Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Tauseef Hussain | -- | 3336 | 2023-09-05 18:46:34 | | | |
| 2 | Tauseef Hussain | + 1 word(s) | 3337 | 2023-09-05 19:48:37 | | | | |
| 3 | Camila Xu | Meta information modification | 3337 | 2023-09-06 02:54:56 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Hussain, T.; Ullah, S.; Fernández-García, R.; Gil, I. High-Frequency Sensors. Encyclopedia. Available online: https://encyclopedia.pub/entry/48847 (accessed on 07 February 2026).
Hussain T, Ullah S, Fernández-García R, Gil I. High-Frequency Sensors. Encyclopedia. Available at: https://encyclopedia.pub/entry/48847. Accessed February 07, 2026.
Hussain, Tauseef, Sana Ullah, Raúl Fernández-García, Ignacio Gil. "High-Frequency Sensors" Encyclopedia, https://encyclopedia.pub/entry/48847 (accessed February 07, 2026).
Hussain, T., Ullah, S., Fernández-García, R., & Gil, I. (2023, September 05). High-Frequency Sensors. In Encyclopedia. https://encyclopedia.pub/entry/48847
Hussain, Tauseef, et al. "High-Frequency Sensors." Encyclopedia. Web. 05 September, 2023.
Copy Citation
Wearable sensing is an emergent technology for the monitoring of human vital signs in various fields such as health, sports, and the military. High-frequency respiration sensors offer unique advantages such as smaller size and wireless communication capabilities, making them suitable for various applications in healthcare and wearable technology. Moreover, this classification based on operating frequency is useful in the context of human safety concerning electromagnetic radiations and for the assessment of sensor systems in the presence of Electromagnetic Interference (EMI).
respiration sensors
breathing sensors
flexible sensors
wearable sensors
1. Introduction
Wearable sensing is an emergent technology for the monitoring of human vital signs in various fields such as health, sports, and the military [1][2][3]. Nowadays, these sensors have gained widespread usage for measuring vital signs in remote health care. Such sensors provide an opportunity to analyze the subject’s health at their own premises, significantly improving the possibility of adaptive medication. Consequently, this has greatly reduced the cost linked with conventional healthcare facilities [4]. Furthermore, the integration of these sensors into textile fiber and clothes for direct connectivity with the human body is employed for health monitoring [5]. Such flexible wearable sensors are able to measure several vital signs, including body temperature, blood pressure, heart rate, breathing rate, etc. [6][7][8]. While many flexible wearable respiration sensors are in their early stages of development, there are already commercially available devices such as Hexoskin and the Zephyr Bioharness etc. [9]. However, these systems are currently lacking in terms of robust analysis software, comprehensive validation studies, and standardized testing protocols.
Among the vital signs, the breathing rate holds particular significance in human physiology, as it contains a wealth of information about a person’s health condition. The normal respiratory rate for a healthy adult typically falls within the range of 12–20 breaths per minute (bpm). However, in specific situations such as high-intensity exercise, the respiratory rate may even increase to as much as 60 bpm [10]. Therefore, monitoring the abnormal respiratory rate (<6 bpm or >24 bpm) is a better predictor of mortality than the heart rate or hypertension. Generally, patients are observed physically to estimate their breathing rate by counting the chest expansion and contraction for a short period of time, which may result in false conclusions about the patient’s health [11]. Therefore, sensors that can monitor breathing in real-time have the potential to provide important diagnostic and monitoring tools for respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), and sleep apnea [12].
Furthermore, breathing rate is an important predictor for cardiac arrest, as reported in clinical studies [13][14]. Likewise, monitoring of the breathing rate is helpful for early diagnosis of respiratory illnesses such as COVID-19. In context, an estimation algorithm has been established for the detection of coronavirus owing to a correlation between abnormal breathing rate and COVID-19 infection [15]. Moreover, respiration sensors have emerged as a valuable tool for monitoring infant health in real time. These sensors facilitate the continuous assessment of respiratory patterns, enabling timely identification of irregularities and facilitating prompt medical intervention [16][17].
2. High-Frequency Sensors
High-frequency sensors offer unique advantages such as smaller size and wireless communication capabilities, making them suitable for various applications in healthcare and wearable technology. Among these sensors, antenna sensors, RFID/NFC-based sensors, metamaterial sensors, and Fiber Bragg Grating (FBG) sensors have emerged as the most promising candidates for high-frequency respiration monitoring. In the following subsections, a brief overview of each technique is presented, including its operating principle and associated challenges.
