Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Catherine Marie Wroclawski | -- | 1830 | 2023-08-16 23:03:10 | | | |
| 2 | Camila Xu | Meta information modification | 1830 | 2023-08-17 02:49:22 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Wroclawski, C.; Mediratta, J.K.; Fillmore, W.J. Temporomandibular Joint Disorder Epidemiology. Encyclopedia. Available online: https://encyclopedia.pub/entry/48144 (accessed on 10 January 2026).
Wroclawski C, Mediratta JK, Fillmore WJ. Temporomandibular Joint Disorder Epidemiology. Encyclopedia. Available at: https://encyclopedia.pub/entry/48144. Accessed January 10, 2026.
Wroclawski, Catherine, Jai Kumar Mediratta, W. Jonathan Fillmore. "Temporomandibular Joint Disorder Epidemiology" Encyclopedia, https://encyclopedia.pub/entry/48144 (accessed January 10, 2026).
Wroclawski, C., Mediratta, J.K., & Fillmore, W.J. (2023, August 16). Temporomandibular Joint Disorder Epidemiology. In Encyclopedia. https://encyclopedia.pub/entry/48144
Wroclawski, Catherine, et al. "Temporomandibular Joint Disorder Epidemiology." Encyclopedia. Web. 16 August, 2023.
Copy Citation
Temporomandibular disorders of all varieties affect people in every culture on every continent, affecting up to 11% of children and even as high as 31% of adults.
temporomandibular joint
TMJ
surgery
arthroscopy
1. Introduction
Temporomandibular disorders of all varieties affect people in every culture on every continent, affecting up to 11% of children and even as high as 31% of adults [1]. While most patients experience relief or at least a significant improvement in symptoms with noninvasive treatments, surgical care may be warranted in refractory cases or frank arthritic disease, among other scenarios.
A surgeon’s management of temporomandibular disorders has progressed over the last several years. This is due, in large part, to advances in understanding pathophysiology, epidemiology, and both surgical techniques and technologies. While this is the case for TMJ surgery, advances in the foundational understanding of the disease state have also brought significant benefits to patients and surgeons alike, leading to better outcomes through better patient selection for surgical intervention, among other modes of care.
A basic understanding of TMD-related epidemiology has helped surgeons appreciate and apply more holistic and collaborative care models as well as recognize patient cohorts who may be more likely to experience favorable outcomes through surgical intervention. Similarly, the last several years have seen a renewed understanding of TMJ involvement in patients with juvenile idiopathic arthritis (JIA). Through improved understanding, consensus diagnostics, imaging, and treatment protocols aim to improve patient outcomes. On the technical side, arthroscopic TMJ surgery has also seen a proliferation of advocates and techniques, particularly with regard to arthroscopic disc repositioning. Additionally, recent investigations have helped identify additional treatments for recurrent TMJ dislocation. Finally, while prosthetic TMJ reconstruction (TMJR) has been firmly established as a safe and effective technique for the treatment of many severe conditions [2], new frontiers of the application of this technology have been opened through the use of extended TMJR prostheses.
While not exhaustive, these areas of recent progress represent important advances for surgeons treating the TMJ, about which they should certainly be aware to provide current and optimal care for their patients (Figure 1).
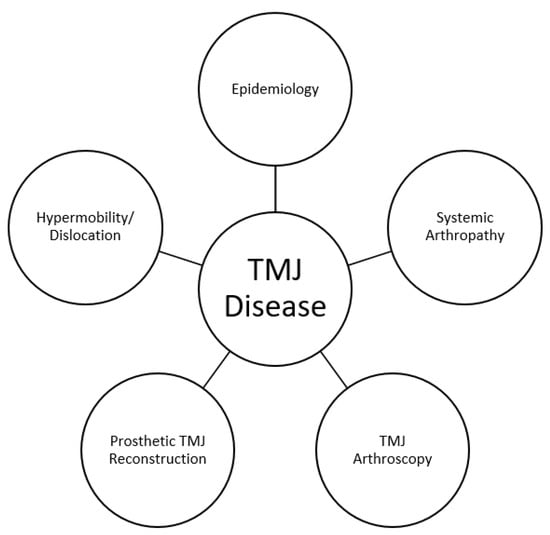
Figure 1. Areas of recent advances impacting surgical management of TMD.
