Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sarfaraz K. Niazi | -- | 5248 | 2023-11-24 14:42:30 | | | |
| 2 | Wendy Huang | Meta information modification | 5248 | 2023-11-27 10:38:29 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Niazi, S.K. Current Techniques in Drug Delivery across Blood–Brain Barrier. Encyclopedia. Available online: https://encyclopedia.pub/entry/52040 (accessed on 08 February 2026).
Niazi SK. Current Techniques in Drug Delivery across Blood–Brain Barrier. Encyclopedia. Available at: https://encyclopedia.pub/entry/52040. Accessed February 08, 2026.
Niazi, Sarfaraz K.. "Current Techniques in Drug Delivery across Blood–Brain Barrier" Encyclopedia, https://encyclopedia.pub/entry/52040 (accessed February 08, 2026).
Niazi, S.K. (2023, November 24). Current Techniques in Drug Delivery across Blood–Brain Barrier. In Encyclopedia. https://encyclopedia.pub/entry/52040
Niazi, Sarfaraz K.. "Current Techniques in Drug Delivery across Blood–Brain Barrier." Encyclopedia. Web. 24 November, 2023.
Copy Citation
Non-invasive drug delivery across the blood-brain barrier (BBB) represents a significant advancement in treating neurological diseases. The BBB is a tightly packed layer of endothelial cells that shields the brain from harmful substances in the blood, allowing necessary nutrients to pass through. It is a highly selective barrier, which poses a challenge to delivering therapeutic agents into the brain. Several non-invasive procedures and devices have been developed or are currently being investigated to enhance drug delivery across the BBB.
blood–brain barrier
neurodegenerative disorders
drug delivery
focused ultrasound
microbubbles
MRI
electromagnetic field
1. Introduction
Evolutionarily, the brain is the body’s control center, responsible for everything from essential autonomic functions like heartbeat and respiration to complex cognitive tasks and emotional processing [1]. The human brain, with its intricate architecture and countless functions, is undeniably one of the most sophisticated organs in the body [2]. Protecting and ensuring the optimal functioning of this organ is of paramount importance. The BBB is central to this protective mechanism, a physiological marvel that safeguards the neural environment from potential toxins and pathogens [3] (Figure 1). However, the very features that make the BBB an efficient protector make it a formidable neurotherapeutic obstacle [4].
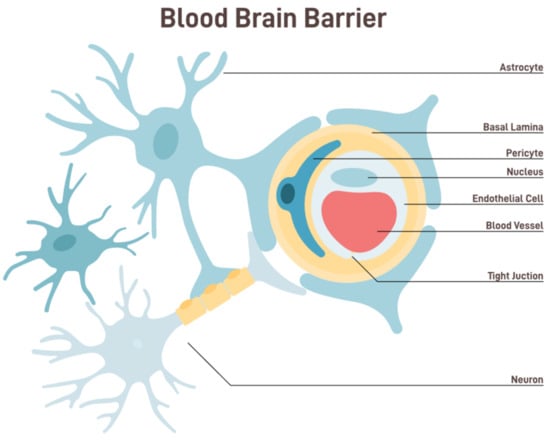
Figure 1. Anatomy and functional components of BBB [shutterstock_2229011587].
The BBB is a semipermeable border that separates the circulating blood from the brain and extracellular fluid in the central nervous system (CNS) [5]. Endothelial cells that line the capillaries make up this barrier; they are tightly packed and have tight junctions to seal them. These tight junctions restrict the passive diffusion of large or hydrophilic molecules into the CNS. Additionally, astrocyte foot processes wrap around the blood vessels, further fortifying this barrier and playing a pivotal role in its function [6]. The BBB, while allowing essential nutrients like glucose and amino acids to reach the brain, filters out potentially harmful substances from entering the neural environment. This selective permeability ensures that the brain remains relatively insulated from fluctuations in blood composition, thereby maintaining a stable internal environment [7].
The BBB poses a monumental challenge for reaching therapeutic agents to the central CNS in the grand drug delivery arena. The development of effective, non-invasive, device-mediated techniques for drug delivery across the BBB has been fraught with challenges but illuminated by moments of innovation and breakthrough. As the field progresses, it is imperative to prioritize safety, ensuring that the integrity and function of the BBB are not compromised in the long term. With continued research and interdisciplinary collaboration, the dream of effective and patient-friendly CNS drug delivery methods may soon become a reality (Figure 2).
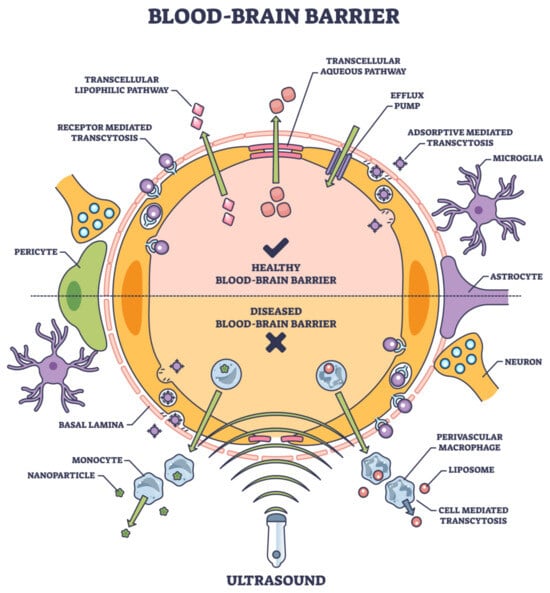
Figure 2. Noninvasive tools and their entry into BBB are based on their physical properties, composition, surface chemistry, and target ligands. [Adobe Stock Photo_603623040].
The drug’s solubility, surface charge distribution, molecular weight, particle size, and other factors should all be considered while creating the formulation [8].
While often successful in peripheral tissues, traditional pharmacological strategies have encountered substantial limitations when aiming for the brain. These methods aim to increase BBB permeability transiently and safely, allowing for targeted drug delivery without the drawbacks of the traditional methods [9]. Many small molecules and virtually all large-molecule biologics, including therapeutic proteins, RNA therapeutics, and antibodies, face impediments in crossing the BBB [10]. Figure 2 lists several approaches to noninvasive deliveries.
Transcellular (drug delivery via cells) and paracellular (drug delivery between adjacent cells) are the two main routes that frequently carry drugs to the brain [11]. Ions and solutes passively diffuse across the BBB via the paracellular pathway, which concentration gradients facilitate. Transcellular delivery across the BBB involves the passage of drugs or molecules through endothelial cells, which form the protective barrier for the brain. Unlike paracellular transport, which consists of passing between cells, transcellular transport goes through the cells themselves, making it a critical route for delivering therapeutic agents to the brain. There are several ways that this process can happen, such as the passive diffusion of small, lipophilic molecules, the carrier-mediated transport made possible by certain proteins, the receptor-mediated transcytosis in which ligands bind to receptors, and the adsorptive-mediated transcytosis in which cationic molecules interact with parts of the cell surface. Each mechanism has unique properties and requirements, making them essential in designing drug-delivery strategies for neurological disorders and brain-related diseases [12] (Figure 2).
Several mechanistic mechanisms, including transcytosis, carrier-mediated transport, and passive diffusion, are part of the transcellular route. The main mechanisms are adsorptive-mediated transcytosis (AMT) and receptor-mediated transcytosis (RMT). Among the most studied targets for RMT in brain endothelial cells are the transferrin receptor, insulin receptor, and low-density lipoprotein (LDL) receptor [13]. Current advancements in RMT provide ways to get past the blood-brain barrier and achieve more efficient medicine administration to the brain. Brain medication administration also uses other transporters, such as organic anion and cation transporters, in addition to these mechanical pathways [14].
