Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Bruno Špiljak | -- | 2133 | 2023-10-04 00:43:41 | | | |
| 2 | Jessie Wu | Meta information modification | 2133 | 2023-10-07 04:06:25 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Japundžić, I.; Bembić, M.; Špiljak, B.; Parać, E.; Macan, J.; Lugović-Mihić, L. Work-Related Hand Eczema in Healthcare Workers. Encyclopedia. Available online: https://encyclopedia.pub/entry/49827 (accessed on 07 February 2026).
Japundžić I, Bembić M, Špiljak B, Parać E, Macan J, Lugović-Mihić L. Work-Related Hand Eczema in Healthcare Workers. Encyclopedia. Available at: https://encyclopedia.pub/entry/49827. Accessed February 07, 2026.
Japundžić, Iva, Massimo Bembić, Bruno Špiljak, Ena Parać, Jelena Macan, Liborija Lugović-Mihić. "Work-Related Hand Eczema in Healthcare Workers" Encyclopedia, https://encyclopedia.pub/entry/49827 (accessed February 07, 2026).
Japundžić, I., Bembić, M., Špiljak, B., Parać, E., Macan, J., & Lugović-Mihić, L. (2023, October 03). Work-Related Hand Eczema in Healthcare Workers. In Encyclopedia. https://encyclopedia.pub/entry/49827
Japundžić, Iva, et al. "Work-Related Hand Eczema in Healthcare Workers." Encyclopedia. Web. 03 October, 2023.
Copy Citation
Work-related skin diseases are among the most common work-related diseases, ranking second in frequency after musculoskeletal diseases. The majority of work-related skin diseases (80–95%) are contact dermatitis, which can be both irritant and allergic in nature. Lesions are most commonly described as hand eczema and occur as a result of contact with various substances (irritants and allergens) in the workplace. The term “eczema” is generally used to describe a group of skin lesions in which the skin is itchy, dry, and inflamed. However, the term eczema usually involves a non-specific clinical picture but is commonly used in real-life and medical settings when working with patients.
contact dermatitis
hand eczema
medical doctors
dentists
etiology
allergy
allergens
patch test
skin
1. Key Features and Etiopathogenesis of Work-Related Hand Eczema
Hand eczema is predominantly the consequence/result of the skin coming into contact with different substances. It mainly manifests as contact dermatitis, including irritant contact dermatitis and allergic contact dermatitis, for which the pathogeneses are different. Irritant contact dermatitis and allergic contact dermatitis are relatively frequent dermatoses, with irritant contact dermatitis being more common than allergic contact dermatitis [1][2]. Recognizing and diagnosing them requires a thorough patient history and, crucially, a detailed clinical picture. As the clinical picture is commonly similar in both, patch tests can differentiate the two dermatoses (a positive patch test, along with a history of allergen sensitivity, indicates allergic contact dermatitis) (Figure 1). Sometimes histology may be helpful (Figure 2). Histologically, prominent features of acute irritant contact dermatitis are spongiosis, irregular acanthosis, the dilation of capillaries in the subepidermal dermis, and perivascular infiltration of neutrophils and lymphocytes in the dermis. A diagnosis of chronic irritant contact dermatitis is made based on the history, clinical picture, and negative patch test results, as histological findings are often non-specific. A diagnosis of acute allergic contact dermatitis is also made based on a patient’s history and clinical picture, though with a positive result to a patch test (epicutaneous) using a standard series of allergens or “target allergens”. Histologically, in allergic contact dermatitis, lymphocytic perivascular infiltrate, edema of the dermis, and epidermal spongiosis and exocytosis are observed. Chronic allergic contact dermatitis is also diagnosed based on a detailed clinical picture and patient history, and it is confirmed with a positive patch test result.

Figure 1. Clinical finding of work-related hand eczema.
