Endoscopy plays a central role in diagnostic and therapeutic approaches to biliary disease in both benign and malignant conditions. A cholangioscope is an endoscopic instrument that allows for the direct exploration of the biliary tree. Cholangioscopy has demonstrated excellent performance in discriminating malignant conditions (such as colangiocarcinoma) from benign inflammatory strictures, and more advances (e.g., artificial intelligence and confocal laser endomicroscopy) could further increase its diagnostic accuracy. Cholangioscopy also plays a primary role in the treatment of benign conditions such as difficult bile stones (DBSs).
1. Introduction
Digestive endoscopy was developed as an evolution of fluoroscopic gastrointestinal examinations (e.g., barium enema and barium swallow), allowing for the direct visualization of the gastrointestinal tract with the possibility of performing diagnostic and operative procedures. Biliopancreatic endoscopy performed via endoscopic retrograde cholangiopancreatography (ERCP) is an operative procedure that functions with the help of the diagnostic features of cholangiopancreatography. However, as in fluoroscopic gastrointestinal examinations, the pathological findings of cholangiopancreatographies (e.g., biliary strictures) are only moderately visible. Moreover, fluoroscopically guided biliary brushing and/or biopsies have sub-optimal diagnostic yields [
1]. Thus, there is a need to endoluminally explore the biliopancreatic tract with dedicated endoscopic devices in challenging situations.
Peroral cholangioscopy (POC) is a technique that allows for the direct visualization of the biliary tree; it was introduced early in the 1970s with the so-called “mother-baby” system consisting of a videocholangioscope, i.e., the baby scope, which is inserted into the accessory channel of the “mother” duodenoscope. This type of system requires two operators, thus limiting its maneuverability. The currently available videocholangioscope (Olympus Medical Systems, Tokyo, Japan) has been shown to improve the quality of images and is also applicable to Narrow-Band Imaging (NBI) systems [
2].
In 2007, a new single-operator cholangioscope (SOC) was introduced with a disposable fiberoptic scope (SpyGlass, Boston Scientific Endoscopy, Marlboro, MA, USA). The first version of the SOC produced sub-optimal images, but in 2015, a digital version of the SpyGlass SOC (DSOC) was developed, leading to enhanced image quality and a wider field of view [
3,
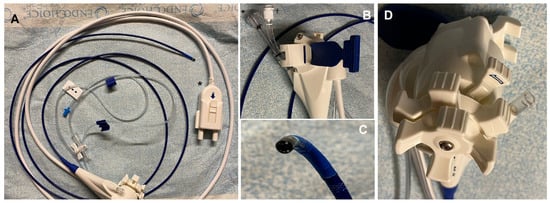
4]. The SOC consists of a disposable delivery catheter of 10 Fr in diameter that is capable of four-way deflected steering and has an outer diameter of 3.3 mm, an accessory channel of 1.2 mm, and separate, dedicated irrigation channels (
Figure 1).
Figure 1. Digital version of the single-operator cholangioscope (DSOC) (SpyGlass, Boston Scientific Endoscopy, Marlboro, MA, USA). (A) The cholangioscope in its full length (214 cm) attached with a catheter cable (white catheter) to the cable connector (black star). (B) Details of the attachment strap (blue part), which allows for the cholangioscope to be fixed to the shaft of the duodenoscope; the Y-port adapter, with a working channel for accessory access (black star); and the irrigation–aspiration port (black cross). (C) Details of the tip of the cholangioscope, featuring two LED lights and two irrigation channels. (D) Details of the two wheels capable of four types of movement and the articulation lock.
As in the “mother-baby” system, the digital SOC is inserted through the accessory channel of a conventional duodenoscope, but it is attached close to the working channel of the duodenoscope, thereby improving the maneuverability and the comfort of the operator. More recently, another digital cholangioscope providing a full high-definition view (eyeMAX™, Micro-Tech™, Nanjing, China) was made available in routine practice [
5].
Another technique involves the use of the peroral direct cholangioscope (D-POC), which was first described in 2006 [
6]. It employs an ultra-slim gastroscope, which was originally developed for use in pediatric patients and for transnasal applications. The advantages of the D-POC are a wider availability of the device in endoscopic services, the ability to obtain high-quality images, and the possibility of using image-enhanced function systems. On the other hand, it is more difficult to insert the scope if the common bile duct (CBD) is not sufficiently dilated, and it is sometimes difficult to stabilize its position; however, the insertion of the D-POC with a balloon catheter on a guidewire introduced in the common bile duct can aid the insertion of the scope [
2].