Several techniques have been developed over the years, endeavoring to overcome the formidable barrier of the BBB and deliver therapeutic agents to the CNS. Conventional methods range from direct injection into the CNS to modifying drug molecules for enhanced permeability. While some of these techniques have had moderate success, they often come with significant drawbacks, such as invasiveness, limited targeting, or potential side effects.
2. Direct Injections
Techniques like intracerebroventricular (ICV) and intraparenchymal injections bypass the BBB by delivering drugs directly into the brain or cerebrospinal fluid. While effective, these methods are highly invasive, bear risks of infection, and might distribute drugs unevenly [15]. Methods such as intracerebral injections or intraventricular infusions were employed to achieve CNS drug delivery [16]. While these approaches enable a direct route of administration, they are invasive and carry associated risks, including infection, hemorrhage, and potential damage to brain tissue [17]. Moreover, these methods can lead to non-uniform distribution in the brain, potentially yielding areas of over-concentration or insufficient drug coverage [18]. Further complicating the drug delivery scenario is the realization that many CNS disorders, such as AD, PD, and MS, involve multiple brain regions [19]. Targeting these dispersed areas necessitates a systemic approach to drug delivery, ensuring that the therapeutic agent is distributed throughout the brain.
3. Molecular Trojan Horses
This ingenious method involves coupling therapeutic agents to molecules crossing the BBB via receptor-mediated transcytosis. By “piggybacking” on these molecules, drugs can be sneaked into the brain. While promising, the complexity of this method and potential immunogenic reactions are challenges that need addressing [20]. It is possible to facilitate the entry of chemical drugs into the brain by employing naturally occurring or artificially modified chemicals and certain simple life forms, predominantly viruses, which can traverse the BBB. This drug delivery strategy is usually called the “Trojan horse” approach. Neurotropic viruses are a class of viruses that exhibit a distinct preference for the nervous system and possess the ability to invade neural cells. These viral agents can traverse the BBB and get access to the CNS. Hence, utilizing neurotropic viruses for drug encapsulation and BBB traversal is a highly effective and practical strategy. Adeno-associated virus (AAV) is the prevailing neurotropic viral vector employed in treating neurological illnesses [21].
4. Biochemical BBB Disruption
Specific agents, like mannitol, can temporarily disrupt the BBB by shrinking endothelial cells. While this allows drugs to enter the CNS, it is a non-specific method that might allow harmful substances to infiltrate the brain, potentially causing side effects [22]. The hyperosmolar technique is employed to transiently disrupt the BBB by generating alterations in osmolarity inside the brain tissue. Usually, an intravenous or intra-arterial infusion of a high-osmolarity solution, predominantly mannitol, facilitates water movement from brain tissue to the blood arteries via osmosis.
Applying mechanical force on the endothelial cells induces mechanical stress, resulting in a transient disturbance of tight junctions. During this phase, the BBB undergoes temporary permeability, facilitating enhanced medication delivery into the brain and enabling therapeutic effects on NDs. Experimental proof from clinical trials shows that giving hyperosmolar mannitol through an intra-arterial infusion after a BBB breach is a safe and effective way to treat central CNS cancers. The findings from subsequent research using rats indicated that proteomics alterations reverted to their original levels after 96 h. This suggests that the approach employed to induce BBB opening is transient and may be reversed [23]. Still, it is important to note that using hyperosmolar mannitol to open the BBB without a guide is an invasive process whose safety should be carefully thought through.
5. Nanoparticle-Mediated Delivery
Nanoparticle systems encompass various carriers, including liposomes, polymeric nanoparticles, and solid lipid nanoparticles (SLNP). These carriers are commonly categorized based on their size (usually ranging from 10 to 300 nm in diameter), chemical composition, and physical morphology. Numerous investigations have examined the utilization of nanoparticles ranging in size from 50 to 200 nm in the context of stroke, AD, and PD. The initial formulation of nanoparticles for cancer treatment received regulatory approval decades ago. Nevertheless, the current repertoire of licensed nanoparticle-based therapies and technologies remains limited. For instance, the utilization of lipid nanoparticles (LNP) for administering mRNA COVID-19 vaccines has gained approval. However, it is essential to note that there is currently a lack of approved central nervous system (CNS) therapy products.
There is great interest in optimizing the physicochemical characteristics of nanoparticles to govern their track and permeability, which might be of great significance in crossing the BBB [24]. Many nanocarriers with particle sizes ranging from 1 to 100 nm have been developed due to advancements in nanotechnology. As shown in Figure 1, these nanocarriers include polymeric nanoparticles (PNPs), solid lipid nanoparticles (SLNPs), liposomes, and micelles. They have been used to treat a number of neurological disorders. More recently developed, sophisticated nanocarriers, such as exosomes [25], prodrugs [26], self-assembled micelles [27], dendrimers [28], PNPs [29], and exosomes [25], have shown great potential over previous delivery methods.
Non-targeted nanoparticles have significant limitations in traversing the intact BBB. Nanoparticles can encapsulate drugs and be designed to target specific receptors or transporters on the BBB, enhancing drug delivery. This field has garnered considerable interest, but concerns about long-term effects and potential toxicity linger [30]. Utilizing tailored nanomedicines to improve brain transport by capitalizing on the compromised BBB resulting from brain illnesses, such as neurodevelopmental disorders, presents a promising strategy for medication delivery [31].
Nanoparticles as non-invasive methods for drug delivery across the BBB have gained traction due to their effectiveness and versatility. They can be engineered to enhance the delivery of various therapeutic agents to the brain, overcoming the formidable obstacle presented by the BBB. One mechanism through which nanoparticles facilitate drug delivery is by encapsulating drugs and protecting them from metabolic degradation in the bloodstream, enhancing their half-life and bioavailability. A study by Saraiva et al. (2016) [30] demonstrated the use of multi-functionalized nanoparticles to deliver anti-inflammatory drugs to the brain, showing a reduction in neuroinflammation in a targeted and controlled manner. Additionally, surface modification of nanoparticles has been explored to improve their ability to cross the BBB. Poly (butyl cyanoacrylate) nanoparticles coated with polysorbate 80 can help deliver drugs like dalargin, tubocurarine, and doxorubicin across the BBB effectively [32].
Targeted delivery is another essential aspect of nanoparticle-based drug delivery, including the development of magnetic nanoparticles, which could be guided to the brain using an external magnetic field, enhancing the site-specific delivery of the encapsulated drugs [33]. Due to their small size and customizable properties, Nanoparticles serve as excellent vehicles for drug delivery. Combined with techniques like FUS, they can be directed precisely, allowing for slow and sustained drug release [34].
Research involving the co-delivery of gold nanoparticles and anticancer drugs to glioblastoma cells showcased enhanced cell uptake and increased therapeutic efficiency, owing to the synergistic combination of nanoparticles and FUS [35].
Nanotechnology offers avenues to develop carriers that can transport drugs and respond to external stimuli, such as temperature or magnetic fields, enabling controlled release at target sites [36]. When combined with focused ultrasound, magnetic-responsive nanoparticles demonstrated synchronized drug release upon reaching targeted brain regions, presenting a dual-control mechanism for drug delivery [37]. Using an external magnetic field to guide their targeted delivery, magnetic nanoparticles to transport therapeutic agents across the BBB are also attempted [38].
