Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Inês Tomada | -- | 2084 | 2023-06-26 08:42:18 | | | |
| 2 | Sirius Huang | Meta information modification | 2084 | 2023-06-28 03:01:47 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Tomada, I.; Tomada, N. Mediterranean Diet and Male Fertility. Encyclopedia. Available online: https://encyclopedia.pub/entry/46023 (accessed on 07 February 2026).
Tomada I, Tomada N. Mediterranean Diet and Male Fertility. Encyclopedia. Available at: https://encyclopedia.pub/entry/46023. Accessed February 07, 2026.
Tomada, Inês, Nuno Tomada. "Mediterranean Diet and Male Fertility" Encyclopedia, https://encyclopedia.pub/entry/46023 (accessed February 07, 2026).
Tomada, I., & Tomada, N. (2023, June 26). Mediterranean Diet and Male Fertility. In Encyclopedia. https://encyclopedia.pub/entry/46023
Tomada, Inês and Nuno Tomada. "Mediterranean Diet and Male Fertility." Encyclopedia. Web. 26 June, 2023.
Copy Citation
Diet has an impact on male reproductive potential, but few studies have focused on the specific impact of food groups or dietary patterns on fertility. Male reproductive health, as indicated by improved semen parameters and increased chances of conceiving, is associated with the Mediterranean diet, while the Western diet is considered a risk factor for male infertility.
Mediterranean diet
male fertility
sperm quality parameters
nutrition
1. Mediterranean Diet versus Western Dietary Pattern
The MedDiet encourages increased consumption of fruits, vegetables, whole grains, nuts, seafood, and low-fat dairy (Figure 1) [1]. This diet is a synonym of a restricted intake of simple carbohydrates, cholesterol, saturated and trans fats, and a higher intake of fiber, vitamins, minerals, and other non-nutritional components with potent antioxidant and anti-inflammatory properties [1].
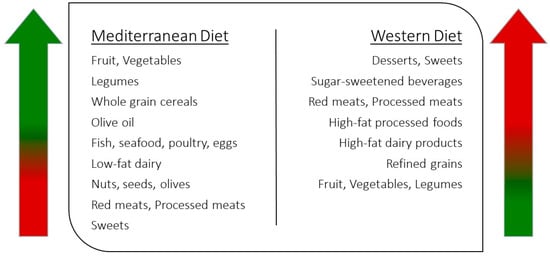
Figure 1. Characteristics of Mediterranean and Western diets.
Cutillas-Tolín and col. (2015) [2] analyzed the relationship between the MedDiet and the Western diet with semen quality parameters in 209 young and healthy men (aged 18–23 years). The researchers found that men who adhered more closely to the MedDiet had normal total sperm count and were more likely to have normal body mass index values, be non-smokers, and have a more active lifestyle [2]. In contrast, among those who preferred a daily Western dietary pattern, low sperm concentration was observed, particularly in overweight and obese men [2]. Indeed, foods included in the Western-style diet (Figure 1), such as high-fat dairy, red meats, and processed meat products (sources of saturated fat and trans fatty acids, respectively), have been inversely related to overall sperm parameters and total sperm count [3][4].
Recently, Cao and col. (2022) [5] published a systematic review and meta-analysis that aimed to explore the effects of higher and lower consumption of healthy diets, including the MedDiet, on semen quality. They found that men with greater compliance to healthy diets had the greatest sperm concentration, progressive sperm motility, and total sperm count [5]. However, other parameters, such as sperm morphology, total sperm motility, and semen volume, seemed to be similar compared to men with the lowest ingestion of healthy diets [6].
