You're using an outdated browser. Please upgrade to a modern browser for the best experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Samuel Smith | -- | 1680 | 2023-11-28 15:28:24 | | | |
| 2 | Catherine Yang | -2 word(s) | 1678 | 2023-11-30 02:15:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Smith, S.; Houghton, A.; Mockeridge, B.; Van Zundert, A. Apps in Anesthesia. Encyclopedia. Available online: https://encyclopedia.pub/entry/52149 (accessed on 21 December 2025).
Smith S, Houghton A, Mockeridge B, Van Zundert A. Apps in Anesthesia. Encyclopedia. Available at: https://encyclopedia.pub/entry/52149. Accessed December 21, 2025.
Smith, Samuel, Andrew Houghton, Brydie Mockeridge, André Van Zundert. "Apps in Anesthesia" Encyclopedia, https://encyclopedia.pub/entry/52149 (accessed December 21, 2025).
Smith, S., Houghton, A., Mockeridge, B., & Van Zundert, A. (2023, November 28). Apps in Anesthesia. In Encyclopedia. https://encyclopedia.pub/entry/52149
Smith, Samuel, et al. "Apps in Anesthesia." Encyclopedia. Web. 28 November, 2023.
Copy Citation
Modern anesthesia continues to be impacted in new and unforeseen ways by digital technology. Combining portability and versatility, mobile applications or “apps” provide a multitude of ways to enhance anesthetic and peri-operative care.
anesthesia
peri-operative medicine
mobile applications
1. Introduction
Medicine has embraced the Internet and mobile technologies at a rapid pace. Whilst the Internet initially relied on computers the size of cabinets, just 50 years later, pocket-sized smartphones have almost two million times their memory capacity and almost limitless potential [1]. These devices are ubiquitous, with 2022 ownership rates greater than 90% in many developed countries [1]. Thus, the cross-over of mobile technology into health was always inevitable.
Using Internet-connected mobile devices such as smartphones, anesthetists have access to information in an expedient manner, up to date, and available almost anywhere, anytime, including at the bedside. There are many areas within anesthesia that could be aided by mobile technology: peri-operative risk assessment, drug formularies and calculators, clinical decision-making support, crisis cognitive aids, billing, as well as on-the-go education [2][3][4][5][6][7][8]. Given the prevalence of mobile devices, it should come as no surprise that smartphone software applications (or apps) have experienced considerable uptake into anesthesia. In both Australian and American studies, 88–97% of anesthetists reported using smartphone apps in their clinical practice [9][10]. There remain, however, many questions about the legal, ethical, and practical usage of mobile technology within anesthesia [11][12].
2. The Definition of an App and its Use in Anesthesia
Mobile applications (or apps as they will be referred to) are software programs downloadable from the Internet “app stores” (e.g., Apple App Store/Google Play) that provide functionality for mobile devices [13]. Apps may be designed by the device manufacturer, or they may be created by independent third-party software developers. A 2022 report estimated that up to 99.99% of available Apple apps were these so-called “third-party apps” [14]. Whilst devices usually come pre-loaded with essential apps, users can download more apps from an app store either free, for a one-off purchase fee, or with a rolling subscription.
According to current estimates, there are well over 350,000 health-related applications available, and this number is expected to double every few years [15][16]. Whilst this number includes consumer-facing apps, apps have also found their way into mainstream medical practice, including anesthesia. Anesthesia-specific health apps can fulfill multiple roles to ensure optimal patient care [16][17]. These include clinical decision support, dosage calculators, and drug interaction guides, providing peri-operative risk and other relevant calculators, providing access to journals and textbooks, and facilitating advanced patient monitoring [16][17][18]. A 2020 survey showed 97% of Australian anesthetists reported using smartphone applications in their work [10][19]. Similar to prior studies, the most common types of apps used were drug and medical references [10][17]. Figure 1 outlines one classification system of anesthesia apps using app functionality, informed by previous reviews and the WHO classification of digital health interventions [16][20][21][22].
