
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Juan Eduardo Sosa-Hernández | -- | 3486 | 2023-10-25 15:37:13 | | | |
| 2 | Fanny Huang | Meta information modification | 3486 | 2023-10-26 07:58:49 | | |
Video Upload Options
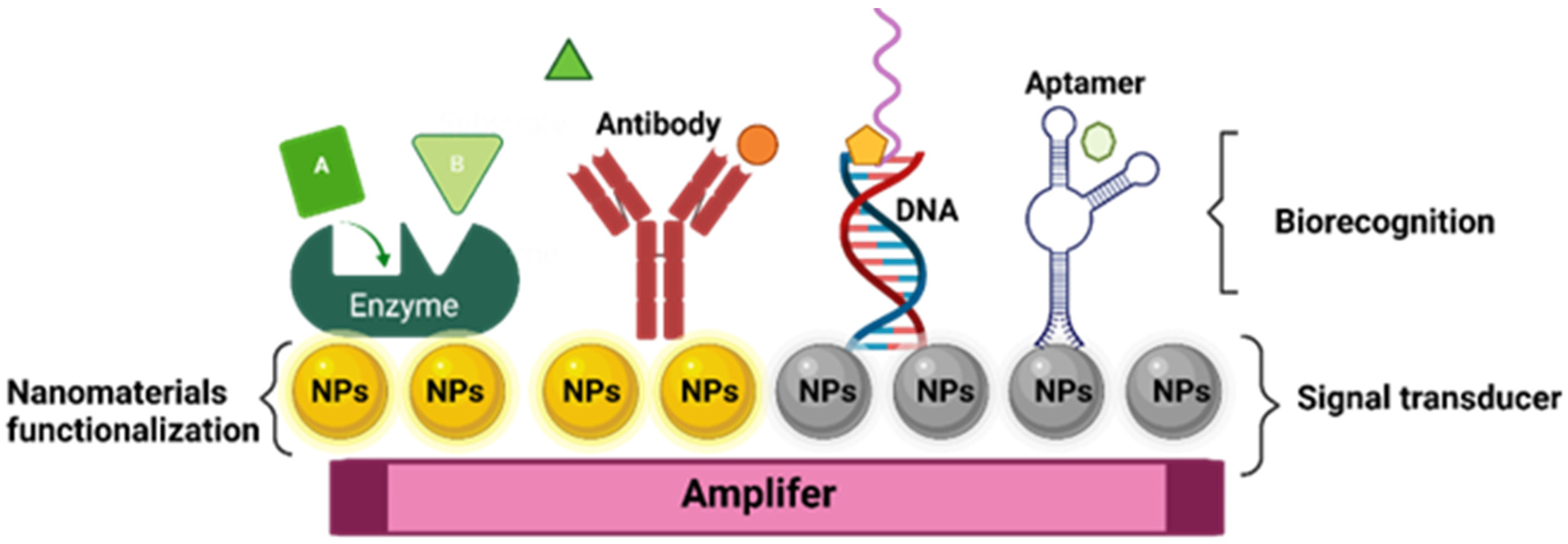
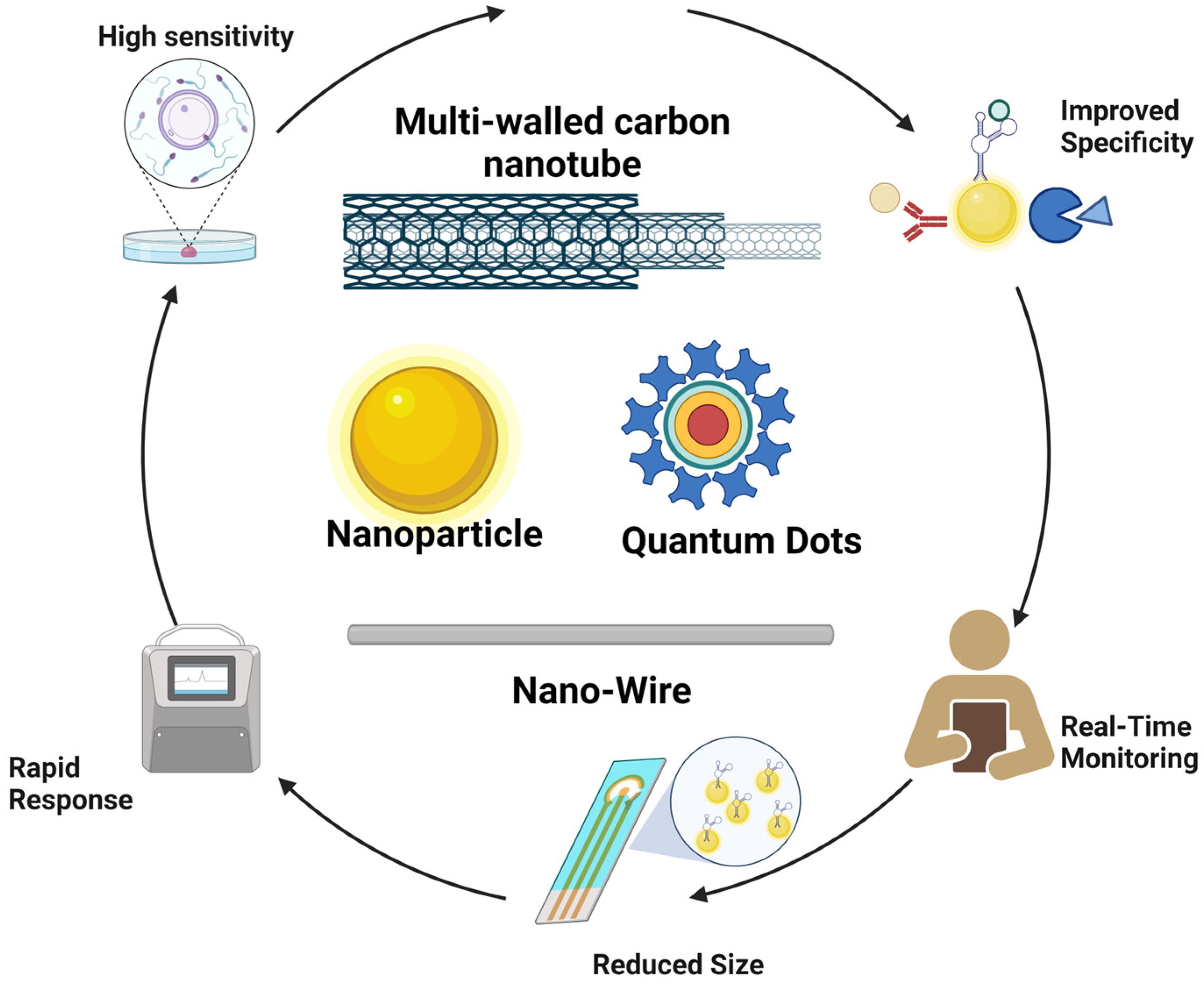
Food and waterborne illnesses are still a major concern in health and food safety areas. Methods based on biosensor devices have emerged as novel tools for faster detection of food and water pathogens, in contrast to traditional methods that are usually time-consuming and are unsuitable for large-scale monitoring. Biosensor devices can be summarized as devices that use biochemical reactions with a biorecognition section (isolated enzymes, antibodies, tissues, genetic materials, or aptamers) to detect pathogens. In most cases, biosensors are based on the correlation of electrical, thermal, or optical signals in the presence of pathogen biomarkers. The application of nano and molecular technologies allows the identification of pathogens in a faster and high-sensibility manner, at extremely low-pathogen concentrations. In fact, the integration of gold, silver, iron, and magnetic nanoparticles (NP) in biosensors has demonstrated an improvement in their detection functionality.