2. TMD Epidemiology: The OPPERA Study
The Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) study is a landmark longitudinal study of temporomandibular disorders (TMDs), with its first publication beginning in 2011 [3]. It aimed to improve the understanding of orofacial pain and TMD by identifying risk factors, clarifying pain mechanisms, assessing treatment outcomes, and examining psychosocial contributions to the disease, among other metrics. Unlike previous studies that primarily used cross-sectional designs and convenience samples, OPPERA overcame this limitation by employing a prospective cohort study with a multi-site approach. It has provided valuable insights into TMD prevalence, demographic trends, the role of jaw headaches and injury as risk factors, and the differentiation between primary headaches and TMD-related secondary headaches, among other findings. Furthermore, the study has facilitated the identification of phenotypical clusters, allowing for a more targeted and comprehensive approach to TMD management in clinical practice. While well known among those involved in headache and facial pain treatment, the authors believe these studies are vastly underrecognized and underutilized in the surgical community.
The OPPERA-I study, conducted between May 2006 and May 2013, included a total of 4346 subjects with an age range of 18–44 living in Baltimore, MD; Buffalo, NY; Chapel Hill, NC; and Gainsville, FL, who were studied between 2006 and 2013. There were three study designs utilized: a prospective cohort study, a case-control study, and a nested case-control study. Between December 2014 and May 2016, the OPPERA-2 study was conducted, connecting with subjects who had not previously withdrawn from OPPERA-1. For individuals who provided consent and participated in the research clinics during OPPERA-2, data was gathered through clinical examinations, quantitative sensory testing, blood samples, and self-reported questionnaires.
2.1. Demographics
One of OPPERA’s major strengths is its study design. For example, in 1993, Bush et al. identified that TMD has a higher prevalence in females than in males [4], with LeResche further characterizing TMD as affecting young and middle-aged adults in 1997 [5]. However, the initial findings of the OPPERA studies revealed that TMD is prevalent in the US, with 4% of the population developing TMD on an annual basis [6]. Slade et al. also published the initial findings of the OPPERA study in 2011 revealing the key demographic data [3]. TMD is highest in patients aged 35–44 (7%) and lowest in patients aged 18–24 (3%). Females are four times more likely to suffer from TMD than men, while African Americans and Hispanics had one-fifth odds of developing TMD compared to non-Hispanic Whites. However, Kim et al. performed a cross-sectional study utilizing the OPPERA database, showing that for both Asians and African Americans compared to non-Hispanic Whites, pain catastrophizing played a significant role in mediating the association between race and pain-related measures [7]. Further, compared to healthy individuals, patients with TMD have higher levels of pain-related disability, and it is well established that catastrophizing is a strong predictor of TMD, as are psychosocial stress, affective distress, and somatic symptoms overall [8]. It is crucial to consider these factors appropriately when treatment planning potential surgical candidates.
2.2. Role of Injury
The OPPERA study has played a pivotal role in the understanding of the development and exacerbation of TMD. Sharma et al. in 2019 sought to elucidate jaw injury as a risk factor for TMD [9]. The initial findings of the prospective cohort study showed that individuals who reported a jaw injury had a fourfold higher risk of developing TMD compared to those without an injury, either extrinsic or intrinsic. Intrinsic was defined as injury attributed to yawning or prolonged mouth opening, whereas extrinsic included tooth extraction or dental treatments; oral intubation; sports injury (including falls, bumps, and blows); motor vehicle accidents; accidents resulting in whiplash; and injuries to the shoulder, neck, and head region. Sharma et al. would expand upon their initial study to show that jaw injury significantly increased the odds of developing TMD by a factor of five after adjusting for confounding variables [10]. In both studies performed, intrinsic injuries were more prevalent than extrinsic. Despite most injuries being intrinsic, the risk of TMD increased to a similar extent irrespective of whether the injury was intrinsic or extrinsic.