The regular intake of sugar-sweetened beverages has been associated with weight gain and obesity, which in turn increase insulin resistance and negatively affect semen quality through increased oxidative stress [7]. Lower semen volume, sperm concentration, total sperm count, and total motility have been reported among sugar-sweetened beverage consumers [7]. Since artificially sweetened beverages are not associated with weight gain and obesity itself, this type of beverage has become popular and frequently consumed in the last decades [7]. However, Meldgaard and col. (2022) [5] recently found that semen quality in young men was not significantly affected by the consumption of sugar-sweetened or artificially sweetened beverages. Nonetheless, the percentage of morphologically normal sperm was slightly lower among consumers of artificially sweetened beverages at least 3 days per week [5].
In a systematic review by Falsig and col. (2019) [8], the results from observational studies were found to be consistent with those from randomized controlled trials (RTCs) concerning the adoption of a healthy diet rich in omega-3 fatty acids (from fish and seafood) and improved semen parameters. Positive associations with omega-3 fatty acids were observed in the following parameters: reduced risk of asthenozoospermia; normal morphology; increased total sperm count, concentration, motility, and volume; and reduced sperm DNA fragmentation [8]. Additionally, some findings indicate that the consumption of foods rich in omega-3 fatty acids may also improve fecundity [9].
Fish and seafood are not the only sources of omega-3 fatty acids. Nuts, such as walnuts, hazelnuts, and almonds, are nutrient-dense foods traditionally present in the MedDiet, and are rich in omega-3 fatty acids, as well as vitamins C and E, selenium, and zinc [10]. Interestingly, in the FERTINUTS (Effect of Nut Consumption on Semen Quality and Functionality in Healthy Males) study, Salas-Huetos and col. (2018) [10] found that when young, healthy men were invited to consume a Western diet enriched with 60 g of nuts for 14 weeks, considerable improvements in total sperm count and vitality, as well as total and progressive motility and morphology of sperm were observed compared to a control group. Nut consumption was also associated with a significant reduction in sperm DNA fragmentation, which can justify these positive results in sperm parameters [10].
Over the last several decades, the Western diet has been the culprit for the growing rate of obesity, which has had a significant negative effect on fertility due to its impact on hormonal levels, sperm function, and gamete molecular composition (Figure 2) [11][12][13][14]. Despite the fact that a higher body mass index has been associated with compromised sperm production and quality [15][16], the molecular mechanisms underlying obesity and male infertility are still not totally understood [17]. Increased body fat mass has been related to impaired reproductive potential due to its effect on the molecular and physical structure of sperm [15][18][19]. Obese men are more likely to be infertile due to the larger proportion of DNA fragmentation, abnormal morphology, and low mitochondrial membrane potential, which have been linked to high levels of ROS [18][19]. Regular consumption of a Western diet is directly associated with the high prevalence of obesity and its comorbidities (such as insulin resistance and diabetes) and has also been related to low sperm quality or function [20][21]. For instance, high-energy and high-fat diets (particularly those higher in animal fat and processed foods) have been associated with testicular disruption and, thus, impairments in spermatogenesis [12].