1. Introduction
2. Nanomaterials for the Detection of Pathogens in Water and Food
| Nanomaterial | Pathogen | Matrix | LOD | Signal | Bioconjugate Material | Reference |
|---|---|---|---|---|---|---|
| Iron core gold NPs | S. enteritidis | Beverage samples | 32 Salmonella mL−1 | Fluorescence | Antibody | [63] |
| FeO-NPS and Quantum dots | E. coli | Water | 1 × 102 CFU | Fluorescence | Aptamer | [84] |
| NAC (N-acetylcysteine) monomer | L. monocytogenes | Milk and pork meat | 1 × 103 CFU mL−1 | Fluorescence | MPIs | [85] |
| Au-N triangles | P. aeruginosa | Water | 1 cell | LSPR | Aptamer | [86] |
| Ag-NPs | E. coli | Water | 150 CFU mL−1 | Electrochemical | Aptamer | [87] |
| AgNPs | S. aureus | Bacterial suspension and human serum | 1.0 CFU mL−1 | Electrochemical | Aptamer | [88] |
| Au-NPs | S. aureus | Tap water | 101 to 104 CFU mL−1 | Fluorescence | Aptamer | [89] |
| AuNPs | S. aureus | Luria-Bertani media | 1.5 × 107 cells mL−1 | Colorimetric | Aptamer | [90] |
| AuNPs | Ochratoxin A | Peanut, soybean, and corn | 28.18 pg/mL | Colorimetric | Aptamer | [91] |
| AuNPs | E. coli | Flour | 2.5 ng µL−1 | Colorimetric | Probe | [92] |
| Graphene oxide coated AuNPs |
E. coli S. Typhimurium |
Bacterial suspension | 1 × 103 CFU | Colorimetric | Antibody | [93] |
| Ag-NPs | S. aureus | Water | 1.0 CFU mL−1 | Electrochemical | Aptamer | [94] |
| Chitosan-AgNPs | Glipopolysaccharide | Bacterial suspension | 248 CFU mL−1 | Electrochemical | - | [95] |
| AgNPs | E. coli | Pork, cabbage and milk | 2.0 CFU mL−1 | Photoelectrochemical | Peptide Magainin | [96] |
| Au-NPs and oxide of graphene NPs | E. coli | Water | 9.34 CFU mL−1 | Electrochemical | Aptamer | [97] |
| Multiwalled carbon nanotubes | E. coli | Water | 0.8 CFU mL−1 | Electrochemical | Antibody | [98] |
| Graphene and carbon nanotubes | Salmonella enteritidis | Water | 102–108 CFU mL−1 | Colorimetric | Antibody | [99] |
| Quantum dots | S. aureus, S. Typhimurium | Water | 16–28 CFU mL−1 | Colorimetric | Aptamers | [100] |
| SiNPs | E. coli | Bacterial suspension | 103 CFU mL−1 | Electrochemical | Polyclonalantibodies | [101] |
| SiNPs | E. coli | Bacterial suspension | 8 CFU mL−1 | Fluorescence | Rhodamine B | [102] |
| SiNPs | AFB1 from filamentous fungi | Peanut, maize, and badam | 0.214 pg mL−1 | Fluorescence | Aptamer | [103] |
| MNPs | S. aureus | Milk, Romaine lettuce, ham, and sausage | 2.5 ng µL−1 |
Colorimetric | Probes | [104] |
| Iron oxide MNPs assisted AuNPs | B. cereus and Shigella flexneri | Inoculated media | 12 cells mL−1 and 3 cells mL−1 |
Electrochemical | Vancomycin | [105] |
| Magnetic NPs | S. Typhimurium | Food | 53 UFC/mL | Fluorescence | Oligonucleotides | [106] |
| Iron oxide encapsulated quantum dots | Hepatitis E virus Norovirus |
Clinical samples | 56 RNA copies mL−1 69 RNA copies mL−1 |
Fluorescence Electrochemical |
Antibody | [107] |
| QDs | S. Typhimurium | Chicken meats | 43 CFU mL−1 | Fluorescence | Antibody | [108] |
| QDs | S. Typhimurium and V. parahaemolyticus | Aquatic samples | 10 CFU mL−1 102 CFU mL−1 |
Fluorescence | Aptamer | [109] |
| QDs nanobeads | S. Typhimurium | Potable water, orange juice, lettuce, and chicken | 10−1 CFU mL−1 | Fluorescence | Antibody | [110] |
| TAA *, TBA **, TMA *** and TE **** | S. aureus | Lettuce/Shrimp | 4 CFU mL−1 | Electrochemical/Fluorescence | MPIs | [111] |
4.1. Gold Nanopartícles (Au-NPs)
4.2. Silver Nanoparticles (Ag-NPs)
4.3. Carbon-Based Nanoparticles
4.4. Magnetic Nanomaterials (MNPs)
4.5. Silica Nanoparticles (Si-NPs)
4.6. Quantum Dots (QD)
References
- Estimating the Burden of Foodborne Diseases. Available online: https://www.who.int/activities/estimating-the-burden-of-foodborne-diseases (accessed on 14 March 2023).
- Riu, J.; Giussani, B. Electrochemical Biosensors for the Detection of Pathogenic Bacteria in Food. TrAC Trends Anal. Chem. 2020, 126, 115863.
- Haughton, P. La OMS Intensifica sus Esfuerzos para Mejorar la Salubridad de los Alimentos y Proteger a la Población de las Enfermedades. Available online: https://www.who.int/es/news/item/07-06-2021-who-steps-up-action-to-improve-food-safety-and-protect-people-from-disease (accessed on 10 May 2023).
- AL-Mamun, M.; Chowdhury, T.; Biswas, B.; Absar, N. Food Poisoning and Intoxication: A Global Leading Concern for Human Health. In Food Safety and Preservation; Elsevier: Amsterdam, The Netherlands, 2018; pp. 307–352. ISBN 978-0-12-814956-0.
- Chin, N.A.; Salihah, N.T.; Shivanand, P.; Ahmed, M.U. Recent Trends and Developments of PCR-Based Methods for the Detection of Food-Borne Salmonella Bacteria and Norovirus. J. Food Sci. Technol. 2022, 59, 4570–4582.