Cholangioscopy is usually performed using the per-oral route, but the small caliber of the device also allows for its application through the percutaneous and intra-operative routes via trans-hepatic and trans-cystic insertion, respectively. Moreover, a novel short DSOC (65 cm in length) (SpyGlass™ Discover, Boston Scientific Endoscopy, Marlboro, MA, USA) was recently developed that permits ergonomic navigation throughout the biliary system.
All these cholangioscopes have the possibility to have different accessories inserted inside the working channel (e.g., biopsy forceps, retrieval baskets and snares, dilation balloon catheters), allowing operative procedures. Indeed, POC has gained popularity for the treatment of complex choledocholithiasis (e.g., large stones and intrahepatic stones) with the use of cholangioscopy-assisted lithotripsy, which aids in complete bile duct clearance. Direct exploration of the biliary tree also has other applications, ranging from retrieval of migrated stents and exploration of the cystic duct in the case of Mirizzi syndrome to the evaluation of the biliary mucosa after radiofrequency.
2. Indeterminate Biliary Strictures
One of the main applications of POC is the evaluation of biliary strictures (BSs). Almost 20% of BSs are of indeterminate etiology at their presentation [7]. Indetermined BSs are defined when cross-sectional imaging, as well as tissue sampling, is inconclusive or negative, and this represents a challenging clinical scenario [8]. BSs located at the biliary hilum require a multidisciplinary approach for diagnostic and therapeutic decisions [9]. Indeed, almost two-thirds of indeterminate BSs are malignant but one-quarter of BSs at the time of surgical resection are benign [10,11]. Therefore, preoperative evaluation is crucial to properly refer patients for oncological/surgical treatment or conservative treatment in the case of malignant or benign disease, respectively.
2.1. Endoscopic Sampling with ERCP and EUS-FNB
Histological diagnosis with endoscopic sampling is needed when non-invasive tests are inconclusive about the nature of BSs. Endoscopic sampling during ERCP is usually the first-line approach for proximal strictures, whereas endoscopic ultrasound fine needle biopsies (EUS-FNB) are performed as the first approach in the case of distal strictures [
15]. However, both procedures have some limitations and sub-optimal diagnostic yields. ERCP-guided brush cytology and forceps biopsies are historically limited by a low sensitivity (45% and 48.1%, respectively) and the combination of the two techniques increases the sensitivity only modestly (59.4%) [
1], even after optimization of the technique by increasing the number of brushing passes and biopsies [
16,
17] and improving device design [
18].
EUS-guided tissue acquisition is increasingly used for the diagnosis of biliary strictures caused by obstructive tumor masses (e.g., pancreatic cancer and mass-forming cholangiocarcinoma). When FNB needles became available on the market, this allowed excellent sensitivity and specificity to detect malignancy in distal lesions [
19]. However, in the case of strictures secondary to endoductal vegetation, strictures located in the biliary hilum, or in the presence of a biliary stent, the performance of EUS-FNB is impaired [
20].
2.2. Per-Oral Cholangioscopy
Recent guidelines suggest the use of POC when tissue acquisition with the standard biliopancreatic endoscopy techniques fails to reach a definitive diagnosis, especially in the case of a proximal stricture [
15]. POC has great advantages over other endoscopic techniques in allowing the direct visualization of the BS, evaluating the characteristics of the surrounding mucosa, and performing targeted biopsies. Diagnostic POC is a safe procedure that does not increase the expected adverse events that are encountered during ERCP (e.g., pancreatitis, cholangitis, bleeding, and perforation); a meta-analysis showed a pooled rate of POC-related adverse events of 7% [
21], which is similar to the expected rate of post-ERCP complications [
22].
The mucosa of malignant BSs is characterized by peculiar aspects such as abnormal vessels, nodulations and vegetations, friability, and an irregular surface with or without ulcerations. Different classifications of the mucosal pattern of BSs have been proposed in recent years in order to differentiate benign and malignant BSs [
23,
24]. Recently, Kahaleh et al. proposed a novel classification: the Mendoza classification [
25]. In their study, 14 experienced endoscopists reviewed images and clips of DSOC using five criteria (the presence of tortuous and dilated vessels, the presence of irregular nodulations, the presence of raised intraductal lesions, the presence of an irregular surface with or without ulcerations, and the presence of friability) derived from a previous expert consensus. The intraclass correlation coefficient was very high for tortuous and dilated vessels (0.86), raised intraductal lesions (0.90), and presence of friability (0.83), while it was moderate for the presence of an irregular surface with or without ulcerations (0.44). Moreover, the diagnostic intraclass correlation was almost perfect for neoplastic (0.90) and non-neoplastic (0.90) diagnoses. The overall diagnostic accuracy using the revised criteria was 77%. The authors concluded that the Mendoza classification increased the DSOC interobserver agreement and accuracy rate by 16% and 20%, respectively, compared to previous criteria.