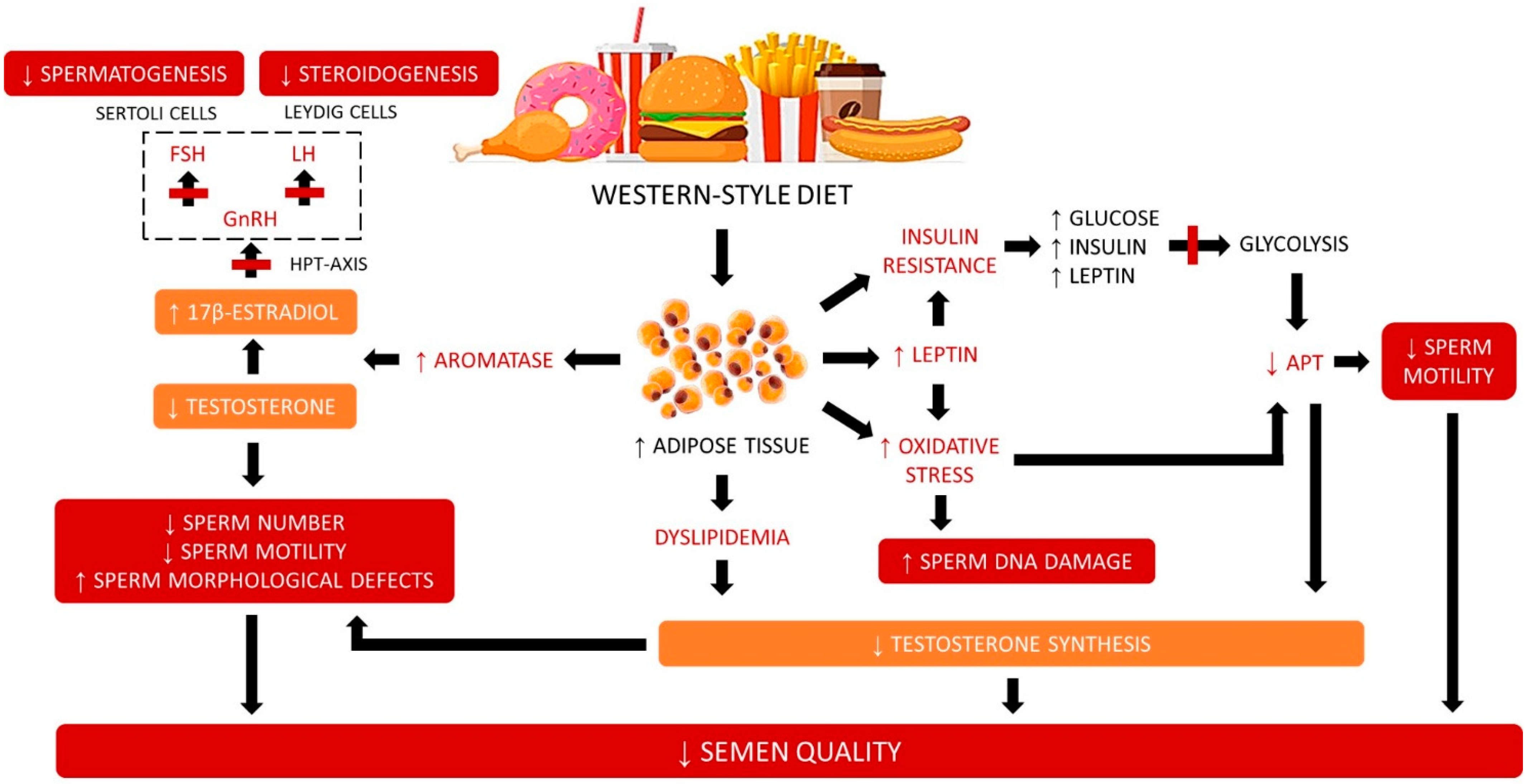
Figure 2. Effects of Western-style diet on semen quality.
The high proportion of adipose tissue is also associated with increased conversion of testosterone to estrogen (mainly through increased aromatase activity), decreased production of testosterone due to the increased secretion of leptin, and decreased gonadotrophin secretion (Figure 2) [22]. However, these conditions can potentially be reversed with diet- and exercise-induced weight loss [14][23]. Interestingly, weight-loss surgeries performed on morbidly obese men, despite inducing an increase in total testosterone and follicle-stimulating hormone levels, do not impact semen quality parameters [24]. Taken together, it seems that diet quality, but not total energy intake, may have a more noticeable impact on spermatogenesis [25].