2.1. Antenna Sensors
Antenna sensors have become increasingly prominent in the last few years for the monitoring of vital signs, especially for respiration. The sensing mechanism is primarily based on two factors: chest wall movement, and displacement of air volume in the lungs. The movement of the chest wall leads to changes in the physical dimensions of the antenna, while the displacement of air volume alters the dielectric properties in the vicinity of the antenna. Both of these effects result in the variation of electrical characteristics of the antenna, such as its reflection coefficient, resonance frequency, and radiation pattern [18]. The variations in the reflection coefficient (S11) of the antenna sensor caused by breathing can be measured through a vector network analyzer (VNA) and then processed for estimation of the breath rate and pattern recognition. Of course, this scheme is limited to the laboratory and valid only as a proof of concept. Another more practical method is based on the utilization of a tuned frequency transmitter connected to an antenna sensor and monitoring of the backscatter power intensity or received signal strength indicator (RSSI) at the receiver end. The RSSI varies, as the impedance of antenna changes during breathing; therefore, the effective transmitted power varies accordingly.
Various types of flexible and wearable antenna-based respiration sensors have been developed for respiration monitoring. For instance, an embroidered meandering dipole antenna-based sensor was integrated into a commercially available t-shirt that detects resonance frequency shifts induced by chest movements during breathing [19], as shown in Figure 1a. In another study, a wearable strain sensor based on a flexible and sinusoidal dipole antenna was fabricated utilizing a conductive polymer material [20], illustrated in Figure 1b. Similarly, flexible and spiral dipole antennas have been designed using multi-material fibers for respiration monitoring [21], as shown in Figure 1c. Moreover, a low-profile fully textile antenna was used as a passive e-textile respiration sensor that relied on the interaction between the human body and the antenna to detect changes in dielectric properties induced by breathing in [22]. This antenna was implemented using a conductive fabric on a felt fabric substrate, providing simplicity and compatibility with different textiles, as shown in Figure 1d.
Commercial RF platforms such as RFID and Bluetooth have been employed for wireless sensing by utilizing the variations in the received signal strength indicator (RSSI). For instance, Patron et al. presented a sensor that employed knitted antennas and inductively coupled RFID tags for comfortable and battery-free monitoring of respiration patterns [23]. Figure 1e depicts a complete RFID-based system for the simultaneous respiration monitoring of multiple persons [24]. Likewise, a number of portable wireless communication platforms were presented in [25][26] that integrate antennas with Bluetooth modules in wearable t-shirts, as shown in Figure 1f. This enables non-invasive and contactless breath detection, with potential applications in medical diagnostics and respiratory condition monitoring.
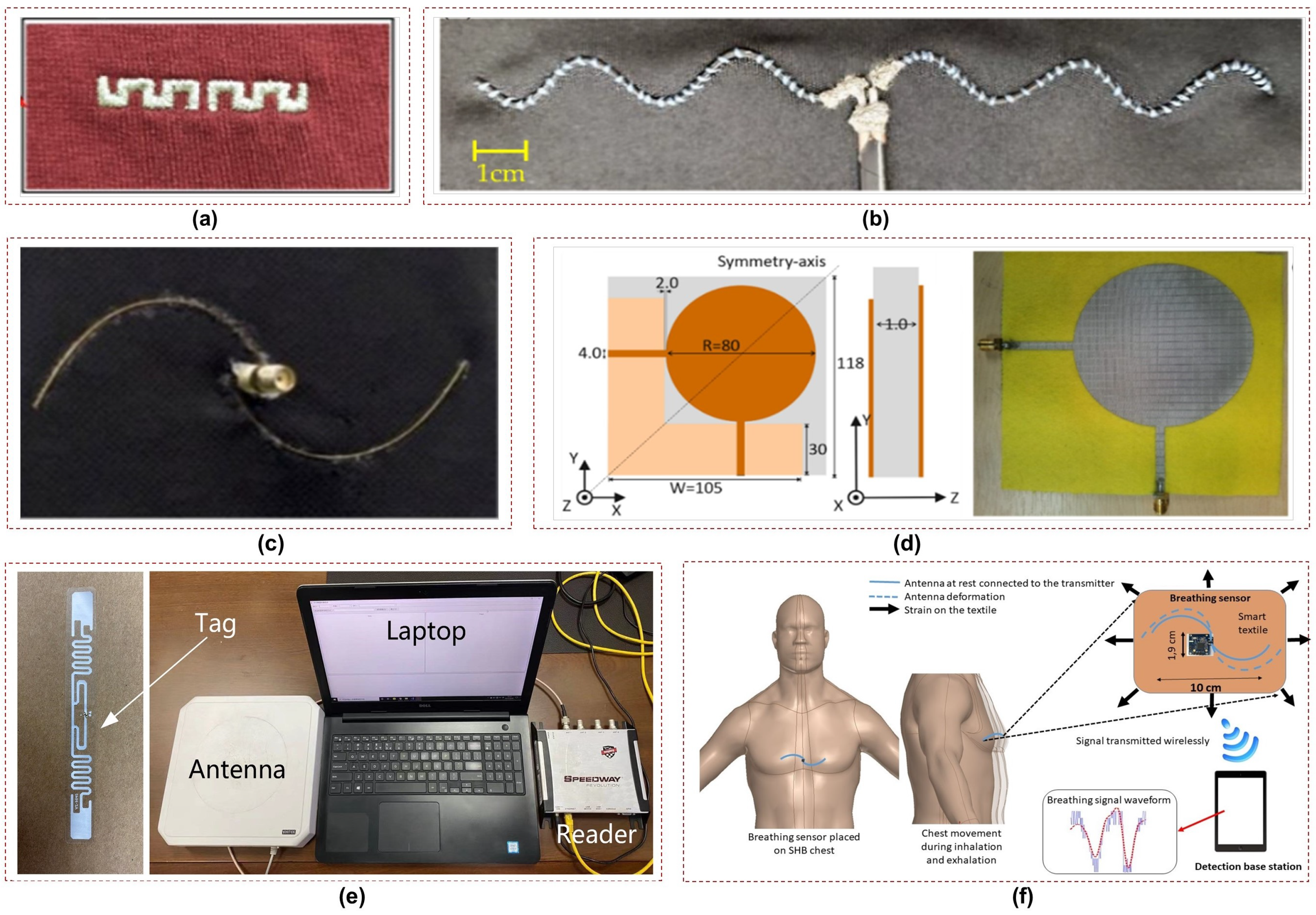
Nevertheless, the development of flexible and wearable antenna sensors is accompanied by several significant challenges. First, achieving conformity to complex surfaces such as the human body poses a key hurdle. These antennas must be able to adapt and conform to irregular and curved surfaces while maintaining reliable signal reception and transmission. Second, balancing performance and efficiency in a compact and flexible form factor is crucial, as the human body acts as a very lossy medium that absorbs and attenuates electromagnetic signals. This results in decreased antenna efficiency, reduced signal transmission range, and altered radiation patterns. Therefore, wearable antennas need to exhibit high radiation efficiency, wide bandwidth, and reliable communication capabilities by carefully tackling these challenges.
