
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jeyson Hermosilla | -- | 2982 | 2023-06-28 21:35:58 | | | |
| 2 | Jessie Wu | -68 word(s) | 2914 | 2023-06-29 05:30:12 | | | | |
| 3 | Jessie Wu | Meta information modification | 2914 | 2023-06-30 09:46:08 | | |
Video Upload Options
Burns are a major threat to public health and the economy due to their costly and laborious treatment and high susceptibility to infection. Efforts have been made recently to investigate natural bioactive compounds with potential use in wound healing.
1. Background
The importance lies in the capacities that these compounds could possess both in infection control by common and resistant microorganisms, as well as in the regeneration of the affected tissues, having in both cases low adverse effects. However, some bioactive molecules are chemically unstable, poorly soluble, and susceptible to oxidative degradation or have low bioavailability. Therefore, developing new technologies for an efficient treatment of wound healing poses a real challenge. In this context, electrospun nanofibers have gained increasing research interest because bioactive molecules can be easily loaded within the nanofiber, resulting in optimal burst control and enhanced drug stability. Additionally, the nanofibers can mimic the extracellular collagen matrix, providing a suitable highly porous structural support for growing cells that facilitate and accelerate skin burns healing.
2. Categorization and Characterization of Electrospun Fibers
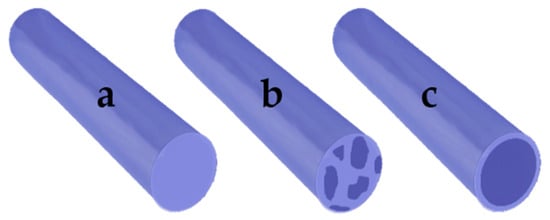
The electrospinning method consists of pumping a simple or complex polymer solution through a capillary subjected to a high-voltage electric field [1][2][3]. Due to electrostatic repulsions from the Taylor cone formed at the tip of the capillary, the polymer solution travels to a collector that may have an opposite electrical charge or be grounded [4][5]. The jet is stretched and churned as it travels to the collector, the solvent evaporates during this process, and a solid, non-woven, fibrous matrix is deposited on the collector [6]. The alignment of the fibers in the collector is random; however, methods such as rotational, magnetic, gap, or post-drawing are being studied to induce a more ordered alignment in order to expand the mechanical properties and improve a variety of physical properties [7]. Many parameters affect the electrospinning process, such as operational variables (electric field intensity, fluid flow, distance to the collector plate), properties of the solution (concentration, viscosity, electrical conductivity, voltage surface, dielectric properties), and environmental parameters such as humidity and temperature [1].
| Matrix | Encapsulated Bioactive Compound |
Electrospinning Parameters |
Diameter of Fibers |
Fiber Type |
Biological Effects of Electrospun Fibers |
Reference |
|---|---|---|---|---|---|---|
| Polyurethane | Badger (Meles meles) oil | Voltage: 20 kV Flow Rate:—L/h Distance:15 cm |
375–518 nm | Blend-composite | Antibacterial | [11] |
| Polyurethane/Silver nanoparticles (10/3% w/w) |
Olive Oil (Olea europaea L.) | Voltage: 15 kV Flow Rate:—mL/h Distance: 10 cm |
250–550 nm | Blend-composite | Antibacterial | [12] |
| Silk fibroin/Gelatin (1:3 w/w) |
Astragaloside IV | Voltage: 15 kV Flow Rate: 0.1 mL/h Distance:—cm |
