Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ahmet Cagdas Seckin | -- | 3310 | 2023-09-19 13:05:42 | | | |
| 2 | Ahmet Cagdas Seckin | + 1 word(s) | 3311 | 2023-09-19 13:06:55 | | | | |
| 3 | Rita Xu | Meta information modification | 3311 | 2023-09-20 03:25:09 | | | | |
| 4 | Brendan Ellis Lowe | -29 word(s) | 3282 | 2025-09-26 12:10:10 | | | | |
| 5 | Catherine Yang | + 29 word(s) | 3311 | 2025-10-10 07:58:48 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Seçkin, A.�.; Ateş, B.; Seçkin, M. Wearable Technology in Sports. Encyclopedia. Available online: https://encyclopedia.pub/entry/49380 (accessed on 07 February 2026).
Seçkin A�, Ateş B, Seçkin M. Wearable Technology in Sports. Encyclopedia. Available at: https://encyclopedia.pub/entry/49380. Accessed February 07, 2026.
Seçkin, Ahmet Çağdaş, Bahar Ateş, Mine Seçkin. "Wearable Technology in Sports" Encyclopedia, https://encyclopedia.pub/entry/49380 (accessed February 07, 2026).
Seçkin, A.�., Ateş, B., & Seçkin, M. (2023, September 19). Wearable Technology in Sports. In Encyclopedia. https://encyclopedia.pub/entry/49380
Seçkin, Ahmet Çağdaş, et al. "Wearable Technology in Sports." Encyclopedia. Web. 19 September, 2023.
Copy Citation
Wearable technology is increasingly vital for improving sports performance through real-time data analysis and tracking. Both professional and amateur athletes rely on wearable sensors to enhance training efficiency and competition outcomes.
wearable
sport
IoT
biomechanic
sensors
1. Introduction
The concept of Wearable Technology (WT) has been used in various fields such as healthcare, sports, entertainment, electronics, textiles, and the defense industry for a long time [1][2][3][4][5]. Thanks to the opportunities provided by sensor and internet technology, WT has made significant progress in the last two decades and ha become devices that we frequently use in our daily lives.
Various definitions have been proposed for the concept of WT, and it is an interdisciplinary field that involves disciplines such as engineering, healthcare, and sports. Godfrey et al. described the concept of WT by focusing on smartwatches and stating that it encompasses numerous devices that are directly or loosely worn on a person [2]. According to Seçkin et al., WT refers to non-invasive devices and sensors that individuals can wear on their bodies to assist in monitoring their health conditions, without requiring subcutaneous applications [5]. Shen et al. defined the concept of WT as mobile electronic devices that can be comfortably worn on the user’s body or attached to their clothing [6]. Park et al., stated that WT devices differ from traditional clothing and enable personalized mobile computing [4]. Coyle and Diamond emphasized that WT devices should be soft, flexible, and washable, and they should meet people’s expectations of normal clothing [7]. Ye et al., defined the concept of WT, which they examined as smart textiles, as fabrics with various integrated electronic components. They emphasized that this technology should meet the fundamental requirements of clothing, such as comfort, lightweight, thermal insulation, and breathability [8]. The common underlying point identified in these studies, in addition to direct definitions, is that WTs should incorporate sensors, processing units, power sources, and be wearable on the body. It is observed in some review papers that various sports equipment are also considered as wearable [3][9]; however, these are not actually wearable on the body and fall into the category of smart equipment, such as a smartphone or remote control device. From this perspective, it is crucial to define the boundaries of wearability clearly. Taking the above definitions together, WT can be described as devices that are worn on the body, non-invasive, and incorporate various electronic components such as sensors, communication units, processors, actuators, and power sources.
2. Hardware and Software of WT in Sport
WT, at its core, is Internet of Things devices and consist of three layers as illustrated in Figure 1: sensor, processing, and network. The first two layers, sensor, and processor, encompass all the operations that take place solely on the electronic hardware of the WT. Additionally, various external devices, computing methods, and communication protocols are incorporated into the network layer as part of WT.
