Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Yiqun Tang | -- | 1687 | 2023-11-09 11:36:01 | | | |
| 2 | Lindsay Dong | -2 word(s) | 1685 | 2023-11-13 02:13:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Tang, Y.; Frisendahl, C.; Lalitkumar, P.G.; Gemzell-Danielsson, K. Experimental Therapeutic Strategies for Thin Endometrium. Encyclopedia. Available online: https://encyclopedia.pub/entry/51354 (accessed on 07 February 2026).
Tang Y, Frisendahl C, Lalitkumar PG, Gemzell-Danielsson K. Experimental Therapeutic Strategies for Thin Endometrium. Encyclopedia. Available at: https://encyclopedia.pub/entry/51354. Accessed February 07, 2026.
Tang, Yiqun, Caroline Frisendahl, Parameswaran Grace Lalitkumar, Kristina Gemzell-Danielsson. "Experimental Therapeutic Strategies for Thin Endometrium" Encyclopedia, https://encyclopedia.pub/entry/51354 (accessed February 07, 2026).
Tang, Y., Frisendahl, C., Lalitkumar, P.G., & Gemzell-Danielsson, K. (2023, November 09). Experimental Therapeutic Strategies for Thin Endometrium. In Encyclopedia. https://encyclopedia.pub/entry/51354
Tang, Yiqun, et al. "Experimental Therapeutic Strategies for Thin Endometrium." Encyclopedia. Web. 09 November, 2023.
Copy Citation
Infertility caused by a thin endometrium remains a significant challenge in assisted reproduction and is often associated with a low success rate after treatment with assisted reproductive technology. There is a lack of consensus in the field concerning both its diagnostic criteria and clinical management. The available treatment options are few with limited efficacy. Advances in cell therapy and bioengineering have, however, shown promising results for the treatment of a thin endometrium. Notably, these novel interventions have demonstrated the ability to increase endometrial thickness, restore endometrial function, and improve reproductive outcomes.
infertility
thin endometrium
platelet-rich plasma
stem cell therapy
bioengineering
1. Introduction
Infertility caused by a thin endometrium represents a challenging condition to treat and is frequently associated with a low success rate and impaired reproductive outcomes using assisted reproductive technologies (ART) [1][2]. An endometrial thickness (EMT) of at least 7 mm is generally regarded as more suitable for successful embryo implantation in an ART program [3]. There is, however, no consensus on the threshold of EMT that should be applied for the diagnosis of a thin endometrium [4][5][6]. The etiology of thin endometria is complex, diverse, and often unknown (Figure 1), making it challenging to treat these patients and to study the underlying pathological mechanisms. Proposed causes of a thin endometrium include Asherman’s syndrome and previous intrauterine surgery including sharp curettage, radiation to the pelvis, genetics, impaired uterine blood flow, and acute or chronic endometrial infection. Moreover, it is linked to the use of medications such as clomiphene citrate as well as low estrogen levels or impaired estrogen signaling as a result of dysfunctional estrogen receptors [7][8][9][10][11]. A recent single-cell RNA sequencing study suggested that cellular senescence in the stroma and epithelium together with collagen overdeposition around the blood vessel is involved in endometrial thinness [12]. Furthermore, results from a cumulative in silico study that included five RNA sequencing datasets on a thin endometrium revealed dysfunctional intercellular communication and metabolic signaling pathways in the thin endometrium [13].
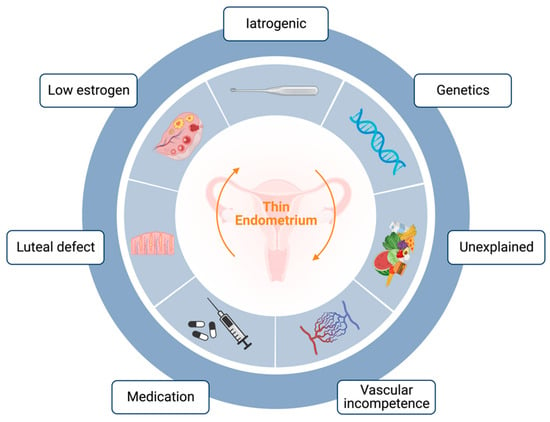
Figure 1. Schematic image of representative etiologies of thin endometrium (created using Biorender).