Despite few studies showing the poor accuracy of visual impressions for the characterization of BSs [
26,
27], there is a lot of available evidence showing that visual impressions have an optimal accuracy that sometimes is superior to a targeted biopsy (the so-called “cholangioscopy paradox”). A meta-analysis conducted by de Olivera et al. of six studies showed an overall pooled sensitivity and specificity of visual interpretation of biliary malignancies by DSOC of 94% (95% CI 89–97) and 95% (95%CI 90–98), respectively [
28]. An interesting recent multicenter prospective study on 289 patients with indeterminate BSs, who underwent a cholangioscopy with Digital SpyGlass, showed that strictures were visualized effectively in 98.6% of cases, in which a diagnostic visual impression was obtained in 87.2% of patients. The visual impression of malignancy showed a sensitivity of 86.7% and a specificity of 71.2% compared with the final diagnosis obtained after a 6-month follow-up [
29]. Finally, a recent Italian prospective multicenter study on 369 patients evaluated the procedural success of DSOC in the setting of indeterminate BSs; the authors found a sensitivity, specificity, and accuracy for visual impressions of 88.5%, 77.3%, and 83.6%, respectively, with the gold standard as surgery or a negative follow-up after 12 or more months [
30].
2.3. Advanced Diagnostics: Artificial Intelligence and Confocal Laser Endomicroscopy
The integration of artificial intelligence (AI) in gastrointestinal endoscopy has gained popularity and has allowed its early application in clinical practice, especially in the upper and lower gastrointestinal tract for the discrimination of pre-cancerous lesions [
33,
34]. Confocal laser endomicroscopy (CLE) is another innovative diagnostic tool that offers real-time in vivo histopathological data during endoscopic examinations, and it is applied in several gastrointestinal fields in order to obtain a real-time diagnosis [
35]. This technology employs low-energy laser light emission to generate tissue images, thereby enhancing the precision of targeted biopsies and facilitating immediate optical biopsies [
36].
Application of these kinds of advanced techniques in bilio-pancreatic diseases is most useful for the discrimination of malignant and benign BSs. Despite many studies, as described above, showing the optimal accuracy of DSOC for BS determination, diagnostic evaluation with cholangioscopy remains challenging, especially for non-expert endoscopists.
In contrast to CLE, AI is increasingly gaining attention and widespread use in endoscopic applications, considering its ease of use and also valid results in randomized trials in other endoscopic fields such as colonoscopy. The application of AI in cholangioscopy is probably the most recent application of this revolutionary technology in endoscopy and some papers are starting to became available in the literature. The first pilot study on AI applied to DSOC was published in 2022 [
40]. The authors developed, trained, and validated a convolutional neural network (CNN) based on DSOC images. Each frame was labeled as a normal/benign finding or as a malignant lesion if histopathologic evidence of biliary malignancy was available. The model had an overall accuracy of 94.9%, a sensitivity of 94.7%, a specificity of 92.1%, and an AUC of 0.988 in a cross-validation analysis.
3. Difficult Bile Duct Stones
Choledocholithiasis represents the most common indication of ERCP [
46]. Approximately 85–90% of bile duct stones can be removed according to the guidelines during a standard ERCP with balloons or basket retrieval catheters, with a comparable effectiveness and safety [
47]. Conversely, the remaining 10–15% of stones are often more challenging to remove and necessitate additional or advanced techniques; these cases are referred to as difficult biliary stones (DBSs). There are different characteristics that could increase the difficulty of stone extraction, such as a size larger than 15 mm, multiple stones or square/barrel-shaped stones, and a location in the intrahepatic duct or in the cystic duct. Anatomical features of the CBDs could also contribute to a challenging stone extraction such as sigmoid-shape CBDs, narrowing of the CBD distal to the stone, acute distal CBD angulation < 135°, or a shorter length of the distal CBD [
48].
3.1. Cholangioscopy-Assisted Lithotripsy
Cholangioscopy-assisted lithotripsy can be performed using electrohydraulic or laser energy. Both techniques use a probe inserted into the operating channel of the cholangioscope. Saline solution irrigation is crucial to provide a medium for shock wave transmission, as well as to allow visualization of the duct and stones and to flush away debris [
49]. Autolith Touch EHL (Nortech; Northgate Technologies Inc., Elgin, IL, USA) is a U.S. Food and Drug Administration-approved EHL (electrohydraulic lithotripsy) system that consists of a single-use probe with different power settings.