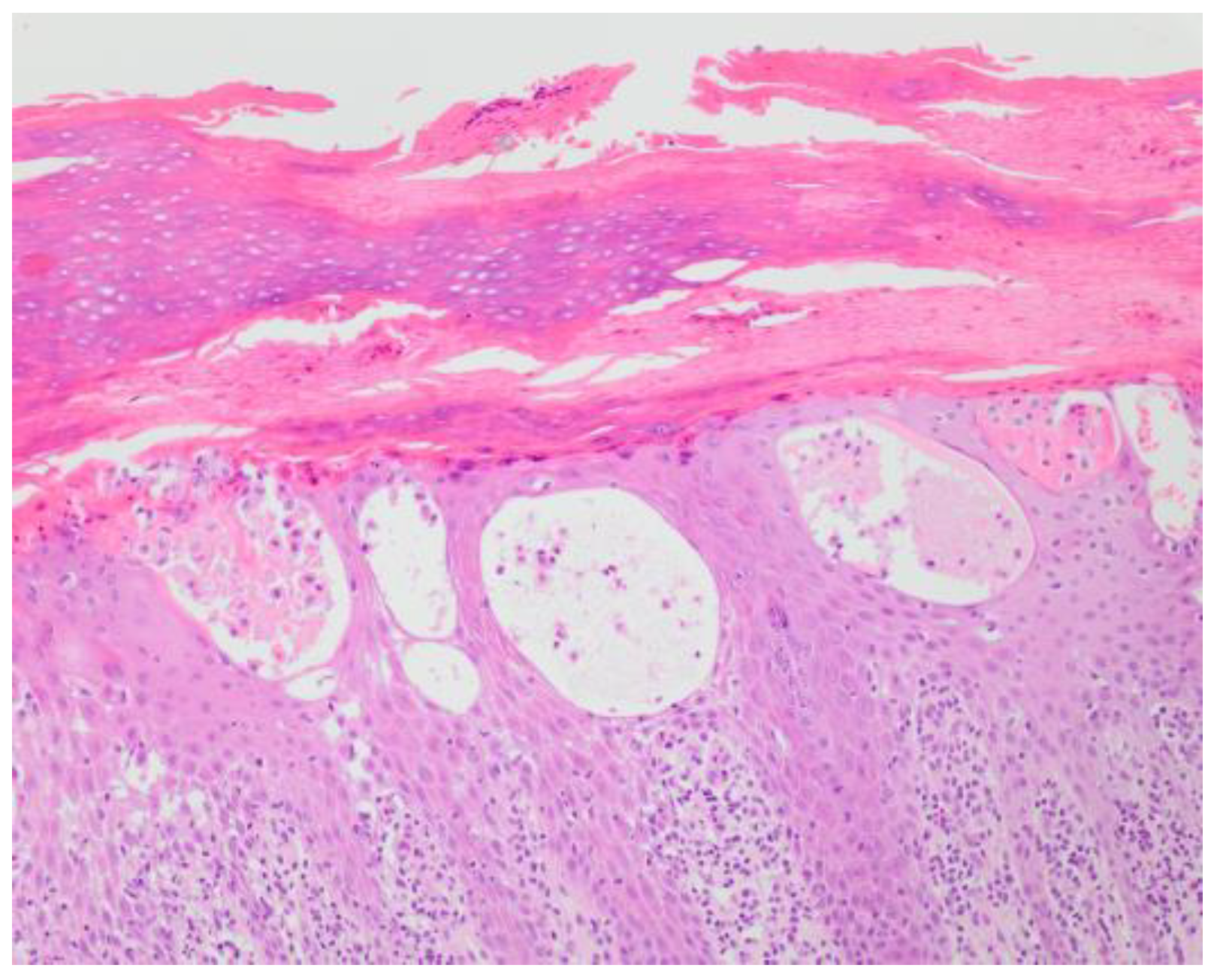
Figure 2. Histological finding of acute allergic contact dermatitis.