There are many interesting interventional trials focused on the effect of increasing the intake of certain foods and/or administering specific nutritional supplements on semen quality parameters without other changes in dietary habits or lifestyle. Recently, Montano and col. (2022) [26] evaluated the outcomes of a dietary and exercise intervention on the semen quality of healthy, young, normal-weight men. The men randomly selected for the intervention group were invited to modify their habits in a relatively short time (4 months), whereas men enrolled in the control group received only general recommendations concerning a healthy lifestyle [26]. The main findings of this randomized trial, known as the “Fertilità, Ambiente, alimentazione, STile di vita” (FASt) study, showed that a lifestyle intervention based on MedDiet principles and regular exercise practice led to an increase in sperm concentration, as well as higher total and progressive motility [26]. Additionally, the proportion of spermatozoa with abnormal morphology and the number of round cells were reduced in these men. Overall, the semen quality parameters of men who modified their lifestyle by adopting a healthy diet and exercising regularly improved significantly compared to those who only received generic health advice. The authors concluded that lifestyle interventions could be paramount in healthy young men for protecting and potentially enhancing semen quality [26].
2. Mechanisms of Mediterranean Diet Effects on Semen Parameters
Adherence to the MedDiet pattern is associated with a diminished risk of low sperm concentration and total count, as previously mentioned. Although the biological mechanisms linking diet, sperm function, and fertility are not yet fully understood, potential mechanisms are discussed here.
MedDiet foods are naturally rich in nutrients with anti-inflammatory effects [27]. Chronic low-grade inflammation may affect reproduction through anatomical or functional changes in the male accessory gland and/or through direct negative effects on spermatozoa [27]. The association between adherence to the MedDiet and semen quality may also be mediated by increased intake of omega-3 fatty acids found in fish and fish oils [28], as well as in nuts [10]. Sperm and testicular cells, compared to other cells or tissues, have a higher concentration of long-chain polyunsaturated fatty acids (LC-PUFAs), particularly docosahexaenoic acid (DHA; 22:6 n-3) [8]. DHA is thought to play an important role in the regulation of membrane fluidity and spermatogenesis and is involved in acrosome reaction and sperm–oocyte fusion [8]. Several studies show that DHA levels in spermatozoa from asthenozoospermic and oligozoospermic men are significantly lower compared to normospermic men [8]. Seafood is also characterized by a high content of fat-soluble vitamins (vitamins A, D, E, and K), which play a crucial role in fertilization [9].
The typical foods of the MedDiet have a low content of saturated and trans fatty acids, two components that can trigger or worsen inflammation and thus affect semen quality [29]. The intake of trans fatty acid-rich foods, such as processed and ultra-processed foods, has been associated with disruptions in testosterone levels, testicular function, and sperm cell membrane quality [30]. Low testosterone levels and lower testicular volume have been reported among unhealthy diet consumers [31]. Furthermore, both saturated and monounsaturated fatty acids content in sperm are negatively linked to sperm motility and sperm concentration, while spermatozoa and seminal plasma DHA content could be considered as predictors of cryopreservation success (sperm DHA were associated with sperm motility and viability after freezing/thawing) [31]. Considering this, MedDiet adoption should be considered to improve overall health and male fertility.
Greater adherence to the MedDiet is significantly associated with improved semen quality, higher sperm concentration, total sperm count, and total and progressive sperm motility [32][33][34][35][36][37], as well as lower DNA fragmentation [37]. These benefits of the MedDiet on semen features are believed to be due to the high intake of fruits and vegetables rich in antioxidant vitamins (such as beta-carotene and vitamins A, C, and E), minerals (such as magnesium), and polyphenols [38]. As sperm membranes are highly sensitive to oxidative damage caused by reactive oxygen species (ROS), the benefit of this diet on semen quality may be due to the greater intake of foods naturally rich in antioxidants and carotenoids [38].
Antioxidants found in plant-based foods can play a significant role in influencing semen quality. Indeed, antioxidants are important for reproductive health, as they protect against excessive production of ROS, which can harm sperm DNA integrity, sperm cell plasma membranes, sperm quantity and function, such as motility, and sperm–oocyte fusion [39][40]. Moreover, these substances also help to prevent sperm agglutination by neutralization of hydroxyl, superoxide, and hydrogen peroxide radicals [40]. The MedDiet, which emphasizes a higher plant-food intake rich in antioxidants rather than meat and meat products, can have favorable effects on semen indicators. For instance, carotenoids have been associated with higher sperm motility in young, healthy males [38].