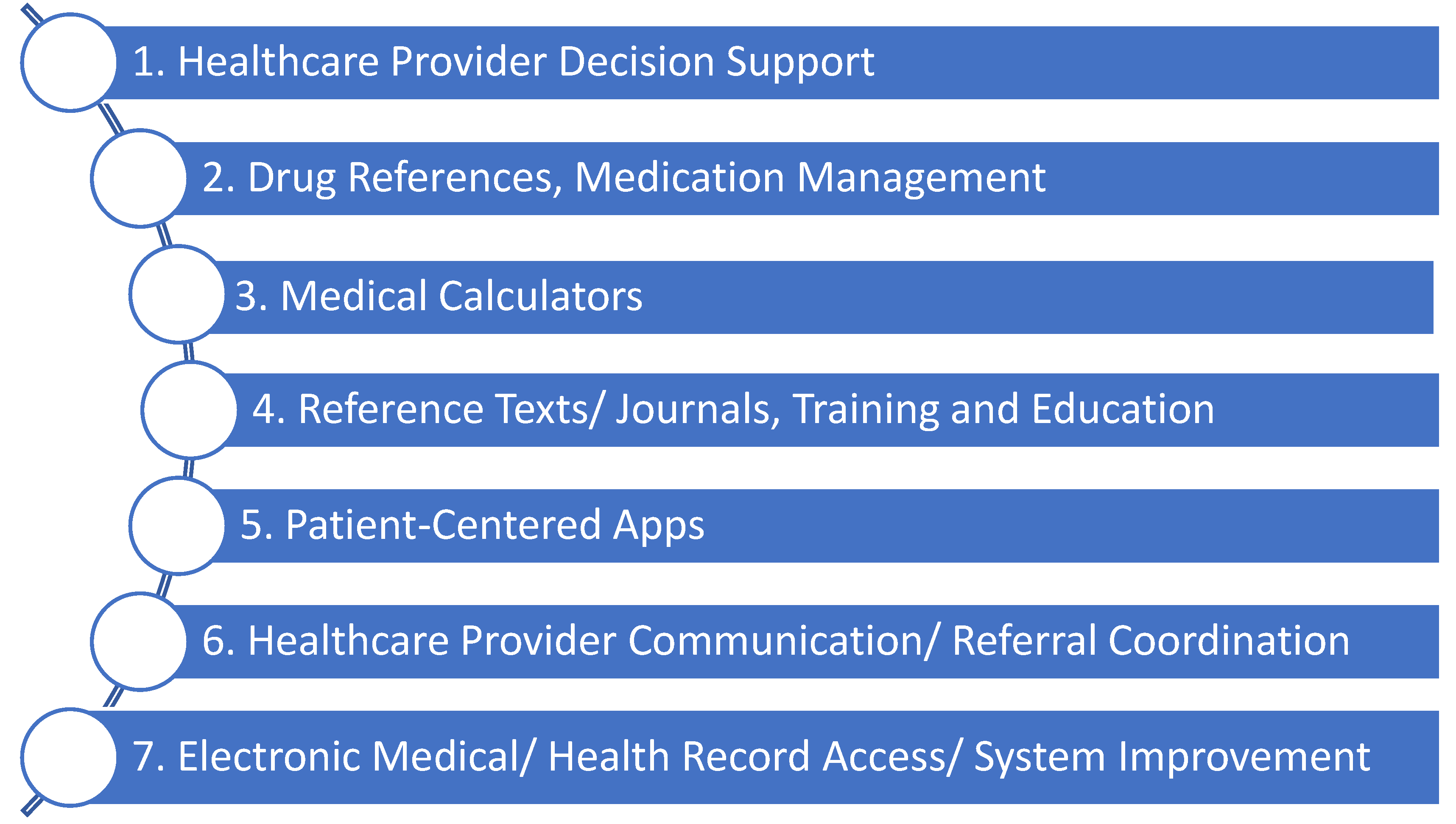
Figure 1. Functionality-based classification of anesthetic-related commercially available medical apps.
One can also classify anesthetic-specific apps by their anesthetic area of use (Figure 2). This alternative method of classification has two functions: firstly, it helps illustrate the many anesthetic-specific functions of apps and secondly, it has utility in focusing search terms when looking for apps [16].