_ | Blend-composite | Accelerate the process of wound healing | [13] |
| Chitosan-Deacetylated | Chitosan/L-arginine | Voltage: 28 kV Flow Rate: 1.2 mL/h Distance: 10 cm |
50–500 nm | Blend-composite | Antibacterial | [14] |
| Polycaprolactone/Gelatin (Core) (8/4% w/w) Gelatin (Shell) |
Minocycline hydrochloride G. sylvestre extracts |
Voltage: 13 kV Flow Rate: 1.2 & 1 mL/h Distance: 12 cm |
300–450 nm | Core/Shell | Antibacterial Nanofibers | [15] |
| Polylactide/Collagen (20/4% w/v) |
Fermented rooibos A. linearis extracts | Voltage: 25 kV Flow Rate: 0.1 mL/min Distance: 22 cm |
13–23 µm | Blend-composite | Antibacterial Nanofibers; Accelerate the process of wound healing |
[10] |
Chitosan |
Bromelain | Voltage: 10 kV Flow Rate: 0.5 mL/h Distance: 20 cm. |
140–360 nm | Blend-composite | Accelerate the process of wound healing |
[16] |
| Polylactide/Poly(ethylene glycol) (Core) (1:1 w/w) Polylactide/Poly(vinyl pyrrolidone) (Shell) (5:5, 7:3, 8:2, 9:1 w/w) |
Peptides HHC36 Curcumin |
Voltage: 20 kV Flow Rate:—mL/h Distance: 15 cm |
3.2–4.6 μm | Core/Shell | Antibacterial | [9] |
| Gelatin | ε-Polylysine | Voltage: 12 kV Flow Rate: 0.8 mL/h Distance: 12 cm |
425 ± 33 nm | Blend-composite | Antibacterial | [17] |
| Poly(vinyl alco-hol) | Chitosan | Voltage: 18 kV Flow Rate: 0.8 mL/h Distance: 12 cm |
130–170 nm | Blend-composite | Antibacterial | [18] |
| Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) | _ | Voltage: 8 kV Flow Rate: 0.002 mL/min Distance: 12 cm |
510–670 nm | Simple Fibers (Mono-polymer) | Accelerate the process of wound healing |
[19] |
| Silk fibroin/Poloxamer 407 (P407) (1:0, 3:1, 1:1 w/w) |
Manuka Honey |
Voltage: 25–23 kV Flow Rate: 3–4 mL/h Distance: 16.5–18 cm |
2.4–5.9 μm | Blend-composite | Antibacterial; Accelerate the process of wound healing |
[8] |
| Sodium Alginate-Poly(ethylene glycol)/Pluronic F127 (surfactant) (8:2 w/w—1.5% w/v) |
Lavender essential oil (Lavandula angustifolia) | Voltage: 25 kV Flow Rate: 0.5 mL/h Distance: 20 cm |
50–125 nm | Blend-Emulsion Electrospinning | Antibacterial Nanofibers; Accelerate the process of wound healing |
[20] |
| Polycaprolactone/Chitosan (10, 15, 20/15% w/w) |
Quercetin/Rutin | Voltage: 24–32 kV Flow Rate: 0.77 mL/h Distance: 15 cm |
90–120 nm | Blend-composite | Antibacterial Nanofibers; Accelerate the process of wound healing |
[21] |
| Chitosan/Poly(ethylene oxide) (2/0.5% w/w) |
Actinidin | Voltage:—kV Flow Rate: 0.5–1.5 mL/h Distance: 7–9 cm |
100–200 nm | Blend-composite + Actinidin enzyme immobilization |
Antibacterial Nanofibers; Accelerate the process of wound healing |
[22] |
| Gelatin (layer 1) Poly(vinyl alcohol)/Sodium Alginate (layer 2) (13/2.5% w/v) Chitosan/Poly(vinyl alcohol) (layer 3) (2/15% w/v) |
Fibrin | Voltage: 25–30 kV Flow Rate: 0.8–1.1 mL/h Distance:—cm |
150–350 nm | Blend-composite | Antibacterial Nanofibers; Accelerate the process of wound healing |
[23] |
| Polycaprolactone | α-Lactalbumin | Voltage: 9–18 kV Flow Rate: 0.3–0.6 mL/min Distance: 15 cm |
183–344 nm | Blend-composite | Accelerate the process of wound healing | [24] |
| Poly(vinyl pyrrolidone)/Keratin (3:1, 2:1, 1:1 w/w) |
Cinnamon essential oil | Voltage: 24 kV Flow Rate: 350–850 μL/h Distance: 25 cm |
315–466 nm | Blend-composite | Antibacterial Nanofibers; Accelerate the process of wound healing |
