
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Garry Kerch | -- | 2509 | 2023-09-22 16:21:38 | | | |
| 2 | Lindsay Dong | Meta information modification | 2509 | 2023-09-22 17:17:21 | | |
Video Upload Options
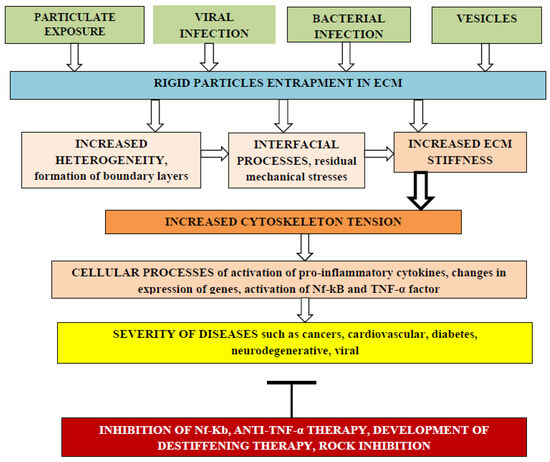
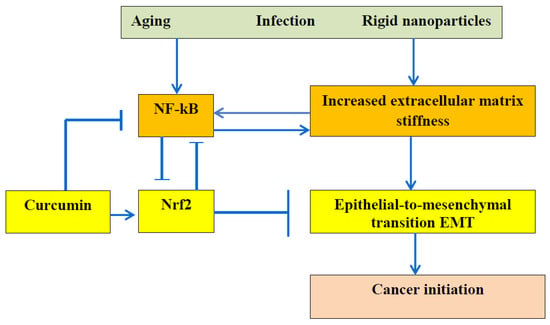
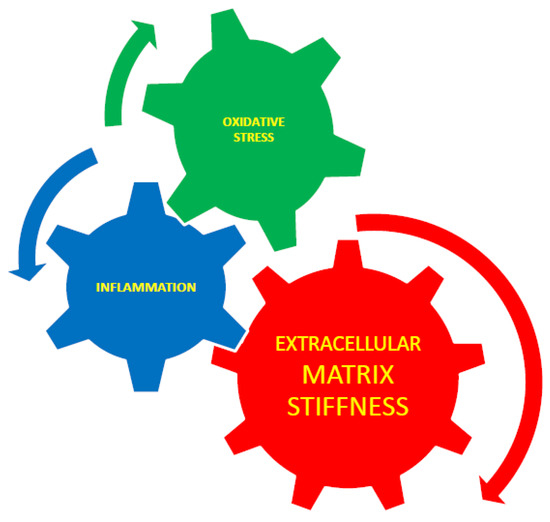
Hydrogels can be considered as mimics of the extracellular matrix (ECM). Through integrins, the cytoskeleton is connected to the ECM, and cytoskeleton tension depends on ECM stiffness. A number of age-related diseases depend on cellular processes related to cytoskeleton function. Some examples of cancer initiation and progression and heart disease in relation to ECM stiffness have been analyzed. The incorporation of rigid particles into the ECM can increase ECM stiffness and promote the formation of internal residual stresses. Water migration, changes in water binding energy to biomactomolecules, and changes in the state of water from tightly bound water to free and loosely bound water lead to changes in the stiffness of the ECM.
1. Introduction
2. Advantages and Risks of Nanocomposite Hydrogels
2.1. Cardiac Tissue Engineering
2.2. Multi-Layer Polyelectrolyte Complex Hydrogels and Bioprinting
2.3. Residual Internal Stresses
2.4. Viscoelastic Hydrogels
2.5. Hydrogel Nanocomposites
2.6. Effect of Water
2.7. ECM Stiffness and Cancer
2.7.1. Cancer Models
2.7.2. Polyphenols Decrease ECM Stiffness
2.7.3. Chitosan and Chitosan Oligosaccharides
2.7.4. Anti-TNF-α and Anti-NF-κB Therapies
2.8. Equivalence of ECM Stiffness, Oxidative Stress, and Inflammation
References
- Annabi, N.; Tamayol, A.; Uquillas, J.A.; Akbari, M.; Bertassoni, L.E.; Cha, C.; Camci-Unal, G.; Dokmeci, M.R.; Peppas, N.A.; Khademhosseini, A. 25th anniversary article: Rational design and applications of hydrogels in regenerative medicine. Adv. Mater. 2014, 26, 85–124.