In addition, the safety of subjects is a crucial aspect to consider in the application of antenna sensors. Compliance with specific absorption rate (SAR) limits is essential to ensure the well-being of users. It can be observed from Figure 1 that dipole antennas are employed mostly for sensing in the UHF and ISM frequency bands due to their simple geometry and ease of fabrication. However, these antennas radiate a substantial amount of power toward the subject; thus, further investigation into other antenna types that have better safety features for the end users is required.
2.2. RFID/NFC Sensors
Wireless transmission of sensor data can be achieved through various technologies, including radio-frequency identification (RFID), near-field communication (NFC), and Bluetooth. However, when comparing RFID/NFC technology to Bluetooth one notable advantage is the potential for battery-free communication. The principle of operation for RFID is backscattering, where the tag receives energy from the reader’s transmission and uses it to send back a reply. In this case, the sensors can derive power from the electromagnetic (EM) field generated by a remote reader.
2.2.1. RFID Sensors
With the advent of the Internet of Things (IoT) era, radio-frequency identification devices (RFID) sensors have gained popularity for wearable sensing. In particularly, passive UHF RFID sensors have become used widely due to their small size and lack of power requirements. These sensors have the advantage of being lightweight and comfortable due to their flexible nature. Typically, RFID systems are utilized for sensing applications in two manners. The first involves the measurement of back-scattered power intensity, while the second entails the transmission of sensor data towards the reader.
For respiration measurements, RFID sensors have been mostly used as strain sensors utilizing the principle of backscattering. In this case, the main sensing element is an antenna which is specially designed according to the impedance of RFID chip and fabricated on a flexible or textile material. When a strain force is applied to an RFID tag, the physical deformation of the embedded antenna causes a shift in its resonant frequency. This results in a variation in the backscattered power (RSSI) transmitted from the passive RFID tag, which can be used as a metric for detecting mechanical deformations. Thus, RFID-based respiration sensors are designed by correlating the RSSI variation to the mechanical deformation of the RFID antenna. This approach has been demonstrated in various studies for monitoring respiration rate and detecting breathing patterns [16][23][27][28], as discussed in the previous section.
Apart from RSSI, RFID technology is utilized to transmit data from other sensors towards the reader. In a study on graphene-based respiration sensing, the AMS SL900A microchip was employed for this purpose [29]. The SL900A is an Electronic Product Code (EPC) tag that operates in both semi-passive mode (battery-assisted passive) and fully passive mode (without battery) and exhibits power sensitivities of −6.9 dBmW and −15 dBmW in these respective power modes. The EPC chip features a direct connection to the antenna along with a 10-bit analog-to-digital converter (ADC) capable of controlling two external analog sensors. Additionally, it incorporates an integrated temperature sensor with a programmable dynamic range of −40 to 150 °C. This demonstrates that a wearable RFID system with such capabilities enables simultaneous multi-parameter sensing, specifically for humidity and temperature measurements, for subsequent respiration monitoring.
2.2.2. NFC Sensors
NFC is a specific subset of RFID technology that is designed for short-range wireless systems. One significant advantage of NFC over conventional RFID is its ability to facilitate peer-to-peer communication between an NFC-based system and any NFC-enabled smartphone acting as a remote reader. This feature makes NFC technology accessible to individual users and thus expands its potential applications. Similar to RFID, the backscattering technique can be applied to NFC for sensing purposes as well.