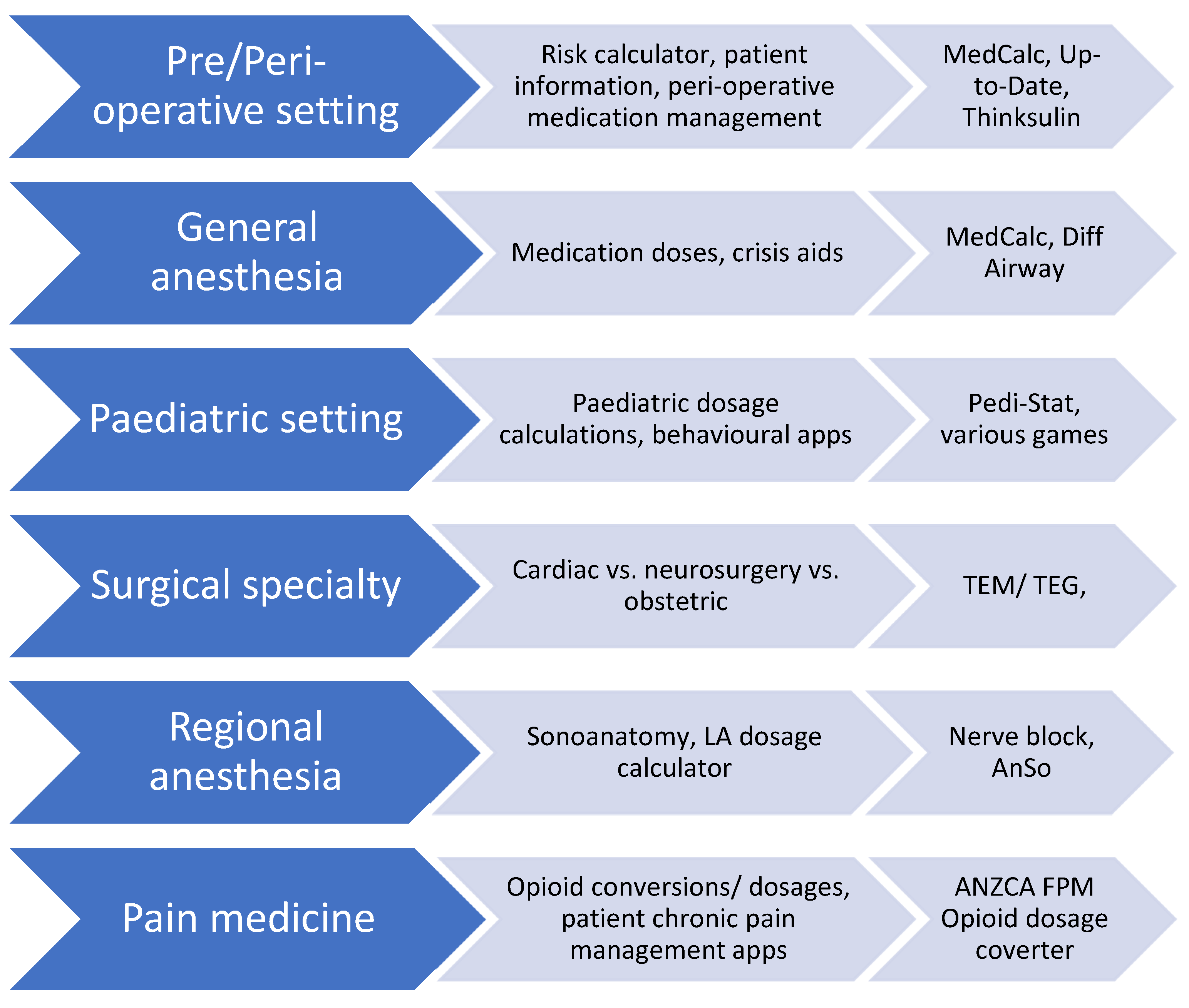
Figure 2. Specialty-based classification system of anesthetic applications.
Not all app categories seen in Figure 1 are at the same implementation stage in clinical practice. Patient-centered apps and clinical communication apps are in their relative infancy and require slightly different considerations than clinical apps used by clinicians currently. Health record access apps are usually designed by the medical records system operator, and thus there is often little choice in which app one can use. Therefore, this article will focus on apps currently commonly used in clinical anesthetic practice, namely: clinical decision tools, drug references, medical calculators, and reference texts [23].
3. Point of Care Healthcare Provider Clinical Decision Support Apps
Point-of-care apps are apps designed to be utilized at the patient's bedside to guide clinical decision making, for example, UpToDate [24]. The key feature of these apps is that they convey information quickly enough to make a clinical decision, which differentiates them from simply an electronic textbook. In general, point-of-care apps provide succinct summaries of conditions or clinical scenarios and outline specific and actionable management options. To support this aim, point-of-care apps must have easy-to-navigate design and make heavy use of algorithms and images. Clinical decision apps are of particular use in emergent situations, where the burden of cognitive load is well documented. One example is Medical Assistance eXpert (MAX), which guides users through common anesthesia emergencies [5]. This app was shown to improve the technical skills of anesthetic residents in crisis scenarios by over 10% [5]. In addition to being a guide to the general management of a condition, point-of-care apps can also utilize patient-level data to guide decision making. This can vary in complexity from simple apps displaying an algorithm to follow, all the way through to continually transmitting patient-worn devices that provide AI-generated clinical advice [25]. Another anesthetic example is a visual reaction time app that assesses the depth of propofol sedation to alert to impending oversedation [8]. Other evolving point-of-care apps can automatically generate cardiac indices from a single snapshot of an arterial waveform or measure exact pupillary light reflex in unconscious patients [26][27]. The Point-of-care clinical support apps have been shown to improve skills in managing local anesthetic toxicity, malignant hyperthermia, and peri-operative blood prescribing [28][29][30][31]. This diversity makes point-of-care apps particularly useful to anesthetists who must be able to manage a broad array of problems across the physiological spectrum.