- Thomas, K.M.; De Glanville, W.A.; Barker, G.C.; Benschop, J.; Buza, J.J.; Cleaveland, S.; Davis, M.A.; French, N.P.; Mmbaga, B.T.; Prinsen, G.; et al. Prevalence of Campylobacter and Salmonella in African Food Animals and Meat: A Systematic Review and Meta-Analysis. Int. J. Food Microbiol. 2020, 315, 108382.
- Dos Santos, J.S.; Biduski, B.; Dos Santos, L.R. Listeria Monocytogenes: Health Risk and a Challenge for Food Processing Establishments. Arch. Microbiol. 2021, 203, 5907–5919.
- EFSA BIOHAZ Panel; Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bover-Cid, S.; Chemaly, M.; Davies, R.; De Cesare, A.; Herman, L.; Hilbert, F.; et al. Pathogenicity Assessment of Shiga Toxin-producing Escherichia coli (STEC) and the Public Health Risk Posed by Contamination of Food with STEC. EFS2 2020, 18, e05967.
- Zhou, J.; Yin, L.; Dong, Y.; Peng, L.; Liu, G.; Man, S.; Ma, L. CRISPR-Cas13a Based Bacterial Detection Platform: Sensing Pathogen Staphylococcus Aureus in Food Samples. Anal. Chim. Acta 2020, 1127, 225–233.
- Mora, Z.V.L.; Macías-Rodríguez, M.E.; Arratia-Quijada, J.; Gonzalez-Torres, Y.S.; Nuño, K.; Villarruel-López, A. Clostridium Perfringens as Foodborne Pathogen in Broiler Production: Pathophysiology and Potential Strategies for Controlling Necrotic Enteritis. Animals 2020, 10, 1718.
- Enosi Tuipulotu, D.; Mathur, A.; Ngo, C.; Man, S.M. Bacillus Cereus: Epidemiology, Virulence Factors, and Host–Pathogen Interactions. Trends Microbiol. 2021, 29, 458–471.
- Gupta, V.; Gulati, P.; Bhagat, N.; Dhar, M.S.; Virdi, J.S. Detection of Yersinia Enterocolitica in Food: An Overview. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 641–650.
- Pichel, N.; Vivar, M.; Fuentes, M. The Problem of Drinking Water Access: A Review of Disinfection Technologies with an Emphasis on Solar Treatment Methods. Chemosphere 2019, 218, 1014–1030.
- Adelodun, B.; Ajibade, F.O.; Ighalo, J.O.; Odey, G.; Ibrahim, R.G.; Kareem, K.Y.; Bakare, H.O.; Tiamiyu, A.O.; Ajibade, T.F.; Abdulkadir, T.S.; et al. Assessment of Socioeconomic Inequality Based on Virus-Contaminated Water Usage in Developing Countries: A Review. Environ. Res. 2021, 192, 110309.
- Ramírez-Castillo, F.; Loera-Muro, A.; Jacques, M.; Garneau, P.; Avelar-González, F.; Harel, J.; Guerrero-Barrera, A. Waterborne Pathogens: Detection Methods and Challenges. Pathogens 2015, 4, 307–334.
- Cissé, G. Food-Borne and Water-Borne Diseases under Climate Change in Low- and Middle-Income Countries: Further Efforts Needed for Reducing Environmental Health Exposure Risks. Acta Trop. 2019, 194, 181–188.
- Mahagamage, M.G.Y.L.; Pathirage, M.V.S.C.; Manage, P.M. Contamination Status of Salmonella Spp., Shigella Spp. and Campylobacter Spp. in Surface and Groundwater of the Kelani River Basin, Sri Lanka. Water 2020, 12, 2187.
- Schoenen, D. Role of Disinfection in Suppressing the Spread of Pathogens with Drinking Water: Possibilities and Limitations. Water Res. 2002, 36, 3874–3888.
- Wen, X.; Chen, F.; Lin, Y.; Zhu, H.; Yuan, F.; Kuang, D.; Jia, Z.; Yuan, Z. Microbial Indicators and Their Use for Monitoring Drinking Water Quality—A Review. Sustainability 2020, 12, 2249.
- Semenza, J.C.; Rocklöv, J.; Ebi, K.L. Climate Change and Cascading Risks from Infectious Disease. Infect. Dis. Ther. 2022, 11, 1371–1390.
- Jahne, M.A.; Schoen, M.E.; Kaufmann, A.; Pecson, B.M.; Olivieri, A.; Sharvelle, S.; Anderson, A.; Ashbolt, N.J.; Garland, J.L. Enteric Pathogen Reduction Targets for Onsite Non-Potable Water Systems: A Critical Evaluation. Water Res. 2023, 233, 119742.
- Parra-Arroyo, L.; Martínez-Ruiz, M.; Lucero, S.; Oyervides-Muñoz, M.A.; Wilkinson, M.; Melchor-Martínez, E.M.; Araújo, R.G.; Coronado-Apodaca, K.G.; Bedran, H.V.; Buitrón, G.; et al. Degradation of Viral RNA in Wastewater Complex Matrix Models and Other Standards for Wastewater-Based Epidemiology: A Review. TrAC Trends Anal. Chem. 2023, 158, 116890.
- Kaya, H.O.; Cetin, A.E.; Azimzadeh, M.; Topkaya, S.N. Pathogen Detection with Electrochemical Biosensors: Advantages, Challenges and Future Perspectives. J. Electroanal. Chem. 2021, 882, 114989.
- Kumar, H.; Kuča, K.; Bhatia, S.K.; Saini, K.; Kaushal, A.; Verma, R.; Bhalla, T.C.; Kumar, D. Applications of Nanotechnology in Sensor-Based Detection of Foodborne Pathogens. Sensors 2020, 20, 1966.
- Kabiraz, M.P.; Majumdar, P.R.; Mahmud, M.M.C.; Bhowmik, S.; Ali, A. Conventional and Advanced Detection Techniques of Foodborne Pathogens: A Comprehensive Review. Heliyon 2023, 9, e15482.
- Clais, S.; Boulet, G.; Van Kerckhoven, M.; Lanckacker, E.; Delputte, P.; Maes, L.; Cos, P. Comparison of Viable Plate Count, Turbidity Measurement and Real-time PCR for Quantification of Porphyromonas Gingivalis. Lett. Appl. Microbiol. 2015, 60, 79–84.
- Rajapaksha, P.; Elbourne, A.; Gangadoo, S.; Brown, R.; Cozzolino, D.; Chapman, J. A Review of Methods for the Detection of Pathogenic Microorganisms. Analyst 2019, 144, 396–411.
- López, M.M.; Ilop, P. Noales Are Molecular Tools Solving the Challenges Posed by Detection of Plant Pathogenic Bacteria and Viruses? Curr. Issues Mol. Biol. 2009, 11, 13–46.
- Aw, T.G.; Rose, J.B. Detection of Pathogens in Water: From Phylochips to qPCR to Pyrosequencing. Curr. Opin. Biotechnol. 2012, 23, 422–430.