An embroidered inductive strain sensor was introduced in [30] for respiration sensing that comprises two embroidered planar coils connected in series, with their mutual inductance being influenced by their relative positions. These coils can serve as antennas for NFC tags that modulate the carrier wave from the reader according to the inductance variations of the sensor, enabling wireless extraction of sensing information. Moreover, an NFC-based smart bandage incorporating wireless strain and temperature sensors is presented in [31]. The bandage utilizes a battery-free NFC transponder (RF430FRL152H) as an intermediary between the sensors and a smartphone application. This enables the acquisition and transmission of data from both sensors. The smartphone application can power the system and provide real-time data acquisition from the sensors at a distance of 25 mm. The authors proposed potential healthcare applications for the smart bandage, including the assessment of respiratory diseases through its usage as a wearable strain sensor.
Despite the inherent flexibility and lack of power requirements of passive RFID tags, a limitation of these tags is the inclusion of an electronic chip. This limits their large-scale production for wearable applications and renders them susceptible to harsh environmental conditions. Therefore, the future of RFID wearable sensing lies in chipless technology, which is more robust and feasible for production due to the absence of any electronic component [32].
2.3. Metamaterial Sensors
Electromagnetic metamaterials are man-made materials comprised of structures with electromagnetic properties that are deliberately engineered to offer a range of responses that are difficult or impossible to achieve in naturally occurring materials or composites. The growing popularity of metamaterials in sensing applications is evident from the increasing number of published works utilizing these engineered structures [33]. In these applications, changes in the resonance frequency or amplitude at resonance are typically used to detect variations in the measured parameter. However, it is worth noting that only a small number of studies in the existing literature have employed metamaterials to design flexible and wearable sensors for respiration monitoring.
2.3.1. Frequency Selective Surfaces
Frequency Selective Surfaces (FSS) are two-dimensional planar structures consisting of periodic arrays of sub-wavelength elements. They are designed to selectively transmit or reflect electromagnetic waves based on their frequency. FSSs are widely utilized in microwave frequency filters, radar absorbing materials (RAMs), and antenna reflectors [34]. For respiration sensing, a wireless apnea detector was proposed in [35] that utilizes a passive respiration sensor to measure the changes in airflow temperature during breathing. A transponder based on a modulated FSS is employed that uses a backscattered field technique for sensing and is composed of an array of dipoles loaded with varactor diodes. The resistance of thermal sensor changes due to the variations in airflow temperature during breathing which modulates the backscatter response. An algorithm based on peak detection has been used to calculate real-time respiration and apnea intervals. However, this system requires a battery to polarize the FSS, and it is rather uncomfortable for the patient due to the many interconnected devices worn on the face and head.
Traditional frequency selective surfaces used for sensing present certain limitations in terms of flexibility, as the materials and structures used are rigid. Therefore, liquid metal-based technologies [36] and textile-based substrates [37] are feasible options that can be explored for designing flexible metamaterials for wearable applications.
2.3.2. Spiral Resonator Tag
Planar spiral structures (SRs) are commonly used as lumped inductors in microwave circuits and serve as a fundamental element for metamaterials [38]. The inductance of a spiral is determined by its geometry (such as square, circular, or polygonal), number of turns, turn width, and spacing between turns. A breath rate sensor based on an SR tag; it is printed on a thin, flexible textile substrate suitable for wearable applications [39]. The sensor detects the respiratory movement of the abdomen during inspiration and expiration. A microstrip probing loop serves as the reader antenna and measures the variation in the real part of input impedance caused by the change in the normal distance between the probing loop and the SR tag. Thus, the respiratory rate is obtained by analyzing the amplitude-modulated signal captured by the probe. The sensor was employed to experimentally measure the breath rate of a test subject in a quasi-real scenario. To enhance the capabilities of the presented sensor, however, future advancements should focus on transitioning from quasi-real environments to a fully operational settings by integrating a signal acquisition board.
2.3.3. Surface Plasmons Resonators
Spoof localized surface plasmons (LSPs) are electromagnetic modes that are highly confined and can be realized using various techniques such as textured metal surfaces, thin metal layers, and conductive textiles [37][40][41]. These modes can be used to design wearable sensors by detecting changes in localized electromagnetic fields. Although these modes are associated with strong subwavelength confinement, which is a characteristic feature of LSP resonances, they extend into the surrounding space evanescently, enabling interactions for sensing and mode excitation.
A wearable textile sensor based on LSP resonance was proposed in [42] for vital sign monitoring such as breathing and heartbeat. The sensor is placed on the chest and excited remotely through a curved dipole antenna. Small movements of the chest during breathing and heartbeat change the resonant frequency of the sensor, which is remotely monitored from the excitation source. Moreover, an energy-efficient and secure wireless body sensor network (WBSN) interconnected through radio surface plasmons on metamaterial textiles was introduced [37]. This conductive fabric shows a three-fold improvement in transmission efficiency compared to conventional radio networks. Wireless communications remain confined to within 10 cm of the body, ensuring greater privacy and security. This textile can be used in conjunction with a range of sensors, including respiration sensors, for the monitoring of vital signs.