Men who consume a diet high in antioxidants and folate have been found to have better semen quality and less DNA damage in spermatozoa. Dark green leafy vegetables are a good source of folate, which is essential for spermatogenesis, DNA and protein synthesis, and DNA and protein methylation processes. Seminal plasma with low folate concentration is linked to sperm DNA damage, as folate shortage increases DNA fragility due to the misincorporation of uracil instead of thymine. If the removal of the misincorporated uracil fails, it can result in double-strand breaks that cause chromosome instability during normal repair processes. Folate deficiency also reduces the supply of methyl groups, which play an important role in DNA protection against damaging exposures [39]. Higher intakes of folate-rich foods, such as fruits and vegetables, have been linked to decreased DNA fragmentation and enhanced motility [41].
Berries, such as blueberries, strawberries, and raspberries, as well as grapes and red wine, are high in fiber, vitamin C, and antioxidant polyphenols. Resveratrol is a potent polyphenol found in these foods, which are typically included in the MedDiet. Several studies have demonstrated that resveratrol may be beneficial for human male fertility due to its proven antioxidant effects and positive effects on several enzymatic pathways [42]. Although the ideal concentration of daily resveratrol consumption and/or supplementation is still unknown, it is consensual that it has beneficial effects on spermatogenesis and contributes to better sperm parameters [43], particularly in obese men [44].
In recent years, multiple studies have emerged concerning the effects of gut microbiota on general health, specifically on fertility. It is well recognized that diet largely affects gut microbiota composition [44][45][46]. High intake of fat and/or simple sugars, as seen in Western-style diets, are two of the primary causes of intestinal dysbiosis. This condition results in a quantitative and qualitative imbalance of intestinal microbiota that disrupts the intestinal barrier [44]. The increased permeability of the intestinal barrier promotes chronic systemic inflammation, which further contributes to obesity and several metabolic diseases [46]. According to recent animal [47][48] and human [49] studies, a high-fat diet may also lower sperm quality by altering the gut microbiota, while modulating the gut microbiota may increase sperm quality.
References
- Tosti, V.; Bertozzi, B.; Fontana, L. Health benefits of the mediterranean diet: Metabolic and molecular mechanisms. J. Gerontol. A 2018, 73, 318–326.
- Cutillas-Tolín, A.; Mínguez-Alarcón, L.; Mendiola, J.; López-Espín, J.J.; Jørgensen, N.; Navarrete-Muñoz, E.M.; Torres-Cantero, A.M.; Chavarro, J.E. Mediterranean and western dietary patterns are related to markers of testicular function among healthy men. Hum. Reprod. 2015, 30, 2945–2955.
- Afeiche, M.C.; Williams, P.L.; Gaskins, A.J.; Mendiola, J.; Jørgensen, N.; Swan, S.H.; Chavarro, J.E. Meat intake and reproductive parameters among young men. Epidemiology 2014, 25, 323–330.
- Mendiola, J.; Torres-Cantero, A.M.; Moreno-Grau, J.M.; Ten, J.; Roca, M.; Moreno-Grau, S.; Bernabeu, R. Food intake and its relationship with semen quality: A case-control study. Fertil. Steril. 2009, 91, 812–818.
- Meldgaard, M.; Brix, N.; Gaml-Sørensen, A.; Ernst, A.; Ramlau-Hansen, C.H.; Tøttenborg, S.S.; Hougaard, K.S.; Bonde, J.P.E.; Toft, G. Consumption of sugar-sweetened or artificially sweetened beverages and semen quality in young men: A cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 682.
- Cao, L.L.; Chang, J.J.; Wang, S.J.; Li, Y.H.; Yuan, M.Y.; Wang, G.F.; Su, P.Y. The effect of healthy dietary patterns on male semen quality: A systematic review and meta-analysis. Asian J. Androl. 2022, 24, 549–557.