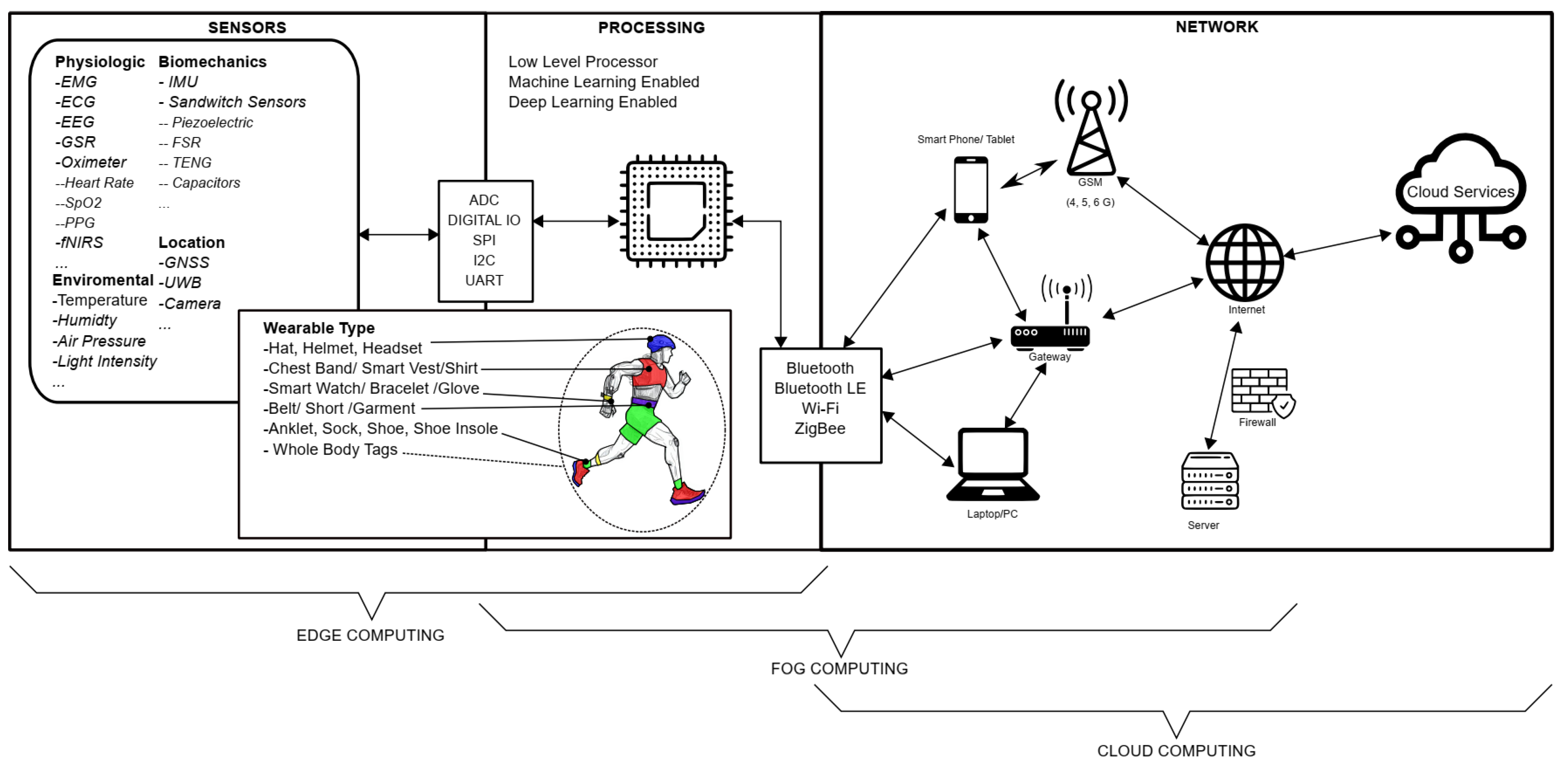
Figure 1. Layered Structure of Wearable Computing.
2.1. Sensors Layer
The first layer is the sensor layer, where information obtained from the human body through various means is transmitted as signals to the processor, the second layer of the WT, using analog-to-digital converters (ADC), digital inputs, Inter-Integrated Circuit (I2C), Universal Asynchronous Receiver/Transmitter (UART), Serial Peripheral Interface (SPI), and similar methods. In today’s sports field, WT with sensors or sensor systems provides valuable data by measuring physiological, motion, position, and environmental conditions.
2.1.1. Physiological Sensors
Physiological data encompasses information derived from the biological processes occurring within the human body, serving as a valuable source of insights into an individual’s health, performance, or overall condition. Prominent among the sensors used for capturing physiological data are well-recognized devices such as Electromyography (EMG), Electrocardiography (ECG), and Electroencephalography (EEG). Furthermore, physiological data acquisition extends to include an array of sensors such as functional Near-Infrared Spectroscopy (fNIRS), Oximeter, Blood Pressure Sensors (BPS), Galvanic Skin Response (GSR), and respiratory monitoring sensors.
In the context of sports and related fields, the term “biometric data” is at times used to describe the physiological data obtained from athletes [10][11][12]. However, it is important to distinguish this usage from the engineering domain, where “biometric data” encompasses information utilized for the purpose of identifying individuals through the analysis of their biological characteristics and events [13]. Biometric identity verification relies on immutable physical or behavioral attributes unique to each individual and is considered unalterable. Governments and security systems employ biometrics as a robust method of personal identification for this reason [14]. It is crucial to acknowledge that data gathered from sensors measuring an athlete’s physiological responses do not inherently possess the same uniqueness or distinctiveness characteristic of biometric data. Consequently, caution must be exercised when applying the term “biometric data” in the context of athletic research, as this misalignment in terminology can potentially lead to legal and ethical complications, as well as cause confusion within the scientific community.
EMG system measures the electrical activity of muscles. By providing data such as muscle contractions and muscle strength, they can provide information about muscle activity and performance [15][16][17]. EMG electrodes are placed to detect the electrical signals originating from the muscles. During muscle contraction and relaxation, neurons in the muscle fibers produce electrical signals. This electrical activity is associated with the movement of muscles or changes in muscle tone. EMG electrodes detect and record the electrical activity of muscles by capturing this electrical activity. The obtained EMG signals are processed and recorded through amplifiers and data recorders. EMG signals reflect the magnitude, duration, timing, and coordination of muscle contractions.
ECG is a technique that records cardiac electrical activity and provides information on heart rate variability (HRV), cardiac arrhythmias, and cardiovascular health [18][19][20]. ECG is a valuable tool for evaluating the health and performance of athletes, as it can reflect the autonomic nervous system regulation, the metabolic demand, and the cardiac adaptation to exercise. ECG is an important tool for monitoring athletes’ health and performance, optimizing exercise programs, and assessing heart health [21].ECG electrodes are placed on specific locations of the torso and limbs to capture the signals generated by the cardiac depolarization and repolarization. Some commercial WT, such as smartwatches and wristbands, claim to have ECG detection capabilities, but they usually measure a single-lead ECG that is more suitable for detecting training load or cardiac disorders than for providing a comprehensive ECG analysis [22][23]. The conventional ECG acquisition is often inconvenient and intrusive, as it requires multiple electrodes and wires that may interfere with the natural movement of the athletes.
