands with her raised arm while the tube rotates, while in the Cranio-Caudal (CC) projection, the tube is at a 90-degree angle, and the patient is standing [29][30][31].
The radiologist reviews the images, analyzing the different sections, focusing on the suspicious area and selecting a specific Region of Interest (ROI). [32] The suspicious area typically shows significant attenuation and may not be present in all sections. It may have irregular margins, microcalcifications, and calcium formations typically found within the lobular ducts [33]. Of course, there are also macrocalcifications, which are larger but not visible in these sections [34][35][36].
The initial diagnosis is made visually by recognizing suspicious structures and localizing the area for biopsy. For the biopsy, the patient is punctured in the suspicious area, and a sample of cells is collected through needle suction [37][38][39][40]. The histology by a pathologist is awaited, who studies the nature of the cells, either individually or in groups [41].
There are different classifications of tumors based on location (always within the mammary gland), such as lobular, intraductal, or pinwheel structures (distortions). [37][38][39][40][41][42][43][44]
New studies are implementing a machine learning algorithm (deep learning) by which Regions of Interest (ROI) obtained from the images can be used to verify the presence or absence of pathology [45][46][47][48]. The network identifies an unhealthy patient from a healthy one, attempting to locate the lesion [49]. This software is known as CAD (Computed Added Detection) [50][51][52].
There are differences between digital mammography (FFDM) and Breast Digital Tomosynthesis [53].
Mammography provides a two-dimensional image in which overlapping structures may hide anomalies, especially in cases of high breast density, potentially leading to false positives or false negatives [54]. In Breast Digital Tomosynthesis, the effect of tissue overlap is significantly reduced, resulting in increased sensitivity for detecting abnormalities and providing a more comprehensive and detailed view of breast structures [55][56].
Regarding dosimetry, mammography, being a single two-dimensional projection, involves a lower dose of radiation compared to Breast Digital Tomosynthesis [57][58]. The cumulative radiation dose for obtaining 3D images is slightly higher in Breast Digital Tomosynthesis, although it remains low [59][60][61][62].
Another difference is the time required for the examination. Traditional mammography is a faster and simpler examination, whereas Breast Digital Tomosynthesis involves greater data processing and longer examination times [63][64][65][66].
In terms of costs, traditional mammography is generally less expensive compared to Breast Digital Tomosynthesis, which requires specialized hardware and software for the acquisition and interpretation of 3D images [67][68][69].
In summary, Breast Digital Tomosynthesis is advantageous over traditional mammography due to its ability to provide more detailed information, reduce tissue overlap effects, and improve diagnostic capabilities while reducing false positives and negatives. However, the choice between the two often depends on availability, cost considerations, and the specific needs of the patient [70][71][72][73].
3. Radionuclide Imaging
Nuclear Medicine is based on the concentration of radioisotopes in living cells and tissues [74].
Nuclear Medicine has unique characteristics in diagnostic imaging because, unlike other methods, the image is based on differences in concentration and not density. [75] The examination is only possible on living humans or animals and expresses pathophysiological and molecular assumptions that provide original information compared to those with a more strictly morphostructural imprint [76].
If it is true that biological premises are also the basis of Magnetic Resonance Imaging and the use of radiological contrast agents, it is only in Nuclear Medicine that imaging is, by definition, “functional”. In fact, the possible marking with radioisotopes of the most important molecules of biological interest, cells, and drugs allows to trace the pathophysiology of all the functions of the human body, obtaining information that can allow for early diagnosis and a better connection with prognosis and therapy. The concept of the tracer expresses the nodal point of radioisotopic methods, much more than the nuclear radiation that gave its name to the discipline. In fact, if it is the radionuclide that allows for the external visualization of a radiocompound injected into a patient, it is the tracer that designs its behavior and capabilities, creating the conditions for a concentration that becomes the tool for understanding the molecular alteration and/or or pathophysiology that characterizes the disease [77].
In recent years, Nuclear Medicine imaging has assumed an important role in study and research, mainly in cardiology [78], neurology [79], and, above all, in oncology [80], due to its ability to produce high-resolution three-dimensional images of alterations in the metabolism of the human body, i.e., biochemical processes and cell activity, even before structural changes are highlighted [81][82][83][84]. These images are formed with computed tomographic methods that reconstruct the distribution in space of radiopharmaceuticals labeled with short half-life radionuclides and with reduced radiotoxicity, specifically injected into the patient [85]. The concentration of a radiocompound is present exclusively in the presence of ”functionally active” cells at the level of the territory examined, not being possible, for example, where there is fibrosis or necrosis [86]. Concentration variations and, therefore, the definition of a pathological event can precede the variations of the morpho-structural characteristics of a lesion [87]. Diagnostic imaging with radionuclides is an important method of investigation for many oncological pathologies. It provides both the evaluation of physiological and anatomical data, and information to easily guide the study, treatment, and follow-up of patients suffering from breast pathologies [88]. Scintimammography has also been shown to provide additional data that may change the planning strategy for primary breast cancer surgery in up to 10% of cases. Scintimammography provides additional information about the true extent of the disease so that surgical planning can be more accurately undertaken with the aim of complete surgical removal of breast cancer in a single operative procedure [89]. Nuclear Medicine also offers other very valid approaches, such as PET and Radioguided Surgery, especially useful in staging, therapy, and follow up of breast cancer [90][91][92].