1.1. Irritant Contact Dermatitis
Previously, it was believed that the development of irritant contact dermatitis did not involve an immune response; however, it is now acknowledged that the immune system plays a crucial role in the onset of irritant contact dermatitis [3]. Irritation can occur either by damaging the cells in the outermost layer of the skin (epidermal cells) [4], disrupting the epidermal barrier, or a combination of both processes [5]. The disruption of the epithelial barrier leads to increased permeability to irritants [6]. Keratinocytes, which are responsible for converting external stimuli into the secretion of cytokines, adhesion molecules, and chemotactic factors act as “signal transducers” in initiating cutaneous inflammation [7]. When keratinocytes are damaged, primary cytokines, such as interleukin-1 alpha (IL-1α), IL-1β, and tumor necrosis factor-alpha (TNF-α), are upregulated [8], which stimulates the proliferation of keratinocytes and the production of lipids [9], contributing to the restoration of the epidermal barrier. Subsequently, additional cytokines, including IL-6, IL-8, and granulocyte-macrophage colony-stimulating factor (GM-CSF), are secreted, activating Langerhans cells, dermal dendritic cells, and endothelial cells [6], which further recruit inflammatory cells to the site of chemical trauma [10]. The adhesion molecule intercellular adhesion molecule 1 (ICAM1) is upregulated on endothelial cells and fibroblasts in the skin, leading to the secretion of additional chemokines, such as C-X-C motif chemokine ligand 8 (CXCL 8), C-C motif chemokine ligand 20 (CCL 20), and interferon gamma (IFN -γ) [11]. Also, C-C motif Chemokine Ligand 21 (CCL21), a chemokine that facilitates the migration of naive T lymphocytes, is upregulated in irritant contact dermatitis [8][12]. T lymphocytes recruited to irritated skin often express the cutaneous lymphocyte-associated antigen (CLA antigen), which plays a significant role in the migration of T lymphocytes across endothelial cells. Irritants can also activate pattern recognition receptors, such as toll-like receptors (TLRs) and nucleotide oligomerization domain-like (NOD-like) receptors, triggering the activation of the innate immune response through the inflammasome and Nuclear factor kappa-light-chain-enhancer of activated B cells’ (NFκB) pathways [6][13][14]. Increasing evidence suggests that oxidative stress and the generation of reactive oxygen species contribute to the pathogenesis of irritant contact dermatitis [15][16]. Concerning the relationship between contact dermatitis and antioxidants, it is possible that most skin irritants and allergens keep their inactive redox status, though some of them can be a source of free radicals and produce reactive oxygen species (ROS) and/or reactive nitrogen species (RNS) [15][17]. In epidermal keratinocytes, some substances may generate free radicals. For example, in keratinocytes, organic hydroperoxides and organic peroxides generate free radicals. Also, in the presence of metals such as chromium and nickel, the levels of free radical formations increase. It has been shown that peroxides inactivate antioxidants in keratinocytes. Also, in the lesions of both irritant contact dermatitis and allergic contact dermatitis, increased levels of iNOS protein expression have been immunohistochemically shown. In addition, the exacerbation of skin inflammation is accompanied by excessive production of ROSs, like superoxide (O2+) and hydroxyl radical (OH+) [18]. It has been hypothesized that targeting oxidative stress could be beneficial in treating irritant contact dermatitis, and clinical studies have shown the therapeutic benefits of antioxidants [16]. According to research data, emollient cream, as well as a combined topical glucocorticoid and emollient cream therapy, reduced glutathione redox status [18].