- Camci-Unal, G.; Annabi, N.; Dokmeci, M.R.; Liao, R.; Khademhosseini, A. Hydrogels for cardiac tissue engineering. NPG Asia Mater. 2014, 6, e99.
- Crocini, C.; Walker, C.J.; Anseth, K.S.; Leinwand, L.A. Three-dimensional encapsulation of adult mouse cardiomyocytes in hydrogels with tunable stiffness. Prog. Biophys. Mol. Biol. 2020, 154, 71–79.
- Pournemati, B.; Tabesh, H.; Jenabi, A.; Aghdam, R.M.; Rezayan, A.H.; Poorkhalil, A.; Tafti, S.H.A.; Mottaghy, K. Injectable conductive nanocomposite hydrogels for cardiac tissue engineering: Focusing on carbon and metal-based nanostructures. Eur. Polym. J. 2022, 174, 111336.
- Liu, G.; Ding, Z.; Yuan, Q.; Xie, H.; Gu, Z. Multi-layered hydrogels for biomedical applications. Front. Chem. 2018, 6, 439.
- Kerch, G.M.; Irgen, L.A. Stiffness of composites based on polypropylene and low-density polyethylene. Mech. Compos. Mater. 1989, 25, 288–292.
- Horkay, F.; Bassera, P.J. Hydrogel composite mimics biological tissues. Soft Matter 2022, 18, 4414–4426.
- Xie, N.; Xiao, C.; Shu, Q.; Cheng, B.; Wang, Z.; Xue, R.; Wen, Z.; Wang, J.; Shi, H.; Fan, D.; et al. Cell response to mechanical microenvironment cues via Rho signaling: From mechanobiology to mechanomedicine. Acta Biomater. 2023, 159, 1–20.
- Lin, Y.; Zheng, Y. Approaches of targeting Rho GTPases in cancer drug discovery. Expert Opin. Drug Discov. 2015, 10, 991–1010.
- Chaudhuri, O.; Cooper-White, J.; Janmey, P.A.; Mooney, D.J.; Shenoy, V.B. Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature 2020, 584, 535–546.
- Nam, S.; Stowers, R.; Lou, J.; Xia, Y.; Chaudhuri, O. Varying PEG density to control stress relaxation in alginate-PEG hydrogels for 3D cell culture studies. Biomaterials 2019, 200, 15–24.
- Liu, Y.; Hu, J.; Xiao, Z.; Jin, X.; Jiang, C.; Yin, P.; Tang, L.; Sun, T. Dynamic behavior of tough polyelectrolyte complex hydrogels from chitosan and sodium hyaluronate. Carbohydr. Polym. 2022, 288, 119403.
- Butcher, A.L.; Offeddu, G.S.; Oyen, M.L. Nanofibrous hydrogel composites as mechanically robust tissue engineering scaffolds. Trends Biotechnol. 2014, 32, 564–570.
- Engin, A.B.; Nikitovic, D.; Neagu, M.; Henrich-Noack, P.; Docea, A.O.; Shtilman, M.I.; Golokhvast, K.; Tsatsakis, A.M. Mechanistic understanding of nanoparticles’ interactions with extracellular matrix: The cell and immune system. Part. Fibre Toxicol. 2017, 14, 22.
- Chaudhuri, O.; Koshy, S.T.; Branco da Cunha, C.; Shin, J.-W.; Verbeke, C.; Allison, K.H.; Mooney, D.J. Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat. Mater. 2014, 13, 970–978.
- Kerch, G.; Chausson, M.; Gautier, S.; Meri, R.M.; Zicans, J.; Jakobsons, E.; Joner, M. Heparin-like polyelectrolyte multilayer coatings based on fungal sulfated chitosan decrease platelet adhesion due to the increased hydration and reduced stiffness. Biomater. Tissue Technol. 2017, 1, 1–5.
- Kerch, G.; Glonin, A.; Zicans, J.; Meri, R.M. A DSC study of the effect of bread making methods on bound water content and redistribution in chitosan enriched bread. J. Therm. Anal. Calorim. 2012, 108, 185–189.
- Kerch, G. Distribution of tightly and loosely bound water in biological macromolecules and age-related diseases. Int. J. Biol. Macromol. 2018, 118 Pt A, 1310–1318.
- Kerch, G. Polymer hydration and stiffness at biointerfaces and related cellular processes. Nanomedicine 2018, 14, 13–25.
- Kerch, G. Role of changes in state of bound water and tissue stiffness in development of age-related diseases. Polymers 2020, 12, 1362.