4. CEM
Mammography, is the most widely used technique for symptomatic patients over 40 years of age and also for breast cancer screening of the entire population [93]. The technique is readily available and inexpensive, but it lacks sensitivity, especially for young patients, reflecting the increased breast density in this patient group. In the last two decades, spectral contrast-enhanced mammography (CEM) has been introduced. It is a technique that combines intravenous administration of iodinated contrast medium and digital mammography, exploiting the dual-energy technique to improve lesion detection [94]. It is also based on dual-energy 26–33 kVp and 44–50 kVp breast exposure after contrast administration, which makes pre-contrast exposure unnecessary. It exploits the neovascularisation of breast tumors in a similar way to breast MRI, providing a more precise imaging element. This is useful for subsequent action, which may be primary surgery or neoadjuvant chemotherapy. While the gold standard for breast cancer diagnostic investigation is MRI, the latter is costly, time-consuming, and prone to false positives. CEM may be an effective alternative due to the combined action of an iodinated contrast and conventional mammography technique, providing greater diagnostic accuracy, especially in patients with denser parenchymal background patterns, and may increase access to vascular imaging while reducing examination costs [95].
CEM allows the visualization of improved findings compared to normal unenhanced breast tissue by exploiting the increased contrast uptake of malignant neoplasms, becoming useful in the diagnosis and staging of primary breast cancer [96].
Retrospective reading studies have shown a significant improvement in the sensitivity and specificity of CEM to detect breast carcinomas compared to standard two-dimensional (2D) mammography. The improvement in sensitivity is due to the ability of CEM to identify tumors that would normally be masked by denser breast parenchyma on conventional mammography. Improvements in sensitivity with CEM are observed in women with denser background patterns and in younger pre-menopausal women, where a >20% improvement in sensitivity is possible. The equipment is similar to the mammogram, but a titanium or copper filter is added to obtain the high-energy image, followed by the use of post-processing software. CEM is performed with a single breast compression following injection of iodinated contrast agent (1.5 mL/kg body weight). MLO and CC projections are then performed on each breast, two minutes after the injection, followed by a double exposure of high and low energy. The low-energy exposure uses the same X-ray energy spectrum as a standard full-field digital mammogram (FFDM) with a kilovoltage peak of about 30 KVp, depending on the thickness and density of the compressed breast. The low-energy component is acquired using an X-ray spectrum identical to an FFDM, so it is not surprising that the image resembles a conventional mammogram. The high-energy exposure exploits the K-edge of the iodine, having a peak kilovoltage of about 45 KVp. As this technique has a double exposure of high and low energy, the radiation dose is therefore higher than FFDM. Using the dual-energy weighted logarithmic subtraction technique, images are produced, although the mode is less sensitive to motion artifacts than traditional temporal subtraction, however, with CEM, the times are more dilated [97].
The recombined image is also subject to a ’rim’ artifact with increased density at the periphery of the breast due to radiation scattering; an artifact that can be reduced by special scatter correction techniques. For each acquisition, lasting from 2 s to 20 s, depending on breast thickness and machine, high- (44–50 kVp) and low-energy (26–33 kVp) images are obtained. Both diagnostic images contribute to anatomical morphological information and the detection of possible lesions. High-energy imaging is obtained using energies above the k-edge of Iodine, which is not useful for diagnostic purposes but is useful for recombination imaging. The images are post-processed with dedicated software, and by using high- and low-energy images, a recombined image is obtained, minimizing the overlap of glandular tissue by maximizing the spread of contrast in the irradiated area. There are no standardized methodologies for the acquisition of contrast medium, dose, flow rate, contrast medium administration interval, and image acquisition, but reference is made to what was published in 2009 by C. Dromain, C. Balleyguier, G. Adler, J. R. Garbay, S. Delaloge, Contrast-enhanced digital mammography [98].
For the administration of contrast medium, the guidelines and precautions used in CT can be considered. In particular, the contrast medium is injected manually or preferably via an automatic injection pump at a rate of 2–3 mL/s, followed by a bolus of saline solution. After injection, the visualization time useful for image acquisition is about 10 min after administration. In particular, the acquisition can take place 2 to 2.5 min after administration within 10 min (including injection time), which is the final time for image acquisition.
The dual-energy technique involves double exposure for each projection, so the radiation dose is higher than in standard mammography.
This remains below the threshold of the European guidelines for screening mammography and the Mammography Quality Standards Act guidelines that state that increased dose is not a significant lifetime risk factor. CEM has high accuracy both in measuring the main lesion and in identifying multifocality and multicentricity of lesions, representing a 5–46% increase in sensitivity and a 3–15% increase in specificity over standard mammography. The limitation in comparison with MRI is the impossibility of an adequate study of the axillary cavities due to the overlapping field of view with mammography [99].