EEG sensors measure brain waves using electrical methods and provide data related to brain activity [24][25]. These data can provide information about an athlete’s brain activity, sleep quality, concentration, and other factors. The working principle of EEG involves the placement of metal plates called electrodes or sensors on the scalp. These electrodes are used to detect electrical activity in the brain. The electrodes are typically placed at specific points on the scalp to capture electrical signals from different regions of the brain. Brain cells or neurons are the cells that generate and transmit electrical signals. This electrical activity is due to the potential differences created as neurons communicate with each other. EEG electrodes detect and record these electrical activities to obtain brain wave patterns. EEG signals consist of different components known as low-frequency (slow) and high-frequency (fast) brain waves. Brain waves can reflect different aspects of brain activity such as sleep, wakefulness, focus, or different mental states [26].
Athlete brain activity monitoring applications are also measured with functional near-infrared spectroscopy (fNIRS) sensors [25][27]. Neuronal activity in the brain causes changes in oxygenation. fNIRS uses near-infrared light emitted by a light source, which is absorbed by hemoglobin in the tissue. When the oxygenation of hemoglobin changes, its absorption properties also change. When the fNIRS detector detects the reflected or scattered light from the brain, it measures the changes in oxygenation and collects this information as a data set.
Pulse oximeter sensors are used by placing them on the fingertip or near blood vessels to provide data such as peripheral oxygen saturation (SpO2), heart rate (HR), and photoplethysmography (PPG). Oximeters operate by using two different light sources: red and infrared. Oxygenated blood absorbs more red light, while deoxygenated blood absorbs more infrared light. The oximeter measures the amount of light passing through the skin or tissues using these two light sources. This data provides information about athletes’ oxygen levels, heart rate, and exercise performance [28][29].
BPS facilitates the assessment of athletes’ blood pressure levels and cardiovascular well-being through blood pressure measurement [30][31][32]. Typically, the BPS is designed as either a cuff or a wristband. This WT employs a mechanism in which the cuff is inflated using air until arterial blood flow is occluded. The pressure reading corresponding to the cessation of arterial blood flow indicates the Systolic blood pressure value. After this occlusion, the applied pressure is gradually released. During this process, oscillations in pressure occur due to cardiac contractions, and the pulse rate is determined by quantifying these oscillations and the time intervals between them. The minimal pressure threshold required for pulse detection designates the Diastolic blood pressure value. Consequently, this methodology enables the determination of both systolic (maximum) and diastolic (minimum) blood pressure values, expressed in pulse per minute and millimeters of mercury (mmHg) units.
The GSR sensor is based on the principle that the skin’s electrical conductivity can vary due to sweating. Sweating increases the moisture level on the skin, thereby increasing electrical conductivity. Therefore, when a person experiences an emotional response or exerts physical effort, the amount of sweating and, consequently, the electrical conductivity change [33][34][35].
Respiratory sensors measure data such as respiratory rate, respiratory depth, and respiratory pattern. These data provide information about athletes’ respiratory performance, exercise capacity, and energy expenditure [36][37][38]. These sensors typically work by measuring respiratory movements using various types of sensors, including optical, mechanical, or electromagnetic sensors, which are usually placed on the chest area. Smart masks are WT capable of monitoring an athlete’s respiratory and metabolic parameters during exercises or other activities. There are many commercial examples such as Calibre [39] K5 [40], and Cortex–Metamax 3B [41]. These devices exhibit the characteristic of becoming the gold standard, particularly in terms of energy expenditure and performance measurements. Wearable smart masks comprise a multitude of sensors such as gas sensors, flow sensors, heart rate sensors, temperature sensors, and humidity sensors [42][43]. However, the primary sensors consist of oxygen and carbon dioxide gas sensors along with a flow measurement sensor. Other sensors serve auxiliary roles, and in some commercial products, they are positioned in a manner that could be more effective outside the mask, incorporating additional systems such as ECG. Wearable smart masks hold considerable potential applications within sports science and medicine. They enable accurate and continuous measurements of fundamental parameters, namely, respiratory gas exchange and metabolic rate, for evaluating aerobic capacity, anaerobic threshold, energy expenditure, substrate utilization, respiratory efficiency, lung function, and more. These parameters can aid in assessing and optimizing physical performance, including monitoring training intensity and duration, recovery, and adaptation processes, as well as identifying health issues or risks. Wearable smart masks also have the capability to offer personalized feedback and guidance tailored to users’ goals and preferences.
2.1.2. Biomechanics Sensors
Biomechanics is the application of mechanical engineering principles to living organisms, and it encompasses studies at the tissue and joint levels [44]. Biomechanics involves applying forces to biological systems and specifically includes the effects of forces applied to the human body [45]. Within this scope, motion data refers to the use of sensors to monitor athletes’ skeletal movements and muscle activities. In sports, the primary sensor used for motion sensing is the IMU and other sensors such as force sensors and EMG sensors are also utilized.
IMU is a type of microelectromechanical system (MEMS) sensor consisting of multiple sensors combined. An IMU sensor can include an accelerometer, gyroscope, and magnetometer sensors. The accelerometer is used to measure changes in acceleration resulting from applied forces. The gyroscope is used to determine the amount of angular rotation. The compass is used to measure the orientation of the sensor based on Earth’s magnetic field. The compass is mainly used as a supporting sensor for sensor fusion with the accelerometer and gyroscope to determine the direction and magnitude of motion [46][47][48]. IMU sensors can be used for various purposes such as swimming [49][50], posture analysis [51][52][53], and exercise tracking [54][55].