Conventional therapies, including estradiol or combined hormonal therapy [14], growth hormone [15], Granulocyte colony-stimulating factor (G-CSF) [16][17], sildenafil citrate [18], and several vasoactive substances [19] such as aspirin, pentoxifylline, tocopherol, and L-Arginine have shown limited and inconsistent efficacy regarding an increase in EMT increase and restoration of endometrial function [20][21]. Consequently, there is a growing demand for novel adjuvant therapies. In recent years, cell-based therapy and other innovative treatment options have emerged as promising strategies in various medical fields [22][23][24]. Considering the encouraging results in numerous experimental studies, these novel approaches may hold great potential as treatment options for thin endometria.
2. Experimental Therapeutic Strategies
2.1. Platelet-Rich Plasma
Platelet-rich plasma (PRP) is an autologous plasma-based concentration of platelets, offering a host of therapeutic advantages [25]. Its autologous nature significantly reduces the risk of immune rejection, pathogen transmission, and cancer development, making it an attractive treatment option [26][27][28]. Rich in growth factors (GFs) and cytokines, PRP has demonstrated pro-regenerative properties, particularly in healing injured tissues. Recently, there has been growing interest in its potential for treating endometrial disorders, such as thin endometria [29].
In 2018, Molina et al. [30] administrated PRP through intrauterine infusions to 19 patients with refractory thin endometria undergoing IVF. After the second PRP injection, the endometrial thickness in each patient exceeded 9 mm. Notably, this resulted in an impressive 73.7% positive pregnancy test rate and 26.2% live births. Later in the same year, the first randomized controlled trial [31] reported significantly higher rates of implantation and clinical pregnancy rates in the PRP group (27.94% vs. 11.67%; 44.12% vs. 20%; p < 0.05, respectively), along with improved endometrial thickness (p = 0.001). Subsequently, an increasing number of prospective clinical studies [32][33][34][35][36][37][38] further support these findings, showing that intrauterine infusion of PRP effectively thickened the endometrial lining and improved clinical pregnancy outcomes to different extents. Although growing evidence indicates that PRP treatment is beneficial for treating thin endometria, the positive effects only manifest for certain parameters.
2.2. Stem Cell Therapy
During the last decades, stem cell therapy has rapidly evolved and been applied in the treatment of various diseases. Stem cells possess unique characteristics, such as high self-renewal capacity and the ability to differentiate into multiple cell types. Stem cell therapy has emerged as a promising frontier in reproductive medicine giving its potential to restore endometrial function for patients with a thin endometrium [39][40].
2.2.1. BMDSCs
Bone-marrow-derived stem cells (BMDSCs) are multipotent stem cells that can differentiate into different functional cells. Due to their easy acquisition in adult bone marrow, these cells have emerged as an important candidate for stem cell therapy in various diseases [41][42][43]. In 2011, Nagori et al. [44] reported a successful pregnancy in a patient with refractory intrauterine adhesions through the autologous transplantation of BMDSCs. Later in 2013, Zhao et al. [45] transplanted autologous BMDSCs into the uterine cavity under ultrasound guidance in a woman with severe intrauterine adhesions, resulting in a spontaneous pregnancy after three months. Moreover, Singh et al. reported that autologous transplantation of BMDSCs significantly increased endometrial thickness at 3, 6, and 9 months compared to pre-treatment thickness in six patients with refractory intrauterine adhesions. Menstruation was also restored in five out of six patients [46].
2.2.2. ADSCs
Adipose-derived stem cells (ADSCs) are another abundant and easily accessible stem cell source that are available in large quantities and have the benefit of allowing for isolation and production using a minimally invasive lipectomy procedure [47]. These cells have been tested in repairing injured endometrium in a few clinical trials. In 2019, one study [48] recruited 25 women with thin endometria (EMT < 5 mm) who had embryo implantation failure at least three times. After subendometrial injection of ADSCs, the EMT increased in 80% (20/25) of patients, leading to 13 pregnancies and 9 healthy live births. Another pilot study in 2020 [49] examined the effectiveness of restoring functional endometrium in patients with severe Asherman’s syndrome (intrauterine adhesions) using autologous adipose-derived stromal vascular fraction (AD-SVF) containing adipose stem cells (ASCs). Five out of six infertile women with severe intrauterine adhesions achieved increased endometrial thickness along with an increased volume of menstrual bleeding. One of the five women who underwent ART treatment and transferred an embryo became pregnant but spontaneously miscarried at nine weeks.