6. Focused Ultrasound (FUS) with Microbubbles
FUS is a non-invasive medical device employing ultrasonic waves to concentrate and transmit energy to locations within tissues. The application of this technique exhibits significant promise in augmenting the transportation of pharmaceutical agents via the BBB to enhance their uptake in the brain for therapeutic purposes. This can be achieved by facilitating the permeability of the BBB or by aiding in the controlled breakdown of microbubbles to facilitate the release of pharmaceuticals [39]). Presently, focused ultrasound (FUS) has been utilized in neurological disorders (NDs) such as AD and PD (PD). This technique can potentially improve the efficacy of brain drug delivery for a wide range of therapeutic agents, including antibodies, nanoparticles, therapeutic viruses, and stem cells. This is achieved through the temporary opening of the BBB. Several studies have investigated the application of FUS in this context [40][41][42][43][44][45]. When used together, FUS and viral vector gene therapy improve the ability of drugs to get to the brain in animal models of Parkinson's disease. The feasibility and safety of FUS-mediated BBB opening of the striatum have been established in clinical surgical operations for PD (PD) [46].
FUS, combined with microbubbles, has emerged as a frontrunner in non-invasive BBB modulation. The process involves injecting microbubbles intravenously and then applying targeted ultrasound waves. The interaction between the microbubbles and the ultrasound waves temporarily increases the permeability of the BBB, allowing for targeted drug delivery. Preclinical studies have shown successful delivery of therapeutic agents, ranging from small molecules to larger biologics, into the brain with this method [47]. The precision of FUS ensures targeted delivery, minimizing potential systemic side effects. One such method, which has garnered significant attention, is focused ultrasound (FUS) in conjunction with microbubbles [48]. The technique involves the transient disruption of the BBB using ultrasound waves targeted to specific brain regions, enabling the delivery of therapeutic agents precisely where needed. Early results from preclinical studies have shown this technique to be both practical and safe, with the BBB being restored within hours post-treatment [49].
7. Magnetic Resonance Imaging (MRI)
To deal with the fact that the hyperosmolar process is invasive, scientists have come up with an MRI method that uses unenhanced chemical exchange saturation transfer to find the buildup of mannitol in the brain after the BBB opens. This technique holds promise as a prompt imaging tool for optimizing the administration of mannitol-based BBB opening, thereby enhancing its safety and effectiveness [50]. Moreover, implementing hyperosmolar BBB opening techniques in murine models using MRI guidance can effectively mitigate the limitations of inconsistent reproducibility and heterogeneous experimental results commonly observed with the intra-arterial administration of hyperosmolar mannitol [51]. Hence, the exclusive utilization of hyperosmolar mannitol infusion has potential hazards in therapeutic contexts. Still, using MRI guidance makes osmotic-based BBB opening safer and more effective, which increases its therapeutic value.
MRI guidance has significantly improved the precision of focused ultrasound techniques. Through MRgFUS, clinicians can visualize the targeted area in real-time, ensuring therapeutic agents’ accurate and effective delivery while monitoring potential complications [52]. A clinical trial exploring the efficacy of MRgFUS for essential tremor treatments showcased the ability to target the thalamus accurately. Patients exhibited substantial improvement in hand tremors, underlining the potential of imaging-guided interventions [53]. In a rat model of ischemic stroke, FUS, combined with microbubbles, facilitated the targeted delivery of neuroprotective drugs. The treated rats exhibited reduced infarct sizes and improved neurological outcomes compared to the control group [54]. For example, trials using FUS and a combination of FUS+MRI for AD trials saw the BBB in the hippocampus and entorhinal cortex open reversibly without adverse effects [55], and patients showed no adverse events and no cognitive or neurological deterioration [56]. The PD trials of 5–7 patients involved the BBB duplication at the parietal–occipital–temporal junction opened reversibly in four patients without side effects [57]. FUS-mediated striatal BBB opening is feasible and safe. In the MPS-II trial of 28 patients, positive changes occurred in 21 patients treated with transferrin receptor ligand, some with mild or moderate, transient, and manageable adverse drug events [58].
8. Electromagnetic Field Modulation
While relatively nascent, using electromagnetic fields (EMFs) to modulate BBB permeability is gaining traction. EMFs can influence ion channels and transport mechanisms in the endothelial cells of the BBB, leading to transient permeability increases [59]. Preliminary studies show promise, but the exact parameters for effective and safe application and long-term implications remain under investigation [60]. Another intriguing approach is the use of electromagnetic fields. By leveraging the inherent electrical properties of the BBB, researchers are exploring ways to transiently increase its permeability, allowing for the passive diffusion of therapeutic agents into the CNS [61].
Preliminary studies have indicated a potential for this technique, although its long-term effects and safety profile are still under investigation. Emerging techniques promise selectivity, control, and reversibility. For instance, focused ultrasound, when coupled with microbubbles, can be directed at specific brain regions to enhance BBB permeability temporarily. Studies have shown that this technique can deliver a variety of therapeutic agents, including antibodies, to targeted brain areas with minimal side effects. Furthermore, although a relatively new entrant in this domain, electromagnetic fields have demonstrated potential in modulating BBB permeability. Initial studies suggest that such fields can influence molecular transport across the BBB, although the precise mechanisms and long-term safety still require thorough investigation.
9. Vasoactive Chemicals
Vasoactive chemicals, including CNS ones, can modulate vascular tone and permeability. Several vasoactive chemicals have been investigated to assess their capacity to induce the opening of the BBB and facilitate the transportation of therapeutic medicines into the brain. The chemicals encompass adenosine, bradykinin, histamine, and peptides derived from bee venom. Adenosine, a nucleoside found in nature, has a role in multiple physiological processes, such as regulating blood flow and inflammation [62].
Numerous studies have demonstrated that it can enhance BBB permeability through various mechanisms. For instance, it can activate adenosine receptors on endothelial cells, initiating intracellular signaling pathways that influence the tight junctions between them. These tight junctions play a critical role in maintaining the integrity of the BBB. The process of fibrinolysis can lead to the production of bradykinin through the action of fibrinolytic agents [63]. This bradykinin can then activate bradykinin B2 receptors, resulting in the opening of the BBB. Researchers have employed the BBB opening mechanism to create bradykinin analogs that can improve the transportation of nanocarriers across the BBB to treat glioblastoma [64].
Furthermore, studies have provided evidence that the disruption of the BBB, facilitated by the bradykinin B2 receptor agonist NG291, is confined to a specific area, dependent on the dosage administered, and can be reversed [65]. Histamine, a neurotransmitter, has been observed to potentially facilitate the opening of the BBB [66][67]. However, the precise mechanism by which this occurs remains uncertain.
Recently, there has been a development in the utilization of bee venom peptides as substances to induce the opening of the BBB. It has been demonstrated that these substances can induce reversible opening of the BBB within 24 h when administered at adequate dosages. Doubtless, vasoactive medicines possess significant promise in facilitating the opening of the BBB and enhancing drug transportation to the brain. Nevertheless, the systemic administration of these medications presents uncertain implications for the overall treatment efficacy, as they cannot selectively target the BBB. Enhancing the precision of BBB targeting with pertinent technology would contribute to advancing future clinical studies.
10. Gut Microbiome [68]
The enhanced longevity of the human life span can be attributed to advancements in diet and healthcare, which the progress of the economy and technology has facilitated. Many microorganisms, encompassing bacteria, archaea, viruses, and diverse eukaryotes, including fungi and protozoa, inhabit distinct ecological niches within the gastrointestinal tract. The term “gut microbiota” is commonly used to refer to this group of microorganisms.
The gut microbiota significantly impacts various areas of human physiology, encompassing nutritional metabolism, anti-infection mechanisms, immune system functionality, and neuron development. The gut microbiota is facing a changing environment due to rapid industrialization, urbanization, and advancements in food and medical technologies. Factors such as increased fast-food consumption have made the gut microbiota more susceptible to vulnerability than previous conditions. Recently, there has been a growing recognition of the significance of gut microbiota due to its crucial involvement in neurodevelopmental disorders (NDs) and its influence on the differentiation, maturation, proliferation, and activation of immune cells residing in the central nervous system (CNS). The gut–brain axis (GBA) facilitates reciprocal communication between the gastrointestinal tract and the central nervous system using neurotransmitters and other metabolites [69][70].
