Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ioannis Ilias | -- | 2329 | 2023-10-16 15:12:09 | | | |
| 2 | Rita Xu | Meta information modification | 2329 | 2023-10-17 03:30:45 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Milionis, C.; Ilias, I.; Tselebis, A.; Pachi, A. Vaccination Hesitancy. Encyclopedia. Available online: https://encyclopedia.pub/entry/50361 (accessed on 07 February 2026).
Milionis C, Ilias I, Tselebis A, Pachi A. Vaccination Hesitancy. Encyclopedia. Available at: https://encyclopedia.pub/entry/50361. Accessed February 07, 2026.
Milionis, Charalampos, Ioannis Ilias, Athanasios Tselebis, Argyro Pachi. "Vaccination Hesitancy" Encyclopedia, https://encyclopedia.pub/entry/50361 (accessed February 07, 2026).
Milionis, C., Ilias, I., Tselebis, A., & Pachi, A. (2023, October 16). Vaccination Hesitancy. In Encyclopedia. https://encyclopedia.pub/entry/50361
Milionis, Charalampos, et al. "Vaccination Hesitancy." Encyclopedia. Web. 16 October, 2023.
Copy Citation
Vaccines are an important tool of preventive medicine. Although organized vaccination programs have saved large populations from serious infectious diseases, there is a considerable part of the population who oppose vaccinations. In particular, anti-vaccination perceptions, among travelers to countries with endemic diseases, are a major public health concern.
vaccines
vaccination refusal
anti-vaccination movement
1. The Content of Vaccine Hesitancy
Despite the achievements of vaccinations in protecting public health by saving countless people from diseases and disabilities, the phenomenon of individuals questioning the need for, and the safety of vaccines, has become increasingly common around the globe over the past years [1][2]. People find data about vaccinations from sources such as the media, social media, and in websites; some of them are rife with anti-vaccine views [3][4]. Although the media are often a valuable tool in informing the public about the benefits of vaccines, sometimes they offer a place for uncritical expression of anti-vaccination ideology. These attitudes result in emerging challenges for the health care community in its effort to fight against anti-vaccination perceptions and to underline the medical importance of vaccines to the general public. The goal of health professionals and health systems is to maintain high vaccination rates among the population despite the reservations of some people towards vaccines [5].
Delays in accepting or refusals to accept vaccines pose a threat to the success of vaccination programs because their efficacy largely relies on high uptake. Indeed, there is a direct impact of the refusal of vaccinations on the incidence of the respective diseases. States and communities with a higher prevalence of vaccine exemptions are more susceptible to outbreaks of vaccine-preventable diseases such as measles and pertussis [6][7]. Moreover, the avoidance of childhood vaccinations due to parental hesitancy is associated with increased morbidity and death among children [8][9]. Unfortunately, health professionals are obliged to carry a heavier occupational burden when encountering individuals with reservations towards vaccinations [10][11].
The economic consequences of declining vaccination coverage on the cost of health care are potentially onerous. Even a modest reduction in the rate of a recommended vaccination could result in a multifold increase in the incidence of the respective disease, with a significant extra cost in treating these patients [12]. Depending on the type of health care funding, any rise in the relevant expenditure will burden the state budget, social insurance contributions, or premiums and out-of-pocket payments (in publicly funded, social-security-based, and private systems, respectively) [13]. For all the above reasons, vaccination hesitancy represents a public health problem from both a medical and a social point of view.
There are various reasons for the increasing prevalence of vaccine hesitancy. Most of the research has been conducted among people hesitant about pediatric vaccinations. Parental concerns about vaccinations may derive from fears of the potential deleterious health effects of vaccines, which may allegedly compromise their safety [14]. In these cases, the novelty of a vaccine can be an additional inhibiting factor for its acceptance [15]. Over the years, there have been several myths that contributed to parental skepticism. Rumors about a link between hepatitis B immunization and the occurrence of multiple sclerosis even led to the temporary suspension of certain school-based vaccine programs in the past, but they were categorically disproven afterwards [16]. The association of vaccines with autism has been extensively investigated and has conclusively been shown to be non-existent [17].