2.2.3. UCMSCs
In contrast to other stem cell sources, umbilical cord mesenchymal stem cells (UCMSCs) stand out as a highly promising cell source for cell therapy due to their abundance, non-controversial nature, painless collection procedure, and rapid self-renewal properties [50]. Particularly noteworthy is the fact that UCMSCs exhibit negligible or undetectable HLA class I expression, indicating the potential for allograft transplantation without the need for immunosuppression [51]. This unique characteristic enhances the appeal of UCMSCs as a viable option for therapeutic applications. In 2018, a phase I clinical trial implanted UCMSCs in biodegradable collagen scaffolds into the uterine cavity of 26 patients with recurrent intrauterine adhesions, resulting in an increase in EMT in all cases from 4.46 ± 0.85 to 5.74 ± 1.2 mm (p < 0.01), which is linked to pregnancy in 10 women (38%), 8 of whose pregnancies resulted in live births [52].
2.2.4. Other Stem Cell Sources
Several other sources of stem cells have also been introduced and emerged as potential sources for the treatment of thin endometrium. One such source is menstrual-blood-derived stromal cells (MenSCs), which comprise a mixed population of mesenchymal stem cells and stromal fibroblasts. In 2016, Tan et al. [53] transplanted autologous MenSCs from the menstrual blood of women with intrauterine adhesions back into the uterine cavity. A significant increase in endometrial thickness to 7 mm in five out of seven cases was observed along with successful pregnancies in two out of four women. However, this source of stem cells has certain limitations such as not being applicable for those patients with hypomenorrhea. To explore the endometrial repair mechanism of transplanted MenSCs, one study [54] demonstrated that MenSCs could increase the microvascular density (MVD) of an injured endometrium in a mouse model by activating the ART and ERK pathways; inducing the upregulation of eNOS, VEGFA, VEGFR1, VEGFR2, and Tie2; and promoting cell proliferation, migration, and angiogenesis in vitro. Additionally, uterine-derived cells have been successfully transplanted in a rat model to repair damaged uterine endometrium, leading to promising outcomes [55]. Through transplantation of endometrium-like cells derived from human embryonic stem cell lines (hESCs), researchers demonstrated that these cells could significantly restore the structure and functionality of severely damaged uterine horns in a rat model [56]. Though most of these studies are at a pre-clinical stage, these promising results have encouraged researchers to develop cell-based biomedical approaches for repairing damaged endometria.
2.2.5. Stem-Cell-Derived Extracellular Vesicles
Stem cells possess the ability to secrete a wide range of regenerative cytokines, and these cellular secretions have been proposed to contribute to the positive therapeutic effects observed in different diseases [57][58][59]. Extracellular vesicles (EVs) are an important component of these secretions that have cytoprotective, antiapoptotic, and angiogenic effects on injured tissues and can promote progenitor and stem cell homing [60]. Building on this idea, researchers are aiming to develop stem-cell-derived exosome-based therapy that focuses on the EVs that the cells secrete, including exosomes. While the clinical research on EVs is still in an early stage, the results from animal studies are encouraging and highlight the potential of EV-based therapies for thin endometria. In 2020, exosomes derived from adipose mesenchymal stem cells were discovered to be able to preserve normal uterine structure, stimulate endometrial regeneration, support collagen remodeling, and elevate the expression of endometrial receptivity markers including integrin β3, LIF, and VEGF [61].
