
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Paolo Spinnato | -- | 1565 | 2023-07-18 10:27:42 |
Video Upload Options
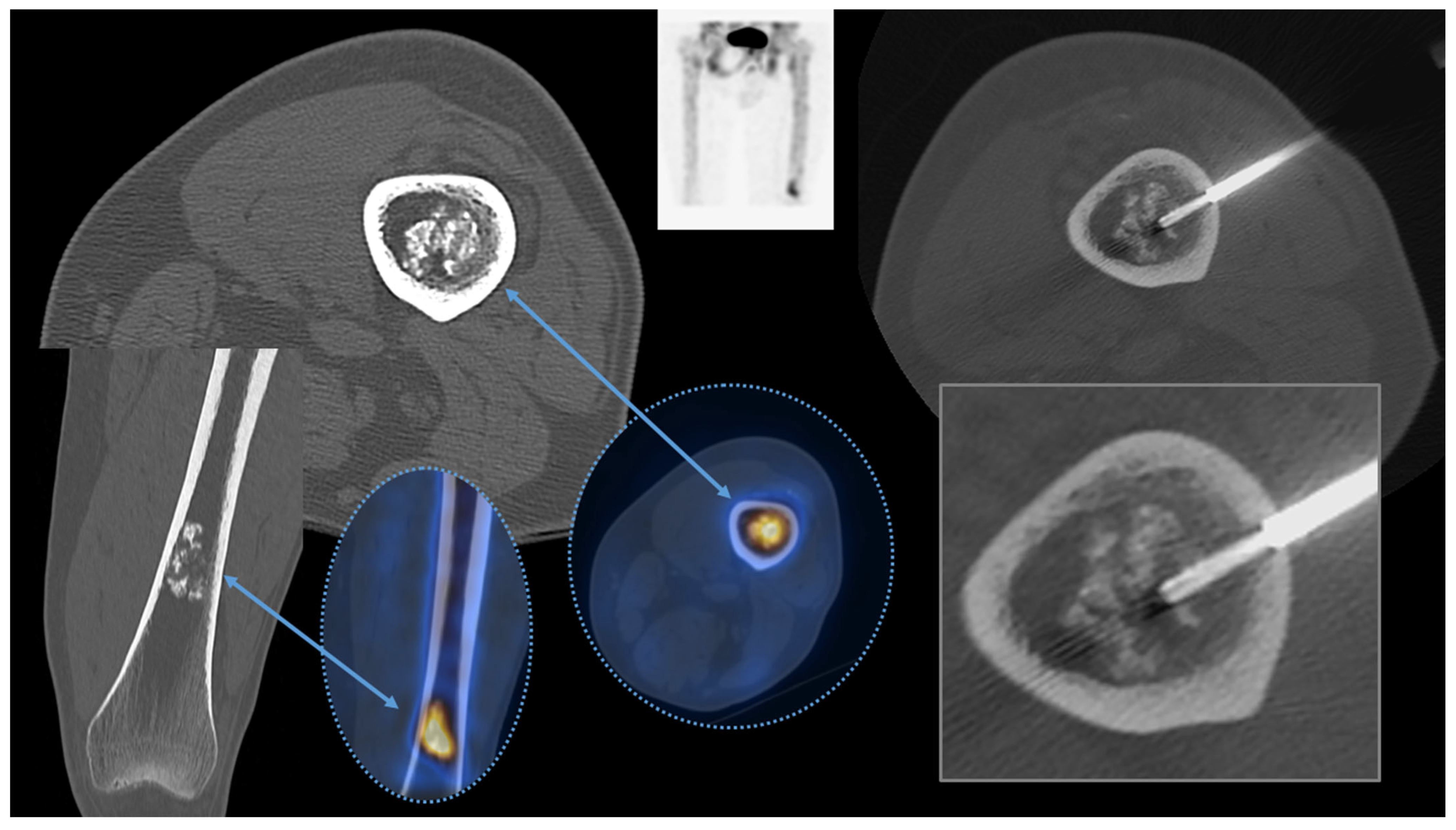
Computed tomography (CT)-guided bone biopsies are currently the diagnostic tool of choice for histopathological (and microbiological) diagnoses of skeletal lesions. Several research works have well-demonstrated their safety and feasibility in almost all skeletal regions.