The blood-brain barrier (BBB) can restrict the transit of molecules produced from the stomach into the brain, even though it acts as a gateway for the passage of many essential compounds needed for CNS functioning and secretes substances into the blood and brain essential for preserving CNS homeostasis [71]. Microorganism-associated molecular patterns (MAMPs), for instance, are vital to microorganisms’ structural integrity and cellular processes [72]. Inadvertent elevation or reduction of MAMPs can cause acute or chronic inflammation linked to several neurological conditions.
The BBB’s permeability is linked to several microbial compounds, including vitamins, lipopolysaccharides (LPS), trimethylamines (TMAs), and short-chain fatty acids (SCFAs) [73][74][75]. These compounds may boost the immunological and endocrine systems to prevent neuroinflammation or neurodegeneration or act directly on brain neurons through the blood-brain barrier. The central nervous system (CNS), autonomic nervous system (ANS), enteric nervous system (ENS), and hypothalamic-pituitary-adrenal (HPA) axis make up the bidirectional communication network.
Through the vagus nerve, microbiota and the brain can communicate. The CNS can affect the functions and activities of intestinal cells more efficiently, thanks to the synergy of neurological and hormonal signals [76][77]. Furthermore, the gut microbiota influences host health by modifying gut cells and preserving intestinal metabolic and immunological balance [78][79][80]. It’s interesting to note that the microbiota also affects the synthesis of hormones and neurotransmitters, including peptide YY, gam-ma-aminobutyric acid (GABA), serotonin (5-HT), adrenaline, noradrenaline, glucagon-like peptide-1, and dopamine, as well as their precursors. These chemicals act on the CNS or ENS either directly through the vagus nerve or indirectly by affecting the circulation [81].
11. Surface Transporters
Activating BBB surface transporters can help drugs get to where they need to go, but it is important to think about the problems with this method, like the fact that it can become saturated, has limited transport capacity, and is not as good at targeting as receptor-mediated endocytosis. Consequently, the latter mechanism is commonly employed in drug development to enhance the targeting and penetration of drugs across the BBB. At the moment, transferrin receptors, insulin receptors, and low-density lipoprotein receptor-related proteins are the most common receptor proteins in the BBB. These receptor proteins are frequently coupled with therapeutic protein drugs through fusion with their respective ligands, thereby enhancing the efficacy of drug targeting and facilitating the passage across the BBB [82].
12. Penetrating Peptides
Penetrating peptides refer to concise sequences of peptides that can efficiently penetrate the BBB. BBB-penetrating peptides’ repertoire includes trans-activating transcriptional activator peptides, R8 peptides, angiopep-2, cell-penetrating peptides, and RVG peptides [83]. Using BBB-targeting ligands for transporting pharmaceuticals across the BBB represents a precise and efficient approach to facilitating drug delivery.
13. Extracellular Vesicles
One approach to enhancing the ability of medications to penetrate the brain is by modifying tiny extracellular vesicles’ surfaces with different peptides that can cross the BBB. This modification facilitates the effective transport of drugs to the brain [84]. Furthermore, integrating extracellular vesicles and intranasal delivery would undeniably assume a crucial function in managing neurodegenerative disorders (NDs). Extracellular vesicles serve as inherent vehicles for drug delivery and possess the ability to traverse the BBB readily. Consequently, it is common practice among researchers to employ extracellular vesicles as carriers for drug encapsulation, aiming to enhance the transportation of pharmaceuticals across the BBB, where the improved permeability of the BBB can be achieved by utilizing tiny extracellular vesicles produced from glial cells, which are loaded with tetraspanin 2 siRNA [85].
14. Liposomes
Like extracellular vesicles, liposomes are also employed as carriers for drug administration across the BBB. Nevertheless, it is essential to acknowledge that liposomes exclusively exhibit BBB penetration capabilities rather than BBB targeting abilities. Consequently, these compounds are frequently co-administered with BBB-targeting agents to elicit their desired outcomes. It has been demonstrated that including neurotransmitter-derived lipids in lipid nanoparticles (LNPs) that are impervious to the BBB facilitates the ability of LNPs to traverse the BBB [86].
15. Optical Imaging
Integrating optical imaging with non-invasive techniques offers detailed real-time visualization at a cellular level. Optogenetics allows for the control of neuronal activity using light, suggesting potential therapeutic applications [87]. A study involving the treatment of Parkinson’s symptoms in rodents used optogenetics. The integration of optical imaging ensured targeted light delivery, leading to controlled neuronal activity and symptom alleviation [88]. Precision is critical in non-invasive drug delivery. The advent of novel imaging techniques promises better visualization, improved targeting, and real-time monitoring of drug delivery [89]. The integration of diffuse optical tomography with ultrasound has shown potential in providing real-time imaging of drug deposition and tissue response, enhancing the safety and efficacy of drug delivery [90].
16. Peptides
Peptides are very important for receptor-mediated transcytosis because they can interact with specific BBB receptors. This is how peptides help deliver different therapeutic agents, such as small molecules, proteins, and genes across the BBB. These peptides target endogenous receptor systems, ensuring a selective and efficient transfer [91].
A lot of research has been done on how peptides can help deliver drugs across the BBB without damaging it. This is because they can use the body's own transport systems to do this without damaging the barrier's structure. One prominent strategy involves the design of peptides that can undergo receptor-mediated transcytosis. These peptides are specifically tailored to bind to specific receptors on the endothelial cells of the BBB, instigating a process that transports them, along with their drug cargo, into the brain. How peptides could be engineered for targeted delivery, enhancing the selectivity and efficiency of drug transport while minimizing systemic exposure, has been reported [92].
Additionally, the use of cell-penetrating peptides (CPPs) has gained attention. CPPs can facilitate the transport of various bioactive cargoes, including small molecules, peptides, proteins, and nucleic acids, across the BBB, particularly the CPP-mediated [93] transport. Furthermore, developing dual-functional peptides that combine BBB targeting and drug delivery is an emerging trend. Constructing a dual-functional peptide that could transport across the BBB and target glioma cells underscores the advancements in precision medicine [94].
17. Antibodies
Antibodies, especially monoclonal ones, have been significantly instrumental in drug delivery across the BBB. They can uniquely target specific receptors on the endothelial cells lining the BBB, enabling receptor-mediated transcytosis. This process involves binding antibodies to these receptors, initiating an internalization process that transports them and their attached drug cargo across the BBB. The efficacy of antibodies in drug delivery can be enhanced by reducing their affinity for a transcytosis target, consequently boosting their brain uptake [95]. The bispecific antibodies, designed to engage with the transferrin receptor to facilitate BBB crossing and an amyloid-beta peptide to reduce its pathological accumulation in AD, exemplify engineered antibodies’ dual targeting capability and therapeutic potential [96]. Antibody engineering to improve antibodies’ pharmacokinetics increases their potential as drug carriers to the brain [97]. Antibodies are equally instrumental in bypassing the BBB. A specific example is the monoclonal antibody against the transferrin receptor, where antibodies with reduced affinity for a transcytosis target can significantly enhance the brain’s uptake of therapeutic antibodies [95].