2.3. Tissue Bioengineering
Bioengineering approaches have demonstrated promising outcomes in the field of regenerative medicine over recent years. Various biomedical materials and techniques, such as collagen scaffolds, decellularized scaffolds, hydrogels, and microfluidics, have been employed to facilitate tissue repair and regeneration [62][63]. The rapid advancement of biomaterials has also enabled new possibilities for therapeutic strategies in thin endometria. Hydrogels, nanostructured delivery systems, bioactive degradable scaffolds, and other innovations have emerged as promising tools to enhance the survival and function of stem cells [64][65]. In 2021, one study [66] investigated the effects of transplanting UCMSCs, seeded on a human acellular amniotic matrix (AAM), to an endometrial injured site in a rat model. The results showed that endometrial thickness significantly increased, and the expression of vimentin, cytokeratin, and integrin β3 were higher in treated rats compared to untreated rats. The UCMSC–AAM combination might potentiate the endometrial repair effect of UCMSCs. The extracellular matrix is indeed an important component in tissue remodeling. Hydrogel, a highly hydrated collagen-based material, has shown great benefits in facilitating constructive and functional tissue remodeling [67].
References
- Liao, Z.; Liu, C.; Cai, L.; Shen, L.; Sui, C.; Zhang, H.; Qian, K. The Effect of Endometrial Thickness on Pregnancy, Maternal, and Perinatal Outcomes of Women in Fresh Cycles after IVF/ICSI: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2022, 12, 814648.
- Liu, K.E.; Hartman, M.; Hartman, A.; Luo, Z.C.; Mahutte, N. The Impact of a Thin Endometrial Lining on Fresh and Frozen-Thaw IVF Outcomes: An Analysis of over 40,000 Embryo Transfers. Hum. Reprod. 2018, 33, 1883–1888.
- Eftekhar, M.; Tabibnejad, N.; Tabatabaie, A.A. The Thin Endometrium in Assisted Reproductive Technology: An Ongoing Challenge. Middle East Fertil. Soc. J. 2018, 23, 1–7.
- Jacobs, E.A.; Van Voorhis, B.; Kawwass, J.F.; Kondapalli, L.A.; Liu, K.; Dokras, A. Endometrial Thickness: How Thin Is Too Thin? Fertil. Steril. 2022, 118, 249–259.
- Buyalos, R.P.; Hubert, G.D.; Shamonki, M.I. The Mystery of Optimal Endometrial Thickness…never Too Thick, but When Is Thin…too Thin? Fertil. Steril. 2022, 117, 801–802.
- El-Toukhy, T.; Coomarasamy, A.; Khairy, M.; Sunkara, K.; Seed, P.; Khalaf, Y.; Braude, P. The Relationship between Endometrial Thickness and Outcome of Medicated Frozen Embryo Replacement Cycles. Fertil. Steril. 2008, 89, 832–839.
- Yuan, R.; Le, A.W. A Study on the Estrogen Receptor α Gene Polymorphism and Its Expression in Thin Endometrium of Unknown Etiology. Gynecol. Obstet. Investig. 2012, 74, 13–20.
- Le, A.W.; Wang, Z.H.; Yuan, R.; Shan, L.L.; Xiao, T.H.; Zhuo, R.; Shen, Y. Association of the Estrogen Receptor-β Gene RsaI and AluI Polymorphisms with Human Idiopathic Thin Endometrium. Genet. Mol. Res. 2013, 12, 5978–5985.
- Talukdar, N.; Bentov, Y.; Chang, P.T.; Esfandiari, N.; Nazemian, Z.; Casper, R.F. Effect of Long-Term Combined Oral Contraceptive Pill Use on Endometrial Thickness. Obstet. Gynecol. 2012, 120, 348–354.
- Gonen, Y.; Casper, R.F. Sonographic Determination of a Possible Adverse Effect of Clomiphene Citrate on Endometrial Growth. Hum. Reprod. 1990, 5, 670–674.
- Casper, R.F. It’s Time to Pay Attention to the Endometrium. Fertil. Steril. 2011, 96, 519–521.
- Lv, H.; Zhao, G.; Jiang, P.; Wang, H.; Wang, Z.; Yao, S.; Zhou, Z.; Wang, L.; Liu, D.; Deng, W.; et al. Deciphering the Endometrial Niche of Human Thin Endometrium at Single-Cell Resolution. Proc. Natl. Acad. Sci. USA 2022, 119, e2115912119.
- Xu, L.; Fan, Y.; Wang, J.; Shi, R. Dysfunctional intercellular communication and metabolic signaling pathways in thin endometrium. Front. Physiol. 2022, 13, 1050690.