Resonators relying on surface plasmons generally have a very high quality factor, as the electrical field is confined in a very limited space. However, these sensors face challenges in terms of the complexity of their fabrication and sensitivity to the environment. Therefore, further research is needed to ensure their reliable performance in the context of wearable sensing.
2.4. Fiber Bragg Gratings
Fiber Bragg Grating (FBG) sensors are well suited for measuring biophysical parameters, including the respiratory behavior of the chest and abdominal regions. These sensors are comprised of a fiber optic grating that reflects a specific wavelength of light [43], as shown in Figure 2a. When the FBG undergoes strain or displacement caused by breathing, its reflected wavelength experiences a corresponding shift. This shift is directly proportional to the applied strain or displacement, enabling FBG sensors to accurately measure and monitor breathing patterns. Various applications of FBG sensors for the monitoring of vital signs are illustrated in Figure 2b, including cardiac and respiration activities [44]. Koyama et. al demonstrated in a study that FBG sensors can efficiently detect respiratory strain in the abdomen, chest, and shoulder regions [45], as shown in Figure 2c.
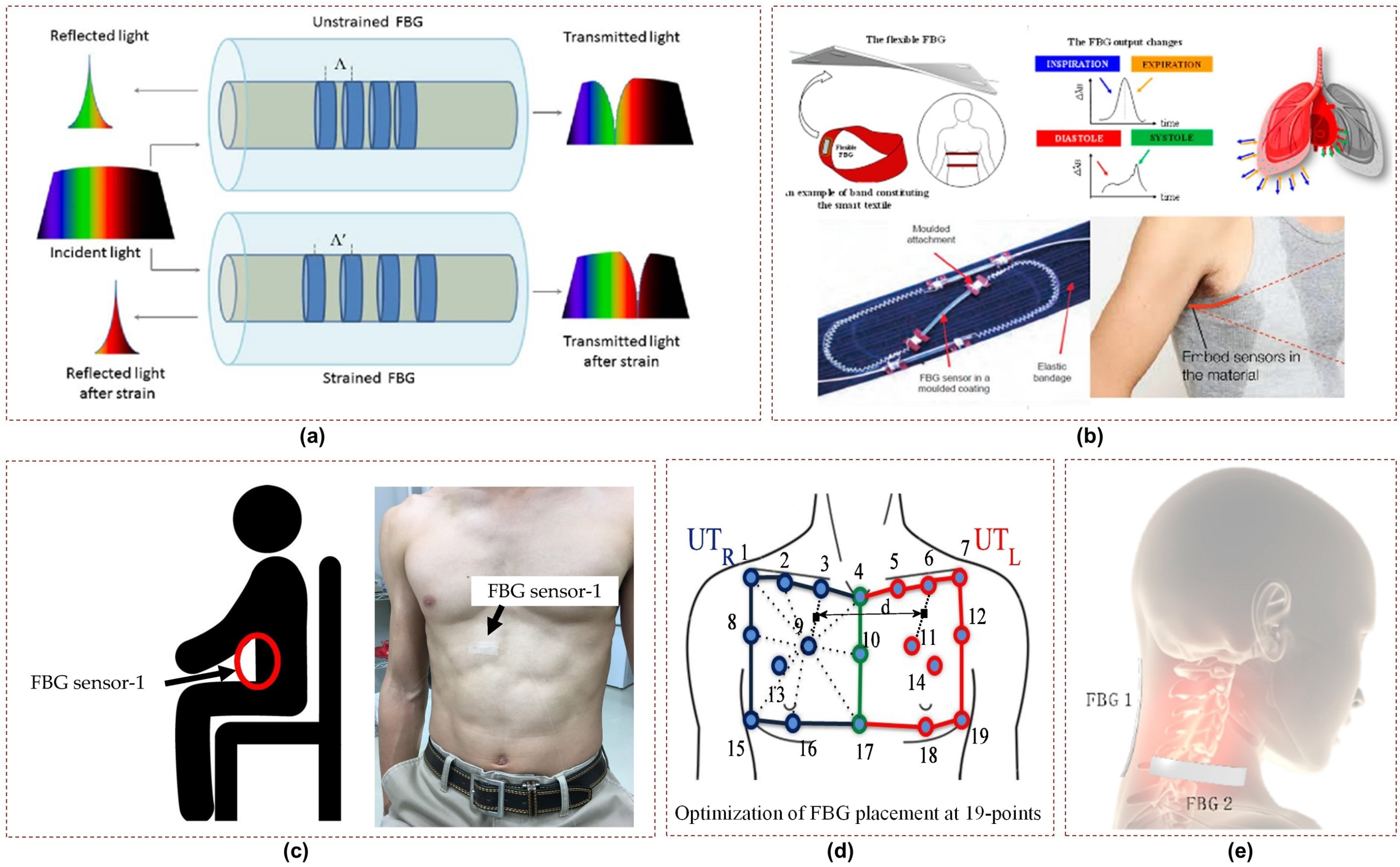
FBG sensors are especially advantageous during MRI testing thanks to their immunity to strong magnetic fields. A study focusing on the design and assessment of an MR-compatible smart textile utilized six FBGs [48]. The objective was to non-intrusively monitor and characterize a patient’s respiration. The study employed the chest wall kinematics during breathing to optimize the positioning of FBGs on the textile and improve their sensitivity in monitoring compartmental volume changes. Figure 2d illustrates a similar study in which the positioning of FBGs on the textile was determined using an optoelectronic system [46]. Another study evaluated an MR-compatible smart textile with FBG sensors for monitoring respiratory and cardiac activities during apnea and quiet breathing [49]. The results showed that accurate measurement of respiratory parameters and heart rate could be obtained without image artifacts in the MR environment.