Nowadays, there is also a growing popular interest in a so-called ‘natural’ way of living, which has led many parents to exclude vaccinations as these are perceived as an artificial means of protection [18][19]. Moreover, trust in the relevant field of institutional medicine is decreasing, and thus, medical providers face difficulties convincing parents about the efficiency of vaccines [20][21]. Sometimes parents even tend to follow unproven or ineffective approaches as alternatives [22]. Other parental concerns include an aversion to the perceived intense vaccination schedule [23] and the combined form of vaccines [24].
Skepticism towards vaccination can be associated with a perceived self-control of one’s health and distrust in medical services and institutions. ‘Healthism’ is an attitude that prioritizes the protection of health as an individual duty. Nowadays, ‘healthist’ attitudes pervade our society and occasionally influence parenting behaviors. Unfortunately, they are often associated with opposition to vaccines. In this case, parents select their own norms of health for their children and refuse to accept immunization programs recommended by medical authorities or the state [25]. In fact, the ideology of healthism may reflect an elite’s commitment to live in a ‘risk society’ where scientific skepticism is a norm [26][27].
2. Vaccine Hesitancy among Travelers
Traveling is a unique condition compared with ordinary life in terms of health protection because of potential inherent hazards and the magnitude of their possible consequences. The avoidance or suboptimal uptake of recommended vaccinations by travelers is particularly problematic from a public health perspective because these individuals are often exposed to serious diseases in their travel destinations, and thus put their health in danger or increase the risk of spreading pathogens upon their return to their home country. Despite the importance of travel medicine vaccines, there has been little attention paid to vaccine hesitancy among travelers [28]. Unfortunately, the existing relevant literature consists only of a narrow range of studies and provides fragmented knowledge. The lack of data in this field is mainly addressed through the extrapolation of findings from studies in the general population.
General anti-vaccination sentiments are certainly present among those who are skeptical about immunization for travel purposes. However, some negative attitudes among travelers may be different from parental reservations about immunization of their children and other everyday vaccination concerns. After all, international traveling is often associated with exotic infectious pathogens and particular living circumstances [29], while travelers themselves may constitute a population of individuals with special personal characteristics and distinct needs and views of life [30]. Therefore, reluctance to accept travel vaccines should be studied independently of anti-vaccination stances of the general population in order to better understand the specific context and etiology and offer guidance for managing them.
Travelers’ rejections of vaccinations are multidimensional constructs. Common reasons for the refusal of the recommended vaccines include doubts about their necessity, concerns about their safety, and cost issues. Ignorance of the risks of tropical infectious disease, as well as a lower level of education, fuel the omission of travel vaccinations. Other secondary dissuading factors may include mistrust against pharmaceutical companies and health authorities, anticipated pain from the injection, uncertainty about previous received vaccinations, lack of available time, and negligence for seeking appropriate pre-travel advice. Sometimes, the refusal of vaccines may be due to the belief that the recommended guidance limits personal autonomy and violates the sense of liberty that is often inextricably related to the procedure of traveling and the identity of travelers [31]. However, the social processes that connect these factors with hesitancy against pre-travel immunization remain unclear. Furthermore, there is insufficient evidence to clearly demonstrate that healthism among higher social strata is a factor of vaccine hesitancy among travelers.