- Vartanyan, E.; Tsaturova, K.; Devyatova, E. Thin endometrium problem in IVF programs. Gynecol. Endocrinol. 2020, 36, 24–27.
- Shang, Y.; Wu, M.; He, R.; Ye, Y.; Sun, X. Administration of growth hormone improves endometrial function in women undergoing in vitro fertilization: A systematic review and meta-analysis. Hum. Reprod. Update 2022, 28, 838–857.
- Fu, L.L.; Xu, Y.; Yan, J.; Zhang, X.Y.; Li, D.D.; Zheng, L.W. Efficacy of granulocyte colony-stimulating factor for infertility undergoing IVF: A systematic review and meta-analysis. Reprod. Biol. Endocrinol. 2023, 21, 34.
- Zhang, Y.; Chen, X.; Chen, S.; Wei, C.; Li, B.; Wang, Z.; Shen, X.; Lin, X. Intrauterine administration of G-CSF for promoting endometrial growth after hysteroscopic adhesiolysis: A randomized controlled trial. Hum. Reprod. 2022, 37, 725–733.
- Li, X.; Luan, T.; Zhao, C.; Zhang, M.; Dong, L.; Su, Y.; Ling, X. Effect of sildenafil citrate on treatment of infertility in women with a thin endometrium: A systematic review and meta-analysis. J. Int. Med. Res. 2020, 48, 300060520969584.
- Ranisavljevic, N.; Raad, J.; Anahory, T.; Grynberg, M.; Sonigo, C. Embryo transfer strategy and therapeutic options in infertile patients with thin endometrium: A systematic review. J. Assist. Reprod. Genet. 2019, 36, 2217–2231.
- Liu, K.E.; Hartman, M.; Hartman, A. Management of Thin Endometrium in Assisted Reproduction: A Clinical Practice Guideline from the Canadian Fertility and Andrology Society. Reprod. Biomed. Online 2019, 39, 49–62.
- Lebovitz, O.; Orvieto, R. REVIEW—Treating Patients with “Thin” Endometrium-an Ongoing Challenge. Gynecol. Endocrinol. 2014, 30, 409–414.
- Gharibeh, N.; Aghebati-Maleki, L.; Madani, J.; Pourakbari, R.; Yousefi, M.; Ahmadian Heris, J. Cell-Based Therapy in Thin Endometrium and Asherman Syndrome. Stem Cell Res. Ther. 2022, 13, 1–13.
- Zhang, L.; Ma, X.J.N.; Fei, Y.Y.; Han, H.T.; Xu, J.; Cheng, L.; Li, X. Stem Cell Therapy in Liver Regeneration: Focus on Mesenchymal Stem Cells and Induced Pluripotent Stem Cells. Pharmacol. Ther. 2022, 232, 108004.
- Konen, F.F.; Schwenkenbecher, P.; Jendretzky, K.F.; Gingele, S.; Grote-Levi, L.; Möhn, N.; Sühs, K.W.; Eiz-Vesper, B.; Maecker-Kolhoff, B.; Trebst, C.; et al. Stem Cell Therapy in Neuroimmunological Diseases and Its Potential Neuroimmunological Complications. Cells 2022, 11, 2165.
- Wu, P.I.-K.; Diaz, R.; Borg-Stein, J. Platelet-Rich Plasma. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 825–853.
- Bos-Mikich, A.; de Oliveira, R.; Frantz, N. Platelet-Rich Plasma Therapy and Reproductive Medicine. J. Assist. Reprod. Genet. 2018, 35, 753–756.
- Sharara, F.I.; Lelea, L.-L.L.; Rahman, S.; Klebanoff, J.S.; Moawad, G.N. Review- A Narrative Review of Platelet-Rich Plasma (PRP) in Reproductive Medicine. J. Assist. Reprod. Genet. 2021, 38, 1003–1012.
- Varghese, J.; Acharya, N. Platelet-Rich Plasma: A Promising Regenerative Therapy in Gynecological Disorders. Cureus 2022, 14, e28998.
- Kim, M.K.; Song, H.; Lyu, S.W.; Lee, W.S. Platelet-Rich Plasma Treatment in Patients with Refractory Thin Endometrium and Recurrent Implantation Failure: A Comprehensive Review. Clin. Exp. Reprod. Med. 2022, 49, 168–174.