18. Intranasal
In recent years, intranasal and intrathecal administration have developed viable and effective methods for enhancing brain-targeting efficiency in medication administration. The intranasal route of drug administration is a favorable method for the targeted delivery of medications to the central CNS owing to the abundant vascularization of the nasal cavity, which is situated near the brain. Research findings have indicated that the intranasal administration of exosomes can lead to a notable accumulation of these particles in the brains of animals with PD [98]. The intranasal delivery of dantrolene has demonstrated enhanced brain concentration and prolonged duration of action compared to oral administration [99]. The process of intrathecal administration entails the direct delivery of medications into the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord. This method bypasses the BBB and enables direct drug delivery to the CNS. Nevertheless, intrathecal administration is constrained because of its invasive characteristics, technical intricacy, probable unfavorable responses, restricted indications, and elevated expenses [100]. Capitalizing on the direct connection between the nasal cavity and the brain via the olfactory and trigeminal nerves, this method offers a direct pathway for drug delivery to the CNS. While still in its infancy, this approach has shown significant potential, especially for delivering peptides and other macromolecules that traditionally have difficulty crossing the BBB.
19. Circadian Rhythm [101]
The circadian rhythms, which regulate several human physiological and behavioral activities, are controlled by endogenous biological clocks coordinated by the suprachiasmatic nucleus. The circadian system significantly impacts various physiological functions, encompassing sleep, alertness, and cognitive ability. The perturbation of circadian homeostasis has harmful implications for human well-being. Neurodegenerative illnesses contain a diverse array of symptoms, with a notable characteristic being the presence of diurnal fluctuations in both frequency and intensity.
Furthermore, these illnesses have been found to alter the equilibrium of the circadian system, resulting in a detrimental impact on symptoms and overall quality of life. There is more and more evidence that circadian homeostasis and neurodegeneration are linked. This means that the proper functioning of circadian rhythms may be very important in making neurodegenerative diseases worse. Hence, the circadian system has emerged as a compelling subject of investigation and a promising avenue for advancements in research and clinical interventions. Looking into how disrupting circadian rhythms can affect neurodegenerative disorders can help us understand how neurodegeneration works and lead to the development of new therapies based on circadian rhythms for these painful conditions.
The sensitivity of the BBB to medications exhibits variability following the circadian rhythm. It has been demonstrated that the administration of the antiepileptic medicine phenytoin during nighttime has enhanced efficacy in the treatment of seizure models in fruit flies [102]. One potential cost-effective method could involve strategically managing medicine administration time to optimize travel efficiency.
20. Precision Medicine
Precision medicine encompasses several strategies to achieve more accurate drug targeting, optimal drug dose, refined illness subtyping, and the meticulous management of individual variations. With targeting methods, localized drug administration to the specific lesions, and techniques like co-focused ultrasound in conjunction with microbubbles, it is possible to get accurate medication targeting and dosage. Nevertheless, categorizing diseases into subtypes remains ambiguous for neurological disorders (NDs), and comprehending individual variations poses significant difficulties. This signifies a substantial avenue for future therapy of neurodegenerative disorders.
21. Light-Induced Techniques
Optogenetics and photobiomodulation harness light to affect cellular activity. Recent advancements indicate potential in modulating BBB permeability using specific wavelengths of light, especially when combined with photosensitive agents [103]. While these techniques are in their infancy regarding BBB modulation, the non-invasive nature and advancements in targeted light delivery make them an area of keen interest.
22. Radiofrequency (RF) Modulation
RF energy, a form of electromagnetic radiation, has been explored for its potential to increase the BBB’s permeability. The concept involves using RF pulses that induce temporary and reversible changes in the BBB, facilitating drug entry [104]. Though the method holds promise, defining the precise parameters for safe and effective delivery is a significant focus of ongoing research.
23. Thermal Techniques
Devices like microwave applicators can increase BBB permeability by inducing mild hyperthermia. The technique exploits the sensitivity of BBB endothelial cells to temperature changes, allowing for a temporary “opening” of the barrier [105]. While the method is promising, ensuring precise temperature control and preventing potential thermal damage to surrounding tissues remain challenges.
These non-invasive, device-mediated techniques significantly depart from traditional methods, favoring precision, control, and safety. The advancements promise more effective drug delivery to the CNS and open avenues for delivering a broader range of therapeutic agents, including those previously deemed unsuitable due to their inability to cross the BBB [106]. As research progresses, there is optimism that these techniques will pave the way for novel treatments, offering hope to millions affected by neurological diseases.
References
- Gazzaniga, M.S.; Ivry, R.B.; Mangun, G.R. Cognitive Neuroscience: The Biology of the Mind; Norton & Company: New York, NY, USA, 2018.
- Bear, M.F.; Connors, B.W.; Paradiso, M.A. Neuroscience: Exploring the Brain; Wolters Kluwer Health: Philadelphia, PA, USA, 2016.
- Abbott, N.J. Dynamics of CNS barriers: Evolution, differentiation, and modulation. Cell. Mol. Neurobiol. 2005, 25, 5–23.
- Pardridge, W.M. The blood-brain barrier: Bottleneck in brain drug development. NeuroRx 2005, 2, 3–14.
- Daneman, R.; Prat, A. The blood–brain barrier. Cold Spring Harb. Perspect. Biol. 2015, 7, a020412.
- Abbott, N.J.; Rönnbäck, L.; Hansson, E. Astrocyte–endothelial interactions at the blood–brain barrier. Nat. Rev. Neurosci. 2006, 7, 41–53.
- Hawkins, B.T.; Davis, T.P. The blood-brain barrier/neurovascular unit in health and disease. Pharmacol. Rev. 2005, 57, 173–185.
- Islam, Y.; Leach, A.G.; Smith, J.; Pluchino, S.; Coxon, C.R.; Sivakumaran, M.; Downing, J.; Fatokun, A.A.; Teixidò, M.; Ehtezazi, T. Physiological and pathological factors affecting drug delivery to the brain by nanoparticles. Adv. Sci. 2021, 8, 2002085.
- Cho, E.E.; Drazic, J.; Ganguly, M.; Stefanovic, B.; Hynynen, K. Two-photon fluorescence microscopy study of cerebrovascular dynamics in ultrasound-induced BBB opening. J. Cereb. Blood Flow Metab. 2018, 38, 1260–1274.
- Begley, D.J. Delivery of therapeutic agents to the central nervous system: The problems and the possibilities. Pharmacol. Ther. 2004, 104, 29–45.
- Pawar, B.; Vasdev, N.; Gupta, T.; Mhatre, M.; More, A.; Anup, N.; Tekade, R.K. Current Update on Transcellular Brain Drug Delivery. Pharmaceutics 2022, 14, 2719.
- Abbott, N.J.; Patabendige, A.A.; Dolman, D.E.; Yusof, S.R.; Begley, D.J. Structure and function of the blood-brain barrier. Neurobiol. Dis. 2010, 37, 13–25.
- Anthony, D.P.; Hegde, M.; Shetty, S.S.; Rafic, T.; Mutalik, S.; Rao, B.S. Targeting receptor-ligand chemistry for drug delivery across blood-brain barrier in brain diseases. Life Sci. 2021, 274, 119326.
- Betterton, R.D.; Davis, T.P.; Ronaldson, P.T. Organic Cation Transporter (OCT/OCTN) Expression at Brain Barrier Sites: Focus on CNS Drug Delivery. Handb. Exp. Pharmacol. 2021, 266, 301–328.
- Lonser, R.R.; Sarntinoranont, M.; Morrison, P.F.; Oldfield, E.H. Convection-enhanced delivery to the central nervous system. J. Neurosurg. 2015, 122, 697–706.
- Lonser, R.R.; Walbridge, S.; Garmestani, K.; Butman, J.A.; Walters, H.A.; Vortmeyer, A.O.; Oldfield, E.H. Successful and safe perfusion of the primate brainstem: In vivo magnetic resonance imaging of macromolecular distribution during infusion. J. Neurosurg. 2002, 97, 905–913.