- Hayden, R.P.; Flannigan, R.; Schlegel, P.N. The role of lifestyle in male infertility: Diet, physical activity, and body habitus. Curr. Urol. Rep. 2018, 19, 56.
- Falsig, A.L.; Gleerup, C.S.; Knudsen, U.B. The influence of omega-3 fatty acids on semen quality markers: A systematic PRISMA review. Andrology 2019, 7, 794–803.
- Gaskins, A.J.; Sundaram, R.; Buck Louis, G.M.; Chavarro, J.E. Seafood intake, sexual activity, and time to pregnancy. J. Clin. Endocrinol. Metab. 2018, 103, 2680–2688.
- Salas-Huetos, A.; Moraleda, R.; Giardina, S.; Anton, E.; Blanco, J.; Salas-Salvadó, J.; Bulló, M. Effect of nut consumption on semen quality and functionality in healthy men consuming a Western-style diet: A randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 953–962.
- Meldrum, D.R.; Morris, M.A.; Gambone, J.C. Obesity pandemic: Causes, consequences, and solutions-but do we have the will? Fertil. Steril. 2017, 107, 833–839.
- Salas-Huetos, A.; Bulló, M.; Salas-Salvadó, J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: A systematic review of observational studies. Hum. Reprod. Update 2017, 23, 371–389.
- Salas-Huetos, A.; James, E.R.; Aston, K.I.; Jenkins, T.G.; Carrell, D.T. Diet and sperm quality: Nutrients, foods and dietary patterns. Reprod. Biol. 2019, 19, 219–224.
- Kahn, B.E.; Brannigan, R.E. Obesity and male infertility. Curr. Opin. Urol. 2017, 27, 441–445.
- Durairajanayagam, D. Lifestyle causes of male infertility. Arab. J. Urol. 2018, 16, 10–20.
- Hunter, E.; Avenell, A.; Maheshwari, A.; Stadler, G.; Best, D. The effectiveness of weight-loss lifestyle interventions for improving fertility in women and men with overweight or obesity and infertility: A systematic review update of evidence from randomized controlled trials. Obes. Rev. 2021, 22, e13325.
- Ferramosca, A.; Zara, V. Diet and Male Fertility: The impact of nutrients and antioxidants on sperm energetic metabolism. Int. J. Mol. Sci. 2022, 23, 2542.
- Lobascio, A.M.; De Felici, M.; Anibaldi, M.; Greco, P.; Minasi, M.G.; Greco, E. Involvement of seminal leukocytes, reactive oxygen species, and sperm mitochondrial membrane potential in the DNA damage of the human spermatozoa. Andrology 2015, 3, 265–270.
- Sermondade, N.; Faure, C.; Fezeu, L.; Shayeb, A.G.; Bonde, J.P.; Jensen, T.K. BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis. Hum. Reprod. Update 2013, 19, 221–231.
- Varani, J. Healthful eating, the Western style diet and chronic disease. Appro Poult. Dairy Vet. Sci. 2017, 1, 3.
- Walczak-Jedrzejowska, R.T.; Wolski, J.K.; Slowikowska-Hilczer, J. The role of oxidative stress and antioxidants in male fertility. Cent. Eur. J. Urol. 2013, 66, 60–67.
- Palmer, N.O.; Bakos, H.W.; Fullston, T.; Lane, M. Impact of obesity on male fertility, sperm function and molecular composition. Spermatogenesis 2012, 2, 253–263.
- Hakonsen, L.B.; Thulstrup, A.M.; Aggerholm, A.S.; Olsen, J.; Bonde, J.P.; Andersen, C.Y.; Bungum, M.; Ernst, E.H.; Hansen, M.L.; Ernst, E.H.; et al. Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men. Reprod. Health 2011, 8, 24.