- Kerch, G. Tissue integrity and COVID-19. Encyclopedia 2021, 1, 206–219.
- Marques, M.P.M.; Batista de Carvalho, A.L.M.; Mamede, A.P.; Dopplapudi, A.; Batista de Carvalho, L.A.E. Role of intracellular water in the normal-to-cancer transition in human cells-insights from quasi-elastic neutron scattering. Struct. Dyn. 2020, 7, 054701.
- Marques, M.P.; Batista de Carvalho, A.L.; Sakai, V.G.; Hatter, L.; Batista de Carvalho, L.A. Intracellular water—An overlooked drug target? Cisplatin impact in cancer cells probed by neutrons. Phys. Chem. Chem. Phys. 2017, 19, 2702–2713.
- Marques, M.P.M.; Santos, I.P.; Batista de Carvalho, A.L.M.; Mamede, A.P.; Martins, C.B.; Figueiredo, P.; Sarter, M.; García Sakai, V.; Batista de Carvalho, L.A.E. Water dynamics in human cancer and non-cancer tissues. Phys. Chem. Chem. Phys. 2022, 24, 15406–15415.
- Bastos, F.R.; da Costa, D.S.; Reis, R.L.; Alves, N.M.; Pashkuleva, I.; Costa, R.R. Layer-by-layer coated calcium carbonate nanoparticles for targeting breast cancer cells. Biomater. Adv. 2023, 153, 213563.
- Keenan, T.M.; Folch, A. Biomolecular gradients in cell culture systems. Lab Chip 2008, 8, 34–57.
- Luo, T.; Tan, B.; Zhu, L.; Wang, Y.; Liao, J. A review on the design of hydrogels with different stiffness and their effects on tissue repair. Front. Bioeng. Biotechnol. 2022, 10, 817391.
- Tang, R.-Z.; Liu, X.-Q. Biophysical cues of in vitro biomaterials-based artificial extracellular matrix guide cancer cell plasticity. Mater. Today Bio 2023, 19, 100607.
- Ondeck, M.G.; Kumar, A.; Placone, J.K.; Plunkett, C.M.; Matte, B.F.; Wong, K.C.; Fattet, L.; Yang, J.; Engler, A.J. Dynamically stiffened matrix promotes malignant transformation of mammary epithelial cells via collective mechanical signaling. Proc. Natl. Acad. Sci. USA 2019, 116, 3502–3507.
- Pendás-Franco, N.; García, J.M.; Peña, C.; Valle, N.; Pálmer, H.G.; Heinäniemi, M.; Carlberg, C.; Jiménez, B.; Bonilla, F.; Muñoz, A.; et al. DICKKOPF-4 is induced by TCF/beta-catenin and upregulated in human colon cancer, promotes tumour cell invasion and angiogenesis and is repressed by 1alpha,25-dihydroxyvitamin D3. Oncogene 2008, 27, 4467–4477.
- Pendás-Franco, N.; Aguilera, O.; Pereira, F.; González-Sancho, J.M.; Muñoz, A. Vitamin D and Wnt/beta-catenin pathway in colon cancer: Role and regulation of DICKKOPF genes. Anticancer Res. 2008, 28, 2613–2623.
- De Bruyne, T.; Steenput, B.; Roth, L.; De Meyer, G.R.Y.; dos Santos, C.N.; Valentová, K.; Dambrova, M.; Hermans, N. Dietary polyphenols targeting arterial stiffness: Interplay of contributing mechanisms and gut microbiome-related metabolism. Nutrients 2019, 11, 578.
- Kerch, G. Severe COVID-19—A review of suggested mechanisms based on the role of extracellular matrix stiffness. Int. J. Mol. Sci. 2023, 24, 1187.
- Serino, A.; Salazar, G. Protective role of polyphenols against vascular inflammation, aging and cardiovascular disease. Nutrients 2019, 11, 53.
- Arcan, I.; Yemenicioğlu, A. Incorporating phenolic compounds opens a new perspective to use zein films as flexible bioactive packaging materials. Food Res. Int. 2011, 44, 550–556.
- Emmambux, M.N.; Stading, M.; Taylor, J.R.N. Sorghum kafirin film property modification with hydrolysable and condensed tannins. J. Cereal Sci. 2004, 40, 127–135.