The administration of an iodinated contrast medium is essential for the examination. It carries a small risk of allergic reactions (<1% of cases), and they are usually mild and self-limiting. Another potential problem with iodinated contrast agent is contrast agent-induced nephropathy, so protocols have been developed to reduce the risk of acute renal damage, suggesting an assessment of renal function prior to contrast agent administration. Although CEM significantly improves the accuracy of local staging, false positives and false negatives still occur. A recognized reason for a false negative is when the lesion is not included in the mammographic field of view, but CEM compares favorably with MRI for local staging of breast cancer. In several studies of women with known carcinomas, CEM approaches the sensitivity of MRI with superior specificity.
5. Notes on Processing
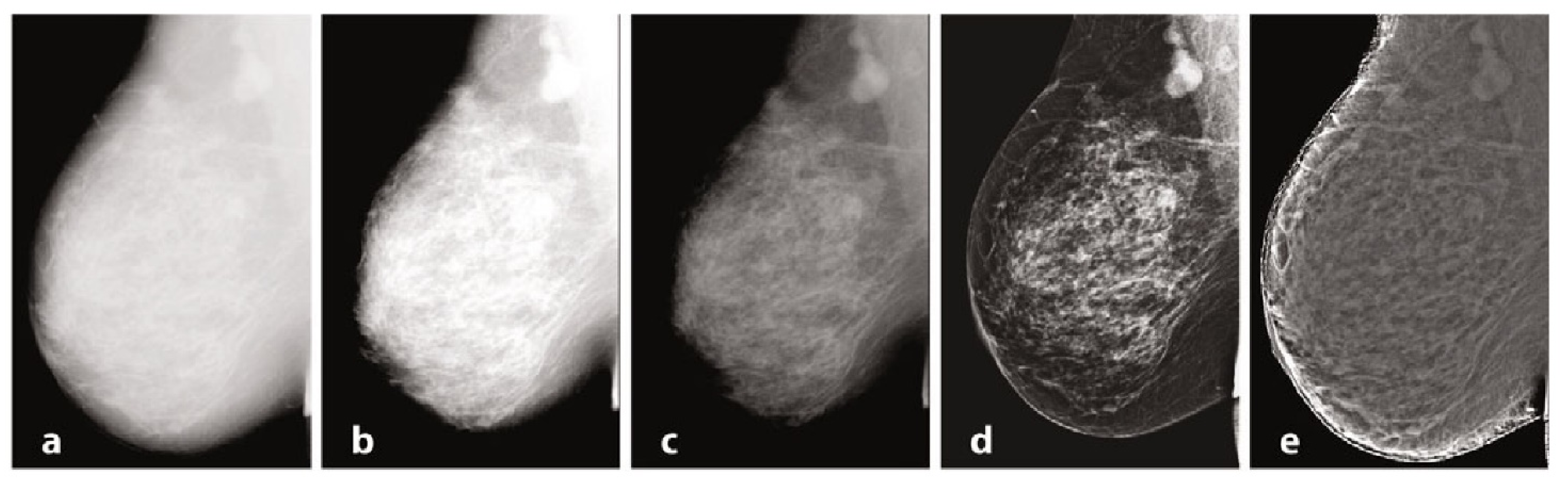
Mammography requires specific characteristics related to the type of instrumentation used and the exposure technique, with geometric parameters and beam energy. Of considerable importance for diagnostics are the characteristics of the detector and intrinsic processing. Processing, in particular, has the primary objective of limiting the effect of the thickness gradient between the part of the organ closest to the chest wall and the more distal part, which will have a decreasing thickness and attenuation [100]. In Figure 1, examples of processing are provided. The raw image (a) has low intrinsic contrast, and (b) varies the windowing by selecting a LUT suitable for more superficial regions, thus enhancing the visualization of peripheral regions with lesser thickness and reduced contrast on the internal tissue at the same time. [101] Also in mammography, as in traditional radiology, it is possible to find the application of LUTs after automatic segmentation of the grey level histogram, relative to tissues of interest: non-compressed adipose tissue, compressed adipose tissue, glandular tissue, and pectoral muscles. Other algorithms exploit unsharp masking, CLAHE histogram equalization, or frequency space analysis. In (c), the contrast was optimized by choosing a LUT suitable for more internal regions, but with a loss of information relative to the more superficial regions. Processing was performed by means of equalization-based processing algorithms, histogram in (d), and peripheral in (e), respectively. The latter is done by first applying a low-pass filter, typically Butterworth, with a cutoff frequency of 0.05 cycles per mm, from which an attenuation map is derived and compared to the original image to even out the thickness-related luminance gradient and allow for a uniform representation of the glandular structure [102].