The phenomenon of vaccine hesitancy among travelers is influenced by the interplay between contextual conditions, individual characteristics, and specific factors related to vaccinations. Vaccine hesitancy is more prevalent in developed countries free of tropical diseases. Poor access to information or dissemination of inaccurate or incomplete data may construct an erroneous knowledge of immunobiological products. In this setting, exaggerated accusations of the side effects and disparagement of the effectiveness of vaccines find fertile ground, especially among people with a low educational level. Moreover, extreme cultural or religious motives may fuel reactions towards immunizations. Personality traits, political ideologies, idiosyncrasies, and the duration of travel are individual features that can affect the acceptance of the recommended vaccinations. Finally, difficulties in the accessibility of the necessary services and products, including incompatibility of working hours, long distance, excessive waiting time, and high cost, may foster indifference towards vaccines, while past failures of immunization programs might shake travelers’ confidence in vaccinations [32]. The interconnection of the various factors that generate vaccine hesitancy is presented in Figure 1.
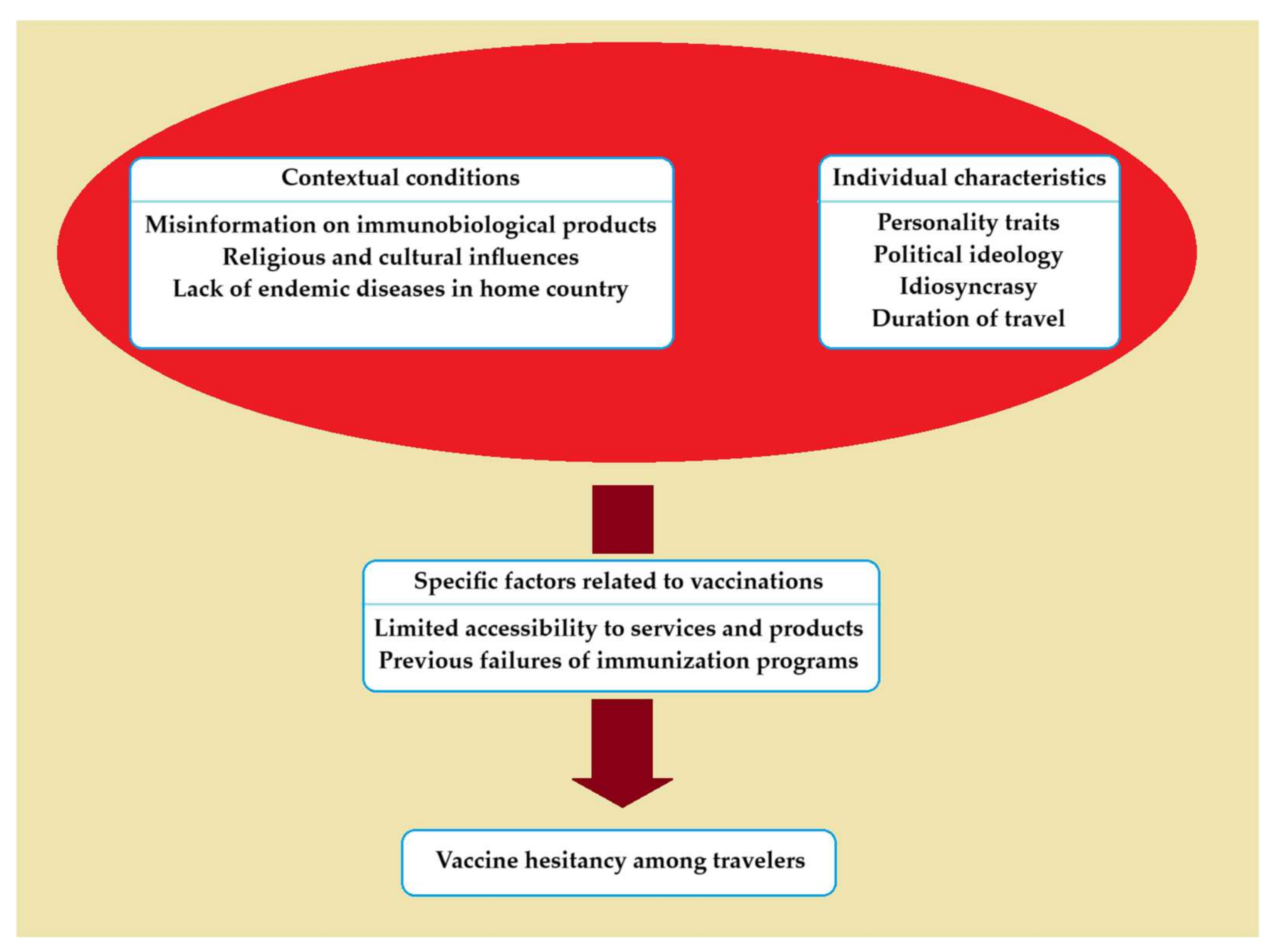
Figure 1. Causative factors associated with vaccine hesitancy among travelers.