Various sensors are used for force and motion detection in the field of sports. Some of these are sandwich-type sensors consisting of piezoelectric [56][57][58][59], resistor [60][61][62][63], capacitor and magnetic elements. These sensors convert mechanical energy into electrical energy to form triboelectric nanogenerator (TENG) systems [64][65][66]. TENGs can be integrated with textile-based systems as wearable sensors in the field of sports [64][65]. Piezoelectric sensors are inexpensive, sensitive, and capable of measuring quickly, but piezo crystals have a fragile structure and are not suitable for highly flexing surfaces. Resistive sensors, on the other hand, measure the deformation of the tissues obtained by knitting conductive threads as a change in resistance. These sensors are affected in situations such as liquid contact and perspiration, and coated systems must be used. The Strain gauge sensor is a coated resistive sensor and must be attached to the surface to detect hand movements. These sensors are custom-made and expensive. Applications for the use of conductive liquid in silicon are resistive sensors with high performance but difficult to manufacture and design [67]. If these sensors are punctured or ruptured, the leaking liquid may harm human health. Capacitive sensors are passive circuit elements that measure the capacitance change of the dielectric material between two conductive plates. These sensors are preferred because of the insulator of biological materials and offer new horizons in the measurement of biopotential energy in humans. Capacitive sensors do not require electrodes to contact the skin, use conductive liquid/gel, or fixation, and can measure as precisely and stable as other methods.
2.1.3. Location Sensors
Location sensors are used to track athletes’ position changes and movements. The most fundamental wearable positioning systems include Global Navigation Satellite System (GNSS), Ultra-wideband (UWB) positioning systems, Wi-Fi, Bluetooth, RFID, and wearable marker positioning systems [68][69][70]. The most used methods among these are GNSS, UWB, and camera-based wearable marker positioning systems.
GNSS refers to satellite-based navigation systems, with the Global Positioning System (GPS) being the most widely used. A GNSS receiver receives satellite signals, analyzes the timing and location of the signals, and determines the user’s position accordingly. GNSS is suitable for open-field applications, but it may not work or may be misleading in indoor environments due to signal weakening and reflections. In sports, it is used for position determination, speed and distance measurement, and activity analysis studies [69][71][72].
The UWB positioning system consists of a transmitter and one or more UWB receivers. The UWB transmitter generates short-duration pulse signals and transmits them over a wide frequency band. UWB receivers receive the signals from the UWB transmitter and analyze their arrival time, power, and frequency spectrum. Through this analysis, the position of the user wearing UWB can be determined based on the time, path, and obstacles through which the signals propagate [69][73]. UWB positioning provides high accuracy and precision and is also inexpensive and easily portable. UWB modules combined with IMUs are used for applications such as motion capture, biomechanics, and action recognition [74][75][76].
Camera-based wearable marker positioning systems involve tracking multiple wearable markers with multiple cameras to monitor the user’s position and movements. These systems allow real-world movements to be reflected in virtual environments. While these systems are designed for positioning purposes, they are primarily used in biomechanical analysis and motion recognition due to their high precision and accuracy [77][78][79].
2.1.4. Environmental Condition Sensors
Environmental condition sensors on the WT are sensors that measure environmental effects such as air quality, humidity, temperature, air pressure, and UV light level [3][80][81]. These sensors are used to monitor the condition of the environment where athletes are present. Air quality sensors assess the impact of factors such as air pollution and allergens by monitoring athletes’ respiratory conditions during exercise. Humidity sensors track the humidity levels in the surroundings, while temperature sensors monitor environmental temperature changes. Air pressure sensors track atmospheric pressure variations and are used for altitude calculations. UV light sensors measure athletes’ exposure levels to sunlight.
2.2. Processing Layer
The processing unit in the second layer is either a microcontroller or a single-board computer/processor that can be integrated within the physical boundaries of the WT. The microcontrollers or processors in the second layer possess relatively low-level capabilities in terms of memory, processing power, and operational time. Edge computing can only be performed with the hardware up to the second layer, allowing the generation of user feedback through methods such as signal processing, feature engineering, data compression, or machine learning. Actuators such as screens, LEDs, vibration motors, and speakers on WTs enable human-computer interaction by producing responses or alerts. Up to this stage, tasks performed in WT such as heart rate monitoring, oxygen level (SpO2) measurement, and step counting are at the edge computing level and do not involve wireless communication. To handle more complex tasks, higher processing capacity is required, and access to the third and fourth layers is achieved through wireless communication.
Current wearable processing units can be classified into three different levels based on their processing capabilities, power consumption, size, and features: low-level microcontrollers, high-level or machine learning-enabled microcontrollers and single-board computers. The processing and memory capacity parameter measures the computational capability of the processing unit and memory. Processing power determines the type and complexity of tasks that can be performed by the processing unit, such as data acquisition, signal processing, and machine learning. Memory affects the storage capacity, data access speed, and power consumption of the processing unit. Power consumption is dependent on the efficiency of the electronics and the amount of processing in the device. Power consumption determines the battery life, heat dissipation, and size of the processing unit. The size parameter measures the physical dimensions of the hardware unit, and it affects the portability, wearability, and aesthetics of the processing unit.
-
Low-level microcontrollers have limited processing power and memory, but are suitable for data collecting and basic signal processing tasks. They are also low-cost, low-power, and small-sized devices that can be integrated with sensors and other peripherals.
-
High-level microcontrollers have more processing power and memory and can support advanced functions such as machine learning, wireless communication, and security. They are also more expensive, consume more power, and require more space than low-level microcontrollers.