- Fu, Y.; Peng, H.; Liu, J.; Nguyen, T.H.; Hashmi, M.Z.; Shen, C. Occurrence and Quantification of Culturable and Viable but Non-Culturable (VBNC) Pathogens in Biofilm on Different Pipes from a Metropolitan Drinking Water Distribution System. Sci. Total Environ. 2021, 764, 142851.
- Srivastava, K.R.; Awasthi, S.; Mishra, P.K.; Srivastava, P.K. Biosensors/Molecular Tools for Detection of Waterborne Pathogens. In Waterborne Pathogens; Elsevier: Amsterdam, The Netherlands, 2020; pp. 237–277. ISBN 978-0-12-818783-8.
- Sun, Y.-J.; Chen, G.-F.; Zhang, C.-Y.; Guo, C.-L.; Wang, Y.-Y.; Sun, R. Development of a Multiplex Polymerase Chain Reaction Assay for the Parallel Detection of Harmful Algal Bloom-Forming Species Distributed along the Chinese Coast. Harmful Algae 2019, 84, 36–45.
- Kim, J.-H.; Oh, S.-W. Rapid and Sensitive Detection of E. coli O157:H7 and S. typhimurium in Iceberg Lettuce and Cabbage Using Filtration, DNA Concentration, and qPCR without Enrichment. Food Chem. 2020, 327, 127036.
- Chen, B.; Jiang, Y.; Cao, X.; Liu, C.; Zhang, N.; Shi, D. Droplet Digital PCR as an Emerging Tool in Detecting Pathogens Nucleic Acids in Infectious Diseases. Clin. Chim. Acta 2021, 517, 156–161.
- Zhao, Y.; Zeng, D.; Yan, C.; Chen, W.; Ren, J.; Jiang, Y.; Jiang, L.; Xue, F.; Ji, D.; Tang, F.; et al. Rapid and Accurate Detection of Escherichia coli O157:H7 in Beef Using Microfluidic Wax-Printed Paper-Based ELISA. Analyst 2020, 145, 3106–3115.
- Liu, S.; Hu, Q.; Li, C.; Zhang, F.; Gu, H.; Wang, X.; Li, S.; Xue, L.; Madl, T.; Zhang, Y.; et al. Wide-Range, Rapid, and Specific Identification of Pathogenic Bacteria by Surface-Enhanced Raman Spectroscopy. ACS Sens. 2021, 6, 2911–2919.
- Bu, T.; Jia, P.; Liu, J.; Liu, Y.; Sun, X.; Zhang, M.; Tian, Y.; Zhang, D.; Wang, J.; Wang, L. Diversely Positive-Charged Gold Nanoparticles Based Biosensor: A Label-Free and Sensitive Tool for Foodborne Pathogen Detection. Food Chem. X 2019, 3, 100052.
- DeMone, C.; Hwang, M.-H.; Feng, Z.; McClure, J.T.; Greenwood, S.J.; Fung, R.; Kim, M.; Weese, J.S.; Shapiro, K. Application of next Generation Sequencing for Detection of Protozoan Pathogens in Shellfish. Food Waterborne Parasitol. 2020, 21, e00096.
- Eyre, D.W. Infection Prevention and Control Insights from a Decade of Pathogen Whole-Genome Sequencing. J. Hosp. Infect. 2022, 122, 180–186.
- Dąbrowiecki, Z.; Dąbrowiecka, M.; Olszański, R.; Siermontowski, P. Developing a Methodology for Testing and Preliminary Determination of the Presence of and in Environmental Water Samples by Immunomagnetic Separation Combined with Flow Cytometry. Pol. Hyperb. Res. 2019, 68, 71–92.
- Bulard, E.; Bouchet-Spinelli, A.; Chaud, P.; Roget, A.; Calemczuk, R.; Fort, S.; Livache, T. Carbohydrates as New Probes for the Identification of Closely Related Escherichia coli Strains Using Surface Plasmon Resonance Imaging. Available online: https://pubs.acs.org/doi/pdf/10.1021/ac5037704 (accessed on 26 April 2023).
- Ahmed, S.; Ansari, A.; Siddiqui, M.A.; Imran, M.; Kumari, B.; Khan, A.; Ranjan, P. Electrochemical and Optical-Based Systems for SARS-CoV-2 and Various Pathogens Assessment. Adv. Nat. Sci. Nanosci. Nanotechnol. 2023, 14, 033001.
- Losada-Garcia, N.; Garcia-Sanz, C.; Andreu, A.; Velasco-Torrijos, T.; Palomo, J.M. Glyconanomaterials for Human Virus Detection and Inhibition. Nanomaterials 2021, 11, 1684.
- Wen, C.-Y.; Liang, X.; Liu, J.; Zhao, T.-Y.; Li, X.; Zhang, Y.; Guo, G.; Zhang, Z.; Zeng, J. An Achromatic Colorimetric Nanosensor for Sensitive Multiple Pathogen Detection by Coupling Plasmonic Nanoparticles with Magnetic Separation. Talanta 2023, 256, 124271.
- Jain, S.; Nehra, M.; Kumar, R.; Dilbaghi, N.; Hu, T.; Kumar, S.; Kaushik, A.; Li, C. Internet of Medical Things (IoMT)-Integrated Biosensors for Point-of-Care Testing of Infectious Diseases. Biosens. Bioelectron. 2021, 179, 113074.
- Salama, A.M.; Yasin, G.; Zourob, M.; Lu, J. Fluorescent Biosensors for the Detection of Viruses Using Graphene and Two-Dimensional Carbon Nanomaterials. Biosensors 2022, 12, 460.
- Nate, Z.; Gill, A.A.S.; Chauhan, R.; Karpoormath, R. Recent Progress in Electrochemical Sensors for Detection and Quantification of Malaria. Anal. Biochem. 2022, 643, 114592.
- Nnachi, R.C.; Sui, N.; Ke, B.; Luo, Z.; Bhalla, N.; He, D.; Yang, Z. Biosensors for Rapid Detection of Bacterial Pathogens in Water, Food and Environment. Environ. Int. 2022, 166, 107357.
- Sharifi, S.; Vahed, S.Z.; Ahmadian, E.; Dizaj, S.M.; Eftekhari, A.; Khalilov, R.; Ahmadi, M.; Hamidi-Asl, E.; Labib, M. Detection of Pathogenic Bacteria via Nanomaterials-Modified Aptasensors. Biosens. Bioelectron. 2020, 150, 111933.
- Hegde, M.; Pai, P.; Shetty, M.G.; Babitha, K.S. Gold Nanoparticle Based Biosensors for Rapid Pathogen Detection: A Review. Environ. Nanotechnol. Monit. Manag. 2022, 18, 100756.
- Sadanandan, S.; Meenakshi, V.S.; Ramkumar, K.; Pillai, N.P.; Anuvinda, P.; Sreelekshmi, P.J.; Devika, V.; Ramanunni, K.; Jeevan Sankar, R.; Sreejaya, M.M. Biorecognition Elements Appended Gold Nanoparticle Biosensors for the Detection of Food-Borne Pathogens—A Review. Food Control 2023, 148, 109510.