3. Implications in Clinical Practice
According to the World Tourism Organization (UNWTO), there were more than 900 million individuals that traveled internationally in 2022 [33]. Although several travel restrictions were implemented to slow down the spread of the novel coronavirus during the pandemic, strong growth of international travel is expected over the next few years. Many locations of arrivals are places where endemic infectious diseases are relatively common. Therefore, the administration of the appropriate vaccines to travelers is important for minimizing the spread of vaccine-preventable disease in individuals and communities. Travel medicine consultation includes, among other things, the recommendation for vaccinations specific to the travel circumstances as well as for routine vaccinations necessary for the up-to-date compliance with the immunization schedule in each country.
A wide range of infectious diseases endanger the health of travelers in tropical destinations. The risk depends on the transportation means, geographical location, living conditions, individual lifestyle and activities, duration of stay, and climatic setting. Citizens of industrialized countries may be exposed to various causative infectious organisms during their stay in tropical locations. The type and extent of health consequences for individuals vary. Among long-term travelers, most health impairments include gastrointestinal and dermatological problems followed by febrile systemic infections [34]. Precautionary immunization against a number of vaccine-preventable diseases, such as yellow fever, typhoid, hepatitis A and B, meningococcal disease, and rabies, is a safe preventive measure against tropical infectious hazards. A personalized update of routine vaccines in case of missed doses is also important [35][36][37][38].
However, international traveling leads not only to an increase in individual health imperilment but also has a global impact. Infected travelers may import tropical pathogens into their community upon their return from abroad. If biological, social, and environmental conditions are met, pathogenic agents may massively or sporadically spread to the population in the new geographical area. For example, tuberculosis, measles, pertussis, diphtheria, and hepatitis B are easily carried by travelers and can disseminate in their home country. In contrast, pathogens that survive only under specific local conditions find it more difficult to thrive in the new environment. For example, yellow fever cannot appear in a geographic area unless competent mosquito vectors are present [39]. Thus, previously immunized travelers prevent the introduction of tropical diseases.
The rate of pre-travel vaccine uptake is regulated by two factors, which include the guidelines provided by health professionals (especially those specialized in travel medicine) and the willingness of travelers to accept vaccinations. Medical recommendations for travel vaccines must be individualized and based on a risk assessment determined by the details of the traveler’s destination, schedule and purpose of travel, season of travel, time before departure, medical history, and immunization status [40]. A traveler’s decision on whether to receive pre-travel vaccinations is determined by supporting or dissuading views of the necessity and safety of vaccines [41].
The use of vaccines (just as with other health products) has an important differentiation in comparison with the consumption of other non-medical goods because there is unequal knowledge between the supplier of the product (the pharmaceutical company) and the consumer (the patient). This means that the consumer/patient, due to a lack of expertise, is not entirely capable of knowing the necessity of receiving a vaccination and the consequences of his/her positive or negative decision. This gap in knowledge is filled with the doctor’s intervention. Specifically, the patient and the doctor are associated with a ‘principal and agent’ relationship [42] in which the doctor (agent) represents the patient (principal) and substitutes him/her in decision making. An essential prerequisite for this interdependence is the patient’s confidence in the doctor’s role and the increased responsibility of the doctor to protect the patient’s health. The doctor–patient relationship is based on the assumption that the medical profession has a unique technical competence, and it is devoted to the benefit of the sick [43].
