Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | João Paulo Mendes Tribst | -- | 2199 | 2023-10-27 15:45:29 | | | |
| 2 | Lindsay Dong | Meta information modification | 2199 | 2023-10-30 01:43:15 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
De Queiroz, T.S.; Da Cruz, B.S.; Demachkia, A.M.M.; Borges, A.L.S.; Tribst, J.P.M.; Paes Junior, T.J.D.A. Sports Mouthguards. Encyclopedia. Available online: https://encyclopedia.pub/entry/50879 (accessed on 08 February 2026).
De Queiroz TS, Da Cruz BS, Demachkia AMM, Borges ALS, Tribst JPM, Paes Junior TJDA. Sports Mouthguards. Encyclopedia. Available at: https://encyclopedia.pub/entry/50879. Accessed February 08, 2026.
De Queiroz, Talita Suelen, Beatriz Serralheiro Da Cruz, Amir Mohidin Mohamed Demachkia, Alexandre Luiz Souto Borges, João Paulo Mendes Tribst, Tarcisio José De Arruda Paes Junior. "Sports Mouthguards" Encyclopedia, https://encyclopedia.pub/entry/50879 (accessed February 08, 2026).
De Queiroz, T.S., Da Cruz, B.S., Demachkia, A.M.M., Borges, A.L.S., Tribst, J.P.M., & Paes Junior, T.J.D.A. (2023, October 27). Sports Mouthguards. In Encyclopedia. https://encyclopedia.pub/entry/50879
De Queiroz, Talita Suelen, et al. "Sports Mouthguards." Encyclopedia. Web. 27 October, 2023.
Copy Citation
Mouthguards are classified into three groups according to their fabrication: stock, boil and bite, and custom-made. Additionally, they can be fabricated from various materials that can influence their effectiveness. Among the most commonly used materials for producing this device are polyvinyl acetate–polyethylene or ethylene vinyl acetate (EVA) copolymer, polyvinyl chloride, latex, acrylic resin, and polyurethane. Although using a mouthguard in sports activities is essential for preventing or reducing orofacial injuries, impacts affecting the rigid structure while using this device remain significant, especially in the anterior region of the maxilla.
sports dentistry
orofacial trauma
sports mouthguard
reinforced mouthguards
1. Introduction
Orofacial traumas involve injuries to both soft and hard tissues of the face, such as dislocations, intrusions, extrusions, avulsions, dental fractures, soft tissue lacerations, facial bone traumas, and damage to the temporomandibular joint [1][2][3][4][5][6][7][8]. The occurrence of these injuries is considered a public health issue. Depending on their severity, they can result in a range of consequences and physical limitations for the affected patients [9][10][11]. Furthermore, in certain cases, the therapeutic process can incur substantial financial costs, and even after treatment, patients may have to cope with permanent sequelae [11][12][13].
The incidence of these traumas can occur from childhood through adulthood, with a high frequency in sports activities, whether they involve contact or non-contact sports [12][14][15][16][17][18]. With the rise in popularity of contact sports and the encouragement of physical activity participation from a young age, orofacial injuries can be observed [9][10][16][17]. However, many athletes may not be fully aware of the severe implications that can arise if proper preventive measures are not taken [16][18].
The average percentages of athletes in various sports who have experienced any type of orofacial injuries are as follows: wrestling (83.3%), boxing (73.7%), basketball (70.6%), karate (60.0%), jiu-jitsu (41.2%), handball (37.1%), soccer (23.3%), judo (22.3%), and field hockey (11.5%) [8]. The causes can range from direct to indirect traumas. Direct traumas occur when an athlete’s facial structures come into contact with another athlete or even equipment during training and competitions [1]. On the other hand, indirect traumas happen when an individual’s maxilla and mandible come into intense contact due to falls or impacts, for instance [19].
In cases of significant impacts, the face is the most vulnerable structure in the human body and often the least protected [16]. An athlete has a 10% chance of experiencing an orofacial trauma in each training or competition session, and a 33% to 56% chance over their entire career [20]. However, it is important to note that the prevalence of such injuries varies depending on the type of sport practiced, the athlete’s age and gender, and the level of contact in the competition [20][21].