-
Single Board Computers (SBC) have a complete system on a single board, including a processor, memory, storage, input/output ports, and operating system. They can perform complex tasks such as image recognition, speech recognition, and natural language processing. They are also more powerful, versatile, and customizable than high-level microcontrollers. These types of processors can also support deep learning applications that require intensive computation and large datasets, but they are the most expensive, power-hungry, and bulky devices among wearable processing units, so they are not widely used.
2.3. Network Layer
Due to the power and size limitations in WTs, the processing capacity is limited, and therefore, if more complex outputs are desired, the data obtained should be included in the process with wireless communication methods such as Bluetooth, Wi-Fi, Zigbee, etc. In the third layer, WT communicates wirelessly, transmitting data to devices with higher processing capacity such as computers, smartphones, gateways, and similar devices, enabling the production of more sophisticated output. The computational operations performed at this level are called fog computing. Cloud computing is used if these devices have difficulty in performing the desired operations or if more advanced services are needed. Fog computing involves processing data from WTs at nearby gateways or cloud services with higher processing capacity. At this stage, data is transferred to cloud-based services for deeper analysis, data mining and other complex operations. Wearables for cloud computing communicate directly with servers with very high processing capacity, either stand-alone or via a smartphone, computer, or gateway device. At this stage, fog or cloud computing can be used as needed.
References
- Guler, S.D.; Gannon, M.; Sicchio, K. A Brief History of Wearables. In Crafting Wearables: Blending Technology with Fashion; Guler, S.D., Gannon, M., Sicchio, K., Eds.; Apress: Berkeley, CA, 2016; pp. 3–10. ISBN 978-1-4842-1808-2.
- Godfrey, A.; Hetherington, V.; Shum, H.; Bonato, P.; Lovell, N.H.; Stuart, S. From A to Z: Wearable Technology Explained. Maturitas 2018, 113, 40–47.
- Aroganam, G.; Manivannan, N.; Harrison, D. Review on Wearable Technology Sensors Used in Consumer Sport Applications. Sensors 2019, 19, 1983.
- Park, S.; Jayaraman, S. Wearables: Fundamentals, Advancements, and a Roadmap for the Future. In Wearable Sensors, 2nd ed.; Academic Press: Oxford, UK, 2021; pp. 3–27. ISBN 978-0-12-819246-7.
- Seçkin, M.; Seçkin, A.Ç.; Gençer, Ç. Biomedical Sensors and Applications of Wearable Technologies on Arm and Hand. Biomed. Mater. Devices 2022.
- Shen, H.; Liu, T.; Qin, D.; Bo, X.; Wang, L.; Wang, F.; Yuan, Q.; Wagberg, T.; Hu, G.; Zhou, M. Chapter 7—Wearable Carbon Nanotube Devices for Sensing. In Industrial Applications of Carbon Nanotubes; Peng, H., Li, Q., Chen, T., Eds.; Micro and Nano Technologies; Elsevier: Boston, MA, USA, 2017; pp. 179–199. ISBN 978-0-323-41481-4.
- Coyle, S.; Diamond, D. Medical Applications of Smart Textiles. In Advances in Smart Medical Textiles; Woodhead Publishing Series in Textiles; Woodhead Publishing: Oxford, 2016; pp. 215–237. ISBN 978-1-78242-379-9.
- Ye, C.; Ren, J.; Wang, Y.; Zhang, W.; Qian, C.; Han, J.; Zhang, C.; Jin, K.; Buehler, M.J.; Kaplan, D.L.; et al. Design and Fabrication of Silk Templated Electronic Yarns and Applications in Multifunctional Textiles. Matter 2019, 1, 1411–1425.
- Rana, M.; Mittal, V. Wearable Sensors for Real-Time Kinematics Analysis in Sports: A Review. IEEE Sens. J. 2020, 21, 1187–1207.
- Nithya, N.; Nallavan, G. Role of Wearables in Sports Based on Activity Recognition and Biometric Parameters: A Survey. In Proceedings of the 2021 International Conference on Artificial Intelligence and Smart Systems (ICAIS), Coimbatore, India, 25–27 March 2021; pp. 1700–1705.
- Casher, C. Moneyball in the Era of Biometrics: Who Has Ownership over the Biometric Data of Professional Athletes. Dalhous. J. Leg. Stud. 2019, 28, 1.
- Garlewicz, A. Athlete Biometric Data in Soccer: Athlete Protection or Athlete Exploitation? DePaul J. Sports Law 2020, 16, ii.
- Martin, L. Chapter 37—Biometrics. In Computer and Information Security Handbook; Vacca, J.R., Ed.; Morgan Kaufmann: Boston, MA, USA, 2009; pp. 645–659. ISBN 978-0-12-374354-1.
- Shavers, B.; Bair, J. Chapter 9—Digital Identity. In Hiding Behind the Keyboard; Shavers, B., Bair, J., Eds.; Syngress: Boston, MA, USA, 2016; pp. 187–202. ISBN 978-0-12-803340-1.
- Ahsan, M.R.; Ibrahimy, M.I.; Khalifa, O.O. EMG Signal Classification for Human Computer Interaction: A Review. Eur. J. Sci. Res. 2009, 33, 480–501.
- Clarys, J.P.; Cabri, J. Electromyography and the Study of Sports Movements: A Review. J. Sports Sci. 1993, 11, 379–448.
- Taborri, J.; Keogh, J.; Kos, A.; Santuz, A.; Umek, A.; Urbanczyk, C.; van der Kruk, E.; Rossi, S. Sport Biomechanics Applications Using Inertial, Force, and EMG Sensors: A Literature Overview. Appl. Bionics Biomech. 2020, 2020, e2041549.