- Cho, I.-H.; Ku, S. Current Technical Approaches for the Early Detection of Foodborne Pathogens: Challenges and Opportunities. IJMS 2017, 18, 2078.
- Li, D.; Liu, L.; Huang, Q.; Tong, T.; Zhou, Y.; Li, Z.; Bai, Q.; Liang, H.; Chen, L. Recent Advances on Aptamer-Based Biosensors for Detection of Pathogenic Bacteria. World J. Microbiol. Biotechnol. 2021, 37, 45.
- Chamundeeswari, M.; Jeslin, J.; Verma, M.L. Nanocarriers for Drug Delivery Applications. Environ. Chem. Lett. 2019, 17, 849–865.
- Ghorbani, F.; Abbaszadeh, H.; Mehdizadeh, A.; Ebrahimi-Warkiani, M.; Rashidi, M.-R.; Yousefi, M. Biosensors and Nanobiosensors for Rapid Detection of Autoimmune Diseases: A Review. Microchim. Acta 2019, 186, 838.
- Ali, A.A.; Altemimi, A.B.; Alhelfi, N.; Ibrahim, S.A. Application of Biosensors for Detection of Pathogenic Food Bacteria: A Review. Biosensors 2020, 10, 58.
- Kuswandi, B. Nanobiosensor Approaches for Pollutant Monitoring. Environ. Chem. Lett. 2019, 17, 975–990.
- Chandra, P.; Prakash, R. (Eds.) Nanobiomaterial Engineering: Concepts and Their Applications in Biomedicine and Diagnostics; Springer: Singapore, 2020; ISBN 978-981-329-839-2.
- Fracchiolla, N.; Artuso, S.; Cortelezzi, A. Biosensors in Clinical Practice: Focus on Oncohematology. Sensors 2013, 13, 6423–6447.
- Zhang, Z.; Zhou, J.; Du, X. Electrochemical Biosensors for Detection of Foodborne Pathogens. Micromachines 2019, 10, 222.
- Saha, K.; Agasti, S.S.; Kim, C.; Li, X.; Rotello, V.M. Gold Nanoparticles in Chemical and Biological Sensing. Chem. Rev. 2012, 112, 2739–2779.
- Tuteja, S.K.; Mutreja, R.; Neethirajan, S.; Ingebrandt, S. Bioconjugation of Different Nanosurfaces With Biorecognition Molecules for the Development of Selective Nanosensor Platforms. In Advances in Nanosensors for Biological and Environmental Analysis; Elsevier: Amsterdam, The Netherlands, 2019; pp. 79–94. ISBN 978-0-12-817456-2.
- Zhao, X.; Smith, G.; Javed, B.; Dee, G.; Gun’ko, Y.K.; Curtin, J.; Byrne, H.J.; O’Connor, C.; Tian, F. Design and Development of Magnetic Iron Core Gold Nanoparticle-Based Fluorescent Multiplex Assay to Detect Salmonella. Nanomaterials 2022, 12, 3917.
- Verma, M.L.; Rani, V. Biosensors for Toxic Metals, Polychlorinated Biphenyls, Biological Oxygen Demand, Endocrine Disruptors, Hormones, Dioxin, Phenolic and Organophosphorus Compounds: A Review. Environ. Chem. Lett. 2021, 19, 1657–1666.
- de Morais Mirres, A.C.; da Silva, B.E.P.d.M.; Tessaro, L.; Galvan, D.; de Andrade, J.C.; Aquino, A.; Joshi, N.; Conte-Junior, C.A. Recent Advances in Nanomaterial-Based Biosensors for Pesticide Detection in Foods. Biosensors 2022, 12, 572.
- Munawar, A.; Ong, Y.; Schirhagl, R.; Tahir, M.A.; Khan, W.S.; Bajwa, S.Z. Nanosensors for Diagnosis with Optical, Electric and Mechanical Transducers. RSC Adv. 2019, 9, 6793–6803.
- Javaid, M.; Haleem, A.; Singh, R.P.; Rab, S.; Suman, R. Exploring the Potential of Nanosensors: A Brief Overview. Sens. Int. 2021, 2, 100130.
- Irkham, I.; Ibrahim, A.U.; Pwavodi, P.C.; Al-Turjman, F.; Hartati, Y.W. Smart Graphene-Based Electrochemical Nanobiosensor for Clinical Diagnosis: Review. Sensors 2023, 23, 2240.
- Song, M.; Yang, M.; Hao, J. Pathogenic Virus Detection by Optical Nanobiosensors. Cell Rep. Phys. Sci. 2021, 2, 100288.
- Naresh, V.; Lee, N. A Review on Biosensors and Recent Development of Nanostructured Materials-Enabled Biosensors. Sensors 2021, 21, 1109.
- Saleh Ibrahim, Y.; Alexis Ramírez-Coronel, A.; Kumar Sain, D.; Haleem Al-qaim, Z.; Hassan Jawhar, Z.; Yaseen Mahmood Alabdali, A.; Hayif Jasim Ali, S.; Althomali, R.H.; Fakri Mustafa, Y.; Mireya Romero-Parra, R. Advances in Nanomaterials-Based Chemiluminescence (Bio)Sensor for Specific and Sensitive Determination of Pathogenic Bacteria. Microchem. J. 2023, 191, 108860.
- Selvolini, G.; Marrazza, G. MIP-Based Sensors: Promising New Tools for Cancer Biomarker Determination. Sensors 2017, 17, 718.
- Hroncekova, S.; Lorencova, L.; Bertok, T.; Hires, M.; Jane, E.; Bučko, M.; Kasak, P.; Tkac, J. Amperometric Miniaturised Portable Enzymatic Nanobiosensor for the Ultrasensitive Analysis of a Prostate Cancer Biomarker. JFB 2023, 14, 161.
- Farrokhnia, M.; Amoabediny, G.; Ebrahimi, M.; Ganjali, M.; Arjmand, M. Ultrasensitive Early Detection of Insulin Antibody Employing Novel Electrochemical Nano-Biosensor Based on Controllable Electro-Fabrication Process. Talanta 2022, 238, 122947.
- Zhang, L.; Mazouzi, Y.; Salmain, M.; Liedberg, B.; Boujday, S. Antibody-Gold Nanoparticle Bioconjugates for Biosensors: Synthesis, Characterization and Selected Applications. Biosens. Bioelectron. 2020, 165, 112370.
- Park, D.H.; Choi, M.Y.; Choi, J.-H. Recent Development in Plasmonic Nanobiosensors for Viral DNA/RNA Biomarkers. Biosensors 2022, 12, 1121.
- Rawat, N.K.; Ghosh, R. Chapter 8—Conducting Polymer–Based Nanobiosensors. In Nanosensors for Smart Cities; Han, B., Tomer, V.K., Nguyen, T.A., Farmani, A., Kumar Singh, P., Eds.; Micro and Nano Technologies; Elsevier: Amsterdam, The Netherlands, 2020; pp. 129–142. ISBN 978-0-12-819870-4.