Nevertheless, access to medical information has dramatically risen nowadays. Medical knowledge that was previously bound to specialized textbooks and journals, is now accessible to the public, especially through the internet. This has shifted the power from doctors as exclusive managers of a patient’s care to the patients themselves, which in turn has led to the need for shared decision making between patients and doctors. Although this condition is beneficial in general, the dissemination of inaccurate and misleading information found on the internet can also lead to negative consequences, such as avoiding necessary vaccinations [44]. The prevalence of anti-vaccination beliefs, the insufficient understanding of biological aspects of immunization, and the modern shift of concern from the greater good to individualism render travelers vulnerable to vaccine hesitancy [45]. Therefore, the need for protection of the patients’ interests by the doctors (or other health professionals) remains unaltered.
Personal attitudes towards vaccines flow primarily from individual characteristics, including awareness, personal beliefs, and past experiences. Vaccine acceptance (and refusal) is further influenced by the interrelation between contextual determinants (health policies, social norms, cultural influences, public health conditions) and organizational parameters (availability and quality of vaccination services, motivation of health staff, properties of vaccines). Nowadays, prevailing views in the media also play a significant role [46]. Unfortunately, occasional failures of past vaccination programs may hamper public acceptance of vaccines. Indeed, a lack of transparency about the safety of vaccinations or an incapacity to promptly recognize potential side effects of vaccines may produce a cascading effect on the decisions of individuals to avoid immunizations [47]. However, sporadic failures in vaccines’ effectiveness or misguided implementation policies cannot serve as a pillar for vaccine hesitancy.
As the COVID-19 pandemic is gradually diminishing, it is important to inform the public about the achievements of vaccination and acknowledge remaining uncertainties. For this purpose, pharmaceutical companies and scientific organizations must be straightforward and sincere about their research data on the safety and efficacy of vaccines. Moreover, the medical community is obliged to investigate, document, and report the adverse effects of immunization. Finally, governments should be transparent about their decisions on implementing vaccination programs. The provision of accurate information to the public in a comprehensible manner is the optimal way to arrest the spread of misconceptions and thereby fight vaccine hesitancy [48].
References
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF joint reporting form data-2015–2017. Vaccine 2018, 36, 3861–3867.
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159.
- Broadbent, J.J. Vaccine hesitancy: Misinformation on social media. BMJ 2019, 366, l4457.
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11.
- Tafuri, S.; Gallone, M.S.; Cappelli, M.G.; Martinelli, D.; Prato, R.; Germinario, C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014, 32, 4860–4865.
- Piccirilli, G.; Lazzarotto, T.; Chiereghin, A.; Serra, L.; Gabrielli, L.; Lanari, M. Spotlight on measles in Italy: Why outbreaks of a vaccine-preventable infection continue in the 21st century. Expert. Rev. Anti Infect. Ther. 2015, 13, 355–362.
- Phadke, V.K.; Bednarczyk, R.A.; Salmon, D.A.; Omer, S.B. Association Between Vaccine Refusal and Vaccine-Preventable Diseases in the United States: A Review of Measles and Pertussis. JAMA 2016, 315, 1149–1158.
- Kubin, L. Is There a Resurgence of Vaccine Preventable Diseases in the U.S.? J. Pediatr. Nurs. 2019, 44, 115–118.
- McGovern, M.E.; Canning, D. Vaccination and All-Cause Child Mortality From 1985 to 2011: Global Evidence from the Demographic and Health Surveys. Am. J. Epidemiol. 2015, 182, 791–798.
- Kempe, A.; Daley, M.F.; McCauley, M.M.; Crane, L.A.; Suh, C.A.; Kennedy, A.M.; Basket, M.M.; Stokley, S.K.; Dong, F.; Babbel, C.I.; et al. Prevalence of Parental Concerns About Childhood Vaccines: The Experience of Primary Care Physicians. Am. J. Prev. Med. 2011, 40, 548–555.