Generally, the frontal region of the maxilla is subjected to horizontal impacts, resulting in a prevalence of 90% of dental injuries occurring in the upper central incisors. These impacts also affect the surrounding structures, causing not only functional and painful issues for the athlete but also aesthetic and psychological concerns [12][14][22][23].
The use of an appropriately designed mouthguard by athletes in sports activities should be encouraged [9][10]. Given the importance of preventing orofacial injuries in sports practice, the American Dental Association recommends the use of mouthguards in various sports, including acrobatic activities, basketball, cycling, boxing, horseback riding, extreme sports, track events, hockey, soccer, gymnastics, handball, ice hockey, skateboarding, lacrosse, martial arts, racquet sports, rugby, skiing, skydiving, softball, squash, surfing, volleyball, water polo, shot putting, weightlifting, and wrestling [11].
Mouthguards are classified into three groups according to their fabrication: stock, boil and bite, and custom-made [1][6][7]. Additionally, they can be fabricated from various materials that can influence their effectiveness [5]. Among the most commonly used materials for producing this device are polyvinyl acetate–polyethylene or ethylene vinyl acetate (EVA) copolymer, polyvinyl chloride, latex, acrylic resin, and polyurethane [2].
Although using a mouthguard in sports activities is essential for preventing or reducing orofacial injuries, impacts affecting the rigid structure while using this device remain significant, especially in the anterior region of the maxilla [6][7]. In this context, studies have been conducted to enhance the effectiveness of mouthguards by incorporating reinforcements, such as laminated layers, air-containing cavities [12], Sorbothane inserts [13], acrylic resin [24], silica mesh [6], titanium [14], sponges, and fiberglass [15]. However, the literature remains inconclusive regarding the best method of reinforcing mouthguards [14][15].
Orofacial trauma resulting from sports activities is common. Therefore, using protective mouthguards is strongly recommended for athletes. Many reports in the literature discuss the effectiveness of different types of sports mouthguards; however, an update about different types of protective mouthguards, materials of fabrication, design, and new technologies used, such as 3D-printed mouthguards, is needed.
2. Ergonomic Sports Mouthguards
2.1. Mouthguards
Given the high incidence of orofacial traumas among athletes during their sports activities, it is essential to encourage the use of effective protection methods [12][23][25]. Mouthguards and facial protectors are two efficient methods for preventing orofacial injuries, with their indications for use varying according to the type of sport being played [17].
Since the first mouthguards were tested in the 1920s, a reduction in oral traumas among boxers was observed, leading to the encouragement of their use among American football athletes [26]. Currently, their significance is well-established in preventing injuries to soft tissues, teeth, and the surrounding bone structures during contact sports [14][15][16]. It is important to highlight that, in dentistry, other intraoral devices such as occlusal splints or night guards are used for protecting teeth from wear in patients with bruxism, relaxing jaw muscles, and treating temporomandibular disorders [27].
In this regard, in 1950, the American Dental Association (ADA) recommended the use of resilient protective devices and mouthguards to prevent or mitigate orofacial injuries, even when the impact is not directly exerted on the tooth [6][7]. After a decade, positive outcomes were observed regarding effectiveness and a reduction in the incidence of damage to orofacial structures, which led to their mandatory use in contact sports [8].
2.2. Characteristics and Mechanisms of Protection
The mechanism of protection provided by these devices in reducing orofacial traumas involves absorbing and dissipating the energy from a received impact, thereby preventing it from directly affecting the oral structures. They function somewhat like a cushion, acting as shock absorbers and reducing the severity of trauma to the surrounding structures [8][20][26]. However, for these devices to effectively fulfill their purpose, they rely on various factors including material type, design, correct manufacturing process, appropriate thickness, and sufficient retention [8][22][28].
Ensuring adequate retention of a mouthguard is a crucial step in determining its effectiveness. This is because the device should remain securely in position during sports activities to ensure it effectively fulfills its function in the event of an impact. Moreover, this characteristic can boost athletes’ willingness to use the protective device, as it provides comfort without compromising their performance [29].
Another important parameter to consider in the characteristics of a mouthguard is its thickness. It should be sufficient to absorb and dissipate impact energy, providing adequate protection without compromising the athlete’s breathing, performance, and comfort. Neglecting these factors can lead to non-compliance with wearing the device [22][28]. While a thicker material tends to absorb more energy [9][28] it will also be more difficult to be used. The mouthguard’s thickness needs to fall within the range of 3 to 4 mm to ensure proper impact absorption and comfort [14][22].