Furthermore, elastic belts integrated with optical fibers for monitoring breathing activities were studied in [50]. The aim was to assess the impact of differences in the participants’ positions on the breathing patterns detected by the optical fibers. Experiments were conducted using FBG sensor arrays to monitor breathing patterns. Two sets of FBG arrays, each comprising five sensors, were placed at specific locations on the body, namely, the abdomen and chest. The diversity technique was employed to enhance detection accuracy. The results showed consistent accuracy for individuals, though variations were observed among the participants. In the same year, a wearable system was proposed by utilizing two FBG sensors positioned on the neck to monitor neck movements and breathing [47], as depicted in Figure 2e. This system effectively captured flexion extension, axial rotation, and respiratory frequency parameters, showing comparable performance to optical reference systems. The estimated mean and breath-by-breath respiratory frequency values exhibited errors ≤6.09% and ≤1.90% during quiet breathing and tachypnea, respectively, demonstrating high accuracy. Additionally, a 3D printed sensor using FBG technology was introduced for respiratory and heart rate monitoring in [51]. Each sensor was equipped with a single FBG fully encapsulated within a 3D-printable flexible material during printing.
The biggest challenge associated with FBG sensors is that the optical fibers are typically rigid and fragile. Therefore, they need to be encapsulated in a material that can provide protection, flexibility, and biocompatibility in order to make them suitable for flexible and wearable applications. Such encapsulation additionally shields the FBG sensor from external influences such as moisture, mechanical stress, or bending which could compromise its performance or usability.
References
- Koncar, V. Introduction to smart textiles and their applications. In Smart Textiles and Their Applications; Woodhead Publishing: Cambridge, UK, 2016; pp. 1–8.
- Morris, D.; Schazmann, B.; Wu, Y.; Coyle, S.; Brady, S.; Hayes, J.; Slater, C.; Fay, C.; Lau, K.T.; Wallace, G.; et al. Wearable sensors for monitoring sports performance and training. In Proceedings of the 2008 5th International Summer School and Symposium on Medical Devices and Biosensors, Hong Kong, China, 1–3 June 2008; pp. 121–124.
- Nayak, R.; Wang, L.; Padhye, R. Electronic textiles for military personnel. In Electronic Textiles; Woodhead Publishing: Cambridge, UK, 2015; pp. 239–256.
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130.
- Kluge, F.; Gaßner, H.; Hannink, J.; Pasluosta, C.; Klucken, J.; Eskofier, B.M. Towards Mobile Gait Analysis: Concurrent Validity and Test-Retest Reliability of an Inertial Measurement System for the Assessment of Spatio-Temporal Gait Parameters. Sensors 2017, 17, 1522.
- Kinkeldei, T.; Zysset, C.; Cherenack, K.; Tröster, G. A textile integrated sensor system for monitoring humidity and temperature. In Proceedings of the 2011 16th International Solid-State Sensors, Actuators and Microsystems Conference, Beijing, China, 5–9 June 2011; pp. 1156–1159.
- Pantelopoulos, A.; Bourbakis, N.G. A Survey on Wearable Sensor-Based Systems for Health Monitoring and Prognosis. IEEE Trans. Syst. Man Cybern. Part C 2010, 40, 1–12.
- Nemati, E.; Deen, M.J.; Mondal, T. A wireless wearable ECG sensor for long-term applications. IEEE Commun. Mag. 2012, 50, 36–43.
- Jayasekera, S.; Hensel, E.; Robinson, R. Feasibility Assessment of Wearable Respiratory Monitors for Ambulatory Inhalation Topography. Int. J. Environ. Res. Public Health 2021, 18, 2990.
- Duan, Z.; Jiang, Y.; Huang, Q.; Yuan, Z.; Zhao, Q.; Wang, S.; Zhang, Y.; Tai, H. A do-it-yourself approach to achieving a flexible pressure sensor using daily use materials. J. Mater. Chem. C 2021, 9, 13659–13667.
- L’Her, E.; N’Guyen, Q.T.; Pateau, V.; Bodenes, L.; Lellouche, F. Photoplethysmographic determination of the respiratory rate in acutely ill patients: Validation of a new algorithm and implementation into a biomedical device. Ann. Intensive Care 2019, 9, 1–10.