2.3. Headache and Chronic Pain Conditions
The OPPERA studies shed light on the association between headaches and their role as a risk factor for TMD. Headaches that arise as a secondary symptom of TMD are distinct from primary headaches that can subsequently contribute to the development of TMD. Headaches attributed to TMD (HATMD) are well established and part of Schiffman’s diagnostic criteria for TMD [11] and was recently included in the finalized version of the International Classification of Headache Disorders—third edition (ICHD-3) [12]. In contrast, primary headaches, such as migraines or tension headaches, are known to have an independent etiology but are thought to be comorbid with TMD. Tchivileva et al. utilized the OPPERA data to show that baseline reports of migraine, as well as frequent headaches, served as risk factors for developing TMD [13]. The association between migraines and TMD is unsurprising when considering the shared anatomical pathway of the trigeminal nerve between migraines and TMD [14]. Tchivileva et al. later showed that not only is the baseline presentation of a migraine a risk factor but that HATMD typically presents as migraine dominating. Sonia et al. sought to define characteristics that distinguish a headache that is comorbid with temporomandibular disorder from a HATMD. Utilizing the data from the OPPERA II study, they showed that the more severe the masticatory system pain with a patient, the more likely the headache was secondary to HATMD versus a primary headache [15].
Headache was not the only pain condition studied within the OPPERA data set. Other chronic overlapping pain conditions (COPCs) often coexist with TMD and exhibit shared biopsychosocial characteristics, symptoms, and risk factors [16]. Research has shown that the overlapping of disease symptoms of COPC can be attributed to central sensitization, a mechanism involving increased synaptic efficiency that affects sensory and nociceptive stimuli [17]. Slade et al. utilized the OPPERA II data set to compare the degree of overlap between TMD and other COPCs, revealing a greater overlap between musculoskeletal conditions such as fibromyalgia and chronic back pain compared to headaches and IBS [18].
2.4. Phenotypical Clusters
While the OPPERA studies have shed light on the heterogenous etiology of TMD with an anatomical focus, they have also statistically validated several risk factors seen among all chronic pain patients allowing for the development of “phenotypical clusters.” Bair et al. were the first to describe these clusters by identifying statistically distinguishable risk factor profiles that patients shared [16]. The three phenotypical clusters described were the adaptive cluster, pain-sensitive cluster (PS), and global symptoms (GS) cluster based on four validated variables: the pressure pain threshold of the trapezius muscle and its association with the subscales of anxiety, depression, and somatization, as measured by the SCL-90R questionnaire [19].
In this study, 33% belonged to the adaptive cluster, which showed minimal hypersensitivity and psychological distress. Individuals in this particular group experience milder pain, minimal psychological distress, and exhibit the lowest sensitivity to muscle pain. The pain they experience is primarily confined to the temporomandibular joint and the surrounding muscles, and they report few comorbidities or COPCs. Additionally, this group has a higher representation of men compared to women. The pain-sensitive cluster comprised 48% of participants. Individuals in this group exhibit the highest sensitivity to muscle pain, slightly elevated psychological distress, and a greater number of associated chronic pain conditions compared to the adaptive group. This group also has a slightly higher number of women compared to men. The remaining cluster, known as global symptoms, accounted for 18% of the participants in Bair’s study. Individuals in this group who have TMD experience the most intense pain and dysfunction. They exhibit a higher number of tender muscle sites and a significantly greater number of associated COPCs. Moreover, they encounter the highest levels of psychological distress among the three groups. Individuals in this group tend to have a higher incidence of jaw injuries and have experienced more traumatic events in their lives. A larger percentage of patients in this group have a history of smoking [19]. Lastly, there is a notable imbalance in gender representation, with a considerably higher proportion of women than men falling into this group.
OPPERA has improved the understanding of the epidemiology of TMD as well as the risk factors associated with the condition. By clarifying the risk factors, such as psychosocial stress, affective distress, somatic symptoms, trauma, and headaches, surgeons can better identify individuals at higher risk and develop targeted prevention strategies. The utilization of the phenotypical clustering method holds great promise for influencing clinical practice in a meaningful way as well. OPPERA has shown that, for individuals in either the PS or GS clusters, it is crucial to initiate a thorough screening for concurrent pain conditions. While there may be clear anatomic abnormalities in a potential TMJ surgical candidate, understanding and applying the findings of the OPPERA studies will help surgeons to make more clear-eyed clinical decisions, seek multidisciplinary treatment, and more thoroughly educate patients to help them understand the implications of their condition.
References
- Valesan, L.F.; Da-Cas, C.D.; Reus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453.
- Mercuri, L.G.; Neto, M.Q.; Pourzal, R. Alloplastic temporomandibular joint replacement: Present status and future perspectives of the elements of embodiment. Int. J. Oral Maxillofac. Surg. 2022, 51, 1573–1578.