In addition to the aforementioned points, a constant analysis of occlusion on the mouthguard’s surface is of utmost importance. Using mouthguards with inadequate occlusal adjustments can lead to mandibular fractures upon significant impact or even the development of temporomandibular joint arthritis due to prolonged use. Additionally, wear on occlusal surfaces can occur during use, making periodic checks by a dentist necessary for occlusal adjustments [30].
Several materials have been used for intraoral sports mouthguards, such as latex rubber, vinyl resins, acrylic resins, and acrylic resins combined with silicone. The optimum material for sports mouthguards should exhibit satisfactory mechanical properties with intermediate hardness and adequate energy absorption capacity, derived from good elasticity and compressive behavior. They should also be biocompatible and comfortable, to allow proper breathing and speech [31]. In this context, ethylene vinyl acetate (EVA) has been considered the most suitable material for mouthguard fabrication due to its satisfactory mechanical properties and ease of manipulation [14][31].
2.3. Classification
2.3.1. Stock Mouthguards (Pre-Fabricated)
Stock mouthguards are defined as plastic trays that cover the teeth. They are the most economical and least precise options. Typically made from polyurethane, polyvinyl chloride, or a copolymer of vinyl acetate and ethylene, and are manufactured in standardized sizes as small, medium, or large. This allows athletes to use them as soon as they acquire them [24]. However, athletes often encounter difficulty in finding information about the thickness of the material, since manufacturers typically just mention small, medium, or large size, but it is evident that there are different thicknesses associated with various available geometries. These mouthguards are characterized by their bulkiness and lack of retention [4]. This is because they are neither custom-made nor adapted for individual patients; instead, users choose them based on their perception of the appropriate size for their dental arch and often without knowledge regarding the different types and required specifications [26]. Users often experience significant discomfort in speech and breathing. Additionally, they must maintain constant occlusion to keep the mouthguard in place, leading to muscular fatigue [4]. Due to their poor retention and inadequate adaptation to the patient’s mouth size, this type of mouthguard provides the least protection against orofacial traumas and gives a false sense of security during sports activities [30], as demonstrated in Figure 1. As a result, it is considered contraindicated for use [4], despite being the most financially accessible and easiest to find on the market [26].
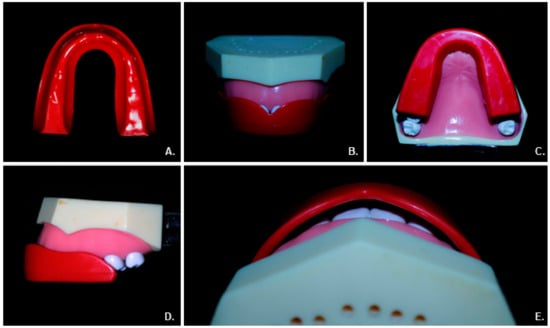
Figure 1. Different views of stock mouthguards show the lack of adequate coverage. (A) Stock mouthguard. (B) Front view showing unprotected dental tissue. (C) Occlusal view without occlusion impressions. (D) Lateral view showing inadequate coverage to the posterior teeth. (E) Space between the anterior teeth and mouthguard indicates inadequate adaptation.
2.3.2. Mouth-Formed Mouthguards (Boil and Bite)
This type of mouthguard, typically made of thermoplastic materials, is the most commonly used protective device among athletes [8]. The prescribed procedure for athletes involves immersing these mouthguards in boiling water and softening the material until it becomes malleable. Subsequently, individuals bite, suck, and modify the mouthguard with their tongue and fingers to ensure a proper fit [26], as illustrated in Figure 2. However, this adaptation method is prone to misfits and variations in thickness depending on the force applied to each area by the fingers. Moreover, it may not cover all the necessary regions for protection due to the limited available size options, particularly when it comes to extending coverage to the posterior teeth [4][31]. Moreover, it is important to consider that the forming process of these mouthguards can lead to a reduction in material thickness of around 70 to 99%, depending on the user’s technique. This lack of control over the fitting process can compromise the protective capabilities of this type of mouthguard [8].