[25] |
| Polycaprolactone/Gelatin (6:4 w/w) |
Plant extracts: I. aspalathoides A. indica M. edule M. andamanica |
Voltage: 15 kV Flow Rate: 1 mL/h Distance: 12 cm |
266–601 nm | Blend-composite | Accelerate the process of wound healing |
[26] |
| Poly-D,L-lactic acid | Microalga Spirulina (Arthrospira platensis) |
Voltage: 15 kV Flow Rate: 2 mL/h Distance: 15 cm |
260–270 nm | Blend-composite | Accelerate the process of wound healing |
[27] |
| Poly(L-lactic acid)/polyhedral oligomeric silsesquioxane nanoparticles (24:1 w/w) |
Plasmid DNA Encoding Angiopoietin-1 (pAng) | Voltage: 13 kV Flow Rate: 0.8 mL/h Distance: 15 cm |
580–780 nm | Blend-composite | Accelerate the process of wound healing |
[28] |
| Polycaprolactone/Collagen (55:25 w/v) |
_ | Voltage: 13 kV Flow Rate: 3 mL/h Distance: 13 cm |
170–275 nm | Blend-composite | Accelerate the process of wound healing |
[29] |
| Poly(lactic-co-glycolic acids)/Collagen (4:1 w/w) |
_ | Voltage: 28 kV Flow Rate: 1 mL/h Distance: 17 cm |
100–300 nm | Blend-composite | Accelerate the process of wound healing |
[30] |
| Polycaprolactone (12.5% w/v) Poly(vinyl al-co-hol) (8% w/v) |
Curcumin | Voltage: 12, 18, 24 kV Flow Rate: 1, 2, 3 mL/h Distance: 16 cm |
_ | Blend-composite | Antibacterial | [31] |
3. Materials Used for Production of Electrospun Fibers
| Material Type | Material Name | Reference |
|---|---|---|
| Natural | Chitosan | [14][16][21][22][23] |
| Collagen | [10][29][30] | |
| Gelatin | [15][23][26][38][39] | |
| Keratin | [25] | |
| Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) | [19] | |
| Silk Fibroin | [13] | |
| Sodium Alginate | [20][23] | |
| Synthetic | Poly(ethylene glycol)/Poly(ethylene oxide)/Polyoxyethylene | [9][22] |
| Poly(lactic-co-glycolic acids) | [30] | |
| Poly(L-lactic acid) | [28] | |
| Poly(vinyl alcohol) | [18][23][31] | |
| Poly(vinyl pyrrolidone) | [9][25] | |
| Polycaprolactone | [15][21][24][26][29][31] | |
| Poly-D,L-lactic acid | [27] | |
| Polylactide | [9][10] | |
| Polyurethane | [11] |
3.1. Natural Materials
3.1.1. Chitosan (CH)
3.1.2. Collagen (COL)
3.1.3. Gelatin (GE)
3.1.4. Keratin
3.1.5. Poly(3-Hydroxybutyrate-co-3-Hydroxyvalerate) (PHBV)
References
- Okutan, N.; Terzi, P.; Altay, F. Affecting parameters on electrospinning process and characterization of electrospun gelatin nanofibers. Food Hydrocoll. 2014, 39, 19–26.
- Rujitanaroj, P.O.; Pimpha, N.; Supaphol, P. Wound-dressing materials with antibacterial activity from electrospun gelatin fiber mats containing silver nanoparticles. Polymer 2008, 49, 4723–4732.
- Paaver, U.; Tamm, I.; Laidmäe, I.; Lust, A.; Kirsimäe, K.; Veski, P.; Heinämäki, J. Soluplus graft copolymer: Potential novel carrier polymer in electrospinning of nanofibrous drug delivery systems for wound therapy. Biomed Res. Int. 2014, 2014, 789765.
- Kajdič, S.; Planinšek, O.; Gašperlin, M.; Kocbek, P. Electrospun nanofibers for customized drug-delivery systems. J. Drug Deliv. Sci. Technol. 2019, 51, 672–681.
- Zheng, G.; Jiang, J.; Wang, X.; Li, W.; Yu, Z.; Lin, L. High-aspect-ratio three-dimensional electrospinning via a tip guiding electrode. Mater. Des. 2021, 198, 109304.
- Vilchez, A.; Acevedo, F.; Cea, M.; Seeger, M.; Navia, R. Applications of electrospun nanofibers with antioxidant properties: A review. Nanomaterials 2020, 10, 175.