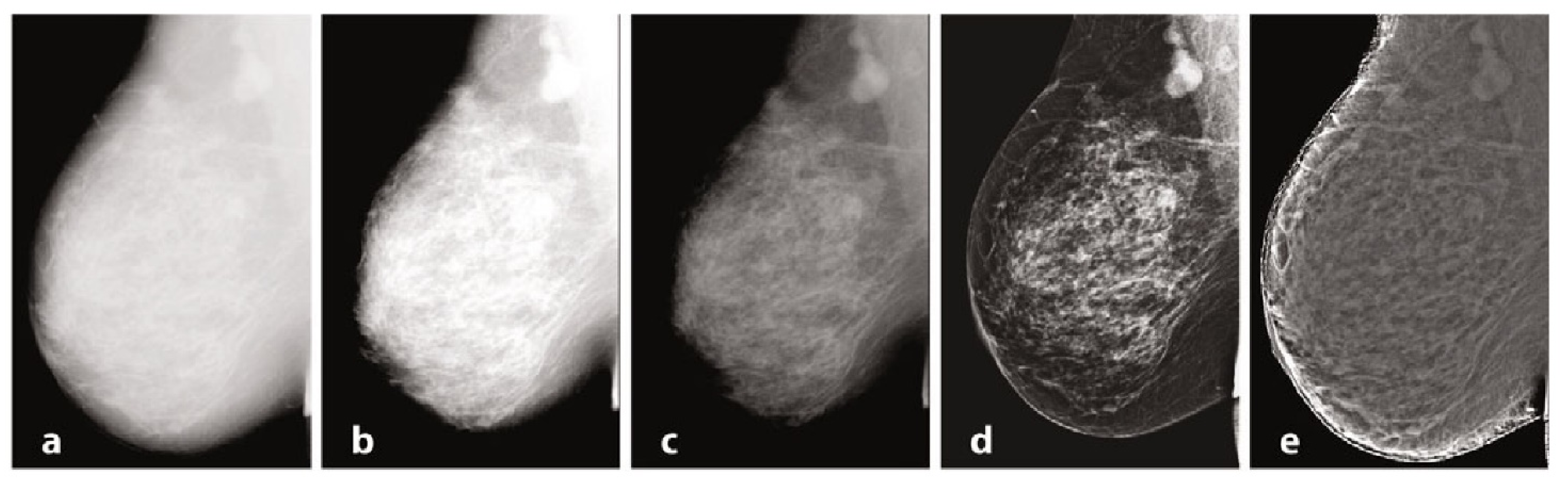
Figure 1. Mammography, different elaborations.
References
- Arzanova, E.; Mayrovitz, H.N. The Epidemiology of Breast Cancer. In Breast Cancer ; Mayrovitz, H.N., Ed.; Exon Publications: Brisbane, Australia, 2022; Chapter 1.
- Hulvat, M.C. Cancer Incidence and Trends. Surg. Clin. N. Am. 2020, 100, 469–481.
- Iacoviello, L.; Bonaccio, M.; de Gaetano, G.; Donati, M.B. Epidemiology of breast cancer, a paradigm of the “common soil” hypothesis. Semin. Cancer Biol. 2021, 72, 4–10.
- Lane, D.S.; Smith, R.A. Cancer Screening: Patient and Population Strategies. Med. Clin. N. Am. 2023, 107, 989–999.
- Duffy, S.; Vulkan, D.; Cuckle, H.; Parmar, D.; Sheikh, S.; Smith, R.; Evans, A.; Blyuss, O.; Johns, L.; Ellis, I.; et al. Annual mammographic screening to reduce breast cancer mortality in women from age 40 years: Long-term follow-up of the UK Age RCT. Health Technol. Assess. 2020, 24, 1–24.
- Evans, D.G.; Astley, S.; Stavrinos, P.; Harkness, E.; Donnelly, L.S.; Dawe, S.; Jacob, I.; Harvie, M.; Cuzick, J.; Brentnall, A.; et al. Improvement in Risk Prediction, Early Detection and Prevention of Breast Cancer in the NHS Breast Screening Programme and Family History Clinics: A Dual Cohort Study; NIHR Journals Library: Southampton, UK, 2016.
- Warner, E. Breast-cancer screening. N. Engl. J. Med. 2011, 365, 1025–1032.
- Berry, D.A. Breast cancer screening: Controversy of impact. Breast 2013, 22 (Suppl. 2), S73–S76.
- Edgar, L.; Glackin, M.; Hughes, C.; Rogers, K.M. Factors influencing participation in breast cancer screening. Br. J. Nurs. 2013, 22, 1021–1026.
- Garcia, E.M.; Storm, E.S.; Atkinson, L.; Kenny, E.; Mitchell, L.S. Current breast imaging modalities, advances, and impact on breast care. Obs. Gynecol. Clin. N. Am. 2013, 40, 429–457.
- Fico, N.; Di Grezia, G.; Cuccurullo, V.; Salvia, A.A.H.; Iacomino, A.; Sciarra, A.; Gatta, G. Breast Imaging Physics in Mammography (Part I). Diagnostics 2023, 13, 3227.
- Chikarmane, S.A.; Offit, L.R.; Giess, C.S. Synthetic Mammography: Benefits, Drawbacks, and Pitfalls. Radiographics 2023, 43, e230018.
- Cheung, Y.C.; Lin, Y.C.; Wan, Y.L.; Yeow, K.M.; Huang, P.C.; Lo, Y.F.; Tsai, H.P.; Ueng, S.H.; Chang, C.J. Diagnostic performance of dual-energy contrast-enhanced subtracted mammography in dense breasts compared to mammography alone: Interobserver blind-reading analysis. Eur. Radiol. 2014, 24, 2394–2403.
- Kerlikowske, K.; Grady, D.; Rubin, S.M.; Sandrock, C.; Ernster, V.L. Efficacy of Screening Mammography: A Meta-analysis. JAMA 1995, 273, 149.