- Molina, A.M.; Sánchez, J.; Sánchez, W.; Vielma, V. Platelet-Rich Plasma as an Adjuvant in the Endometrial Preparation of Patients with Refractory Endometrium. JBRA Assist. Reprod. 2018, 22, 42–48.
- Eftekhar, M.; Neghab, N.; Naghshineh, E.; Khani, P. Can Autologous Platelet Rich Plasma Expand Endometrial Thickness and Improve Pregnancy Rate during Frozen-Thawed Embryo Transfer Cycle? A Randomized Clinical Trial. Taiwan J. Obstet. Gynecol. 2018, 57, 810–813.
- Chang, Y.; Li, J.; Wei, L.-N.N.; Pang, J.; Chen, J.; Liang, X. Autologous Platelet-Rich Plasma Infusion Improves Clinical Pregnancy Rate in Frozen Embryo Transfer Cycles for Women with Thin Endometrium. Medicine 2019, 98, e14062.
- Kim, H.; Shin, J.E.; Koo, H.S.; Kwon, H.; Choi, D.H.; Kim, J.H. Effect of Autologous Platelet-Rich Plasma Treatment on Refractory Thin Endometrium During the Frozen Embryo Transfer Cycle: A Pilot Study. Front. Endocrinol. 2019, 10, 61.
- Kusumi, M.; Ihana, T.; Kurosawa, T.; Ohashi, Y.; Tsutsumi, O. Intrauterine Administration of Platelet-Rich Plasma Improves Embryo Implantation by Increasing the Endometrial Thickness in Women with Repeated Implantation Failure: A Single-Arm Self-Controlled Trial. Reprod. Med. Biol. 2020, 19, 350–356.
- Russell, S.J.; Kwok, Y.S.S.; Nguyen, T.T.T.N.; Librach, C. Autologous Platelet-Rich Plasma Improves the Endometrial Thickness and Live Birth Rate in Patients with Recurrent Implantation Failure and Thin Endometrium. J. Assist. Reprod. Genet. 2022, 39, 1305–1312.
- Agarwal, M.; Mettler, L.; Jain, S.; Meshram, S.; Günther, V.; Alkatout, I. Management of a Thin Endometrium by Hysteroscopic Instillation of Platelet-Rich Plasma Into The Endomyometrial Junction: A Pilot Study. J. Clin. Med. 2020, 9, 2795.
- Dogra, Y.; Singh, N.; Vanamail, P. Autologous Platelet-Rich Plasma Optimizes Endometrial Thickness and Pregnancy Outcomes in Women with Refractory Thin Endometrium of Varied Aetiology during Fresh and Frozen-Thawed Embryo Transfer Cycles. JBRA Assist. Reprod. 2022, 26, 13–21.
- Gangaraju, B.; Mahajan, P.; Subramanian, S.; Kulkarni, A.; Mahajan, S. Lyophilized Platelet–Rich Plasma for the Management of Thin Endometrium and Facilitation of in-Vitro Fertilization. JBRA Assist. Reprod. 2022, 27, 55–59.
- Mouhayar, Y.; Sharara, F.I. G-CSF and Stem Cell Therapy for the Treatment of Refractory Thin Lining in Assisted Reproductive Technology. J. Assist. Reprod. Genet. 2017, 34, 831–837.
- Keyhanvar, N.; Zarghami, N.; Bleisinger, N.; Hajipour, H.; Fattahi, A.; Nouri, M.; Dittrich, R. Cell-Based Endometrial Regeneration: Current Status and Future Perspectives. Cell Tissue Res. 2021, 1, 3.
- Huang, L.Y.; Sun, X.; Pan, H.X.; Wang, L.; He, C.Q.; Wei, Q. Cell Transplantation Therapies for Spinal Cord Injury Focusing on Bone Marrow Mesenchymal Stem Cells: Advances and Challenges. World J. Stem Cells 2023, 15, 385–399.
- Arshad, M.; Jalil, F.; Jaleel, H.; Ghafoor, F. Bone Marrow Derived Mesenchymal Stem Cells Therapy for Rheumatoid Arthritis—A Concise Review of Past Ten Years. Mol. Biol. Rep. 2023, 50, 4619–4629.