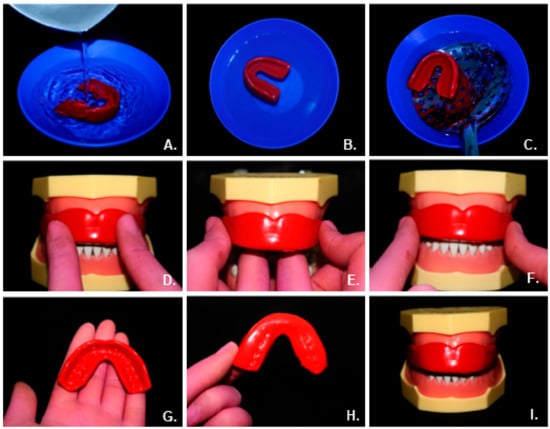
Figure 2. (A) Boil and bite mouthguard inserted into boiling water. (B) Plasticization procedure of the mouthguard in a few minutes. (C) Removal process of the mouthguard from boiling water after plasticization. (D–F) Adaptation procedure of the mouthguard in the mouth. (G–I) Final result.
2.3.3. Ergonomic Custom-Made Mouthguards
Custom-made mouthguards can be categorized as single-layer or laminated. Laminated ones consist of multiple layers of thermoplastic material firmly fused during the manufacturing process [8]. To produce these mouthguards, athletes must visit a dentist to undergo oral impressions and create a plaster model that accurately replicates the patient’s mouth structure, including the final molars, labial frenum, palate, and complete vestibular extension. Using this technique, the resulting mouthguard will be precise and efficient with an ergonomic shape. This approach also brings advantages such as enhanced speech capabilities, improved cardiopulmonary function, and reduced discomfort for the athlete [26][31][32][33][34].
The production of custom-made mouthguards employs thermoplastic materials that are heated using plasticizing machines and then adapted to the plaster model through vacuum or pressure equipment [33]. The most commonly used material is ethylene vinyl acetate (EVA), which should be heated between 80 to 120 °C [35] and formed to include all teeth in the arch, extend up to 2 mm from the vestibular fornix on the buccal side, and have a 10 mm extension in the palatal region from the gingival margin [8]. After fabrication, the dentist must perform occlusal adjustments to ensure proper protection for the athlete [30]. The steps of fabrication of custom-made mouthguards are shown in Figure 3.
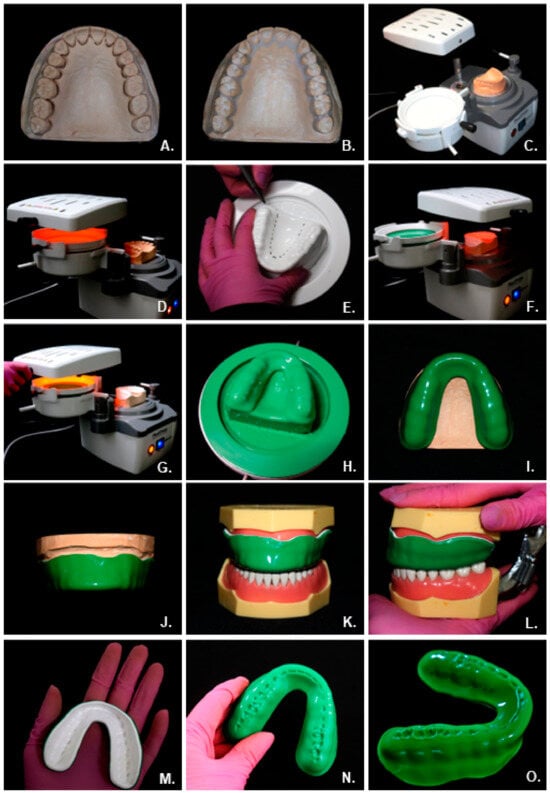
Figure 3. (A) Obtaining the plaster model. (B) Relieving undercut areas with silicone. (C) Positioning of the first layer of the EVA 3 mm plate at Plastpress Machine (Bio-art Intelligent Solutions, Sao Carlos, Sao Paulo, Brazil) to perform the vacuum plasticization procedure. (D) EVA plate heating for plasticization. (E) Delimitation of the mouthguard limit areas. (F) Heating the first layer of EVA is already plasticized to allow adhesion with the second. (G) Plasticization of the second 3 mm EVA sheet. (H) Obtaining EVA plates after the vacuum plasticization process. (I) Occlusal view of the final mouthguard. (J) Frontal view of the mouthguard on the plaster model. (K) Mouthguard on the typodont model. (L) The lateral view of the mouthguard shows the correct adaptation. (M–O) The final result of the custom-made mouthguard with occlusal registration.