- Reis, L.O.; Zani, E.L.; Saad, R.D.; Chaim, E.A.; de Oliveira, L.C.; Fregonesi, A. Bariatric surgery does not interfere with sperm quality—A preliminary long-term study. Reprod. Sci. 2012, 19, 1057–1062.
- Rato, L.; Alves, M.G.; Cavaco, J.E.; Oliveira, P.F. High-energy diets: A threat for male fertility? Obes. Rev. 2014, 15, 996–1007.
- Montano, L.; Ceretti, E.; Donato, F.; Bergamo, P.; Zani, C.; Viola, G.C.V.; Notari, T.; Pappalardo, S.; Zani, D.; Ubaldi, S.; et al. Effects of a lifestyle change intervention on semen quality in healthy young men living in highly polluted areas in Italy: The FASt randomized controlled trial. Eur. Urol. Focus 2022, 8, 351–359.
- La Vignera, S.; Condorelli, R.A.; Vicari, E.; Tumino, D.; Morgia, G.; Favilla, V.; Cimino, S.; Calogero, A.E. Markers of semen inflammation: Supplementary semen analysis? J. Reprod. Immunol. 2013, 100, 2–10.
- Hosseini, B.; Nourmohamadi, M.; Hajipour, S.; Taghizadeh, M.; Asemi, Z.; Keshavarz, S.A.; Jafarnejad, S. The effect of omega-3 fatty acids, EPA, and/or DHA on male infertility: A systematic review and meta-analysis. J. Diet. Suppl. 2019, 16, 245–256.
- Chavarro, J.E.; Minguez-Alarcon, L.; Mendiola, J.; Cutillas-Tolin, A.; Lopez-Espin, J.J.; Torres-Cantero, A.M. Trans fatty acid intake is inversely related to total sperm count in young healthy men. Hum. Reprod. 2014, 29, 429–440.
- Minguez-Alarcon, L.; Chavarro, J.E.; Mendiola, J.; Roca, M.; Tanrikut, C.; Vioque, J.; Jørgensen, N.; Torres-Cantero, A.M. Fatty acid intake in relation to reproductive hormones and testicular volume among young healthy men. Asian J. Androl. 2017, 19, 184–190.
- Collodel, G.; Moretti, E.; Noto, D.; Corsaro, R.; Signorini, C. Oxidation of polyunsaturated fatty acids as a promising area of research in infertility. Antioxidants 2022, 19, 1002.
- Karayiannis, D.; Kontogianni, M.D.; Mendorou, C.; Douka, L.; Mastrominas, M.; Yiannakouris, N. Association between adherence to the Mediterranean diet and semen quality parameters in male partners of couples attempting fertility. Hum. Reprod. 2017, 32, 215–222.
- Salas-Huetos, A.; Babio, N.; Carrell, D.T.; Bulló, M.; Salas-Salvadó, J. Adherence to the Mediterranean diet is positively associated with sperm motility: A cross-sectional analysis. Sci. Rep. 2019, 9, 3389.
- Braga, D.P.; Halpern, G.; Figueira, R.; Setti, A.S.; Iaconelli, A.; Borges, E. Food intake and social habits in male patients and its relationship to intracytoplasmic sperm injection outcomes. Fertil. Steril. 2012, 97, 53–59.
- Jurewicz, J.; Radwan, M.; Sobala, W.; Radwan, P.; Bochenek, M.; Hanke, W. Dietary patterns and their relationship with semen quality. Am. J. Men’s Health 2018, 12, 575–583.
- Mínguez-Alarcón, L.; Mendiola, J.; López-Espín, J.J.; Sarabia-Cos, L.; Vivero-Salmerón, G.; Vioque, J.; Navarrete-Muñoz, E.M.; Torres-Cantero, A.M. Dietary intake of antioxidant nutrients is associated with semen quality in young university students. Hum. Reprod. 2012, 27, 2807–2814.