1.2. Allergic Contact Dermatitis
Allergic contact dermatitis occurs due to skin contact with an allergen to which the person is sensitized and a subsequent T-cell-mediated response (type 4 hypersensitivity reaction) [19][20][21]. The initial severity of the condition plays a crucial role in determining its duration and the effectiveness of treatment and ultimately affects the patient’s overall well-being. This disease has two phases: sensitization to the antigen and the response to re-exposure (elicitation). The pathophysiology of allergic contact dermatitis initiates when the allergen comes into contact with the skin. The allergen permeates the stratum corneum and is taken up by Langerhans cells [22][23]. These Langerhans cells then migrate towards nearby lymph nodes, where they process the antigens and present them on their surface. Adjacent T lymphocytes come into contact with the presented antigens, leading to the creation of antigen-specific T lymphocytes through clonal expansion and cytokine-induced proliferation. These newly formed lymphocytes can travel through the bloodstream and reach the epidermis, marking the sensitization phase of allergic contact dermatitis. The elicitation phase occurs upon re-exposure to the antigen. Langerhans cells, which still contain the antigen, interact with the antigen-specific T lymphocytes, triggering a cytokine-induced proliferation process. This localized inflammatory response leads to the characteristic symptoms of allergic contact dermatitis. According to experimental models, acute damage to the skin’s epidermal barrier after exposure to allergens stimulates keratinocytes and antigen-presenting cells (through toll-like receptor activation) to release cytokines IL-1, IL-6 and TNF-α, which are crucial for pro-inflammatory and chemotactic effects on immune cells, initially directing them towards the regional lymph nodes and, subsequently, towards the site of damage or skin contact with the allergen [24][25]. It is important to note that although small molecular weight substances (haptens) can penetrate intact, undamaged skin, the maintained epidermal barrier can partially prevent sensitization to specific allergens. In addition to keratinocytes and antigen-presenting cells, other immune cells play roles in both phases of allergic contact dermatitis. For example, neutrophils and mast cells, activated via local inflammatory reactions, participate in the secretion of pro-inflammatory cytokines (such as IL-6 and TNF-α) [25]. Mast cells, upon contact with allergens, can release various cytokines and histamine, thereby influencing the endothelium and recruiting a greater number of immune cells to the site of allergen contact [19][25]. Antigen presentation of allergens to lymphocytes in the regional lymph nodes also leads to the development of specific regulatory T cells (Tregs), which, through the secretion of suppressive cytokines, reduce and halt the contact hypersensitivity reaction [25]. Their role is to restore immune balance and interrupt excessive contact hypersensitivity reactions to allergens.
2. Skin Care in Healthcare Professionals
Skin health is a critical aspect of overall well-being, especially for healthcare professionals, who are often exposed to a variety of potential skin irritants. The skin barrier, which is the uppermost layer of the skin, serves as a physical and functional protection system. It is composed of skin cells and specialized immune system cells that work together to recognize and keep out intruding organisms and substances. Certain conditions, such as eczema, can weaken this barrier. This issue leads to a cycle of uncomfortable dryness, irritation, and inflammation. These symptoms, in turn, can contribute to further degradation of the skin barrier, worsening symptoms, and a vicious cycle of skin damage [26]. Furthermore, individuals with pre-existing skin barrier dysfunction, such as atopic dermatitis, may experience magnified symptoms due to increased hand hygiene practices [27]. Healthcare workers, in particular, experience frequent hand sanitizer use and a higher incidence of irritant contact dermatitis. This issue may explain their significantly higher transepidermal water loss (TEWL, a measure of the skin’s barrier function), as they already have a compromised skin barrier. Despite the use of emollients, TEWL increased, indicating that even with the application of creams and lotions, skin barrier function was not fully restored [27]. Healthcare professionals are advised to follow a few key steps to maintain and improve skin health. Moisturizing is crucial because it improves the barrier function of the skin. For more severe dryness, experts recommend moisturizing after short “soaks” in a lukewarm bath. Thick ointments or creams may be preferable to lotions to prevent skin from drying out while also protecting it from irritants [26]. Minimizing exposure to allergens, irritants, and typical triggers is another important step. Common eczema triggers include dry skin, dust, pet dander, pollen, metals like nickel, cigarette smoke, soaps and household cleaners, fragrances, fabrics like wool and polyester, certain chemicals, dry air, and stress. Avoiding these triggers can help to strengthen the skin barrier and prevent further