- Ebell, M.H. Predicting Pneumonia in Adults with Respiratory Illness. Am. Fam. Physician 2007, 76, 560–562.
- Churpek, M.M.; Yuen, T.C.; Huber, M.T.; Park, S.Y.; Hall, J.B.; Edelson, D.P. Predicting Cardiac Arrest on the Wards: A Nested Case-Control Study. Chest 2012, 141, 1170–1176.
- Mochizuki, K.; Shintani, R.; Mori, K.; Sato, T.; Sakaguchi, O.; Takeshige, K.; Nitta, K.; Imamura, H. Importance of respiratory rate for the prediction of clinical deterioration after emergency department discharge: A single-center, case–control study. Acute Med. Surg. 2017, 4, 172–178.
- Miller, D.J.; Capodilupo, J.V.; Lastella, M.; Sargent, C.; Roach, G.D.; Lee, V.H.; Capodilupo, E.R. Analyzing changes in respiratory rate to predict the risk of COVID-19 infection. PLoS ONE 2020, 15, e0243693.
- Tajin, M.A.S.; Amanatides, C.E.; Dion, G.; Dandekar, K.R. Passive UHF RFID-Based Knitted Wearable Compression Sensor. IEEE Internet Things J. 2021, 8, 13763–13773.
- Wu, Y.; Jiang, D.; Bardill, A.; Bayford, R.; Demosthenous, A. A 122 fps, 1 MHz Bandwidth Multi-Frequency Wearable EIT Belt Featuring Novel Active Electrode Architecture for Neonatal Thorax Vital Sign Monitoring. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 927–937.
- Bansal, R. Antenna theory; analysis and design. Proc. IEEE 1984, 72, 989–990.
- Gharbi, M.E.; Fernández-García, R.; Gil, I. Embroidered wearable Antenna-based sensor for Real-Time breath monitoring. Measurement 2022, 195, 111080.
- Ahadi, M.; Roudjane, M.; Dugas, M.A.; Miled, A.; Messaddeq, Y. Wearable Sensor Based on Flexible Sinusoidal Antenna for Strain Sensing Applications. Sensors 2022, 22, 4069.
- Guay, P.; Gorgutsa, S.; LaRochelle, S.; Messaddeq, Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors 2017, 17, 1050.
- Wagih, M.; Malik, O.; Weddell, A.S.; Beeby, S. E-Textile Breathing Sensor Using Fully Textile Wearable Antennas. Eng. Proc. 2022, 15, 9.
- Patron, D.; Mongan, W.; Kurzweg, T.P.; Fontecchio, A.; Dion, G.; Anday, E.K.; Dandekar, K.R. On the Use of Knitted Antennas and Inductively Coupled RFID Tags for Wearable Applications. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 1047–1057.
- Zang, C.; Zhang, C.; Zhang, M.; Niu, Q. An RFID-Based Method for Multi-Person Respiratory Monitoring. Sensors 2022, 22, 6166.
- Gharbi, M.E.; Fernández-García, R.; Gil, I. Wireless Communication Platform Based on an Embroidered Antenna-Sensor for Real-Time Breathing Detection. Sensors 2022, 22, 8667.
- Roudjane, M.; Bellemare-Rousseau, S.; Khalil, M.; Gorgutsa, S.; Miled, A.; Messaddeq, Y. A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection. Sensors 2018, 18, 973.
- Luo, C.; Gil, I.; Fernández-García, R. Electro-Textile UHF-RFID Compression Sensor for Health-Caring Applications. IEEE Sens. J. 2022, 22, 12332–12338.
- Liu, Y.; Yu, M.; Xia, B.; Wang, S.; Wang, M.; Chen, M.; Dai, S.; Wang, T.; Ye, T.T. E-Textile Battery-Less Displacement and Strain Sensor for Human Activities Tracking. IEEE Internet Things J. 2021, 8, 16486–16497.
- Caccami, M.C.; Mulla, M.Y.S.; Di Natale, C.; Marrocco, G. Wireless monitoring of breath by means of a graphene oxide-based radiofrequency identification wearable sensor. In Proceedings of the 2017 11th European Conference on Antennas and Propagation (EUCAP), Paris, France, 19–24 March 2017; pp. 3394–3396.
- Liu, Y.; Wang, M.; Yu, M.; Xia, B.; Ye, T.T. Embroidered Inductive Strain Sensor for Wearable Applications. In Proceedings of the 2020 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops), Austin, TX, USA, 23–27 March 2020; pp. 1–6.
- Escobedo, P.; Bhattacharjee, M.; Nikbakhtnasrabadi, F.; Dahiya, R. Smart Bandage With Wireless Strain and Temperature Sensors and Batteryless NFC Tag. IEEE Internet Things J. 2021, 8, 5093–5100.
- Behera, S.K. Chipless RFID Sensors for Wearable Applications: A Review. IEEE Sens. J. 2022, 22, 1105–1120.
- Chen, T.; Li, S.; Sun, H. Metamaterials Application in Sensing. Sensors 2012, 12, 2742–2765.