- Kim, S.G.; George, N.P.; Hwang, J.S.; Park, S.; Kim, M.O.; Lee, S.H.; Lee, G. Human Bone Marrow-Derived Mesenchymal Stem Cell Applications in Neurodegenerative Disease Treatment and Integrated Omics Analysis for Successful Stem Cell Therapy. Bioengineering 2023, 10, 621.
- Nagori, C.; Panchal, S.; Patel, H. Endometrial Regeneration Using Autologous Adult Stem Cells Followed by Conception by in Vitro Fertilization in a Patient of Severe Ashermans Syndrome. J. Hum. Reprod. Sci. 2011, 4, 43–48.
- Zhao, Y.; Wang, A.; Tang, X.; Li, M.; Yan, L.; Shang, W.; Gao, M.; Zhao, Y.; Wang, A.; Tang, X.; et al. Intrauterine Transplantation of Autologous Bone Marrow Derived Mesenchymal Stem Cells Followed by Conception in a Patient of Severe Intrauterine Adhesions. Open J. Obstet. Gynecol. 2013, 3, 377–380.
- Singh, N.; Mohanty, S.; Seth, T.; Shankar, M.; Bhaskaran, S.; Dharmendra, S. Autologous Stem Cell Transplantation in Refractory Asherman’s Syndrome: A Novel Cell Based Therapy. J. Hum. Reprod. Sci. 2014, 7, 93–98.
- Mazini, L.; Rochette, L.; Amine, M.; Malka, G. Regenerative Capacity of Adipose Derived Stem Cells (ADSCs), Comparison with Mesenchymal Stem Cells (MSCs). Int. J. Mol. Sci. 2019, 20, 2523.
- Sudoma, I.; Pylyp, L.; Kremenska, Y.; Goncharova, Y. Application of Autologous Adipose-Derived Stem Cells for Thin Endometrium Treatment in Patients with Failed ART Programs. J. Stem Cell Ther. Transplant. 2019, 3, 001–008.
- Lee, S.Y.; Shin, J.E.; Kwon, H.; Choi, D.H.; Kim, J.H. Effect of Autologous Adipose-Derived Stromal Vascular Fraction Transplantation on Endometrial Regeneration in Patients of Asherman’s Syndrome: A Pilot Study. Reprod. Sci. 2020, 27, 561–568.
- Nagamura-Inoue, T.; He, H. Umbilical Cord-Derived Mesenchymal Stem Cells: Their Advantages and Potential Clinical Utility. World J. Stem Cells 2014, 6, 195.
- Christodoulou, I.; Goulielmaki, M.; Devetzi, M.; Panagiotidis, M.; Koliakos, G.; Zoumpourlis, V. Mesenchymal Stem Cells in Preclinical Cancer Cytotherapy: A Systematic Review. Stem Cell Res. Ther. 2018, 9, 1–38.
- Cao, Y.; Sun, H.; Zhu, H.; Zhu, X.; Tang, X.; Yan, G.; Wang, J.; Bai, D.; Wang, J.; Wang, L.; et al. Allogeneic Cell Therapy Using Umbilical Cord MSCs on Collagen Scaffolds for Patients with Recurrent Uterine Adhesion: A Phase I Clinical Trial. Stem Cell Res. Ther. 2018, 9, 1–10.
- Tan, J.; Li, P.; Wang, Q.; Li, Y.; Li, X.; Zhao, D.; Xu, X.; Kong, L. Autologous Menstrual Blood-Derived Stromal Cells Transplantation for Severe Asherman’s Syndrome. Hum. Reprod. 2016, 31, 2723–2729.
- Zhang, Y.; Lin, X.; Dai, Y.; Hu, X.; Zhu, H.; Jiang, Y.; Zhang, S. Endometrial Stem Cells Repair Injured Endometrium and Induce Angiogenesis via AKT and ERK Pathways. Reproduction 2016, 152, 389–402.
- Kuramoto, G.; Shimizu, T.; Takagi, S.; Ishitani, K.; Matsui, H.; Okano, T. Endometrial Regeneration Using Cell Sheet Transplantation Techniques in Rats Facilitates Successful Fertilization and Pregnancy. Fertil. Steril. 2018, 110, 172–181.e4.