1. Introduction
2. Biopsy: General Concepts
3. History
4. Image Guidance
|
Affected Skeletal Region |
Radiologic Pattern |
Imaging Guidance |
|---|---|---|
|
Appendicular skeleton |
Sclerotic pattern, osteolytic or mixed pattern without cortical disruption or intramedullary only involvement |
CT, Fluoroscopy |
|
Appendicular Skeleton |
Osteolytic or mixed pattern with cortical disruption or cortical thinning |
Ultrasound, CT, Fluoroscopy |
|
Pelvic bones |
Lesions without large extra-skeletal soft tissue involvement |
CT |
|
Pelvic bones |
Osteolytic or mixed with large soft tissue extra-skeletal involvement |
CT, Ultrasound |
|
Spine |
All |
CT |
|
Spine |
Large lesions of the vertebral body |
CT, Fluoroscopy |
|
Spine |
Large lesions with posterior extra-osseous involvement |
CT, Ultrasound |
|
Ribs |
Osteolytic or mixed pattern with cortical disruption or cortical thinning |
CT, Ultrasound |
|
Ribs |
Sclerotic pattern, osteolytic or mixed pattern without cortical disruption or intramedullary only involvement |
CT |
|
Sternum |
All |
CT |
|
Sternum |
Anterior extra-skeletal soft tissue involvement |
CT, Ultrasound |
|
Skull and Craniovertebral junction |
All |
CT |
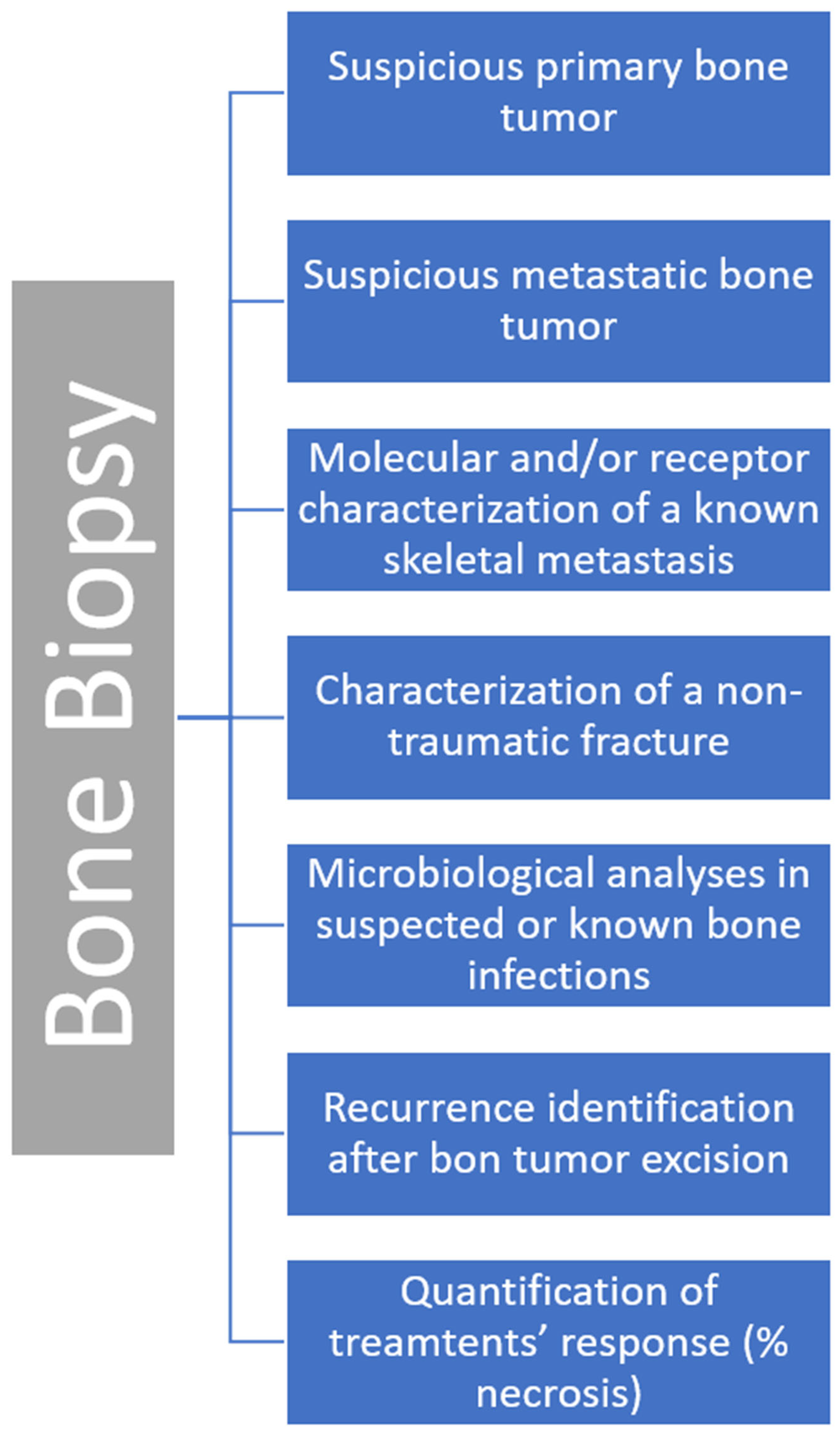
5. Clinical Indications
6. Contraindications and Complications
References
- Huang, A.J.; Kattapuram, S.V. Musculoskeletal Neoplasms: Biopsy and Intervention. Radiol. Clin. N. Am. 2011, 49, 1287–1305.