- Munk, B.A. Frequency Selective Surfaces: Theory and Design; John Wiley & Sons: Hoboken, NJ, USA, 2005.
- Milici, S.; Lorenzo, J.; Lázaro, A.; Villarino, R.; Girbau, D. Wireless Breathing Sensor Based on Wearable Modulated Frequency Selective Surface. IEEE Sens. J. 2017, 17, 1285–1292.
- Ren, Y.; Sun, X.; Liu, J. Advances in Liquid Metal-Enabled Flexible and Wearable Sensors. Micromachines 2020, 11, 200.
- Tian, X.; Lee, P.M.; Tan, Y.J.; Wu, T.L.Y.; Yao, H.; Zhang, M.; Li, Z.; Ng, K.A.; Tee, B.C.K.; Ho, J.S. Wireless body sensor networks based on metamaterial textiles. Nat. Electron. 2019, 2, 243–251.
- Elgeziry, M.; Costa, F.; Genovesi, S. Design Guidelines for Sensors Based on Spiral Resonators. Sensors 2022, 22, 2071.
- Elgeziry, M.; Costa, F.; Tognetti, A.; Genovesi, S. Wearable Textile-Based Sensor Tag for Breath Rate Measurement. IEEE Sens. J. 2022, 22, 22610–22619.
- Shen, X.; Cui, T.J. Ultrathin plasmonic metamaterial for spoof localized surface plasmons. Laser Photonics Rev. 2014, 8, 137–145.
- Pors, A.; Moreno, E.; Martin-Moreno, L.; Pendry, J.B.; Garcia-Vidal, F.J. Localized Spoof Plasmons Arise while Texturing Closed Surfaces. Phys. Rev. Lett. 2012, 108, 223905.
- Yang, X.; Tian, X.; Ho, J.S. Wearable Radio-frequency Plasmonic Resonance Sensor for Non-contact Vital Sign Monitoring. In Proceedings of the 2021 IEEE International Symposium on Antennas and Propagation and USNC-URSI Radio Science Meeting (APS/URSI), Singapore, 4–10 December 2021; pp. 1261–1262.
- Massaroni, C.; Saccomandi, P.; Schena, E. Medical smart textiles based on fiber optic technology: An overview. J. Funct. Biomater. 2015, 6, 204–221.
- Perezcampos Mayoral, C.; Gutiérrez Gutiérrez, J.; Cano Pérez, J.L.; Vargas Treviño, M.; Gallegos Velasco, I.B.; Hernández Cruz, P.A.; Torres Rosas, R.; Tepech Carrillo, L.; Arnaud Ríos, J.; Apreza, E.L.; et al. Fiber optic sensors for vital signs monitoring. A review of its practicality in the health field. Biosensors 2021, 11, 58.
- Koyama, S.; Fujimoto, A.; Yasuda, Y.; Satou, Y. Verification of the Propagation Range of Respiratory Strain Using Signal Waveform Measured by FBG Sensors. Sensors 2020, 20, 7076.
- Ciocchetti, M.; Massaroni, C.; Saccomandi, P.; Caponero, M.A.; Polimadei, A.; Formica, D.; Schena, E. Smart textile based on fiber bragg grating sensors for respiratory monitoring: Design and preliminary trials. Biosensors 2015, 5, 602–615.
- Presti, D.L.; Carnevale, A.; D’Abbraccio, J.; Massari, L.; Massaroni, C.; Sabbadini, R.; Zaltieri, M.; Tocco, J.D.; Bravi, M.; Miccinilli, S.; et al. A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers. Sensors 2020, 20, 536.
- Massaroni, C.; Saccomandi, P.; Formica, D.; Presti, D.L.; Caponero, M.A.; Tomaso, G.D.; Giurazza, F.; Muto, M.; Schena, E. Design and Feasibility Assessment of a Magnetic Resonance-Compatible Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring. IEEE Sens. J. 2016, 16, 8103–8110.
- Lo Presti, D.; Massaroni, C.; Formica, D.; Giurazza, F.; Schena, E.; Saccomandi, P.; Caponero, M.A.; Muto, M. Respiratory and cardiac rates monitoring during MR examination by a sensorized smart textile. In Proceedings of the 2017 IEEE International Instrumentation and Measurement Technology Conference (I2MTC), Turin, Italy, 22–25 May 2017; pp. 1–6.
- Issatayeva, A.; Beisenova, A.; Tosi, D.; Molardi, C. Fiber-Optic Based Smart Textiles for Real-Time Monitoring of Breathing Rate. Sensors 2020, 20, 3408.
- Tavares, C.; Leitão, C.; Presti, D.L.; Domingues, M.F.; Alberto, N.; Silva, H.; Antunes, P. Respiratory and heart rate monitoring using an FBG 3D-printed wearable system. Biomed. Opt. Express BOE 2022, 13, 2299–2311.
More
Information
Subjects:
Engineering, Biomedical
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
848
Revisions:
3 times
(View History)
Update Date:
06 Sep 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