- Fang, R.H.; Jiang, Y.; Fang, J.C.; Zhang, L. Cell Membrane-Derived Nanomaterials for Biomedical Applications. Biomaterials 2017, 128, 69–83.
- Aliakbar Ahovan, Z.; Hashemi, A.; De Plano, L.M.; Gholipourmalekabadi, M.; Seifalian, A. Bacteriophage Based Biosensors: Trends, Outcomes and Challenges. Nanomaterials 2020, 10, 501.
- Solaimuthu, A.; Vijayan, A.N.; Murali, P.; Korrapati, P.S. Nano-Biosensors and Their Relevance in Tissue Engineering. Curr. Opin. Biomed. Eng. 2020, 13, 84–93.
- Negahdary, M.; Angnes, L. Electrochemical Nanobiosensors Equipped with Peptides: A Review. Microchim. Acta 2022, 189, 94.
- Tsao, Y.-H.; Husain, R.A.; Lin, Y.-J.; Khan, I.; Chen, S.-W.; Lin, Z.-H. A Self-Powered Mercury Ion Nanosensor Based on the Thermoelectric Effect and Chemical Transformation Mechanism. Nano Energy 2019, 62, 268–274.
- Yu, R.; Niu, S.; Pan, C.; Wang, Z.L. Piezotronic Effect Enhanced Performance of Schottky-Contacted Optical, Gas, Chemical and Biological Nanosensors. Nano Energy 2015, 14, 312–339.
- Pandit, C.; Alajangi, H.K.; Singh, J.; Khajuria, A.; Sharma, A.; Hassan, M.S.; Parida, M.; Semwal, A.D.; Gopalan, N.; Sharma, R.K.; et al. Development of Magnetic Nanoparticle Assisted Aptamer-Quantum Dot Based Biosensor for the Detection of Escherichia coli in Water Samples. Sci. Total Environ. 2022, 831, 154857.
- Zhao, X.; Cui, Y.; Wang, J.; Wang, J. Preparation of Fluorescent Molecularly Imprinted Polymers via Pickering Emulsion Interfaces and the Application for Visual Sensing Analysis of Listeria Monocytogenes. Polymers 2019, 11, 984.
- Hu, J.; Fu, K.; Bohn, P.W. Whole-Cell Pseudomonas Aeruginosa Localized Surface Plasmon Resonance Aptasensor. Anal. Chem. 2018, 90, 2326–2332.
- Dabhade, A.H.; Verma, R.P.; Paramasivan, B.; Kumawat, A.; Saha, B. Development of Silver Nanoparticles and Aptamer Conjugated Biosensor for Rapid Detection of E. coli in a Water Sample. 3 Biotech 2023, 13, 244.
- Shahdost-Fard, F.; Faridfar, S.; Keihan, A.H.; Aghaei, M.; Petrenko, I.; Ahmadi, F.; Ehrlich, H.; Rahimi-Nasrabadi, M. Applicability of a Green Nanocomposite Consisted of Spongin Decorated Cu2WO4(OH)2 and AgNPs as a High-Performance Aptasensing Platform in Staphylococcus Aureus Detection. Biosensors 2023, 13, 271.
- Sun, R.; Zou, H.; Zhang, Y.; Zhang, X.; Chen, L.; Lv, R.; Sheng, R.; Du, T.; Li, Y.; Wang, H.; et al. Vancomycin Recognition and Induced-Aggregation of the Au Nanoparticles through Freeze-Thaw for Foodborne Pathogen Staphylococcus aureus Detection. Anal. Chim. Acta 2022, 1190, 339253.
- Lim, S.H.; Ryu, Y.C.; Hwang, B.H. Aptamer-Immobilized Gold Nanoparticles Enable Facile and On-Site Detection of Staphylococcus aureus. Biotechnol. Bioprocess Eng. 2021, 26, 107–113.
- Yang, X.; Huang, R.; Xiong, L.; Chen, F.; Sun, W.; Yu, L. A Colorimetric Aptasensor for Ochratoxin A Detection Based on Tetramethylrhodamine Charge Effect-Assisted Silver Enhancement. Biosensors 2023, 13, 468.
- Dester, E.; Kao, K.; Alocilja, E.C. Detection of Unamplified E. coli O157 DNA Extracted from Large Food Samples Using a Gold Nanoparticle Colorimetric Biosensor. Biosensors 2022, 12, 274.
- Kaushal, S.; Pinnaka, A.K.; Soni, S.; Singhal, N.K. Antibody Assisted Graphene Oxide Coated Gold Nanoparticles for Rapid Bacterial Detection and near Infrared Light Enhanced Antibacterial Activity. Sens. Actuators B Chem. 2021, 329, 129141.
- Abbaspour, A.; Norouz-Sarvestani, F.; Noori, A.; Soltani, N. Aptamer-Conjugated Silver Nanoparticles for Electrochemical Dual-Aptamer-Based Sandwich Detection of Staphylococcus aureus. Biosens. Bioelectron. 2015, 68, 149–155.
- Imran, M.; Ehrhardt, C.J.; Bertino, M.F.; Shah, M.R.; Yadavalli, V.K. Chitosan Stabilized Silver Nanoparticles for the Electrochemical Detection of Lipopolysaccharide: A Facile Biosensing Approach for Gram-Negative Bacteria. Micromachines 2020, 11, 413.
- Yin, M.; Liu, C.; Ge, R.; Fang, Y.; Wei, J.; Chen, X.; Chen, Q.; Chen, X. Paper-Supported near-Infrared-Light-Triggered Photoelectrochemical Platform for Monitoring Escherichia coli O157:H7 Based on Silver Nanoparticles-Sensitized-Upconversion Nanophosphors. Biosens. Bioelectron. 2022, 203, 114022.
- Qaanei, M.; Taheri, R.A.; Eskandari, K. Electrochemical Aptasensor for Escherichia coli O157:H7 Bacteria Detection Using a Nanocomposite of Reduced Graphene Oxide, Gold Nanoparticles and Polyvinyl Alcohol. Anal. Methods 2021, 13, 3101–3109.
- Ertaş, T.; Dinç, B.; Üstünsoy, R.; Eraslan, H.; Ergenç, A.F.; Bektaş, M. Novel Electrochemical Biosensor for Escherichia coli Using Gold-Coated Tungsten Wires and Antibody Functionalized Short Multiwalled Carbon Nanotubes. Instrum. Sci. Technol. 2023, 2, 1–16.
- Wang, Z.; Yao, X.; Wang, R.; Ji, Y.; Yue, T.; Sun, J.; Li, T.; Wang, J.; Zhang, D. Label-Free Strip Sensor Based on Surface Positively Charged Nitrogen-Rich Carbon Nanoparticles for Rapid Detection of Salmonella Enteritidis. Biosens. Bioelectron. 2019, 132, 360–367.