- Burhenne, H.J.; Burhenne, L.W.; Goldberg, F.; Hislop, T.G.; Worth, A.J.; Rebbeck, P.M.; Kan, L. Interval breast cancers in the Screening Mammography Program of British Columbia: Analysis and classification. AJR Am. J. Roentgenol. 1994, 162, 1067–1071 discussion 1072–1075.
- Zackrisson, S.; Andersson, I. The development of breast radiology: The Acta Radiologica perspective. Acta Radiol. 2021, 62, 1473–1480.
- Zhang, M.; Mesurolle, B.; Theriault, M.; Meterissian, S.; Morris, E.A. Imaging of breast cancer-beyond the basics. Curr. Probl. Cancer 2023, 47, 100967.
- Gatta, G.; Pinto, A.; Romano, S.; Scaglione, A.A.M.; Volterrani, L. Clinical, mammographic and ultrasonographic features of blunt breast trauma. Eur. J. Radiol. 2006, 59, 327–333.
- Mahoney, M.C.; Newell, M.S. Breast intervention: How I do it. Radiology 2013, 268, 12–24.
- Hawley, J.R.; Kang-Chapman, J.K.; Bonnet, S.E.; Kerger, A.L.; Taylor, C.R.; Erdal, B.S. Diagnostic Accuracy of Digital Breast Tomosynthesis in the Evaluation of Palpable Breast Abnormalities. Acad. Radiol. 2018, 25, 297–304.
- Houssami, N.; Skaane, P. Overview of the evidence on digital breast tomosynthesis in breast cancer detection. Breast 2013, 22, 101–108.
- James, J.R.; Pavlicek, W.; Hanson, J.A.; Boltz, T.F.; Patel, B.K. Breast Radiation Dose With CESM Compared With 2D FFDM and 3D Tomosynthesis Mammography. AJR Am. J. Roentgenol. 2017, 208, 362.
- Nicosia, L.; Gnocchi, G.; Gorini, I.; Venturini, M.; Fontana, F.; Pesapane, F.; Abiuso, I.; Bozzini, A.C.; Pizzamiglio, M.; Latronico, A.; et al. History of Mammography: Analysis of Breast Imaging Diagnostic Achievements over the Last Century. Healthcare 2023, 11, 1596.
- Mandoul, C.; Verheyden, C.; Millet, I.; Orliac, C.; Pages, E.; Thomassin, I.; Taourel, P. Breast tomosynthesis: What do we know and where do we stand? Diagn. Interv. Imaging 2019, 100, 537–551.
- Chong, A.; Weinstein, S.P.; McDonald, E.S.; Conant, E.F. Digital Breast Tomosynthesis: Concepts and Clinical Practice. Radiology 2019, 292, 1–14.
- Rocha García, A.M.; Mera Fernández, D. Breast tomosynthesis: State of the art. Radiologia (Engl. Ed.) 2019, 61, 274–285.
- Tirada, N.; Li, G.; Dreizin, D.; Robinson, L.; Khorjekar, G.; Dromi, S.; Ernst, T. Digital Breast Tomosynthesis: Physics, Artifacts, and Quality Control Considerations. Radiographics 2019, 39, 413–426.
- Sujlana, P.S.; Mahesh, M.; Vedantham, S.; Harvey, S.C.; Mullen, L.A.; Woods, R.W. Digital breast tomosynthesis: Image acquisition principles and artifacts. Clin. Imaging 2019, 55, 188–195.
- Alzaghal, A.A.; DiPiro, P.J. Applications of Advanced Breast Imaging Modalities. Curr. Oncol. Rep. 2018, 20, 57.
- Durand, M.A. Synthesized Mammography: Clinical Evidence, Appearance, and Implementation. Diagnostics 2018, 8, 22.
- Liberatore, M.; Cucchi, J.M.; Fighiera, M.; Binet, A.; Missana, M.C.; Brunner, P.; Mourou, M.Y.; Iannessi, A. Interest of systematic tomosynthesis (3D mammography) with synthetic 2D mammography in breast cancer screening. Horm. Mol. Biol. Clin. Investig. 2017, 32, 20170024.
- Arıbal, E. Future of Breast Radiology. Eur. J. Breast Health 2023, 19, 262–266.
- Cuccurullo, V.; Prisco, M.; Di Stasio, G.; Mansi, L. Nuclear Medicine in Patients with NET: Radiolabeled Somatostatin Analogues and their Brothers. Curr. Radiopharm. 2017, 10, 74–84.
- Grigoryants, N.F.; Sass, S.; Alexander, J. Novel Technologies in Breast Imaging: A Scoping Review. Cureus 2023, 15, e44061.
- Di Grezia, G.; Prisco, V.; Iannaccone, T.; Grassi, R.; Serra, N.; Gatta, G. Personality disorders and temperamental traits in patients with breast disease: Preliminary results. Minerva Psichiatr. 2016, 57, 85–92.
- Takahashi, T.A.; Lee, C.I.; Johnson, K.M. Cleve Breast cancer screening: Does tomosynthesis augment mammography? Clin. J. Med. 2017, 84, 522–527.