- Traina, F.; Errani, C.; Toscano, A.; Pungetti, C.; Fabbri, D.; Mazzotti, A.; Donati, D.; Faldini, C. Current concepts in the biopsy of musculoskeletal tumors. J. Bone Joint Surg. Am. 2015, 97, e7.
- Martin, H.E.; Ellis, E.B. Biopsy by needle puncture and aspiration. Ann. Surg. 1930, 92, 169–181.
- Coley, B.L.; Sharp, G.S.; Ellis, E.B. Diagnosis of bone tumors by aspiration. Am. J. Surg. 1931, 13, 215–224.
- Murphy, W.A.; Destouet, J.M.; Gilula, L.A. Percutaneous skeletal biopsy 1981: A procedure for radiologists—Results, review, and recommendations. Radiology 1981, 139, 545–549.
- Chira, R.I.; Chira, A.; Manzat-Saplacan, R.M.; Nagy, G.; Bintintan, A.; Mircea, P.A.; Valean, S. Ultrasound-guided bone lesions biopsies—A systematic review. Med. Ultrason. 2017, 19, 302–309.
- Huang, J.W.; Souza, C.; Jibri, Z.; Rakhra, K.S. Ultrasound-guided percutaneous rib biopsy: A safe procedure with high diagnostic yield. Clin. Radiol. 2019, 74, 650.e1–650.e6.
- Ponti, F.; Arioli, A.; Longo, C.; Miceli, M.; Colangeli, M.; Papalexis, N.; Spinnato, P. Ultrasound-Guided Percutaneous Bone Biopsy: Feasibility, Diagnostic Yield and Technical Notes. Diagnostics 2023, 13, 1773.
- Liu, M.; Sequeiros, R.B.; Xu, Y.; He, X.; Zhu, T.; Li, L.; Lu, Y.; Huang, J.; Li, C. MRI-guided percutaneous transpedicular biopsy of thoracic and lumbar spine using a 0.23t scanner with optical instrument tracking. J. Magn. Reson. Imaging 2015, 42, 1740–1746.