degradation [28]. A soap-free cleanser is recommended, since synthetic detergents have a neutral or slightly acidic pH, making them less irritating to the skin [29]. Soap-free cleansers also typically contain a relatively high amount of free fatty acids, which help moisturize the skin and prevent hand irritation and dryness. As an alternative to detergents, it is advisable to use alcohol-based hand sanitizers that include moisturizers and avoid common allergens [30]. Barrier creams are formulated to create a protective layer on the skin, aiming to prevent the penetration of irritants. While they are believed to play a role in preventing irritant contact dermatitis, they are generally recommended for use with low-grade irritants [31]. However, a recent Cochrane review indicated that using barrier creams alone may have a minor protective effect. Nonetheless, the evidence was considered low quality and not clinically significant [32]. While topical corticosteroids are commonly used for the treatment of irritant contact dermatitis, their effectiveness is disputed, with some studies suggesting they may reduce skin barrier function, and although they may be beneficial for some chronic hyperkeratotic lesions, prolonged use can lead to skin thinning and increased sensitivity, necessitating systemic corticosteroids during severe episodes [33][34][35]. Topical calcineurin inhibitors are topical immunomodulators that offer a safe alternative to corticosteroids. However, there have been suggestions of a potential association between topical calcineurin inhibitors and skin cancer and lymphoma, though the evidence is not strong [36][37]. In addition, for systemic treatments, alitretinoin has been found to be effective in treating chronic hand eczema, with 43.2% of patients diagnosed with irritant contact dermatitis showing positive results in one study [38]. In cases where other first- or second-line treatments have failed, oral immunomodulators may be necessary for chronic irritation. Cyclosporine has shown beneficial effects in treating chronic hand eczema [35], but its use should be cautiously due to associated side effects. Limited evidence has indicated that dupilumab, a monoclonal antibody treatment approved for treating atopic dermatitis, may be effective in treating chronic recalcitrant hyperkeratotic irritant contact dermatitis [39] and non-atopic hyperkeratotic hand eczema [40]. However, further studies are needed to determine the potential use of dupilumab as a therapeutic agent in irritant contact dermatitis. In terms of advancements in preventing irritant contact dermatitis, recent research on human subjects has shown the effectiveness of inflammasome-targeted therapies, such as topical disulfiram. This treatment has demonstrated inhibitory effects on irritant contact dermatitis, likely due to a reduction in the inflammatory cytokine IL-18 [41]. This development presents a novel approach to the prevention of irritant contact dermatitis. Despite these measures, healthcare workers continue to experience skin issues. This issue highlights the need for further research into the effects of specific emollients and the development of more effective skincare routines. It also underscores the importance of occupational health professionals regularly surveying employees about the acceptance of hand cleansing and hand care products and adjusting them to prevent work-related hand eczema. The goal is to maintain the integrity of the skin barrier, prevent skin diseases, and ensure the well-being of healthcare professionals.
References
- Sonsmann, F.; Beaumann, A.; Wilke, A.; John, S.M.; Sulfhorst, B. Occupational Skin Diseases in the Hairdressing Trade–Medical Reference Document. Available online: https://www.safehair.eu/en/trainer/facts-to-know/medical-reference-document/ (accessed on 26 June 2023).
- Novak-Bilić, G.; Vučić, M.; Japundžić, I.; Meštrović-Štefekov, J.; Stanić-Duktaj, S.; Lugović-Mihić, L. Irritant and allergic contact dermatitis-skin lesion characteristics. Acta Clin.Croat. 2018, 57, 713–720.
- Levin, C.; Maibach, H. Irritant contact dermatitis: Is there an immunological component? Int. Immunopharmacol. 2002, 2, 183–189.
- Angelova-Fischer, I. Irritants and skin barrier function. Curr. Probl. Dermatol. 2016, 49, 80–89.
- Welss, T.; Basketter, D.A.; Schroder, K.R. In vitro skin irritation: Facts and future. State of the art review of mechanisms and models. Toxicol. Vitr. 2004, 18, 231–243.
- Bains, S.; Nash, P.; Fonacier, L. Irritant contact dermatitis. Clin. Rev. Allergy Immunol. 2019, 56, 99–109.
- Gittler, J.K.; Krueger, J.G.; Guttman-Yassky, E. Atopic dermatitis results in intrinsic barrier and immune abnormalities: Implications for contact dermatitis. J. Allergy Clin. Immunol. 2013, 131, 300–313.
- Spiekstra, S.W.; Toebak, M.J.; Sampat-Sardjoepersad, S.; van Beek, P.J.; Boorsma, D.M.; Stoof, T.J.; von Blomberg, B.M.; Scheper, R.J.; Bruynzeel, D.P.; Rustemeyer, T.; et al. Induction of cytokine (interleukin-1alpha and tumor necrosis factor-alpha) and chemokine (CCL20, CCL27, and CXCL8) alarm signals after allergen and irritant exposure. Exp. Dermatol. 2005, 14, 109–116.
- Feingold, K.; Schmuth, M.; Elias, P. The regulation of permeability barrier homeostasis. J. Investig. Dermatol. 2007, 127, 1547–1576.