Among all types of mouthguards, the custom-made type emerges as the most suitable choice and offers the highest level of protection against injuries for athletes when properly fabricated [16][33]. This is attributed to its proper fit, retention, comfort, and the absence of a negative impact on performance during sports activities, in comparison to other mouthguards [8].
References
- Saini, R. Sports Dentistry. Natl. J. Maxillofac. Surg. 2011, 2, 129.
- Knapik, J.J.; Marshall, S.W.; Lee, R.B.; Darakjy, S.S.; Jones, S.B.; Mitchener, T.A.; Dela Cruz, G.G.; Jones, B.H. Mouthguards in sports activities history, physical properties, and injury prevention effectiveness. Sports Med. 2007, 37, 117–144.
- Lam, R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust. Dent. J. 2016, 61, 4–20.
- Piccininni, P.; Clough, A.; Padilla, R.; Piccininni, G. Dental and orofacial injuries. Clin. Sports Med. 2017, 36, 369–405.
- Fernandes, L.M.; Neto, J.C.; Lima, T.F.; Magno, M.B.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.D. The use of mouthguards and prevalence of dento-alveolar trauma among athletes: A systematic review and meta-analysis. Dent. Traumatol. 2019, 35, 54–72.
- Tribst, J.P.M.; Dal Piva, A.M.O.; de Carvalho, P.C.; Gonçalves, P.H.P.; Borges, A.L.S.; Paes-Junior, T.J. Does silica–nylon mesh improves the biomechanical response of custom-made mouthguards? Sport Sci. Health 2020, 16, 75–84.
- Tribst, J.P.M.; Dal Piva, A.M.O.; Bottino, M.A.; Kleverlaan, C.J.; Koolstra, J.H. Mouthguard use and TMJ injury prevention with different occlusions: A three-dimensional finite element analysis. Dent. Traumatol. 2020, 36, 662–669.
- Sousa, A.M.; Pinho, A.C.; Messias, A.; Piedade, A.P. Present status in polymeric mouthguards. A future area for additive manufacturing? Polymers 2020, 12, 1490.
- Tulunoglu, I.; Özbek, M. Oral trauma, mouthguard awareness, and use in two contact sports in Turkey. Dent. Traumatol. 2006, 22, 242–246.
- Emerich, K.; Kaczmarek, J. First aid for dental trauma caused by sports activities: State of knowledge, treatment and prevention. Sports Med. 2010, 40, 361–366.
- Ahmed, I.; Fine, P. ‘Injury prevention versus performance’: Has the time come to mandate the use of mouthguards in all contact sports? BMJ Open Sport Exerc. Med. 2021, 7, e000828.
- Takeda, T.; Ishigami, K.; Handa, J.; Naitoh, K.; Kurokawa, K.; Shibusawa, M.; Nakajima, K.; Kawamura, S. Does hard insertion and space improve shock absorption ability of mouthguard? Dent. Traumatol. 2006, 22, 77–82.
- Bulsara, Y.R.; Matthew, I.R. Forces transmitted through a laminated mouthguard material with a Sorbothane insert. Dent. Traumatol. 1998, 14, 45–47.
- Kataoka, S.H.; Setzer, F.C.; Gondim, E., Jr.; Caldeira, C.L. Impact absorption and force dissipation of protective mouthguards with or without titanium reinforcement. J. Am. Dent. Assoc. 2014, 145, 956–959.
- Matsuda, Y.; Nakajima, K.; Saitou, M.; Katano, K.; Kanemitsu, A.; Takeda, T.; Fukuda, K. The effect of light-cured resin with a glass fiber net as an intermediate material for Hard & Space mouthguard. Dent. Traumatol. 2020, 36, 654–661.
- Kumamoto, D.P. Sports dentistry. Compendium 1993, 14, 492–502.
- Frontera, R.R.; Zanin, L.; Ambrosano, G.M.B.; Flório, F.M. Orofacial trauma in Brazilian basketball players and level of information concerning trauma and mouthguards. Dent. Traumatol. 2011, 27, 208–216.