- Kurt, H.; Yüce, M.; Hussain, B.; Budak, H. Dual-Excitation Upconverting Nanoparticle and Quantum Dot Aptasensor for Multiplexed Food Pathogen Detection. Biosens. Bioelectron. 2016, 81, 280–286.
- Mathelié-Guinlet, M.; Cohen-Bouhacina, T.; Gammoudi, I.; Martin, A.; Béven, L.; Delville, M.-H.; Grauby-Heywang, C. Silica Nanoparticles-Assisted Electrochemical Biosensor for the Rapid, Sensitive and Specific Detection of Escherichia coli. Sens. Actuators B Chem. 2019, 292, 314–320.
- Jenie, S.N.A.; Kusumastuti, Y.; Krismastuti, F.S.H.; Untoro, Y.M.; Dewi, R.T.; Udin, L.Z.; Artanti, N. Rapid Fluorescence Quenching Detection of Escherichia coli Using Natural Silica-Based Nanoparticles. Sensors 2021, 21, 881.
- Wu, Z.; Sun, D.-W.; Pu, H.; Wei, Q. A Dual Signal-on Biosensor Based on Dual-Gated Locked Mesoporous Silica Nanoparticles for the Detection of Aflatoxin B1. Talanta 2023, 253, 124027.
- Boodoo, C.; Dester, E.; David, J.; Patel, V.; Kc, R.; Alocilja, E.C. Multi-Probe Nano-Genomic Biosensor to Detect S. aureus from Magnetically-Extracted Food Samples. Biosensors 2023, 13, 608.
- Diouani, M.F.; Sayhi, M.; Djafar, Z.R.; Ben Jomaa, S.; Belgacem, K.; Gharbi, H.; Ghita, M.; Popescu, L.-M.; Piticescu, R.; Laouini, D. Magnetic Separation and Centri-Chronoamperometric Detection of Foodborne Bacteria Using Antibiotic-Coated Metallic Nanoparticles. Biosensors 2021, 11, 205.
- Wen, J.; Ren, L.; He, Q.; Bao, J.; Zhang, X.; Pi, Z.; Chen, Y. Contamination-Free V-Shaped Ultrafast Reaction Cascade Transferase Signal Amplification Driven CRISPR/Cas12a Magnetic Relaxation Switching Biosensor for Bacteria Detection. Biosens. Bioelectron. 2023, 219, 114790.
- Ganganboina, A.B.; Chowdhury, A.D.; Khoris, I.M.; Doong, R.; Li, T.-C.; Hara, T.; Abe, F.; Suzuki, T.; Park, E.Y. Hollow Magnetic-Fluorescent Nanoparticles for Dual-Modality Virus Detection. Biosens. Bioelectron. 2020, 170, 112680.
- Kulkarni, M.B.; Ayachit, N.H.; Aminabhavi, T.M. Biosensors and Microfluidic Biosensors: From Fabrication to Application. Biosensors 2022, 12, 543.
- Liu, L.; Hong, J.; Wang, W.; Xiao, S.; Xie, H.; Wang, Q.; Gan, N. Fluorescent Aptasensor for Detection of Live Foodborne Pathogens Based on Multicolor Perovskite-Quantum-Dot-Encoded DNA Probes and Dual-Stirring-Bar-Assisted Signal Amplification. J. Pharm. Anal. 2022, 12, 913–922.
- Shang, Y.; Cai, S.; Ye, Q.; Wu, Q.; Shao, Y.; Qu, X.; Xiang, X.; Zhou, B.; Ding, Y.; Chen, M.; et al. Quantum Dot Nanobeads-Labelled Lateral Flow Immunoassay Strip for Rapid and Sensitive Detection of Salmonella Typhimurium Based on Strand Displacement Loop-Mediated Isothermal Amplification. Engineering 2022, 19, 62–70.
- Wang, L.; Lin, X.; Liu, T.; Zhang, Z.; Kong, J.; Yu, H.; Yan, J.; Luan, D.; Zhao, Y.; Bian, X. Reusable and Universal Impedimetric Sensing Platform for the Rapid and Sensitive Detection of Pathogenic Bacteria Based on Bacteria-Imprinted Polythiophene Film. Analyst 2022, 147, 4433–4441.
- Alafeef, M.; Moitra, P.; Pan, D. Nano-Enabled Sensing Approaches for Pathogenic Bacterial Detection. Biosens. Bioelectron. 2020, 165, 112276.
- Ayodhya, D. Recent Progress on Detection of Bivalent, Trivalent, and Hexavalent Toxic Heavy Metal Ions in Water Using Metallic Nanoparticles: A Review. Results Chem. 2023, 5, 100874.
- Patel, R.; Mitra, B.; Vinchurkar, M.; Adami, A.; Patkar, R.; Giacomozzi, F.; Lorenzelli, L.; Baghini, M.S. A Review of Recent Advances in Plant-Pathogen Detection Systems. Heliyon 2022, 8, e11855.
- Loiseau, A.; Asila, V.; Boitel-Aullen, G.; Lam, M.; Salmain, M.; Boujday, S. Silver-Based Plasmonic Nanoparticles for and Their Use in Biosensing. Biosensors 2019, 9, 78.
- Ibrahim, N.; Jamaluddin, N.D.; Tan, L.L.; Mohd Yusof, N.Y. A Review on the Development of Gold and Silver Nanoparticles-Based Biosensor as a Detection Strategy of Emerging and Pathogenic RNA Virus. Sensors 2021, 21, 5114.
- Yu, X.; Jiao, Y.; Chai, Q. Applications of Gold Nanoparticles in Biosensors. Nano LIFE 2016, 6, 1642001.
- Baetsen-Young, A.M.; Vasher, M.; Matta, L.L.; Colgan, P.; Alocilja, E.C.; Day, B. Direct Colorimetric Detection of Unamplified Pathogen DNA by Dextrin-Capped Gold Nanoparticles. Biosens. Bioelectron. 2018, 101, 29–36.
- Hui, C.; Hu, S.; Yang, X.; Guo, Y. A Panel of Visual Bacterial Biosensors for the Rapid Detection of Genotoxic and Oxidative Damage: A Proof of Concept Study. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2023, 888, 503639.
- Liu, J.; Xu, J.-Z.; Rao, Z.-M.; Zhang, W.-G. An Enzymatic Colorimetric Whole-Cell Biosensor for High-Throughput Identification of Lysine Overproducers. Biosens. Bioelectron. 2022, 216, 114681.
- Miranda, R.R.; Sampaio, I.; Zucolotto, V. Exploring Silver Nanoparticles for Cancer Therapy and Diagnosis. Colloids Surf. B Biointerfaces 2022, 210, 112254.
- Douaki, A.; Demelash Abera, B.; Cantarella, G.; Shkodra, B.; Mushtaq, A.; Ibba, P.; Inam, A.S.; Petti, L.; Lugli, P. Flexible Screen Printed Aptasensor for Rapid Detection of Furaneol: A Comparison of CNTs and AgNPs Effect on Aptasensor Performance. Nanomaterials 2020, 10, 1167.