- Vujkovic, M.; de Vries, J.H.; Lindemans, J.; Macklon, N.S.; van der Spek, P.J.; Steegers, E.A.; Steegers-Theunissen, R.P. The preconception Mediterranean dietary pattern in couples undergoing in vitro fertilization/intracytoplasmic sperm injection treatment increases the chance of pregnancy. Fertil. Steril. 2010, 94, 2096–2101.
- Zareba, P.; Colaci, D.S.; Afeiche, M.; Gaskins, A.J.; Jørgensen, N.; Mendiola, J.; Swan, S.H.; Chavarro, J.E. Semen quality in relation to antioxidant intake in a healthy male population. Fertil. Steril. 2013, 100, 1572–1579.
- Boxmeer, J.C.; Smit, M.; Weber, R.F.; Lindemans, J.; Romijn, J.C.; Eijkemans, M.J.; Maklon, N.S.; Steegers-Theunissen, R.P. Seminal plasma cobalamin significantly correlates with sperm concentration in men undergoing IVF or ICSI procedures. J. Androl. 2007, 28, 521–527.
- Ahmadi, S.; Bashiri, R.; Ghadiri-Anari, A.; Nadjarzadeh, A. Antioxidant supplements and semen parameters: An evidence based review. Int. J. Reprod. Biomed. 2016, 14, 729–736.
- Oostingh, E.C.; Steegers-Theunissen, R.P.M.; de Vries, J.H.M.; Laven, J.S.E.; Koster, M.P.H. Strong adherence to a healthy dietary pattern is associated with better semen quality, especially in men with poor semen quality. Fertil. Steril. 2017, 107, 916–923.
- Illiano, E.; Trama, F.; Zucchi, A.; Iannitti, R.G.; Fioretti, B.; Costantini, E. Resveratrol-based multivitamin supplement increases sperm concentration and motility in idiopathic male infertility: A pilot clinical study. J. Clin. Med. 2020, 9, 4017.
- Mongioì, L.M.; Perelli, S.; Condorelli, R.A.; Barbagallo, F.; Crafa, A.; Cannarella, R.; La Vignera, S.; Calogero, A.E. The role of resveratrol in human male fertility. Molecules 2021, 26, 2495.
- Bibbo, S.; Ianiro, G.; Giorgio, V.; Scaldaferri, F.; Masucci, L.; Gasbarrini, A.; Cammarota, G. The role of diet on gut microbiota composition. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4742–4749.
- Vancamelbeke, M.; Vermeire, S. The intestinal barrier: A fundamental role in health and disease. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 821–834.
- Rychter, A.; Skoracka, K.; Skrypnik, D. The influence of western-style diet on the permeability of the intestinal barrier. Metab. Disord. Forum 2019, 10, 88–97.
- Ding, N.; Zhang, X.; Zhang, X.D.; Jing, J.; Liu, S.S.; Mu, Y.P.; Peng, L.L.; Yan, Y.J.; Xiao, G.M.; Bi, X.Y.; et al. Impairment of spermatogenesis and sperm motility by the high-fat diet-induced dysbiosis of gut microbes. Gut 2020, 69, 1608–1619.
- Zhang, P.; Feng, Y.; Li, L.; Ge, W.; Yu, S.; Hao, Y.; Shen, W.; Han, X.; Ma, D.; Yin, S.; et al. Improvement in sperm quality and spermatogenesis following faecal microbiota transplantation from alginate oligosaccharide dosed mice. Gut 2021, 70, 222–225.
- Yang, H.; Zhang, J.; Xue, Z.; Zhao, C.; Lei, L.; Wen, Y.; Dong, Y.; Yang, J.; Zhang, L. Potential pathogenic bacteria in seminal microbiota of patients with different types of dysspermatism. Sci. Rep. 2020, 10, 6876.
More
Information
Subjects:
Endocrinology & Metabolism; Nutrition & Dietetics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
28 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