- Bhalla, A.; Grewal, N.; Tiwari, U.; Mishra, V.; Mehla, N.S.; Raviprakash, S.; Kapur, P. Shock absorption ability of laminate mouth guards in two different malocclusions using fiber Bragg grating (FBG) sensor. Dent. Traumatol. 2013, 29, 218–225.
- Ozawa, T.; Takeda, T.; Ishigami, K.; Narimatsu, K.; Hasegawa, K.; Nakajima, K.; Noh, K. Shock absorption ability of mouthguard against forceful, traumatic mandibular closure. Dent. Traumatol. 2014, 30, 204–210.
- Tuna, E.B.; Ozel, E. Factors affecting sports-related orofacial injuries and the importance of mouthguards. Sports Med. 2014, 44, 777–783.
- Andrade, R.A.; Modesto, A.; Evans, P.L.; Almeida, A.L.; de Jesus Rodrigues da Silva, J.; Guedes, A.M.; Guedes, F.R.; Ranalli, D.N.; Tinoco, E.M. Prevalence of oral trauma in Para-Pan American Games athletes. Dent. Traumatol. 2013, 29, 280–284.
- Cummins, N.K.; Spears, I.R. The effect of mouthguard design on stresses in the tooth-bone complex. Med. Sci. Sports Exerc. 2002, 34, 942–947.
- Takeda, T.; Ishigami, K.; Nakajima, K.; Naitoh, K.; Kurokawa, K.; Handa, J.; Shomura, M.; Regner, C.W. Are all mouthguards the same and safe to use? Part 2. The influence of anterior occlusion against a direct impact on maxillary incisors. Dent. Traumatol. 2008, 24, 360–365.
- Patrick, D.G.; Van Noort, R.; Found, M.S. Evaluation of laminated structures for sports mouthguards. Key Eng. Mater. 2001, 221, 133–144.
- Park, H.K.; Park, J.Y.; Choi, N.R.; Kim, U.K.; Hwang, D.S. Sports-related oral and maxillofacial injuries: A 5-year retrospective study, Pusan National University Dental Hospital. J. Oral Maxillofac. Surg. 2021, 79, 203.e1–203.e8.
- Parker, K.; Marlow, B.; Patel, N.; Gill, D.S. A review of mouthguards: Effectiveness, types, characteristics and indications for use. Br. Dent. J. 2017, 222, 629–633.
- Crout, D.K. Anatomy of an occlusal splint. Gen Dent. 2017, 65, 52–59.
- Verissimo, C.; Costa, P.V.; Santos-Filho, P.C.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Custom-Fitted EVA Mouthguards: What is the ideal thickness? A dynamic finite element impact study. Dent. Traumatol. 2016, 32, 95–102.
- Karaganeva, R.; Pinner, S.; Tomlinson, D.; Burden, A.; Taylor, R.; Yates, J.; Winwood, K. Effect of mouthguard design on retention and potential issues arising with usability in sport. Dent. Traumatol. 2019, 35, 73–79.
- Takeda, T.; Ishigami, K.; Ogawa, T.; Nakajima, K.; Shibusawa, M.; Shimada, A.; Regner, C.W. Are all mouthguards the same and safe to use? The influence of occlusal supporting mouthguards in decreasing bone distortion and fractures. Dent. Traumatol. 2004, 20, 150–156.
- Bishop, B.M.; Davies, E.H.; von Fraunhofer, J.A. Materials for mouth protectors. J. Prosthet. Dent. 1985, 53, 256–261.
- Green, J.I. The role of mouthguards in preventing and reducing sports-related trauma. Prim. Dent. J. 2017, 6, 27–34.
- Patrick, D.G.; Van Noort, R.; Found, M.S. Scale of protection and the various types of sports mouthguard. Br. J. Sports Med. 2005, 39, 278–281.
- Caneppele, T.M.; Borges, A.B.; Pereira, D.M.; Fagundes, A.A.; Fidalgo, T.K.; Maia, L.C. Mouthguard use and cardiopulmonary capacity: A systematic review and meta-analysis. Sports Med. Int. Open. 2017, 1, E172–E182.
- Mizuhashi, F.; Koide, K. Appropriate fabrication method for vacuum-formed mouthguards. Dent. Traumatol. 2017, 33, 110–113.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
611
Revisions:
2 times
(View History)
Update Date:
30 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