- Corsini, E.; Galli, C. Epidermal cytokines in experimental contact dermatitis. Toxicology 2000, 142, 203–211.
- Lee, H.; Stieger, M.; Yawalkar, N.; Kakeda, M. Cytokines and chemokines in irritant contact dermatitis. Mediat. Inflamm. 2013, 2013, 916497.
- Eberhand, Y.; Ortiz, S.; Ruiz, L.A.; Kuznitzky, R.; Serra, H. Up-regulation of the chemokine CCL21 in the skin of subjects exposed to irritants. BMC Immunol. 2004, 26, 7.
- Soler, D.; Humphreys, T.L.; Spinola, S.M.; Campbell, J.J. CCR4 versus CCR10 in human cutaneous TH lymphocyte trafficking. Blood 2003, 101, 1677–1682.
- Ale, I.; Maibach, H. Irritant contact dermatitis. Rev. Environ. Health 2014, 29, 195–206.
- Nakai, K.; Yoneda, K.; Kubota, Y. Oxidative stress in allergic and irritant dermatitis: From basic research to clinical management. Recent. Pat. Inflamm. Allergy Drug Discov. 2012, 6, 202–209.
- Wagemaker, T.A.L.; Maia Campos, P.; Shimizu, K.; Kyotani, D.; Yoshida, D. Antioxidant-based topical formulations influence on the inflammatory response of Japanese skin: A clinical study using non-invasive techniques. Eur. J. Pharm. Biopharm. 2017, 117, 195–202.
- Fuchs, J.; Zollner, T.M.; Kaufmann, R.; Podda, M. Redox-modulated pathways in inflammatory skin diseases. Free Radic. Biol. Med. 2001, 30, 337–353.
- Kaur, S.; Eisen, M.; Zilmer, M.; Rehema, A.; Kullisaar, T.; Vihalemm, T.; Zilmer, K. Emollient cream and topical glucocorticoid treatment of chronic hand dermatitis: Influence on oxidative stress status of the skin. J. Dermatol. Sci. 2003, 33, 127–129.
- Nixon, R.L.; Mowad, C.M.; Marks, J.G., Jr. Allergic Contact Dermatitis. In Dermatology, 4th ed.; Bolognia, J.L., Schaffer, J.V., Cerroni, L., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 242–261.
- Aquino, M.; Rosner, G. Systemic Contact Dermatitis. Clin. Rev. Allergy Immunol. 2019, 56, 9–18.
- Buse, A.S.; Wilke, A.; John, S.M.; Hansen, A. Illness Perceptions of Occupational Hand Eczema in German Patients Based on the Common-Sense Model of Self-Regulation: A Qualitative Study. PLoS ONE 2023, 18, e0285791.
- Vocanson, M.; Hennino, A.; Rozières, A.; Poyet, G.; Nicolas, J.F. Effector and regulatory mechanisms in allergic contact dermatitis. Allergy 2009, 64, 1699–1714.
- Bock, S.; Said, A.; Müller, G.; Schäfer-Korting, M.; Zoschke, C.; Weindl, G. Characterization of reconstructed human skin containing Langerhans cells to monitor molecular events in skin sensitization. Toxicol. Vitr. 2018, 46, 77–85.
- Peiser, M.; Tralau, T.; Heidler, J.; Api, A.M.; Arts, J.H.; Basketter, D.A.; English, J.; Diepgen, T.L.; Fuhlbrigge, R.C.; Gaspari, A.A.; et al. Allergic contact dermatitis: Epidemiology, molecular mechanisms, in vitro methods and regulatory aspects. Current knowledge assembled at an international workshop at BfR, Germany. Cell Mol. Life Sci. 2012, 69, 763–781.
- Silvestre, M.C.; Sato, M.N.; Reis, V.M.S.D. Innate immunity and effector and regulatory mechanisms involved in allergic contact dermatitis. An. Bras. Dermatol. 2018, 93, 242–250.
- Symanzik, C.; Skudlik, C.; John, S.M. Acceptance of skin products in healthcare workers: An empirical investigation. Occup. Med. 2023, 73, 29–32.