Laser lithotripsy (LL) is a laser light usually obtained with holmium with a precise wavelength that delivers an impulse to induce wave-mediated stone fragmentation. After lithotripsy, the stone fragments are subsequently extracted with standard techniques.
The efficacy of cholangioscopy-assisted lithotripsy for treatment of DBSs has been evaluated in several studies. In the meta-analysis by Korrapati and colleagues, an overall estimated stone clearance rate of 88% (95% CI 85–91%) and an estimated stone recurrence rate of 13% (95% CI 7–20%) were reported, without significant evidence of heterogeneity among the studies [
50]. In a recent multicenter prospective “real-life” study, Fugazza and colleagues investigated the safety and efficacy of lithotripsy performed either with EHL or LL. They treated 152 patients for DBSs with a median size of 20 mm (range 12–45 mm) and a “difficult” localization in 23% of patients [
30]. Overall, the complete duct clearance was comparable to the results of the meta-analysis by Korrapati et al. (92.1%); interestingly, in 82.1% of patients, complete bile duct clearance was obtained in one session.
3.2. Diagnostic Role of Cholangioscopy in DBS Clearance
When DBSs are treated with EPLBD or mechanical lithotripsy, evaluation of the complete clearance of the biliary tree from biliary stones could be challenging. Usually, balloon-occluded cholangiography is performed to confirm bile duct clearance [
59]. However, in patients with residual small-sized stones, a large bile duct, or pneumobilia, adequate bile duct evaluation can be difficult. Moreover, complete clearance of bile ducts is fundamental to prevent future complications [
60]. For these reasons, when clearance of the bile ducts is uncertain and the CBD is sufficiently dilated, it is possible to directly evaluate the presence of residual stones with D-POC using an ultra-slim gastroscope or a standard gastroscope, according to the size of the CBD. This type of examination does not increase the global costs of the procedure and it confirms the clearance of the CBD.
4. Other Applications of Cholangioscopy
4.1. Primary Sclerosing Cholangitis
Primary sclerosing cholangitis (PSC) is a rare, chronic cholestatic liver disease characterized by intrahepatic or extrahepatic strictures or both, with bile duct fibrosis. Patients with PSC are at increased risk of developing cholangiocarcinoma. Differential diagnosis between inflammatory and neoplastic strictures has probably been the most challenging issue throughout the natural history of the disease. Surveillance strategies with MRCP, CA19-9 dosage, and ERCP sampling may have limited the diagnostic yield to detect malignancy [
61].
Cholangioscopy in patients with PSC allows a direct endoscopic evaluation of the stricture and may increase the sensitivity to detecting malignancies. However, few studies are available on the topic, with small sample sizes and suboptimal evidence of efficacy. The first generation of SOC appeared promising in comparison to ERCP for detecting malignancy in patients with PSC in terms of the overall accuracy (93% vs. 55%;
p < 0.001) [
62].
4.2. Mirizzi Syndrome
Mirizzi syndrome (MS) is a rare biliary stone disease generally caused by external compression of the CBD or common hepatic duct due to an impacted gallstone within the gallbladder or cystic duct. Cholangioscopy-assisted lithotripsy has emerged as a successful treatment option since conventional ERCP often fails to remove this kind of stone.
4.3. Other Diagnostic and Operative Applications
Cholangioscopy has other clinical applications that are described in several case reports and case series. Internal migration of the biliary stent is a challenging situation that is usually treated during ERCP. However, fluoroscopic-guided retrieval of the stent is especially difficult when the CBD is markedly dilated and the ERCP accessories float in the duct or when the stent is migrated above the biliary confluence. Direct visualization of the stent during cholangioscopy allows its removal under endoscopic visualization [
68].
Benign polyps or low-grade malignant lesions could grow, on rare occasions, inside the bile ducts, causing symptoms such as jaundice and/or cholangitis. In such cases, demolitive surgery is not indicated but an operative treatment is required to avoid clinical complications. Endoscopic removal of endo-biliary lesions has been described in several reports and it is a valid, minimally invasive option [
70,
71,
72].