- Saltzman, W.M. Drug Delivery: Engineering Principles for Drug Therapy; Oxford University Press: Oxford, UK, 2001.
- Morrison, P.F.; Laske, D.W. Direct delivery of medications to the central nervous system. Clin. Pharmacokinet. 1994, 26, 85–100.
- Rubin, L.L.; Staddon, J.M. The cell biology of the blood-brain barrier. Annu. Rev. Neurosci. 1999, 22, 11–28.
- Johnsen, K.B.; Moos, T.; Burkhart, A. Receptor-mediated drug delivery to the brain in the treatment of central nervous system diseases. J. Mol. Med. 2014, 92, 497–506.
- Chen, W.; Hu, Y.; Ju, D. Gene therapy for neurodegenerative disorders: Advances, insights and prospects. Acta Pharm. Sin. B 2020, 10, 1347–1359.
- Rapoport, S.I. Osmotic opening of the blood-brain barrier: Principles, mechanism, and therapeutic applications. Cell. Mol. Neurobiol. 2000, 20, 217–230.
- Chakraborty, S.; Filippi, C.; Wong, T.; Ray, A.; Fralin, S.; Tsiouris, A.; Praminick, B.; Demopoulos, A.; McCrea, H.; Bodhinayake, I.; et al. Superselective intraarterial cerebral infusion of cetuximab after osmotic blood/brain barrier disruption for recurrent malignant glioma: Phase I study. J. Neuro-Oncol. 2016, 128, 405–415.
- Li, J.; Kataoka, K. Chemo-physical Strategies to Advance the in Vivo Functionality of Targeted Nanomedicine: The Next Generation. J. Am. Chem. Soc. 2021, 143, 538–559.
- Jiang, Y.; Wang, F.; Wang, K.; Zhong, Y.; Wei, X.; Wang, Q.; Zhang, H. Engineered Exosomes: A Promising Drug Delivery Strategy for Brain Diseases. Curr. Med. Chem. 2022, 29, 3111–3124.
- Yue, Q.; Peng, Y.; Zhao, Y.; Lu, R.; Fu, Q.; Chen, Y.; Yang, Y.; Hai, L.; Guo, L.; Wu, Y. Dual-targeting for brain-specific drug delivery: Synthesis and biological evaluation. Drug Deliv. 2018, 25, 426–434.
- Jiang, T.; Qiao, Y.; Ruan, W.; Zhang, D.; Yang, Q.; Wang, G.; Chen, Q.; Zhu, F.; Yin, J.; Zou, Y. Cation-Free siRNA Micelles as Effective Drug Delivery Platform and Potent RNAi Nanomedicines for Glioblastoma Therapy. Adv. Mater. 2021, 33, 2104779.
- Ban, J.; Li, S.; Zhan, Q.; Li, X.; Xing, H.; Chen, N.; Long, L.; Hou, X.; Zhao, J.; Yuan, X. PMPC modified PAMAM dendrimer enhances brain tumor-targeted drug delivery. Macromol. Biosci. 2021, 21, 2000392.
- Caraway, C.A.; Gaitsch, H.; Wicks, E.E.; Kalluri, A.; Kunadi, N.; Tyler, B.M. Polymeric nanoparticles in brain cancer therapy: A review of current approaches. Polymers 2022, 14, 2963.
- Saraiva, C.; Praça, C.; Ferreira, R.; Santos, T.; Ferreira, L.; Bernardino, L. Nanoparticle-mediated brain drug delivery: Overcoming blood–brain barrier to treat neurodegenerative diseases. J. Control. Release 2016, 235, 34–47.
- Wu, J.; Hernandez, Y.; Miyasaki, K.; Kwon, E. Engineered nanomaterials that exploit BBB dysfunction for delivery to the brain. Adv. Drug Deliv. Rev. 2023, 197, 114820.
- Kreuter, J. Drug delivery to the central nervous system by polymeric nanoparticles: What do we know? Adv. Drug Deliv. Rev. 2014, 71, 2–14.
- Gao, X.; Qian, J.; Zheng, S.; Changyi, Y.; Zhang, J.; Ju, S.; Zhu, J.; Li, C. Overcoming the Blood–Brain Barrier for Delivering Drugs into the Brain by Using Adenosine Receptor Nanoagonist. ACS Nano 2018, 12, 9968–9978.
- Sonavane, G.; Tomoda, K.; Makino, K. Biodistribution of colloidal gold nanoparticles after intravenous administration: Effect of particle size. Colloids Surf. B Biointerfaces 2008, 66, 274–280.
- Timbie, K.F.; Afzal, U.; Date, A.; Zhang, C.; Song, J.; Wilson Miller, G.; Suk, J.S.; Hanes, J. MR image-guided delivery of cisplatin-loaded brain-penetrating nanoparticles to invasive glioma with focused ultrasound. J. Control. Release 2017, 263, 120–131.
- Timbie, K.F.; Mead, B.P. Drug delivery across the blood-brain barrier: Recent advances in the use of nanocarriers. Nanomedicine 2017, 12, 159–167.
- Mead, B.P.; Price, R.J. Targeted drug delivery to the brain using focused ultrasound: A review. J. Drug Target. 2016, 24, 871–882.
- Pardridge, W.M. Blood-brain barrier delivery. Drug Discov. Today 2007, 12, 54–61.
- Gorick, C.; Breza, V.; Nowak, K.; Cheng, V.; Fisher, D.; Debski, A.; Hoch, M.; Demir, Z.; Tran, N.; Schwartz, M.; et al. Applications of focused ultrasound-mediated BBB opening. Adv. Drug Deliv. Rev. 2022, 191, 114583.
- Burgess, A.; Ayala-Grosso, C.; Ganguly, M.; Jordaõ, J.; Aubert, I.; Hynynen, K. Targeted delivery of neural stem cells to the brain using MRI-guided focused ultrasound to disrupt the blood-brain barrier. PLoS ONE 2011, 6, e27877.
- Diaz, R.; McVeigh, P.; O’Reilly, M.; Burrell, K.; Bebenek, M.; Smith, C.; Etame, A.; Zadeh, G.; Hynynen, K.; Wilson, B.; et al. Focused ultrasound delivery of Raman nanoparticles across the blood-brain barrier: Potential for targeting experimental brain tumors. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 1075–1087.
- Kinoshita, M.; McDannold, N.; Jolesz, F.; Hynynen, K. Noninvasive localized delivery of Herceptin to the mouse brain by MRI-guided focused ultrasound-induced BBB disruption. Proc. Natl. Acad. Sci. USA 2006, 103, 11719–11723.
- Nisbet, R.; Van der Jeugd, A.; Leinenga, G.; Evans, H.; Janowicz, P.; Götz, J. Combined effects of scanning ultrasound and a tau-specific single chain antibody in a tau transgenic mouse model. Brain J. Neurol. 2017, 140, 1220–1230.
- Raymond, S.; Treat, L.; Dewey, J.; McDannold, N.; Hynynen, K.; Bacskai, B. Ultrasound enhanced delivery of molecular imaging and therapeutic agents in Alzheimer’s disease mouse models. PLoS ONE 2008, 3, e2175.
- Th’evenot, E.; Jordão, J.; O’Reilly, M.; Markham, K.; Weng, Y.; Foust, K.; Kaspar, B.; Hynynen, K.; Aubert, I. Targeted delivery of self-complementary adeno-associated virus serotype 9 to the brain, using magnetic resonance imaging-guided focused ultrasound. Hum. Gene Ther. 2012, 23, 1144–1155.