- Machado Leite, S.; Freitas, J.; Campelo, M.; Maciel, M.J. Electrocardiographic Evaluation in Athletes: ‘Normal’ Changes in the Athlete’s Heart and Benefits and Disadvantages of Screening. Rev. Port. Cardiol. 2016, 35, 169–177.
- Sarubbi, B.; Papaccioli, G.; Ciriello, G.D.; Russo, V.; Correra, A.; Baggish, A. Chapter 3—Electrocardiogram in Athletes. In Athlete’ s Heart; D’Andrea, A., Bossone, E., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 51–76. ISBN 978-0-323-95221-7.
- Romagnoli, S.; Ripanti, F.; Morettini, M.; Burattini, L.; Sbrollini, A. Wearable and Portable Devices for Acquisition of Cardiac Signals While Practicing Sport: A Scoping Review. Sensors 2023, 23, 3350.
- Löllgen, H.; Leyk, D. Exercise Testing in Sports Medicine. Dtsch. Ärztebl. Int. 2018, 115, 409.
- Isakadze, N.; Martin, S.S. How Useful Is the Smartwatch ECG? Trends Cardiovasc. Med. 2020, 30, 442–448.
- Sarhaddi, F.; Kazemi, K.; Azimi, I.; Cao, R.; Niela-Vilén, H.; Axelin, A.; Liljeberg, P.; Rahmani, A.M. A Comprehensive Accuracy Assessment of Samsung Smartwatch Heart Rate and Heart Rate Variability. PLoS ONE 2022, 17, e0268361.
- Thompson, T.; Steffert, T.; Ros, T.; Leach, J.; Gruzelier, J. EEG Applications for Sport and Performance. Methods 2008, 45, 279–288.
- Perrey, S.; Besson, P. Chapter 14—Studying Brain Activity in Sports Performance: Contributions and Issues. In Progress in Brain Research; Marcora, S., Sarkar, M., Eds.; Sport and the Brain: The Science of Preparing, Enduring and Winning, Part C; Elsevier: Amsterdam, The Netherlands, 2018; Volume 240, pp. 247–267.
- Casson, A.J. Wearable EEG and Beyond. Biomed. Eng. Lett. 2019, 9, 53–71.
- Chen, Y.; Lu, Y.; Zhou, C.; Wang, X. The Effects of Aerobic Exercise on Working Memory in Methamphetamine-Dependent Patients: Evidence from Combined fNIRS and ERP. Psychol. Sport Exerc. 2020, 49, 101685.
- Fu, Y.; Liu, J. System Design for Wearable Blood Oxygen Saturation and Pulse Measurement Device. Procedia Manuf. 2015, 3, 1187–1194.
- Seçkin, A.Ç. Multi-Sensor Glove Design and Bio-Signal Data Collection. Nat. Appl. Sci. J. 2021, 3, 87–93.
- Xin, Q.; Wu, J. A Novel Wearable Device for Continuous, Non-Invasion Blood Pressure Measurement. Comput. Biol. Chem. 2017, 69, 134–137.
- Ray, T.; Choi, J.; Reeder, J.; Lee, S.P.; Aranyosi, A.J.; Ghaffari, R.; Rogers, J.A. Soft, Skin-Interfaced Wearable Systems for Sports Science and Analytics. Curr. Opin. Biomed. Eng. 2019, 9, 47–56.
- Li, L.; Li, Y.; Yang, L.; Fang, F.; Yan, Z.; Sun, Q. Continuous and Accurate Blood Pressure Monitoring Based on Wearable Optical Fiber Wristband. IEEE Sens. J. 2021, 21, 3049–3057.
- Oweis, K.; Quteishat, H.; Zgoul, M.; Haddad, A. A Study on the Effect of Sports on Academic Stress Using Wearable Galvanic Skin Response. In Proceedings of the 2018 12th International Symposium on Medical Information and Communication Technology (ISMICT), Sydney, NSW, Australia, 26–28 March 2018; pp. 1–6.
- Shu, Y.-S.; Chen, Z.-X.; Lin, Y.-H.; Wu, S.-H.; Huang, W.-H.; Chiou, A.Y.-C.; Huang, C.-Y.; Hsieh, H.-Y.; Liao, F.-W.; Zou, T.-F. 26.1 A 4.5 Mm 2 Multimodal Biosensing SoC for PPG, ECG, BIOZ and GSR Acquisition in Consumer Wearable Devices. In Proceedings of the 2020 IEEE International Solid-State Circuits Conference-(ISSCC), San Francisco, CA, USA, 16–20 February 2020; pp. 400–402.
- Liaqat, S.; Dashtipour, K.; Rizwan, A.; Usman, M.; Shah, S.A.; Arshad, K.; Assaleh, K.; Ramzan, N. Personalized Wearable Electrodermal Sensing-Based Human Skin Hydration Level Detection for Sports, Health and Wellbeing. Sci. Rep. 2022, 12, 3715.
- Vanegas, E.; Igual, R.; Plaza, I. Sensing Systems for Respiration Monitoring: A Technical Systematic Review. Sensors 2020, 20, 5446.
- De Fazio, R.; Stabile, M.; De Vittorio, M.; Velázquez, R.; Visconti, P. An Overview of Wearable Piezoresistive and Inertial Sensors for Respiration Rate Monitoring. Electronics 2021, 10, 2178.
- Bernhart, S.; Harbour, E.; Jensen, U.; Finkenzeller, T. Wearable Chest Sensor for Running Stride and Respiration Detection. Sports Eng. 2022, 26, 19.
- Biometrics, C. Unlock the Data in Your Breath! Available online: https://calibrebio.com/ (accessed on 30 August 2023).
- COSMED—K5: Wearable Metabolic System for Both Laboratory and Field Testing. Available online: https://www.cosmed.com/en/products/cardio-pulmonary-exercise-test/k5 (accessed on 30 August 2023).