- Robinson, A.J.; Pérez-Nava, A.; Ali, S.C.; González-Campos, J.B.; Holloway, J.L.; Cosgriff-Hernandez, E.M. Comparative analysis of fiber alignment methods in electrospinning. Matter 2021, 4, 821–844.
- Kadakia, P.U.; Growney Kalaf, E.A.; Dunn, A.J.; Shornick, L.P.; Sell, S.A. Comparison of silk fibroin electrospun scaffolds with poloxamer and honey additives for burn wound applications. J. Bioact. Compat. Polym. 2018, 33, 79–94.
- Li, W.; Yu, Q.; Yao, H.; Zhu, Y.; Topham, P.D.; Yue, K.; Wang, L. Superhydrophobic hierarchical fiber/bead composite membranes for efficient treatment of burns. Acta Biomater. 2019, 92, 60–70.
- Ilomuanya, M.O.; Adebona, A.C.; Wang, W.; Sowemimo, A.; Eziegbo, C.L.; Silva, B.O.; Adeosun, S.O.; Joubert, E.; De Beer, D. Development and characterization of collagen-based electrospun scaffolds containing silver sulphadiazine and Aspalathus linearis extract for potential wound healing applications. SN Appl. Sci. 2020, 2, 1–13.
- Kim, J.H.; Unnithan, A.R.; Kim, H.J.; Tiwari, A.P.; Park, C.H.; Kim, C.S. Electrospun badger (Meles meles) oil/Ag nanoparticle based anti-bacterial mats for biomedical applications. J. Ind. Eng. Chem. 2015, 30, 254–260.
- Amina, M.; Amna, T.; Hassan, M.S.; Ibrahim, T.A.; Khil, M.S. Facile single mode electrospinning way for fabrication of natural product based silver decorated polyurethane nanofibrous membranes: Prospective medicated bandages. Colloids Surf. A: Physicochem. Eng. Asp. 2013, 425, 115–121.
- Zhang, D.; Li, L.; Shan, Y.; Xiong, J.; Hu, Z.; Zhang, Y.; Gao, J. In vivo study of silk fibroin/gelatin electrospun nanofiber dressing loaded with astragaloside IV on the effect of promoting wound healing and relieving scar. J. Drug Deliv. Sci. Technol. 2019, 52, 272–281.
- Antunes, B.P.; Moreira, A.F.; Gaspar, V.M.; Correia, I.J. Chitosan/arginine–chitosan polymer blends for assembly of nanofibrous membranes for wound regeneration. Carbohydr. Polym. 2015, 130, 104–112.
- Ramalingam, R.; Dhand, C.; Mayandi, V.; Leung, C.M.; Ezhilarasu, H.; Karuppannan, S.K.; Prasannan, P.; Ong, S.T.; Sunderasan, N.; Kaliappan, I.; et al. Core–Shell Structured Antimicrobial Nanofiber Dressings Containing Herbal Extract and Antibiotics Combination for the Prevention of Biofilms and Promotion of Cutaneous Wound Healing. ACS Appl. Mater. Interfaces 2021, 13, 24356–24369.
- Bayat, S.; Amiri, N.; Pishavar, E.; Kalalinia, F.; Movaffagh, J.; Hashemi, M. Bromelain-loaded chitosan nanofibers prepared by electrospinning method for burn wound healing in animal models. Life Sci. 2019, 229, 57–66.
- Mayandi, V.; Wen Choong, A.C.; Dhand, C.; Lim, F.P.; Aung, T.T.; Sriram, H.; Dwivedi, N.; Periayah, M.H.; Sridhar, S.; Fazil, M.H.U.T.; et al. Multifunctional antimicrobial nanofiber dressings containing ε-polylysine for the eradication of bacterial bioburden and promotion of wound healing in critically colonized wounds. ACS Appl. Mater. Interfaces 2020, 12, 15989–16005.
- Elshishiny, F.; Mamdouh, W. Fabrication of Nanofibrous/Xerogel Layer-by-Layer Biocomposite Scaffolds for Skin Tissue Regeneration: In Vitro Study. ACS Omega 2020, 5, 2133–2147.