- Ancona, A.; Capodieci, M.; Galiano, A.; Mangieri, F.; Lorusso, V.; Gatta, G. Vacuum-assisted biopsy diagnosis of atypical ductal hyperplasia and patient management|Diagnosi di iperplasia duttale atipica (ADH) con VAB. Manag. Radiol. Medica 2011, 116, 276–291.
- Gatta, G.; Di Grezia, G.; Ancona, A.; Capodieci, M.; Cappabianca, S.; Grassi, R. Underestimation of atypical lobular hyperplasia and lobular carcinoma in situ at stereotaxic 11-gauge vacuum-assisted breast biopsy. Eur. J. Inflamm. 2013, 11, 825–835.
- Sardu, C.; Gatta, G.; Pieretti, G.; Viola, L.; Sacra, C.; Di Grezia, G.; Musto, L.; Minelli, S.; La Forgia, D.; Capodieci, M.; et al. Underestimation of atypical lobular hyperplasia and lobular carcinoma in situ at stereotaxic 11-gauge vacuum-assisted breast biopsy. JACC Cardiovasc. Imaging 2021, 14, 426–438.
- Perry, N.; Broeders, M.; De Wolf, C.; Tornberg, S.; Holland, R.; Von Karsa, L. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition--summary document. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2008, 19, 614.
- Amy, D.; Durante, E.; Tot, T. The lobar approach to breast ultrasound imaging and surgery. J. Med. Ultrason. 2015, 42, 331–339.
- Smith, R.A.; Duffy, S.W.; Tabár, L. Breast cancer screening: The evolving evidence. Oncology 2012, 26, 471–475, 479–481, 485–486.
- Sharma, T.; Radosevich, J.A.; Pachori, G.; Mandal, C.C. A Molecular View of Pathological Microcalcification in Breast Cancer. J. Mammary Gland. Biol. Neoplasia. 2016, 21, 25–40.
- Gøtzsche, P.; Jørgensen, K. Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 2013.
- Jha, A.K.; Mithun, S.; Sherkhane, U.B.; Dwivedi, P.; Puts, S.; Osong, B.; Traverso, A.; Purandare, N.; Wee, L.; Rangarajan, V.; et al. Emerging role of quantitative imaging (radiomics) and artificial intelligence in precision oncology. Explor. Target. Antitumor. Ther. 2023, 4, 569–582.
- Najjar, R. Redefining Radiology: A Review of Artificial Intelligence Integration in Medical Imaging. Diagnostics 2023, 13, 2760.
- Kang, W.; Qiu, X.; Luo, Y.; Luo, J.; Liu, Y.; Xi, J.; Li, X.; Yang, Z. Application of radiomics-based multiomics combinations in the tumor microenvironment and cancer prognosis. J. Transl. Med. 2023, 21, 598.
- Wei, L.; Niraula, D.; Gates, E.D.H.; Fu, J.; Luo, Y.; Nyflot, M.J.; Bowen, S.R.; El Naqa, I.M.; Cui, S. Artificial intelligence (AI) and machine learning (ML) in precision oncology: A review on enhancing discoverability through multiomics integration. Br. J. Radiol. 2023, 96, 20230211.
- Erickson, B.; Korfiatis, P.; Akkus, Z.; Kline, T. Machine learning for medical imaging. Radiographics 2017, 37, 505–515.
- Brink, J.; Arenson, R.; Grist, T.M.; Lewin, J.S.; Enzmann, D. Bits and bytes: The future of radiology lies in informatics and information technology. Eur. Radiol. 2017, 27, 3647–3651.
- Syed, A.; Zoga, A.C. Artificial Intelligence in Radiology: Current Technology and Future Directions. Semin. Musculoskelet. Radiol. 2018, 22, 540.
- Kortesniemi, M.; Tsapaki, V.; Trianni, A.; Russo, P.; Maas, A.; Källman, H.; Brambilla, M.; Damilakis, J. The European Federation of Organisations for Medical Physics (EFOMP) White Paper: Big data and deep learning in medical imaging and in relation to medical physics profession. Phys. Medica 2018, 56, 90–93.
- Kornecki, A. Current Status of Contrast Enhanced Mammography: A Comprehensive Review. Can. Assoc. Radiol. J. 2022, 73, 141–156.
- Vaughan, C.L. Novel imaging approaches to screen for breast cancer: Recent advances and future prospects. Med. Eng. Phys. 2019, 72, 27–37.
- Di Grezia, G.; Romano, T.; De Francesco, F.; Somma, F.; Rea, G.; Grassi, R.; Gatta, G. Breast ultrasound in the management of gynecomastia in Peutz-Jeghers syndrome in monozygotic twins: Two case reports. J. Med. Case Rep. 2014, 8, 440.
- Sardu, C.; Gatta, G.; Pieretti, G.; Onofrio, N.; Balestrieri, M.L.; Scisciola, L.; Cappabianca, S.; Ferraro, G.; Nicoletti, G.F.; Signoriello, G.; et al. SGLT2 breast expression could affect the cardiovascular performance in pre-menopausal women with fatty vs. non fatty breast via over-inflammation and sirtuins’ down regulation. Eur. J. Intern. Med. 2023, 113, 57–68.