- Song, T.; Zhao, X.; Sun, H.; Li, X.; Lin, N.; Ding, L.; Dai, J.; Hu, Y. Regeneration of Uterine Horns in Rats Using Collagen Scaffolds Loaded with Human Embryonic Stem Cell-Derived Endometrium-like Cells. Tissue Eng. Part A 2015, 21, 353–361.
- Pincela Lins, P.M.; Pirlet, E.; Szymonik, M.; Bronckaers, A.; Nelissen, I. Manufacture of Extracellular Vesicles Derived from Mesenchymal Stromal Cells. Trends Biotechnol. 2023, 41, 965–981.
- Ortiz, G.G.R.; Zaidi, N.H.; Saini, R.S.; Ramirez Coronel, A.A.; Alsandook, T.; Hadi Lafta, M.; Arias-Gonzáles, J.L.; Amin, A.H.; Maaliw, R.R. The Developing Role of Extracellular Vesicles in Autoimmune Diseases: Special Attention to Mesenchymal Stem Cell-Derived Extracellular Vesicles. Int. Immunopharmacol. 2023, 122, 110531.
- Bhujel, B.; Oh, S.-H.; Kim, C.-M.; Yoon, Y.-J.; Kim, Y.-J.; Chung, H.-S.; Ye, E.-A.; Lee, H.; Kim, J.-Y. Mesenchymal Stem Cells and Exosomes: A Novel Therapeutic Approach for Corneal Diseases. Int. J. Mol. Sci. 2023, 24, 10917.
- Tabeeva, G.; Silachev, D.; Vishnyakova, P.; Asaturova, A.; Fatkhudinov, T.; Smetnik, A.; Dumanovskaya, M. The Therapeutic Potential of Multipotent Mesenchymal Stromal Cell—Derived Extracellular Vesicles in Endometrial Regeneration. Int. J. Mol. Sci. 2023, 24, 9431.
- Zhao, S.; Qi, W.; Zheng, J.; Tian, Y.; Qi, X.; Kong, D.; Zhang, J.; Huang, X. Exosomes Derived from Adipose Mesenchymal Stem Cells Restore Functional Endometrium in a Rat Model of Intrauterine Adhesions. Reprod. Sci. 2020, 27, 1266–1275.
- Egami, M.; Haraguchi, Y.; Shimizu, T.; Yamato, M.; Okano, T. Latest Status of the Clinical and Industrial Applications of Cell Sheet Engineering and Regenerative Medicine. Arch. Pharm. Res. 2014, 37, 96–106.
- Takahashi, H.; Okano, T. Thermally-Triggered Fabrication of Cell Sheets for Tissue Engineering and Regenerative Medicine. Adv. Drug Deliv. Rev. 2019, 138, 276–292.
- Lin, Y.; Dong, S.; Ye, X.; Liu, J.; Li, J.; Zhang, Y.; Tu, M.; Wang, S.; Ying, Y.; Chen, R.; et al. Synergistic Regenerative Therapy of Thin Endometrium by Human Placenta-Derived Mesenchymal Stem Cells Encapsulated within Hyaluronic Acid Hydrogels. Stem Cell Res. Ther. 2022, 13, 66.
- Li, X.; Lv, H.F.; Zhao, R.; Ying, M.F.; Samuriwo, A.T.; Zhao, Y.Z. Recent Developments in Bio-Scaffold Materials as Delivery Strategies for Therapeutics for Endometrium Regeneration. Mater. Today Bio 2021, 11, 100101.
- Wang, S.; Shi, C.; Cai, X.; Wang, Y.; Chen, X.; Han, H.; Shen, H. Human Acellular Amniotic Matrix with Previously Seeded Umbilical Cord Mesenchymal Stem Cells Restores Endometrial Function in a Rat Model of Injury. Mediat. Inflamm. 2021, 2021, 5573594.
- Saldin, L.T.; Cramer, M.C.; Velankar, S.S.; White, L.J.; Badylak, S.F. Extracellular Matrix Hydrogels from Decellularized Tissues: Structure and Function. Acta Biomater. 2017, 49, 1–15.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
739
Revisions:
2 times
(View History)
Update Date:
13 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