4. Drug References and Medication Management Apps
Drug reference apps provide information about dosages, frequency, indications and contraindications, and adverse reactions to medications. Advanced features include pill identification (based on pill shape, color, or imprint), drug interaction generators, and automatic dose calculation. With an ever-increasing number of medications, it is almost impossible to stay abreast of every drug or formulation, especially as indications and safety advice change over time as a drug is in use. On average, 28 new medications are approved in the U.S. every year, each with its own interactions and anesthetic considerations [32]. Complicating this is the fact that 40% of patients over 75 years already present with polypharmacy, and this will only continue to grow as the population ages [33]. These patients are at high risk of medication-related harm; however, several apps are now available to help guide medication management in the peri-operative period, guiding which agents need to be discontinued, which anesthetic drugs should be avoided, which doses are required in specific patient groups (e.g., obesity, renal failure), and to help clinicians avoid medication-related harm [34].
There are several limitations to drug reference app use. These apps provide a very specific function within the larger clinical picture and cannot take over the role of the prescriber. Secondly, given the rapid pace of drug development, apps may not always be up to date, although they hold a large advantage over paper references in this respect. Finally, these apps suffer from regionality given geographical differences in drug availability. Thus, before using or purchasing a drug reference app, one must be sure it is applicable in one’s locality.
5. Medical Calculator Apps
There are many mathematical formulae used daily in anesthesia, the most common being weight-based medication dosing. Whilst there may be something said for the sad state of arithmetic in modern medicine, there is undeniably a patient safety advantage in automating these procedures. Such apps have a wide array of uses. For example, one available app allows an anesthetist to calculate the carbon dioxide emissions and thus the environmental impact of inhalational anesthesia [6]. Another use of medical calculators is risk score calculation. Risk stratification scores have multiplied in recent years to support evidence-based decision-making, for example, the CHA2DS2-VASc of stroke in atrial fibrillation, the Child-Pugh score for cirrhosis grading, and the Apfel score for post-operative nausea and vomiting [35][36][37][38][39]. Having these scoring systems available on an app has several advantages. Firstly, it takes a relatively small amount of space for an app to store up to several thousand scoring systems, far more than any person’s memory could contain. Having such a large array of risk prediction tools on an app also means anesthetists can be exposed to scoring tools they may not otherwise have known about. Secondly, with improved access to these tools on an anesthetist’s phone, there is easier integration of evidence-based scoring systems into practice. Thirdly, most calculator apps provide clinical suggestions about how to proceed with management based on the risk scores produced. This saves time compared to a clinician calculating a score (which will take extra time without an app), and then using several resources to determine what to do with said score. Finally, increased availability of “big data” means more complex, but potentially more powerful, risk prediction tools can be produced that might only be able to be calculated using app technology. For example, the American College of Emergency Physicians COVID-19 management tool was rapidly developed using national datasets in response to the ongoing pandemic; however, it is complex and would be extremely difficult to do without an app. Dissemination and calculation via apps such as MDCalc allowed for rapid national and international uptake, improving management for patients [39]. The allure of medical calculator apps is the effective, rapid, conversion of patient parameters into actionable scores or numbers, allowing anesthetists to better provide evidence-based care [39].
6. Reference Texts/Journal and Education Apps
Reference apps centralize access to databases, journals, or books. As medicine evolves the ability to access the most up-to-date information and research on the go is invaluable as it affords the opportunity to essentially change practice to be in line with the best evidence in real-time. Apps may belong to either a single journal or provide a single login point to multiple journals or resources. With a reference app, a large array of multi-modal educational opportunities can be presented wherever an anesthetist is, without the need to carry voluminous texts around. Furthermore, as these apps are internet-connected, they can provide anesthetists with research updates on relevant topics, ensuring that one remains as current as possible. Apps with a pure education focus also exist, allowing mobile training in a wide array of areas, including simulated cases, general medical knowledge, and more.