- Pineda-Pardo, J.; Gasca-Salas, C.; Fernández-Rodríguez, B.; Rodríguez-Rojas, R.; Del Alamo, M.; Obeso, I.; Hernández-Fernández, F.; Trompeta, C.; Martínez-Fernández, R.; Matarazzo, M.; et al. Striatal BBB opening in Parkinson’s disease dementia: A pilot exploratory study. Mov. Disord. Off. J. Mov. Disord. Soc. 2022, 37, 2057–2065.
- Aryal, M.; Vykhodtseva, N.; Zhang, Y.Z.; McDannold, N. Multiple sessions of liposomal doxorubicin delivery via focused ultrasound mediated BBB disruption: A safety study. J. Control. Release 2014, 204, 60–69.
- Konofagou, E.E. Optimization of the ultrasound-induced BBB opening. Theranostics 2012, 2, 1223.
- McDannold, N.; Arvanitis, C.D.; Vykhodtseva, N.; Livingstone, M.S. Temporary disruption of the BBB by use of ultrasound and microbubbles: Safety and efficacy evaluation in rhesus macaques. Cancer Res. 2012, 72, 3652–3663.
- Liu, J.; Chu, C.; Zhang, J.; Bie, C.; Chen, L.; Aafreen, S.; Xu, J.; Kamson, D.; van Zijl, P.; Walczak, P.; et al. Label-free assessment of mannitol accumulation following osmotic BBB opening ssing chemical exchange saturation transfer magnetic resonance imaging. Pharmaceutics 2022, 14, 2529.
- Chu, C.; Jablonska, A.; Gao, Y.; Lan, X.; Lesniak, W.; Liang, Y.; Liu, G.; Li, S.; Magnus, T.; Pearl, M.; et al. Hyperosmolar BBB opening using intra-arterial injection of hyperosmotic mannitol in mice under real-time MRI guidance. Nat. Protoc. 2022, 17, 76–94.
- McDannold, N.; Vykhodtseva, N.; Hynynen, K. Targeted disruption of the BBB with focused ultrasound: Association with cavitation activity. Phys. Med. Biol. 2006, 51, 793.
- Elias, W.J.; Lipsman, N.; Ondo, W.G.; Ghanouni, P.; Kim, Y.G.; Lee, W.; Schwartz, M.; Hynynen, K.; Lozano, A.M.; Shah, B.B.; et al. A randomized trial of focused ultrasound thalamotomy for essential tremor. N. Engl. J. Med. 2016, 375, 730–739.
- Liu, H.L.; Hua, M.Y.; Chen, P.Y.; Chu, P.C.; Pan, C.H.; Yang, H.W.; Huang, C.Y.; Wang, J.J.; Yen, T.C.; Wei, K.C. Blood-brain barrier disruption with focused ultrasound enhances delivery of chemotherapeutic drugs for glioblastoma treatment. Radiology 2010, 255, 415–425.
- Mehta, R.; Carpenter, J.; Mehta, R.; Haut, M.; Ranjan, M.; Najib, U.; Lockman, P.; Wang, P.; D’haese, P.; Rezai, A. Blood-brain barrier opening with MRI-guided focused ultrasound elicits meningeal venous permeability in humans with early Alzheimer disease. Radiology 2021, 298, 654–662.
- Rezai, A.; Ranjan, M.; D’Haese, P.; Haut, M.; Carpenter, J.; Najib, U.; Mehta, R.; Chazen, J.; Zibly, Z.; Yates, J.; et al. Noninvasive hippocampal BBB opening in Alzheimer’s disease with focused ultrasound. Proc. Natl. Acad. Sci. USA 2020, 117, 9180–9182.
- Gasca-Salas, C.; Fernández-Rodríguez, B.; Pineda-Pardo, J.; Rodríguez-Rojas, R.; Obeso, I.; Hernández-Fernández, F.; Del Alamo, M.; Mata, D.; Guida, P.; Ordás-Bandera, C.; et al. Blood-brain barrier opening with focused ultrasound in Parkinson’s disease dementia. Nat. Commun. 2021, 12, 779.
- Tanizawa, K.; Sonoda, H.; Sato, Y. A phase 2/3 trial of pabinafusp alfa, IDS fused with anti-human transferrin receptor antibody, targeting neurodegeneration in MPS-II. Mol. Ther. J. Am. Soc. Gene Ther. 2021, 29, 671–679.
- Cuccurazzu, B.; Leone, L. Exposure to extremely low-frequency (50 Hz) electromagnetic fields enhances adult hippocampal neurogenesis in C57BL/6 mice. Exp. Neurol. 2014, 261, 328–335.
- Hjouj, M.; Last, D. MRI study on reversible and irreversible electroporation induced BBB disruption. PLoS ONE 2012, 7, e42817.
- Cichoń, N.; Bijak, M.; Miller, E.; Saluk, J. The influence of electromagnetic fields on the pharmacokinetics of drugs in the brain: Current state of knowledge and directions for the future. Cent. Eur. J. Immunol. 2017, 42, 407–413.
- Simpson, R.; Phillis, J. Adenosine in exercise adaptation. Br. J. Sports Med. 1992, 26, 54–58.
- Marcos-Contreras, O.; Martinez de Lizarrondo, S.; Bardou, I.; Orset, C.; Pruvost, M.; Anfray, A.; Frigout, Y.; Hommet, Y.; Lebouvier, L.; Montaner, J.; et al. Hyperfibrinolysis increases BBB permeability by a plasmin- and bradykinin-dependent mechanism. Blood 2016, 128, 2423–2434.
- Xie, Z.; Shen, Q.; Xie, C.; Lu, W.; Peng, C.; Wei, X.; Li, X.; Su, B.; Gao, C.; Liu, M. Retro-inverso bradykinin opens the door of blood-brain tumor barrier for nanocarriers in glioma treatment. Cancer Lett. 2015, 369, 144–151.
- Rodríguez-Masso’, S.; Erickson, M.; Banks, W.; Ulrich, H.; Martins, A. The bradykinin B2 receptor agonist (NG291) causes rapid onset of transient BBB disruption without evidence of early brain injury. Front. Neurosci. 2021, 15, 791709.
- Domer, F.; Boertje, S.; Bing, E.; Reddix, I. Histamine- and acetylcholine-induced changes in the permeability of the BBB of normotensive and spontaneously hypertensive rats. Neuropharmacology 1983, 22, 615–619.
- Schilling, L.; Wahl, M. Opening of the BBB during cortical superfusion with histamine. Brain Res. 1994, 653, 289–296.
- Zhang, H.; Chen, Y.; Wang, Z.; Xie, G.; Liu, M.; Yuan, B.; Chai, H.; Wang, W.; Cheng, P. Implications of Gut Microbiota in Neurodegenerative Diseases. Front. Immunol. 2022, 13, 785644.
- Sherwin, E.; Bordenstein, S.R.; Quinn, J.L.; Dinan, T.G.; Cryan, J.F. Microbiota and the Social Brain. Science 2019, 366, 6465.
- Needham, B.D.; Kaddurah-Daouk, R.; Mazmanian, S.K. Gut Microbial Molecules in Behavioural and Neurodegenerative Conditions. Nat. Rev. Neurosci. 2020, 21, 717–731.
- Banks, W.A. The Blood–Brain Barrier as an Endocrine Tissue. Nat. Rev. Endocrinol. 2019, 15, 444–455.
- Sellge, G.; Kufer, T.A. PRR-Signaling Pathways: Learning from Microbial Tactics. Semin. Immunol. 2015, 27, 75–84.
- Harrington, M. For Lack of Gut Microbes, the Blood-Brain Barrier ‘Leaks’. Lab. Anim. 2015, 44, 6–7.