- METAMAX 3B. Available online: https://cortex-medical.com/EN/METAMAX-3B-en.htm (accessed on 30 August 2023).
- Macfarlane, D.J. Open-Circuit Respirometry: A Historical Review of Portable Gas Analysis Systems. Eur. J. Appl. Physiol. 2017, 117, 2369–2386.
- Escobedo, P.; Fernández-Ramos, M.D.; López-Ruiz, N.; Moyano-Rodríguez, O.; Martínez-Olmos, A.; Pérez de Vargas-Sansalvador, I.M.; Carvajal, M.A.; Capitán-Vallvey, L.F.; Palma, A.J. Smart Facemask for Wireless CO2 Monitoring. Nat. Commun. 2022, 13, 72.
- Koff, M.F. 9—Biomechanics of Peripheral Joints. In Rheumatology, 6th ed.; Hochberg, M.C., Silman, A.J., Smolen, J.S., Weinblatt, M.E., Weisman, M.H., Eds.; Mosby: Philadelphia, 2015; pp. 65–71. ISBN 978-0-323-09138-1.
- Howell, J. 12—Principles and Components of Upper Limb Orthoses. In Atlas of Orthoses and Assistive Devices, 5th ed.; Webster, J.B., Murphy, D.P., Eds.; Elsevier: Philadelphia, PA, USA, 2019; pp. 134–145.e1. ISBN 978-0-323-48323-0.
- Fonseca, J.; Ramos, V.; Amaro, J.P.; Moita, F.; Roseiro, L. Framework for Knee Joint Movement Analysis with Inertial Sensors and Recursive Filters. In Proceedings of the 2019 IEEE 6th Portuguese Meeting on Bioengineering (ENBENG), Lisbon, Portugal, 22–23 February 2019; pp. 1–4.
- Wilk, M.P.; Walsh, M.; O’Flynn, B. Multimodal Sensor Fusion for Low-Power Wearable Human Motion Tracking Systems in Sports Applications. IEEE Sens. J. 2020, 21, 5195–5212.
- Waqar, A.; Ahmad, I.; Habibi, D.; Hart, N.; Phung, Q.V. Enhancing Athlete Tracking Using Data Fusion in Wearable Technologies. IEEE Trans. Instrum. Meas. 2021, 70, 4004013.
- Beanland, E.; Main, L.C.; Aisbett, B.; Gastin, P.; Netto, K. Validation of GPS and Accelerometer Technology in Swimming. J. Sci. Med. Sport 2014, 17, 234–238.
- Kos, A.; Umek, A. Wearable Sensor Devices for Prevention and Rehabilitation in Healthcare: Swimming Exercise with Real-Time Therapist Feedback. IEEE Internet Things J. 2019, 6, 1331–1341.
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The Use of Wearable Devices for Walking and Running Gait Analysis Outside of the Lab: A Systematic Review. Gait Posture 2018, 63, 124–138.
- Ahamed, N.U.; Kobsar, D.; Benson, L.; Clermont, C.; Kohrs, R.; Osis, S.T.; Ferber, R. Using Wearable Sensors to Classify Subject-Specific Running Biomechanical Gait Patterns Based on Changes in Environmental Weather Conditions. PLoS ONE 2018, 13, e0203839.
- Hwang, T.-H.; Reh, J.; Effenberg, A.O.; Blume, H. Validation of Real Time Gait Analysis Using a Single Head-Worn IMU. In Proceedings of the Europe-Korea Conference on Science and Technology; Springer: Singapore, 2019; pp. 87–97.
- Ashry, S.; Ogawa, T.; Gomaa, W. CHARM-Deep: Continuous Human Activity Recognition Model Based on Deep Neural Network Using IMU Sensors of Smartwatch. IEEE Sens. J. 2020, 20, 8757–8770.
- Yeo, H.-S.; Feng, W.; Huang, M.X. WATouCH: Enabling Direct Input on Non-Touchscreen Using Smartwatch’s Photoplethysmogram and IMU Sensor Fusion. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–10.
- Kos, M.; Kramberger, I. A Wearable Device and System for Movement and Biometric Data Acquisition for Sports Applications. IEEE Access 2017, 5, 6411–6420.
- Liu, Y.; Ghannam, R.; Heidari, H. Smart Multi-Sensor Wristband for Gesture Classification. In Proceedings of the IEEE UKCAS 2019, London, UK, 6 December 2019.
- Liu, W.; Long, Z.; Yang, G.; Xing, L. A Self-Powered Wearable Motion Sensor for Monitoring Volleyball Skill and Building Big Sports Data. Biosensors 2022, 12, 60.
- Gao, X.; Zheng, M.; Lv, H.; Zhang, Y.; Zhu, M.; Hou, Y. Ultrahigh Sensitive Flexible Sensor Based on Textured Piezoelectric Composites for Preventing Sports Injuries. Compos. Sci. Technol. 2022, 229, 109693.
- Kreil, M.; Ogris, G.; Lukowicz, P. Muscle Activity Evaluation Using Force Sensitive Resistors. In Proceedings of the 2008 5th International Summer School and Symposium on Medical Devices and Biosensors, Hong Kong, China, 1–3 June 2008; pp. 107–110.
- Mengüç, Y.; Park, Y.-L.; Pei, H.; Vogt, D.; Aubin, P.M.; Winchell, E.; Fluke, L.; Stirling, L.; Wood, R.J.; Walsh, C.J. Wearable Soft Sensing Suit for Human Gait Measurement. Int. J. Robot. Res. 2014, 33, 1748–1764.