References
- Deffree, S. Electronic News Design. Available online: https://www.edn.com/arpanet-establishes-1st-computer-to-computer-link-october-29-1969/ (accessed on 4 March 2023).
- Baumann, D.; Dibbern, N.; Sehner, S.; Zöllner, C.; Reip, W.; Kubitz, J.C. Validation of a mobile app for reducing errors of administration of medications in an emergency. J. Clin. Monit. Comput. 2019, 33, 531–539.
- Karippacheril, J.G.; Mathai, R.T.; Abraham, S.S. Insulin IP Calc: A smartphone application for insulin infusion protocol in Intensive Care Units. Indian J. Anaesth. 2015, 59, 829–830.
- Lee, D.W.; Thampi, S.; Yap, E.P.; Liu, E.H. Evaluation of a smartphone camera system to enable visualization and image transmission to aid tracheal intubation with the Airtraq(®) laryngoscope. J. Anesth. 2016, 30, 514–517.
- Lelaidier, R.; Balança, B.; Boet, S.; Faure, A.; Lilot, M.; Lecomte, F.; Lehot, J.J.; Rimmelé, T.; Cejka, J.C. Use of a hand-held digital cognitive aid in simulated crises: The MAX randomized controlled trial. Br. J. Anaesth. 2017, 119, 1015–1021.
- Pierce, J.M.T.; Taylor, R. Validation of the mathematics in the anaesthetic impact calculator, a smartphone app for the calculation the CO2 e of inhalational anaesthesia. Anaesthesia 2020, 75, 136–138.
- Schiavoni, L.; Pascarella, G.; Grande, S.; Agrò, F.E. Neuromuscular block monitoring by smartphone application (i-TOF© system): An observational pilot study. NPJ Digit. Med. 2020, 3, 137.
- Thomson, A.J.; Nimmo, A.F.; Tiplady, B.; Glen, J.B. Evaluation of a new method of assessing depth of sedation using two-choice visual reaction time testing on a mobile phone. Anaesthesia 2009, 64, 32–38.
- Green, M.S.; Mathew, J.J.; Gundigi Venkatesh, A.; Green, P.; Tariq, R. Utilization of Smartphone Applications by Anesthesia Providers. Anesthesiol. Res. Pract. 2018, 2018, 8694357.
- Perkins, E.J.; Edelman, D.; Brewster, D.J. Smartphone use and perceptions of their benefit and detriment within Australian anaesthetic practice. Anaesth. Intensive Care 2020, 48, 366–372.
- Parker, L.; Karliychuk, T.; Gillies, D.; Mintzes, B.; Raven, M.; Grundy, Q. A health app developer’s guide to law and policy: A multi-sector policy analysis. BMC Med. Inform. Decis. Mak. 2017, 17, 141.
- Yang, Y.T.; Silverman, R.D. Mobile health applications: The patchwork of legal and liability issues suggests strategies to improve oversight. Health Aff. 2014, 33, 222–227.
- U.S. Food and Drug Administration. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/policy-device-software-functions-and-mobile-medical-applications (accessed on 24 April 2023).
- Camindale, J.; von Wartburg, M. The Success of Third-Party Apps on the App Store. AG 2022. Available online: https://www.apple.com/newsroom/pdfs/the-success-of-third-party-apps-on-the-app-store.pdf (accessed on 16 March 2023).
- Gordon, W.J.; Landman, A.; Zhang, H.; Bates, D.W. Beyond validation: Getting health apps into clinical practice. NPJ Digit. Med. 2020, 3, 14.
- Pan, S.; Rong, L.Q. Mobile Applications in Clinical and Perioperative Care for Anesthesia: Narrative Review. J. Med. Internet Res. 2021, 23, e25115.
- Alhomary, M.; Kinirons, B. Survey of Smartphone Use among Anaesthetists In Saolta University Health Care Group Midlands Setting. Ir. Med. J. 2018, 111, 709.
- Bhansali, R.; Armstrong, J. Smartphone applications for pediatric anesthesia. Paediatr. Anaesth. 2012, 22, 400–404.
- Irfan, M.E.; Ginige, J.A. Comparative Study of Medical Reference and Information Mobile Apps for Healthcare Professionals and Students. Stud. Health Technol. Inform. 2018, 254, 43–52.