- Jochelson, M.; Hayes, D.F.; Ganz, P.A. Surveillance and monitoring in breast cancer survivors: Maximizing benefit and minimizing harm. Am. Soc. Clin. Oncol. Educ. Book 2013, 33, e13–e18.
- Moadel, R.M. Breast cancer imaging devices. Semin. Nucl. Med. 2011, 41, 229–241.
- Boujemaa, S.; Bosmans, H.; Bentayeb, F. Mammography Dose Survey Using International Quality Standards. J. Med. Imaging Radiat. Sci. 2019, 50, 529–535.
- Feig, S.A. Mammography equipment: Principles, features, selection. Radiol. Clin. N. Am. 1987, 25, 897–911.
- Behling, R. On a new multi-source X-ray tube concept for minimizing imaging time in digital breast tomosynthesis. Phys. Med. 2021, 88, 20–22.
- Bushberg, J.T. The AAPM/RSNA physics tutorial for residents. X-ray interactions. Radiographics 1998, 18, 457.
- Yaffe, M.J.; Rowlands, J.A. X-ray detectors for digital radiography. Phys. Med. Biol. 1997, 42, 1–39.
- Adcock, D.F.; Howe, D.B. Radiation dose and risk in screening mammography. J. Med. Syst. 1994, 18, 1738.
- Garton, A.J.; Dance, D.R. Estimation of tube potential in mammography from transmission measurements. Phys. Med. Biol. 1994, 39, 1247–1261.
- Bushberg, J.T. Uses of effective dose: The good, the bad, and the future. Health Phys. 2019, 116, 129.
- Maria, S.D.; Vedantham, S.; Vaz, P. X-ray dosimetry in breast cancer screening: 2D and 3D mammography. Eur. J. Radiol. 2022, 151, 110278.
- Wang, G.; Shi, D.; Guo, Q.; Zhang, H.; Wang, S.; Ren, K. Radiomics Based on Digital Mammography Helps to Identify Mammographic Masses Suspicious for Cancer. Front. Oncol. 2022, 12, 843436.
- Dromain, C.; Balleyguier, C.; Adler, G.; Garbay, J.R.; Delaloge, S. Contrast-enhanced digital mammography. Eur. J. Radiol. 2009, 69, 34.
- Young, K.C. Radiation doses in the UK trial of breast screening in women aged 40–48 years. Br. J. Radiol. 2002, 75, 362–370.
- Haus, A.G.; Yaffe, M.J.; Feig, S.A.; Hendrick, R.E.; Butler, P.A.; Wilcox, P.A.; Bansal, S. Relationship between phantom failure rates and radiation dose in mammography accreditation. Med. Phys. 2001, 28, 2297–2301.
- Hammerstein, G.; Miller, D.; White, D.; Masterson, M.; Woodard, H.; Laughlin, J. Absorbed radiation dose in mammography. Radiology 1979, 130, 485–491.
- Robson, K.J. A parametric method for determining mammographic X-ray tube output and half value layer. Br. J. Radiol. 2001, 74, 335–340.
- Goldsmith, S.J. Update on nuclear medicine imaging of neuroendocrine tumors. Future Oncol. 2009, 5, 75–84.
- Miles, K.; McQueen, L.; Ngai, S.; Law, P. Evidence-based medicine and clinical fluorodeoxyglucose PET/MRI in oncology. Cancer Imaging 2015, 15, 18.
- Basu, S.; Hess, S.; Nielsen Braad, P.E.; Olsen, B.B.; Inglev, S.; Høilund-Carlsen, P.F. The Basic Principles of FDG-PET/CT Imaging. PET Clin. 2014, 9, 355–370.
- Farwell, M.D.; Pryma, D.A.; Mankoff, D.A. PET/CT imaging in cancer: Current applications and future directions. Cancer 2014, 120, 3433–3445.
- Cascini, G.; Cuccurullo, V.; Tamburrini, O.; Rotondo, A.; Mansi, L. Neurological applications for myocardial MIBG scintigraphy. Nucl. Med. Rev. Cent. East. Eur. 2013, 16, 35–41.
- Payami, H. The emerging science of precision medicine and pharmacogenomics for Parkinson’s disease. Mov. Disord. 2017, 32, 1139–1146.
- Basu, S.; Kwee, T.C.; Surti, S.; Akin, E.A.; Yoo, D.; Alavi, A. Fundamentals of PET and PET/CT imaging. Ann. N. Y. Acad. Sci. 2011, 1228, 1–18.
- Fraum, T.J.; Fowler, K.J.; McConathy, J. PET/MRI: Emerging Clinical Applications in Oncology. Acad. Radiol. 2016, 23, 220–236.
- Evangelista, L.; Cervino, A.R.; Guttilla, A.; Zattoni, F.; Cuccurullo, V.; Mansi, L. 18F-fluoromethylcholine or 18F-fluoroethylcholine pet for prostate cancer imaging: Which is better? A literature revision. Nucl. Med. Biol. 2015, 42, 340–348.