- Leib, S.; Liberatos, P.; Edwards, K. Pediatricians’ Experience with and Response to Parental Vaccine Safety Concerns and Vaccine Refusals: A Survey of Connecticut Pediatricians. Public Health Rep. 2011, 126 (Suppl. 2), 13–23.
- Lo, N.C.; Hotez, P.J. Public Health and Economic Consequences of Vaccine Hesitancy for Measles in the United States. JAMA Pediatr. 2017, 171, 887–892.
- Milionis, C. Provision of healthcare in the context of financial crisis: Approaches to the Greek health system and international implications. Nurs. Philos. 2013, 14, 17–27.
- Nicoli, F.; Appay, V. Immunological considerations regarding parental concerns on pediatric immunizations. Vaccine 2017, 35, 3012–3019.
- Szilagyi, P.G.; Albertin, C.; Gurfinkel, D.; Saville, A.W.; Vangala, S.; Rice, J.; Helmkamp, L.; Zimet, G.D.; Valderrama, R.; Breck, A.; et al. Prevalence and Characteristics of HPV Vaccine Hesitancy Among Parents of Adolescents Across the US. Vaccine 2020, 38, 6027–6037.
- Sestili, C.; Grazina, I.; La Torre, G. HBV vaccine and risk of developing multiple sclerosis: A systematic review and meta-analysis. Hum. Vaccin. Immunother. 2021, 17, 2273–2278.
- Gabis, L.V.; Attia, O.L.; Goldman, M.; Barak, N.; Tefera, P.; Shefer, S.; Shaham, M.; Lerman-Sagie, T. The myth of vaccination and autism spectrum. Eur. J. Paediatr. Neurol. 2022, 36, 151–158.
- Gross, K.; Hartmann, K.; Zemp, E.; Merten, S. ‘I know it has worked for millions of years’: The role of the ‘natural’ in parental reasoning against child immunization in a qualitative study in Switzerland. BMC Public Health 2015, 15, 373.
- Dubé, E.; Vivion, M.; Sauvageau, C.; Gagneur, A.; Gagnon, R.; Guay, M. “Nature Does Things Well, Why Should We Interfere?”: Vaccine Hesitancy Among Mothers. Qual. Health Res. 2016, 26, 411–425.
- Ward, P.R.; Attwell, K.; Meyer, S.B.; Rokkas, P.; Leask, J. Understanding the perceived logic of care by vaccine-hesitant and vaccine-refusing parents: A qualitative study in Australia. PLoS ONE 2017, 12, e0185955.
- Goldenberg, M.J. Public Misunderstanding of Science? Reframing the Problem of Vaccine Hesitancy. Perspect. Sci. 2016, 24, 552–581.
- Jacobson, R.M.; St Sauver, J.L.; Griffin, J.M.; MacLaughlin, K.L.; Finney Rutten, L.J. How health care providers should address vaccine hesitancy in the clinical setting: Evidence for presumptive language in making a strong recommendation. Hum. Vaccin. Immunother. 2020, 16, 2131–2135.
- Wheeler, M.; Buttenheim, A.M. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum. Vaccin. Immunother. 2013, 9, 1782–1789.
- Hulsey, E.; Bland, T. Immune overload: Parental attitudes toward combination and single antigen vaccines. Vaccine 2015, 33, 2546–2550.
- Reich, J.A. Neoliberal Mothering and Vaccine Refusal: Imagined Gated Communities and the Privilege of Choice. Gend. Soc. 2014, 28, 679–704.
- Kirbiš, A. The Impact of Socioeconomic Status, Perceived Threat and Healthism on Vaccine Hesitancy. Sustainability 2023, 15, 6107.
- Peretti-Watel, P.; Raude, J.; Sagaon-Teyssier, L.; Constant, A.; Verger, P.; Beck, F. Attitudes toward vaccination and the H1N1 vaccine: Poor people’s unfounded fears or legitimate concerns of the elite? Soc. Sci. Med. 2014, 109, 10–18.