- Seabrook, H.J.; Stromer, J.N.; Shevkenek, C.; Bharwani, A.; de Grood, J.; Ghali, W.A. Medical applications: A database and characterization of apps in Apple iOS and Android platforms. BMC Res. Notes 2014, 7, 573.
- Ventola, C.L. Mobile devices and apps for health care professionals: Uses and benefits. Pharm. Ther. 2014, 39, 356–364.
- World Health Organization. Available online: https://apps.who.int/iris/bitstream/handle/10665/260480/WHO-RHR-18.06-eng.pdf;jsessionid=EF5C7B012765D3D18F62E3B3C71E67DC?sequence=1 (accessed on 18 May 2023).
- Carvalho, H.; Verdonck, M.; Forget, P.; Poelaert, J. Acceptance of mHealth among health professionals: A case study on anesthesia practitioners. BMC Anesth. 2020, 20, 55.
- UpToDate. Available online: www.uptodate.com (accessed on 2 May 2023).
- Colquhoun, D.A.; Davis, R.P.; Tremper, T.T.; Mace, J.J.; Gombert, J.M.; Sheldon, W.D.; Connolly, J.J.; Adams, J.F.; Tremper, K.K. Design of a novel multifunction decision support/alerting system for in-patient acute care, ICU and floor (AlertWatch AC). BMC Anesth. 2021, 21, 196.
- Hoppe, P.; Gleibs, F.; Briesenick, L.; Joosten, A.; Saugel, B. Estimation of pulse pressure variation and cardiac output in patients having major abdominal surgery: A comparison between a mobile application for snapshot pulse wave analysis and invasive pulse wave analysis. J. Clin. Monit. Comput. 2021, 35, 1203–1209.
- Shin, Y.D.; Bae, J.H.; Kwon, E.J.; Kim, H.T.; Lee, T.S.; Choi, Y.J. Assessment of pupillary light reflex using a smartphone application. Exp. Ther. Med. 2016, 12, 720–724.
- Berkenstadt, H.; Yusim, Y.; Ziv, A.; Ezri, T.; Perel, A. An assessment of a point-of-care information system for the anesthesia provider in simulated malignant hyperthermia crisis. Anesth. Analg. 2006, 102, 530–532.
- Gupta, R.K.; McEvoy, M.D. Initial Experience of the American Society of Regional Anesthesia and Pain Medicine Coags Regional Smartphone Application: A Novel Report of Global Distribution and Clinical Usage of an Electronic Decision Support Tool to Enhance Guideline Use. Reg. Anesth. Pain Med. 2016, 41, 334–338.
- McEvoy, M.D.; Hand, W.R.; Stoll, W.D.; Furse, C.M.; Nietert, P.J. Adherence to guidelines for the management of local anesthetic systemic toxicity is improved by an electronic decision support tool and designated “Reader”. Reg. Anesth. Pain Med. 2014, 39, 299–305.
- Watson, P.; Watson, D.; Dhesi, A.; New, H.V.; Davidson, A.; Armstrong, R.; Birchall, J. Improving blood-prescribing decisions: Evaluating the efficacy of a blood guidelines app. Transfus. Med. 2020, 30, 485–491.
- Batta, A.; Kalra, B.S.; Khirasaria, R. Trends in FDA drug approvals over last 2 decades: An observational study. J. Fam. Med. Prim. Care 2020, 9, 105–114.
- World Health Organization. Available online: https://www.who.int/publications/i/item/WHO-UHC-SDS-2019.11 (accessed on 12 December 2022).
- Smith, S. Medscape and iPhone apps: The stethoscope of the 21st-century medical student? App review. Med. Stud. J. Aust. 2017, 8, 30–36.
- Apfel, C.C.; Läärä, E.; Koivuranta, M.; Greim, C.A.; Roewer, N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anaesthesia 1999, 91, 693–700.
- Child, C.G.; Turcotte, J.G. Surgery and portal hypertension. Major Probl. Clin. Surg. 1964, 1, 50–64.
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272.
- Suh, E.H.; Lang, K.J.; Zerihun, L.M. Modified PRIEST score for identification of very low-risk COVID patients. Am. J. Emerg. Med. 2021, 47, 213–216.
- Patel, R.S.; Bachu, R.; Adikey, A.; Malik, M.; Shah, M. Factors Related to Physician Burnout and Its Consequences: A Review. Behav. Sci. 2018, 8, 98.
More
Information
Subjects:
Anesthesiology; Medical Informatics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
870
Revisions:
2 times
(View History)
Update Date:
30 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