- Raza, T.; Tufail, M.K.; Ali, A.; Boakye, A.; Qi, X.; Ma, Y.; Ali, A.; Qu, L.; Tian, M. Wearable and Flexible Multifunctional Sensor Based on Laser-Induced Graphene for the Sports Monitoring System. ACS Appl. Mater. Interfaces 2022, 14, 54170–54181.
- Balkhi, P.; Moallem, M. A Multipurpose Wearable Sensor-Based System for Weight Training. Automation 2022, 3, 132–152.
- Li, Q.; Dai, K.; Zhang, W.; Wang, X.; You, Z.; Zhang, H. Triboelectric Nanogenerator-Based Wearable Electronic Devices and Systems: Toward Informatization and Intelligence. Digit. Signal Process. 2021, 113, 103038.
- Li, C.; Zhu, Y.; Sun, F.; Jia, C.; Zhao, T.; Mao, Y.; Yang, H. Research Progress on Triboelectric Nanogenerator for Sports Applications. Energies 2022, 15, 5807.
- Dassanayaka, D.G.; Alves, T.M.; Wanasekara, N.D.; Dharmasena, I.G.; Ventura, J. Recent Progresses in Wearable Triboelectric Nanogenerators. Adv. Funct. Mater. 2022, 32, 2205438.
- Park, Y.-G.; Lee, G.-Y.; Jang, J.; Yun, S.M.; Kim, E.; Park, J.-U. Liquid Metal-Based Soft Electronics for Wearable Healthcare. Adv. Healthc. Mater. 2021, 10, 2002280.
- Rico-González, M.; Los Arcos, A.; Clemente, F.M.; Rojas-Valverde, D.; Pino-Ortega, J. Accuracy and Reliability of Local Positioning Systems for Measuring Sport Movement Patterns in Stadium-Scale: A Systematic Review. Appl. Sci. 2020, 10, 5994.
- Waqar, A.; Ahmad, I.; Habibi, D.; Phung, Q.V. Analysis of GPS and UWB Positioning System for Athlete Tracking. Meas. Sens. 2021, 14, 100036.
- Liu, J.; Huang, G.; Hyyppä, J.; Li, J.; Gong, X.; Jiang, X. A Survey on Location and Motion Tracking Technologies, Methodologies and Applications in Precision Sports. Expert Syst. Appl. 2023, 229, 120492.
- Szot, T.; Specht, C.; Dabrowski, P.S.; Specht, M. Comparative Analysis of Positioning Accuracy of Garmin Forerunner Wearable GNSS Receivers in Dynamic Testing. Measurement 2021, 183, 109846.
- Liu, Y. Research and Development of GNSS Wearable Device for Sports Performance Monitoring by Example of Soccer Player Analysis∗. In Proceedings of the 2022 6th International Conference on Electronic Information Technology and Computer Engineering, Xiamen, China, 21–23 October 2022; pp. 901–906.
- Pino-Ortega, J.; Rico-González, M. Review of Ultra-Wide Band in Team Sports. In Innovations in Ultra-Wideband Technologies; InechOpen: Londn, UK, 2020; pp. 93–102.
- Zhang, H.; Zhang, Z.; Gao, N.; Xiao, Y.; Meng, Z.; Li, Z. Cost-Effective Wearable Indoor Localization and Motion Analysis via the Integration of UWB and IMU. Sensors 2020, 20, 344.
- Vleugels, R.; Van Herbruggen, B.; Fontaine, J.; De Poorter, E. Ultra-Wideband Indoor Positioning and IMU-Based Activity Recognition for Ice Hockey Analytics. Sensors 2021, 21, 4650.
- Li, X.; Shen, Y.; Qu, Y.; Wu, X.; Liu, Y. Real-Time Ski Jumping Trajectory Reconstruction and Motion Analysis Using the Integration of UWB and IMU. In Proceedings of the Methods and Applications for Modeling and Simulation of Complex Systems: 21st Asia Simulation Conference, AsiaSim 2022, Changsha, China, 9–11 December 2022; Proceedings, Part I. Springer: Singapore, 2022; pp. 463–478.
- Nagymáté, G.; Kiss, R.M. Application of OptiTrack Motion Capture Systems in Human Movement Analysis: A Systematic Literature Review. Recent Innov. Mechatron. 2018, 5, 1–9.
- Wang, H.; Li, L.; Chen, H.; Li, Y.; Qiu, S.; Gravina, R. Motion Recognition for Smart Sports Based on Wearable Inertial Sensors. In Proceedings of the Body Area Networks: Smart IoT and Big Data for Intelligent Health Management, Florence, Italy, 2–3 October 2019; Mucchi, L., Hämäläinen, M., Jayousi, S., Morosi, S., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 114–124.
- Boddy, K.J.; Marsh, J.A.; Caravan, A.; Lindley, K.E.; Scheffey, J.O.; O’Connell, M.E. Exploring Wearable Sensors as an Alternative to Marker-Based Motion Capture in the Pitching Delivery. PeerJ 2019, 7, e6365.
- Li, R.T.; Kling, S.R.; Salata, M.J.; Cupp, S.A.; Sheehan, J.; Voos, J.E. Wearable Performance Devices in Sports Medicine. Sports Health 2016, 8, 74–78.
- Kamišalić, A.; Fister, I.; Turkanović, M.; Karakatič, S. Sensors and Functionalities of Non-Invasive Wrist-Wearable Devices: A Review. Sensors 2018, 18, 1714.
More
Information
Subjects:
Engineering, Electrical & Electronic; Computer Science, Hardware & Architecture; Rehabilitation
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.9K
Revisions:
5 times
(View History)
Update Date:
10 Oct 2025
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