- Li, G. Nano-Inspired Biosensors for Protein Assay with Clinical Applications; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 978-0-12-815054-2.
- Varghese Alex, K.; Tamil Pavai, P.; Rugmini, R.; Shiva Prasad, M.; Kamakshi, K.; Sekhar, K.C. Green Synthesized Ag Nanoparticles for Bio-Sensing and Photocatalytic Applications. ACS Omega 2020, 5, 13123–13129.
- Nguyen, T.N.; Phung, V.-D.; Tran, V.V. Recent Advances in Conjugated Polymer-Based Biosensors for Virus Detection. Biosensors 2023, 13, 586.
- Bakhshandeh, B.; Sorboni, S.G.; Haghighi, D.M.; Ahmadi, F.; Dehghani, Z.; Badiei, A. New Analytical Methods Using Carbon-Based Nanomaterials for Detection of Salmonella Species as a Major Food Poisoning Organism in Water and Soil Resources. Chemosphere 2022, 287, 132243.
- Sharma, A.; Sharma, N.; Kumari, A.; Lee, H.-J.; Kim, T.; Tripathi, K.M. Nano-Carbon Based Sensors for Bacterial Detection and Discrimination in Clinical Diagnosis: A Junction between Material Science and Biology. Appl. Mater. Today 2020, 18, 100467.
- Bhattacharya, K.; Mukherjee, S.P.; Gallud, A.; Burkert, S.C.; Bistarelli, S.; Bellucci, S.; Bottini, M.; Star, A.; Fadeel, B. Biological Interactions of Carbon-Based Nanomaterials: From Coronation to Degradation. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 333–351.
- Duan, N.; Wu, S.; Dai, S.; Miao, T.; Chen, J.; Wang, Z. Simultaneous Detection of Pathogenic Bacteria Using an Aptamer Based Biosensor and Dual Fluorescence Resonance Energy Transfer from Quantum Dots to Carbon Nanoparticles. Microchim. Acta 2015, 182, 917–923.
- Shen, Y.; Zhang, Y.; Gao, Z.F.; Ye, Y.; Wu, Q.; Chen, H.-Y.; Xu, J.-J. Recent Advances in Nanotechnology for Simultaneous Detection of Multiple Pathogenic Bacteria. Nano Today 2021, 38, 101121.
- Fang, Y.; Wang, Y.; Zhu, L.; Liu, H.; Su, X.; Liu, Y.; Chen, Z.; Chen, H.; He, N. A Novel Cartridge for Nucleic Acid Extraction, Amplification and Detection of Infectious Disease Pathogens with the Help of Magnetic Nanoparticles. Chin. Chem. Lett. 2023, 34, 108092.
- Hussain, C.M. Analytical Applications of Functionalized Magnetic Nanoparticles; Royal Society of Chemistry: London, UK, 2021; ISBN 978-1-83916-276-3.
- Huang, H.T.; Garu, P.; Li, C.H.; Chang, W.C.; Chen, B.W.; Sung, S.Y.; Lee, C.M.; Chen, J.Y.; Hsieh, T.F.; Sheu, W.J.; et al. Magnetoresistive Biosensors for Direct Detection of Magnetic Nanoparticle Conjugated Biomarkers on a Chip. SPIN 2019, 9, 1940002.
- Min, C.; Shao, H.; Liong, M.; Yoon, T.-J.; Weissleder, R.; Lee, H. Mechanism of Magnetic Relaxation Switching Sensing. ACS Nano 2012, 6, 6821–6828.
- Arya, S.; Singh, A.; Sharma, A.; Gupta, V. 11—Silicon-Based Biosensor. In Silicon-Based Hybrid Nanoparticles; Thomas, S., Nguyen, T.A., Ahmadi, M., Yasin, G., Joshi, N., Eds.; Micro and Nano Technologies; Elsevier: Amsterdam, The Netherlands, 2022; pp. 247–267. ISBN 978-0-12-824007-6.
- Bagheri, E.; Ansari, L.; Sameiyan, E.; Abnous, K.; Taghdisi, S.M.; Ramezani, M.; Alibolandi, M. Sensors Design Based on Hybrid Gold-Silica Nanostructures. Biosens. Bioelectron. 2020, 153, 112054.
- Costanzo, H.; Gooch, J.; Frascione, N. Nanomaterials for Optical Biosensors in Forensic Analysis. Talanta 2023, 253, 123945.
- Aggett, P.; Aguilar, F.; Crebelli, R.; Dusemund, B.; Filipič, M.; Frutos, M.J.; Galtier, P.; Gott, D.; Gundert-Remy, U.; Kuhnle, G.G.; et al. Re-evaluation of Silicon Dioxide (E 551) as a Food Additive. EFS2 2018, 16, e05088.
- Şen Karaman, D.; Pamukçu, A.; Karakaplan, M.B.; Kocaoglu, O.; Rosenholm, J.M. Recent Advances in the Use of Mesoporous Silica Nanoparticles for the Diagnosis of Bacterial Infections. IJN 2021, 16, 6575–6591.
- Wen, L.; Qiu, L.; Wu, Y.; Hu, X.; Zhang, X. Aptamer-Modified Semiconductor Quantum Dots for Biosensing Applications. Sensors 2017, 17, 1736.
- Sun, H.; Zhou, P.; Su, B. Electrochemiluminescence of Semiconductor Quantum Dots and Its Biosensing Applications: A Comprehensive Review. Biosensors 2023, 13, 708.
- Ma, F.; Li, C.; Zhang, C. Development of Quantum Dot-Based Biosensors: Principles and Applications. J. Mater. Chem. B 2018, 6, 6173–6190.
- Pourmadadi, M.; Rahmani, E.; Rajabzadeh-Khosroshahi, M.; Samadi, A.; Behzadmehr, R.; Rahdar, A.; Ferreira, L.F.R. Properties and Application of Carbon Quantum Dots (CQDs) in Biosensors for Disease Detection: A Comprehensive Review. J. Drug Deliv. Sci. Technol. 2023, 80, 104156.
- Smith, R.P.; Barraza, I.; Quinn, R.J.; Fortoul, M.C. Chapter One—The Mechanisms and Cell Signaling Pathways of Programmed Cell Death in the Bacterial World. In Cell Death Regulation in Health and Disease—Part B; Spetz, J.K.E., Galluzzi, L., Eds.; International Review of Cell and Molecular Biology; Academic Press: Cambridge, MA, USA, 2020; Volume 352, pp. 1–53.
- Hao, L.; Xue, L.; Huang, F.; Cai, G.; Qi, W.; Zhang, M.; Han, Q.; Wang, Z.; Lin, J. A Microfluidic Biosensor Based on Magnetic Nanoparticle Separation, Quantum Dots Labeling and MnO2 Nanoflower Amplification for Rapid and Sensitive Detection of Salmonella Typhimurium. Micromachines 2020, 11, 281.