- Cuccurullo, V.; Cioce, F.; Sica, A.; Iasiello, F.; Capasso, R.; Gatta, G.; Rubini, G. Gastroenteric diseases in the third millennium: A rational approach to optimal imaging technique and patient selection. Recenti Prog. Med. 2012, 103, 426–430.
- Fendler, W.P.; Rahbar, K.; Herrmann, K.; Kratochwil, C.; Eiber, M. 177Lu-PSMA Radioligand Therapy for Prostate Cancer. J. Nucl. Med. 2017, 58, 1196–1200.
- Win, Z.; Al-Nahhas, A.; Rubello, D.; Gross, M.D. Somatostatin receptor PET imaging with Gallium-68 labeled peptides. Q. J. Nucl. Med. Mol. Imaging Off. Publ. Ital. Assoc. Nucl. Med. 2007, 51, 244–250.
- Cuccurullo, V.; Di Stasio, G.; Schilliro, M.L.; Mansi, L. Small-Animal Molecular Imaging for Preclinical Cancer Research: PET and SPECT. Curr. Radiopharm. 2016, 9, 102–113.
- Schwarzenboeck, S.M.; Rauscher, I.; Bluemel, C.; Fendler, W.P.; Rowe, S.P.; Pomper, M.G.; Afshar-Oromieh, A.; Herrmann, K.; Eiber, M. PSMA Ligands for PET Imaging of Prostate Cancer. J. Nucl. Med. 2017, 58, 1545–1552.
- Briganti, V.; Cuccurullo, V.; Di Stasio, G.; Mansi, L. Gamma Emitters in Pancreatic Endocrine Tumors Imaging in the PET Era: Is there a Clinical Space for 99mTc-peptides? Curr. Radiopharm. 2019, 12, 156–170.
- Cuccurullo, V.; Di Stasio, G.; Prisco, M.; Mansi, L. Is there a clinical usefulness for radiolabeled somatostatin analogues beyond the consolidated role in NETs? Indian J. Radiol. Imaging 2017, 27, 509–516.
- Buscombe, J.R.; Holloway, B.; Roche, N.; Bombardieri, E. Position of nuclear medicine modalities in the diagnostic work-up of breast cancer. Q. J. Nucl. Med. Mol. Imaging 2004, 48, 109–118.
- Cuccurullo, V.; Di Stasio, G.; Mansi, L. Radioguided surgery with radiolabeled somatostatin analogs: Not only in GEP-NETs. Nucl. Med. Rev. Cent. East. Eur. 2017, 20, 49–56.
- Maffione, A.M.; Marzola, M.C.; Capirci, C.; Colletti, P.M.; Rubello, D. Value of (18)F-FDG PET for Predicting Response to Neoadjuvant Therapy in Rectal Cancer: Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2015, 204, 1261–1268.
- James, J.; Tennant, S.L. Contrast-enhanced spectral mammography (CESM). Clin. Radiol. 2018, 73, 715.
- Zanardo, M.; Cozzi, A.; Trimboli, R.M.; Labaj, O.; Monti, C.B.; Schiaffino, S.; Carbonaro, L.A.; Sardanelli, F. Technique, protocols and adverse reactions for contrast-enhanced spectral mammography (CESM): A systematic review. Insights Imaging 2019, 10, 76.
- Ferraro, G.; Romano, T.; De Francesco, F.; Grandone, A.; D’Andrea, F.; Del Giudice, E.; Cataldo, C.; Gatta, G.; Di Grezia, G.; Perrone, L.; et al. Management of prepubertal gynecomastia in two monozygotic twins with Peutz-Jeghers syndrome: From aromatase inhibitors to subcutaneous mastectomy. Aesthetic Plast. Surg. 2013, 37, 1012–1022.
- Fischer, U.; Diekmann, F.; Helbich, T.; Preibsch, H.; Püsken, M.; Wenkel, E.; Wienbeck, S.; Fallenberg, E.M. Use of contrast-enhanced mammography for diagnosis of breast cancer. Radiologie 2023.
- Mahesh, M. The essential physics of medical imaging. Med. Phys. 2013, 40, 077301.
- van Nijnatten, T.J.A.; Lobbes, M.B.I.; Cozzi, A.; Patel, B.K.; Zuley, M.L.; Jochelson, M.S. Barriers to Implementation of Contrast-Enhanced Mammography in Clinical Practice: AJR Expert Panel Narrative Review. AJR Am. J. Roentgenol. 2023, 221, 3–6.
- Savaridas, S.L.; Tennant, S.L. Quantifying lesion enhancement on contrast-enhanced mammography: A review of published data. Clin. Radiol. 2022, 77, e313–e320.
- Samei, E. AAPM/RSNA physics tutorial for residents: Technological and psychophysical considerations for digital mammographic displays. Radiographics 2005, 25, 491–501.
- Pisano, E.D.; Yaffe, M.J. Digital mammography. Radiology 2005, 234, 353–362.
- Neri, E.; De Souza, N.; Brady, A.; Bayarri, A.A.; Becker, C.D.; Coppola, F.; Visser, J.; European Society of Radiology. What the radiologist should know about artificial intelligence—An ESR white paper. Insights Imaging 2019, 10, 44.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
756
Revisions:
2 times
(View History)
Update Date:
13 Dec 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