- Hui-Beckman, J.; Leung, D.Y.M.; Goleva, E. Hand hygiene impact on the skin barrier in health care workers and individuals with atopic dermatitis. Ann. Allergy Asthma Immunol. 2022, 128, 108–110.
- Litchman, G.; Nair, P.A.; Atwater, A.R.; Bhutta, B.S. Contact Dermatitis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK459230/ (accessed on 26 June 2023).
- Abtahi-Naeini, B. Frequent handwashing amidst the COVID-19 outbreak: Prevention of hand irritant contact dermatitis and other considerations. Health Sci. Rep. 2020, 3, e163.
- Rundle, C.W.; Presley, C.L.; Militello, M.; Barber, C.; Powell, D.L.; Jacob, S.E.; Atwater, A.R.; Watsky, K.L.; Yu, J.; Dunnick, C.A. Hand hygiene during COVID-19: Recommendations from the American Contact Dermatitis Society. J. Am. Acad. Dermatol. 2020, 83, 1730–1737.
- Mostosi, C.; Simonart, T. Effectiveness of barrier creams against irritant contact dermatitis. Dermatology 2016, 232, 353–362.
- Bauer, A.; Rönsch, H.; Elsner, P.; Dittmar, D.; Bennett, C.; Schuttelaar, M.L.A.; Lukács, J.; John, S.M.; Williams, H.C. Interventions for preventing occupational irritant hand dermatitis. Cochrane Database Syst. Rev. 2018, 4, CD004414.
- Azizi, N.; Maibach, H.I. Are topical corticoids efficacious in acute irritant dermatitis: The evidence. Dermatitis 2020, 31, 244–246.
- Antonov, D.; Schliemann, S.; Elsner, P. Contact dermatitis due to Irritation. In Kanerva’s Occupational Dermatology, 3rd ed.; John, S.M., Johansen, J.D., Rustemeyer, T., Elsner, P., Maibach, H.I., Eds.; Springer Nature: Basel, Switzerland, 2020; pp. 119–137.
- Elsner, P.; Agner, T. Hand eczema: A ‘neglected’ disease. J. Eur. Acad. Dermatol. Venereol. 2020, 34 (Suppl. S1), 3.
- Asgari, M.M.; Tsai, A.L.; Avalos, L.; Sokil, M.; Quesenberry, C.P., Jr. Association between topical calcineurin inhibitor use and keratinocyte carcinoma risk among adults with atopic dermatitis. JAMA Dermatol. 2020, 156, 1066–1073.
- Lam, M.; Zhu, J.W.; Tadrous, M.; Drucker, A.M. Association between topical calcineurin inhibitor use and risk of cancer, including lymphoma, keratinocyte carcinoma, and melanoma: A systematic review and meta-analysis. JAMA Dermatol. 2021, 157, 549–558.
- Ferrucci, S.; Persichini, P.; Gola, M.; Scandagli, I.; Pigatto, P.; Legori, A.; Musumeci, M.L.; Micali, G.; D’Agata, E.; Schena, D.; et al. DECISA Project (DErmatology Clinics in Italy: Survey on Alitretinoin): A real-life retrospective cohort multicenter study on 438 subjects with chronic hand eczema. Dermatol. Ther. 2021, 34, e14911.
- Zhu, G.A.; Honari, G.; Ko, J.M.; Chiou, A.S.; Chen, J.K. Dupilumab for occupational irritant hand dermatitis in a non-atopic individual: A case report. JAAD Case Rep. 2020, 6, 296–298.
- Loman, L.; Diercks, G.F.H.; Schuttelaar, M.L.A. Three cases of non-atopic hyperkeratotic hand eczema treated with dupilumab. Contact Dermat. 2021, 84, 124–127.
- Bonnekoh, H.; Vera, C.; Abad-Perez, A.; Radetzki, S.; Neuenschwander, M.; Specker, E.; Mahnke, N.A.; Frischbutter, S.; Latz, E.; Nazaré, M.; et al. Topical inflammasome inhibition with disulfiram prevents irritant contact dermatitis. Clin. Transl. Allergy 2021, 11, e12045.
More
Information
Subjects:
Dermatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
07 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