- Sundaramurthi, D.; Krishnan, U.M.; Sethuraman, S. Epidermal differentiation of stem cells on poly (3-hydroxybutyrate-co-3-hydroxyvalerate)(PHBV) nanofibers. Ann. Biomed. Eng. 2014, 42, 2589–2599.
- Hajiali, H.; Summa, M.; Russo, D.; Armirotti, A.; Brunetti, V.; Bertorelli, R.; Mele, E. Alginate–lavender nanofibers with antibacterial and anti-inflammatory activity to effectively promote burn healing. J. Mater. Chem. B 2016, 4, 1686–1695.
- Zhou, L.; Cai, L.; Ruan, H.; Zhang, L.; Wang, J.; Jiang, H.; Wu, Y.; Feng, S.; Chen, J. Electrospun chitosan oligosaccharide/polycaprolactone nanofibers loaded with wound-healing compounds of Rutin and Quercetin as antibacterial dressings. Int. J. Biol. Macromol. 2021, 183, 1145–1154.
- Ketabchi, N.D.; Adabi, M.; Gholami, M.; Firoozi, S.; Amanzadi, B.; Faridi-Majidi, R. Study of Third-Degree Burn Wounds Debridement and Treatment by Actinidin Enzyme Immobilized on Electrospun Chitosan/PEO Nanofibers in Rats. Biointerface Res. Appl. Chem. 2021, 11, 10358–10370.
- Talukder, M.E.; Hasan, K.F.; Wang, J.; Yao, J.; Li, C.; Song, H. Novel fibrin functionalized multilayered electrospun nanofiber membrane for burn wound treatment. J. Mater. Sci. 2021, 56, 12814–12834.
- Guo, X.; Liu, Y.; Bera, H.; Zhang, H.; Chen, Y.; Cun, D.; Foderà, V.; Yang, M. α-Lactalbumin-based nanofiber dressings improve burn wound healing and reduce scarring. ACS Appl. Mater. Interfaces 2020, 12, 45702–45713.
- Kossyvaki, D.; Suarato, G.; Summa, M.; Gennari, A.; Francini, N.; Gounaki, I.; Venieri, D.; Tirelli, N.; Bertorelli, R.; Athanassiou, A.; et al. Keratin–cinnamon essential oil biocomposite fibrous patches for skin burn care. Mater. Adv. 2020, 1, 1805–1816.
- Jin, G.; Prabhakaran, M.P.; Kai, D.; Annamalai, S.K.; Arunachalam, K.D.; Ramakrishna, S. Tissue engineered plant extracts as nanofibrous wound dressing. Biomaterials 2013, 34, 724–734.
- Steffens, D.; Leonardi, D.; da Luz Soster, P.R.; Lersch, M.; Rosa, A.; Crestani, T.; Pranke, P. Development of a new nanofiber scaffold for use with stem cells in a third degree burn animal model. Burns 2014, 40, 1650–1660.
- Li, W.; Wu, D.; Zhu, S.; Liu, Z.; Luo, B.; Lu, L.; Zhou, C. Sustained release of plasmid DNA from PLLA/POSS nanofibers for angiogenic therapy. Chem. Eng. J. 2019, 365, 270–281.
- Venugopal, J.R.; Zhang, Y.; Ramakrishna, S. In vitro culture of human dermal fibroblasts on electrospun polycaprolactone collagen nanofibrous membrane. Artif. Organs 2006, 30, 440–446.
- Sadeghi-Avalshahr, A.R.; Khorsand-Ghayeni, M.; Nokhasteh, S.; Molavi, A.M.; Naderi-Meshkin, H. Synthesis and characterization of PLGA/collagen composite scaffolds as skin substitute produced by electrospinning through two different approaches. J. Mater. Sci. Mater. Med. 2017, 28, 14.
- Saeed, S.M.; Mirzadeh, H.; Zandi, M.; Barzin, J. Designing and fabrication of curcumin loaded PCL/PVA multi-layer nanofibrous electrospun structures as active wound dressing. Prog. Biomater. 2017, 6, 39–48.
- Buzgo, M.; Mickova, A.; Rampichova, M.; Doupnik, M. Blend electrospinning, coaxial electrospinning, and emulsion electrospinning techniques. In Core-Shell Nanostructures for Drug Delivery and Theranostics; Woodhead Publishing: Cambridge, UK, 2018; pp. 325–347.