- Ashrafizadeh, M.; Ahmadi, Z.; Mohammadinejad, R.; Farkhondeh, T.; Samarghandian, S. Curcumin activates the Nrf2 pathway and induces cellular protection against oxidative injury. Curr. Mol. Med. 2020, 20, 116–133.
- Liu, Z.; Dou, W.; Zheng, Y.; Wen, Q.; Qin, M.; Wang, X.; Tang, H.; Zhang, R.; Lv, D.; Wang, J.; et al. Curcumin upregulates Nrf2 nuclear translocation and protects rat hepatic stellate cells against oxidative stress. Mol. Med. Rep. 2016, 13, 1717–1724.
- Ghafouri-Fard, S.; Shoorei, H.; Bahroudi, Z.; Hussen, B.M.; Talebi, S.F.; Taheri, M.; Ayatollahi, S.A. Nrf2-related therapeutic effects of curcumin in different disorders. Biomolecules 2022, 12, 82.
- Kerch, G. Role of extracellular matrix stiffness inhibitors in Alzheimer’s disease. Alzheimers’s Dis. Dement. 2022, 6, 140–144.
- Rashid, N.; Khalid, S.H.; Khan, I.U.; Chauhdary, Z.; Mahmood, H.; Saleem, A.; Umair, M.; Asghar, S. Curcumin-Loaded bioactive polymer composite film of PVA/Gelatin/Tannic Acid downregulates the pro-inflammatory cytokines to expedite healing of full-thickness wounds. ACS Omega 2023, 8, 7575–7586.
- Wang, J.; Xie, S.; Li, N.; Zhang, T.; Yao, W.; Zhao, H.; Pang, W.; Han, L.; Liu, J.; Zhou, J. Matrix stiffness exacerbates the proinflammatory responses of vascular smooth muscle cell through the DDR1-DNMT1 mechanotransduction axis. Bioact. Mater. 2022, 17, 406–424.
- Ta, H.T.; Dass, C.R.; Dunstan, D.E. Injectable chitosan hydrogels for localized cancer therapy. J. Control. Release 2008, 126, 205–216.
- Garshasbi, H.; Salehi, S.; Naghib, S.M.; Ghorbanzadeh, S.; Zhang, W. Stimuli-responsive injectable chitosan based hydrogels for controlled drug delivery systems. Front. Bioeng. Biotechnol. 2023, 10, 1126774.
- Andrade, F.; Roca-Melendres, M.M.; Durán-Lara, E.F.; Rafael, D.; Schwartz, S. Stimuli-responsive hydrogels for cancer treatment: The role of pH, light, ionic strength and magnetic field. Cancers 2021, 13, 1164.
- Mäki-Petäjä, K.M.; Hall, F.C.; Booth, A.D.; Wallace, S.M.; Yasmin; Bearcroft, P.W.; Harish, S.; Furlong, A.; McEniery, C.M.; Brown, J. Rheumatoid arthritis is associated with increased aortic pulse-wave velocity, which is reduced by anti–tumor necrosis factor-α therapy. Circulation 2006, 114, 1185–1192.
- Zhou, R.H.; Vendrov, A.E.; Tchivilev, I.; Niu, X.L.; Molnar, K.C.; Rojas, M.; Carter, J.D.; Tong, H.; Stouffer, G.A.; Madamanchi, N.R.; et al. Mitochondrial oxidative stress in aortic stiffening with age: The role of smooth muscle cell function. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 745–755.
- Urbano, R.L.; Swaminathan, S.; Clyne, A.M. Stiff substrates enhance endothelial oxidative stress in response to protein kinase C activation. Appl. Bionics Biomech. 2019, 2019, 6578492.
- Shahin, Y.; Khan, J.A.; Chetter, I. Angiotensin converting enzyme inhibitors effect on arterial stiffness and wave reflections: A meta-analysis and meta-regression of randomised controlled trials. Atherosclerosis 2012, 221, 18–33.
- Neves, M.F.; Cunha, A.R.; Cunha, M.R.; Gismondi, R.A.; Oigman, W. The role of renin-angiotensin-aldosterone system and its new components in arterial stiffness and vascular aging. High Blood Press. Cardiovasc. Prev. 2018, 25, 137–145.
- Koumaras, C.; Tziomalos, K.; Stavrinou, E.; Katsiki, N.; Athyros, V.G.; Mikhailidis, D.P.; Karagiannis, A. Effects of renin-angiotensin-aldosterone system inhibitors and beta-blockers on markers of arterial stiffness. J. Am. Soc. Hypertens. 2014, 8, 74–82.