- Kovacevic, L.; Cavka, M.; Marusic, Z.; Kresic, E.; Stajduhar, A.; Grbanovic, L.; Dumic-Cule, I.; Prutki, M. Percutaneous CT-Guided Bone Lesion Biopsy for Confirmation of Bone Metastases in Patients with Breast Cancer. Diagnostics 2022, 12, 2094.
- Filippiadis, D.; Mazioti, A.; Kelekis, A. Percutaneous, Imaging-Guided Biopsy of Bone Metastases. Diagnostics 2018, 8, 25.
- Spinnato, P.; Bazzocchi, A.; Facchini, G.; Filonzi, G.; Nanni, C.; Rambaldi, I.; Rimondi, E.; Fanti, S.; Albisinni, U. Vertebral Fractures of Unknown Origin: Role of Computed Tomography-Guided Biopsy. Int. J. Spine Surg. 2018, 12, 673–679.
- Saifuddin, A.; Palloni, V.; du Preez, H.; Junaid, S.E. Review article: The current status of CT-guided needle biopsy of the spine. Skelet. Radiol. 2021, 50, 281–299.
- Sambri, A.; Spinnato, P.; Tedeschi, S.; Zamparini, E.; Fiore, M.; Zucchini, R.; Giannini, C.; Caldari, E.; Crombé, A.; Viale, P.; et al. Bone and Joint Infections: The Role of Imaging in Tailoring Diagnosis to Improve Patients’ Care. J. Pers. Med. 2021, 11, 1317.
- Spinnato, P.; Patel, D.B.; Di Carlo, M.; Bartoloni, A.; Cevolani, L.; Matcuk, G.R.; Crombé, A. Imaging of Musculoskeletal Soft-Tissue Infections in Clinical Practice: A Comprehensive Updated Review. Microorganisms 2022, 10, 2329.
- Naselli, N.; Facchini, G.; Lima, G.M.; Evangelisti, G.; Ponti, F.; Miceli, M.; Spinnato, P. MRI in differential diagnosis between tuberculous and pyogenic spondylodiscitis. Eur. Spine J. 2022, 31, 431–441.
- Nanni, P.; Landuzzi, L.; Manara, M.C.; Righi, A.; Nicoletti, G.; Cristalli, C.; Pasello, M.; Parra, A.; Carrabotta, M.; Ferracin, M.; et al. Bone sarcoma patient-derived xenografts are faithful and stable preclinical models for molecular and therapeutic investigations. Sci. Rep. 2019, 9, 12174.
- Crombé, A.; Kind, M.; Fadli, D.; Miceli, M.; Linck, P.-A.; Bianchi, G.; Sambri, A.; Spinnato, P. Soft-tissue sarcoma in adults: Imaging appearances, pitfalls and diagnostic algorithms. Diagn. Interv. Imaging 2023, 104, 207–220.
- Spinnato, P.; Sambri, A.; Fujiwara, T.; Ceccarelli, L.; Clinca, R.; Medellin, M.R.; Paolis, M.; Donati, D.M.; Bianchi, G. Myxofibrosarcoma: Clinical and Prognostic Value of MRI Features. Curr. Med. Imaging 2021, 17, 217–224.
- Patel, I.J.; Rahim, S.; Davidson, J.C.; Hanks, S.E.; Tam, A.L.; Walker, T.G.; Wilkins, L.R.; Sarode, R.; Weinberg, I. Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions—Part II: Recommendations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J. Vasc. Interv. Radiol. 2019, 30, 1168–1184.e1.
- Rimondi, E.; Rossi, G.; Bartalena, T.; Ciminari, R.; Alberghini, M.; Ruggieri, P.; Errani, C.; Angelini, A.; Calabrò, T.; Abati, C.N.; et al. Percutaneous CT-guided biopsy of the musculoskeletal system: Results of 2027 cases. Eur. J. Radiol. 2011, 77, 34–42.