- Jiang, S.; Chen, Y.; Duan, G.; Mei, C.; Greiner, A.; Agarwal, S. Electrospun nanofiber reinforced composites: A review. Polym. Chem. 2018, 9, 2685–2720.
- Lu, X.; Wang, C.; Wei, Y. One-dimensional composite nanomaterials: Synthesis by electrospinning and their applications. Small 2009, 5, 2349–2370.
- Xu, Y.; Ndayikengurukiye, J.; Akono, A.T.; Guo, P. Fabrication of fiber-reinforced polymer ceramic composites by wet electrospinning. Manuf. Lett. 2021.
- Chen, S.; Gao, J.; Yan, E.; Wang, Y.; Li, Y.; Lu, H.; Fan, L.; Wang, D.; An, Q. A novel porous composite membrane of PHA/PVA via coupling of electrospinning and spin coating for antibacterial applications. Mater. Lett. 2021, 301, 130279.
- Qin, X. Coaxial electrospinning of nanofibers. In Electrospun Nanofibers; Woodhead Publishing: Cambridge, UK, 2017; pp. 41–71.
- Pati, F.; Adhikari, B.; Dhara, S. Isolation and characterization of fish scale collagen of higher thermal stability. Bioresour. Technol. 2010, 101, 3737–3742.
- Zhang, Y.; Atala, A. Regenerative medicine of the bladder. In Principles of Regenerative Medicine, 3rd ed.; Academic Press: Waltham, MA, USA, 2019; pp. 1263–1279.
- Souza, P.R.; de Oliveira, A.C.; Vilsinski, B.H.; Kipper, M.J.; Martins, A.F. Polysaccharide-Based Materials Created by Physical Processes: From Preparation to Biomedical Applications. Pharmaceutics 2021, 13, 621.
- Shariatinia, Z. Pharmaceutical applications of chitosan. Adv. Colloid Interface Sci. 2019, 263, 131–194.
- Singer, A.J.; Taira, B.R.; Anderson, R.; McClain, S.A.; Rosenberg, L. Reepithelialization of mid-dermal porcine burns after rapid enzymatic debridement with Debrase®. J. Burn Care Res. 2011, 32, 647–653.
- Chattopadhyay, S.; Raines, R.T. Collagen-based biomaterials for wound healing. Biopolymers 2014, 101, 821–833.
- Okuyama, K.; Hongo, C.; Fukushima, R.; Wu, G.; Narita, H.; Noguchi, K.; Tanaka, Y.; Nishino, N. Crystal structures of collagen model peptides with Pro-Hyp-Gly repeating sequence at 1.26 Å resolution: Implications for proline ring puckering. Pept. Sci. Orig. Res. Biomol. 2004, 76, 367–377.
- Liu, D.; Nikoo, M.; Boran, G.Z.; Regenstein, J.M. Collagen and gelatin. Annu. Rev. Food Sci. Technol. 2015, 6, 527–557.
- Ki, C.S.; Baek, D.H.; Gang, K.D.; Lee, K.H.; Um, I.C.; Park, Y.H. Characterization of gelatin nanofiber prepared from gelatin–formic acid solution. Polymer 2005, 46, 5094–5102.
- Dhand, C.; Barathi, V.A.; Ong, S.T.; Venkatesh, M.; Harini, S.; Dwivedi, N.; Goh, E.T.L.; Nandhakumar, M.; Venugopal, J.R.; Diaz, S.M.; et al. Latent oxidative polymerization of catecholamines as potential cross-linkers for biocompatible and multifunctional biopolymer scaffolds. ACS Appl. Mater. Interfaces 2016, 8, 32266–32281.
- Slater, S.; Mitsky, T.A.; Houmiel, K.L.; Hao, M.; Reiser, S.E.; Taylor, N.B.; Tran, M.; Valentin, H.E.; Rodriguez, D.J.; Stone, D.A.; et al. Metabolic engineering of Arabidopsis and Brassica for poly (3-hydroxybutyrate-co-3-hydroxyvalerate) copolymer production. Nat. Biotechnol. 1999, 17, 1011–1016.