- Taddio, A.; MacDonald, N. Addressing vaccine hesitancy in travellers: The CARDTM system. J. Travel Med. 2019, 26, taz056.
- Nicolaï, H.; Verhasselt, Y. Health and tropical geography. Belgeo 2000, 1-2-3-4, 103–114.
- Zhu, O.Y.; Grün, B.; Dolnicar, S. Tourism and vaccine hesitancy. Ann. Tour. Res. 2022, 92, 103320.
- Adongo, C.A.; Amenumey, E.K.; Kumi-Kyereme, A.; Dubé, E. Beyond fragmentary: A proposed measure for travel vaccination concerns. Tour. Manag. 2021, 83, 104180.
- Lopes, V.D.S.; Souza, P.C.; Garcia, É.M.; Lima, J.C. Yellow fever vaccine hesitancy and its relationship with contextual, individual, or group influences and vaccine-specific issues: A scoping review. Cien. Saude Colet. 2023, 28, 1717–1727.
- World Tourism Organization (UNWTO). International tourism recovered 63% of pre-pandemic levels in 2022, with Europe and Middle East in the lead. World Tour. Barom. 2023, 21, 1–40.
- Kitro, A.; Ngamprasertchai, T.; Srithanaviboonchai, K. Infectious diseases and predominant travel-related syndromes among long-term expatriates living in low-and middle- income countries: A scoping review. Trop. Dis. Travel Med. Vaccines 2022, 8, 11.
- Rapose, A. Travel to Tropical Countries: A Review of Travel-Related Infectious Diseases. Trop. Med. Surg. 2013, 1, 1000128.
- Toovey, S.; Moerman, F.; van Gompel, A. Special Infectious Disease Risks of Expatriates and Long-Term Travelers in Tropical Countries. Part II: Infections Other Than Malaria. J. Travel Med. 2007, 14, 50–60.
- Roupa, Z.; Noula, M.; Farazi, E.; Stylianides, A.; Papaneophytou, C. Vaccination Coverage and Awareness of Hepatitis B Virus Among Healthcare Students at a University in Cyprus. Mater. Sociomed. 2019, 31, 190–196.
- Roupa, Z.; Zikos, D.; Vasilopoulos, A.; Diomidous, M. Common health risks, required precautions of travelers and their customs towards the use of travel medicine services. Mater. Sociomed. 2012, 24, 131–134.
- Wilson, M.E. Travel and the emergence of infectious diseases. Emerg. Infect. Dis. 1995, 1, 39–46.
- Virk, A. Medical Advice for International Travelers. Mayo Clin. Proc. 2001, 76, 831–840.
- Crockett, M.; Keystone, J. “I Hate Needles” and Other Factors Impacting on Travel Vaccine Uptake. J. Travel Med. 2005, 12 (Suppl. 1), S41–S46.
- Weinstein, M.C. Should physicians be gatekeepers of medical resources? J. Med. Ethics 2001, 27, 268–274.
- Relman, A.S. Cost Control, Doctors’ Ethics, And Patient Care. Issues Sci. Technol. 1985, 1, 103–111.
- Hussain, A.; Ali, S.; Ahmed, M.; Hussain, S. The Anti-vaccination Movement: A Regression in Modern Medicine. Cureus 2018, 10, e2919.
- Bauer, I.L. Travel vaccination examined through the tourism lens. J. Travel Med. 2021, 28, taab142.
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert. Rev. Vaccines 2015, 14, 99–117.
- Fatima, K.; Syed, N.I. Dengvaxia controversy: Impact on vaccine hesitancy. J. Glob. Health 2018, 8, 010312.
- Machingaidze, S.; Wiysonge, C.S. Understanding covid-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339.
More
Information
Subjects:
Medicine, General & Internal
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
591
Revisions:
2 times
(View History)
Update Date:
17 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