Radiofrequency ablation (RFA) is performed in cases of intraductal biliary lesions for therapeutic or palliative reasons. However, the effectiveness of RFA based on radiographic guidance alone may be insufficient, and when it is performed outside the target, severe complications may occur [
74]. Therefore, cholangioscopy has the possibility to perform RFA under direct view [
75] or to evaluate the effect of previous RFA procedures [
76].
Post-ERCP bleeding is a life-threatening condition that sometimes could be difficult to manage with standard endoscopic hemostatic techniques. When endoscopic management fails, radiological embolization may be performed, but interventional radiology is not always available and embolization of branches of the pancreatoduodenal artery could also create complications. When the source of bleeding is endoductal, exploration of the CBD with the D-POC allows the identification of the source of bleeding and the execution of the most appropriate hemostasis technique [
77].
5. Cholangioscopy through Different Routes
5.1. Percutaneous
Percutaneous cholangioscopy (PC) was firstly described in 1983, when the first case series of 39 patients was published by Gazzaniga et al., showing that the procedure was safe and effective for removing biliary stones [
85].
The PC procedure requires the preliminary execution of percutaneous transhepatic biliary access with the standard interventional radiology technique. Once the percutaneous biliary tube is in place, a preliminary cholangiogram is measured to confirm its location and a guidewire is advanced through the biliary tube and into the small bowel. Then, the biliary tube is removed and a tract dilation is usually performed in order to permit access to a 12F or 16F sheath. Cholangioscopy is therefore performed through the percutaneous catheter [
86].
PC could be performed with the same endoscopes used for POC [
32]; however, the standard cholangioscopes used for POC are too long to pass through the short transhepatic route, and they could therefore be cumbersome to manage.
The indications for PC are both diagnostic and therapeutic. The main diagnostic indication is the assessment of indeterminate BSs. The therapeutic indications include difficult bile stones, unreachable papilla (e.g., in the case of altered anatomy), and failed papilla cannulation. The data in the literature are limited to several case reports and small case series. The largest multicenter series on 28 patients was published 2021; the majority of patients had an altered post-surgical anatomy (25/28 patients) and PC was technically successful in one session in 96% of patients [
89]. The majority of patients successfully received lithotripsy for biliary stones and five malignant strictures were found with a histology accuracy of 100% and a visual impression sensitivity of 83.3%.
Post-orthotopic liver transplantation (OLTx) BSs are a common complication that may occur in both preserved anatomies (stricture at the level of biliary anastomosis of the recipient and donor) and altered anatomies (stricture at the level of hepatic-jejunal anastomosis) and may require multiple endoscopic interventions (e.g., endoscopic multistenting) [
91]. However, endoscopic multiple access in the case of an altered anatomy could be time consuming and challenging [
92].
POC could also be challenging in the case of normal anatomies and successful biliary cannulation when biliary stones are located in the more proximal biliary branches, where biliary angulations may block POC passage or may create instability during therapeutic procedures. In such situations, PC may provide valid and easier access to intrahepatic/hilar bile ducts for the treatment of biliary stones [
94,
95,
96,
97,
98].
5.2. Trans-Cystic
Intraoperative exploration of CBD is an old procedure that is performed by surgeons during cholecystectomy for the clearance of concomitant choledocholithiasis. Surgical CBD stone clearance has demonstrated its efficacy in several previous trials [
99], but the use of older choledochoscopes is difficult and not routinely performed by all surgeons [
100]. In addition, the rapid development and wide diffusion of ERCP has led to a further reduction in the use of surgical choledochoscopes [
101].
In the case of concomitant gallbladder and CBD lithiasis, ERCP is usually performed before cholecystectomy or during surgery with the rendez-vous technique [
102]. However, ERCP with the rendez-vous technique is uncommon in routine clinical practice because of organizational drawbacks such as the availability of the endoscopic and surgical equipment.
5.3. Trans-Hepaticogastrostomy
Therapeutic biliopancreatic endoscopy has had an impressive evolution in the last decade, especially with the expansion of interventional EUS. Biliary drainage can now be performed with different EUS-guided techniques such as choledochoduodenostomy, hepaticogastrostomy (HGS), and gallbladder drainage [
109]. HGS is a challenging technique that allows for transgastric or transjejunal biliary drainage, according to the specific anatomy of the left biliary segments [
110]. This type of drainage is more physiological than percutaneous drainage and has less long-term adverse events [
111,
112]. HGS is usually performed in the case of malignant obstruction of both hilar or distal strictures when standard endoscopic drainage techniques are not feasible (duodenal obstruction, failed ERCP, and altered anatomy) [
110]. HGS is actually performed with dedicated metal stents that have a diameter of eight or ten mm [
113].