- Braniste, V.; Al-Asmakh, M.; Kowal, C.; Anuar, F.; Abbaspour, A.; Tóth, M.; Korecka, A.; Bakocevic, N.; Ng, L.G.; Kundu, P.; et al. The gut microbiota influences blood-brain barrier permeability in mice. Sci. Transl. Med. 2014, 6, 263ra158, Erratum in Sci. Transl. Med. 2014, 6, 266er7.
- Aho, V.T.E.; Houser, M.C.; Pereira, P.A.B.; Chang, J.; Rudi, K.; Paulin, L.; Hertzberg, V.; Auvinen, P.; Tansey, M.G.; Scheperjans, F. Relationships of gut microbiota, short-chain fatty acids, inflammation, and the gut barrier in Parkinson’s disease. Mol. Neurodegener. 2021, 16, 6.
- Available online: https://www.alz.org/media/documents/alzheimers-facts-and-figures.pdf (accessed on 10 July 2023).
- Available online: https://www.parkinson.org/understanding-parkinsons/statistics (accessed on 10 July 2023).
- Smith, P.M.; Howitt, M.R.; Panikov, N.; Michaud, M.; Gallini, C.A.; Bohlooly-Y, M.; Glickman, J.N.; Garrett, W.S. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 2013, 341, 569–573.
- Honda, K.; Littman, D.R. The Microbiota in Adaptive Immune Homeostasis and Disease. Nature 2016, 535, 75–84.
- Sun, M.; He, C.; Cong, Y.; Liu, Z. Regulatory Immune Cells in Regulation of Intestinal Inflammatory Response to Microbiota. Mucosal Immunol. 2015, 8, 969–978.
- Huang, F.; Wu, X. Brain Neurotransmitter Modulation by Gut Microbiota in Anxiety and Depression. Front. Cell Dev. Biol. 2021, 9, 649103.
- Terstappen, G.; Meyer, A.; Bell, R.; Zhang, W. Strategies for delivering therapeutics across the blood-brain barrier. Nat. Rev. Drug Discov. 2021, 20, 362–383.
- Gao, X.; Xu, J.; Yao, T.; Liu, X.; Zhang, H.; Zhan, C. Peptide-decorated nanocarriers penetrating the BBB for imaging and therapy of brain diseases. Adv. Drug Deliv. Rev. 2022, 187, 114362.
- Zhu, Z.; Zhai, Y.; Hao, Y.; Wang, Q.; Han, F.; Zheng, W.; Hong, J.; Cui, L.; Jin, W.; Ma, S.; et al. Specific anti-glioma targeted-delivery strategy of engineered small extracellular vesicles dual-functionalised by Angiopep-2 and TAT peptides. J. Extracell. Vesicles 2022, 11, e12255.
- Reynolds, J.; Mahajan, S. Transmigration of tetraspanin 2 (Tspan2) siRNA via microglia derived exosomes across the blood brain barrier modifies the production of immune mediators by microglia cells. J. NeuroImmune Pharmacol. Off. J. Soc. NeuroImmune Pharmacol. 2020, 15, 554–563.
- Ma, F.; Yang, L.; Sun, Z.; Chen, J.; Rui, X.; Glass, Z.; Xu, Q. Neurotransmitter-derived lipidoids (NT-lipidoids) for enhanced brain delivery through intravenous injection. Sci. Adv. 2020, 6, eabb4429.
- Fenno, L.; Yizhar, O.; Deisseroth, K. The development and application of optogenetics. Annu. Rev. Neurosci. 2011, 34, 389–412.
- Gradinaru, V.; Mogri, M.; Thompson, K.R.; Henderson, J.M.; Deisseroth, K. Optical deconstruction of parkinsonian neural circuitry. Science 2009, 324, 354–359.
- McDannold, N.; Maier, S.E. Magnetic resonance acoustic radiation force imaging. Med. Phys. 2015, 42, 4838–4846.
- Zhu, L.; Wang, L.V. Photoacoustic tomography: Applications and advances. Photons Plus Ultrasound Imaging Sens. 2013, 8581, 85810V.
- Zlokovic, B.V. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 2008, 57, 178–201.
- Pardridge, W.M. Receptor mediated peptide transport through the blood-brain barrier. Endocr. Metab. Immune Disord.-Drug Targets 2016, 16, 182–187.
- Spencer, B.J.; Verma, I.M. Targeted delivery of proteins across the blood-brain barrier. Proc. Natl. Acad. Sci. USA 2007, 104, 7594–7599.
- Zhang, B.; Sun, X.; Mei, H.; Wang, Y.; Liao, Z.; Chen, J.; Zhang, Q. LDLR-mediated peptide-22-conjugated nanoparticles for dual-targeting therapy of brain glioma. Biomaterials 2019, 217, 119264.
- Yu, Y.J.; Zhang, Y.; Kenrick, M.; Hoyte, K.; Luk, W.; Lu, Y.; Atwal, J.; Elliott, J.M.; Prabhu, S.; Watts, R.J.; et al. Boosting brain uptake of a therapeutic antibody by reducing its affinity for a transcytosis target. Sci. Transl. Med. 2011, 3, 84ra44.
- Niewoehner, J.; Bohrmann, B.; Collin, L.; Urich, E.; Sade, H.; Maier, P.; Neumann, U. Increased brain penetration and potency of a therapeutic antibody using a monovalent molecular shuttle. Neuron 2014, 81, 49–60.
- Couch, J.A.; Yu, Y.J.; Zhang, Y. The blood-brain barrier and beyond: Strategies for advancing brain drug delivery. Drug Discov. Today Technol. 2017, 25, 63–71.
- Haney, M.; Klyachko, N.; Zhao, Y.; Gupta, R.; Plotnikova, E.; He, Z.; Patel, T.; Piroyan, A.; Sokolsky, M.; Kabanov, A.; et al. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J. Control. Release Off. J. Control. Release Soc. 2015, 207, 18–30.
- Wang, J.; Shi, Y.; Yu, S.; Wang, Y.; Meng, Q.; Liang, G.; Eckenhoff, M.; Wei, H. Intranasal administration of dantrolene increased brain concentration and duration. PLoS ONE 2020, 15, e0229156.
- Qweider, M.; Gilsbach, J.; Rohde, V. Inadvertent intrathecal vincristine administration: A neurosurgical emergency. Case Rep. J. Neurosurg. Spine 2007, 6, 280–283.
- Nassan, M.; Videnovic, A. Circadian rhythms in neurodegenerative disorders. Nat. Rev. Neurol. 2022, 18, 7–24.
- Zhang, S.; Yue, Z.; Arnold, D.; Artiushin, G.; Sehgal, A. A circadian clock in the BBB regulates xenobiotic efflux. Cell 2018, 173, 130–139.
- Deisseroth, K. Optogenetics. Nat. Methods 2011, 8, 26–29.
- Moriyama, Y.; Nguyen, J. Rapid initiation of guided focused ultrasound-induced BBB disruption using radiofrequency. Ultrasonics 2009, 49, 566–573.
- Dromi, S.; Frenkel, V.; Luk, A.; Traughber, B.; Angstadt, M.; Bur, M.; Wood, B.J. Pulsed-high intensity focused ultrasound and low temperature–sensitive liposomes for enhanced targeted drug delivery and antitumor effect. Clin. Cancer Res. 2007, 13, 2722–2727.
- Poon, C.; McMahon, D.; Hynynen, K. Noninvasive and targeted drug delivery to the brain using focused ultrasound. ACS Chem. Neurosci. 2017, 8, 16–26.
More
Information
Subjects:
Physiology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
829
Revisions:
2 times
(View History)
Update Date:
27 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