- Slade, G.D.; Bair, E.; By, K.; Mulkey, F.; Baraian, C.; Rothwell, R.; Reynolds, M.; Miller, V.; Gonzalez, Y.; Gordon, S.; et al. Study methods, recruitment, sociodemographic findings, and demographic representativeness in the OPPERA study. J. Pain 2011, 12, T12–T26.
- Bush, F.M.; Harkins, S.W.; Harrington, W.G.; Price, D.D. Analysis of gender effects on pain perception and symptom presentation in temporomandibular pain. Pain 1993, 53, 73–80.
- LeResche, L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit. Rev. Oral Biol. Med. 1997, 8, 291–305.
- Slade, G.D.; Fillingim, R.B.; Sanders, A.E.; Bair, E.; Greenspan, J.D.; Ohrbach, R.; Dubner, R.; Diatchenko, L.; Smith, S.B.; Knott, C.; et al. Summary of findings from the OPPERA prospective cohort study of incidence of first-onset temporomandibular disorder: Implications and future directions. J. Pain 2013, 14, T116–T124.
- Kim, H.J.; Greenspan, J.D.; Ohrbach, R.; Fillingim, R.B.; Maixner, W.; Renn, C.L.; Johantgen, M.; Zhu, S.; Dorsey, S.G. Racial/ethnic differences in experimental pain sensitivity and associated factors-Cardiovascular responsiveness and psychological status. PLoS ONE 2019, 14, e0215534.
- Willassen, L.; Johansson, A.A.; Kvinnsland, S.; Staniszewski, K.; Berge, T.; Rosén, A. Catastrophizing Has a Better Prediction for TMD Than Other Psychometric and Experimental Pain Variable. Pain Res. Manag. 2020, 12, 7893023.
- Sharma, S.; Wactawski-Wende, J.; LaMonte, M.J.; Zhao, J.; Slade, G.D.; Bair, E.; Greenspan, J.D.; Fillingim, R.B.; Maixner, W.; Ohrbach, R. Incident injury is strongly associated with subsequent incident temporomandibular disorder: Results from the OPPERA study. Pain 2019, 160, 1551–1561.
- Sharma, S.; Ohrbach, R.; Fillingim, R.B.; Greenspan, J.D.; Slade, G. Pain Sensitivity Modifies Risk of Injury-Related Temporomandibular Disorder. J. Dent. Res. 2020, 99, 530–536.
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J. Oral Facial Pain Headache 2014, 28, 6–27.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211.
- Tchivileva, I.E.; Ohrbach, R.; Fillingim, R.B.; Greenspan, J.D.; Maixner, W.; Slade, G.D. Temporal change in headache and its contribution to the risk of developing first-onset temporomandibular disorder in the Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) study. Pain 2017, 158, 120–129.
- Chichorro, J.G.; Porreca, F.; Sessle, B. Mechanisms of craniofacial pain. Cephalalgia 2017, 37, 613–626.
- Sharma, S.; Slade, G.D.; Fillingim, R.B.; Ohrbach, R. A rose by another name? Characteristics that distinguish headache secondary to temporomandibular disorder from headache that is comorbid with temporomandibular disorder. Pain 2023, 164, 820–830.
- Bair, E.; Gaynor, S.; Slade, G.D.; Ohrbach, R.; Fillingim, R.B.; Greenspan, J.D.; Dubner, R.; Smith, S.B.; Diatchenko, L.; Maixner, W. Identification of clusters of individuals relevant to temporomandibular disorders and other chronic pain conditions: The OPPERA study. Pain 2016, 157, 1266–1278.
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15.
- Slade, G.D.; Greenspan, J.D.; Fillingim, R.B.; Maixner, W.; Sharma, S.; Ohrbach, R. Overlap of Five Chronic Pain Conditions: Temporomandibular Disorders, Headache, Back Pain, Irritable Bowel Syndrome, and Fibromyalgia. J. Oral Facial Pain Headache 2020, 34, s15–s28.
- Gaynor, S.M.; Bortsov, A.; Bair, E.; Fillingim, R.B.; Greenspan, J.D.; Ohrbach, R.; Diatchenko, L.; Nackley, A.; Tchivileva, I.E.; Whitehead, W.; et al. Phenotypic profile clustering pragmatically identifies diagnostically and mechanistically informative subgroups of chronic pain patients. Pain 2021, 162, 1528–1538.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
663
Revisions:
2 times
(View History)
Update Date:
17 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




