Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Gisela Sjøgaard | -- | 2596 | 2023-06-07 12:16:58 | | | |
| 2 | Rita Xu | Meta information modification | 2596 | 2023-06-08 03:19:38 | | | | |
| 3 | Rita Xu | Meta information modification | 2596 | 2023-06-08 03:19:55 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Sjøgaard, G.; Søgaard, K.; Hansen, A.F.; Oestergaard, A.S.; Teljigovic, S.; Dalager, T. Intelligent Physical Exercise Training. Encyclopedia. Available online: https://encyclopedia.pub/entry/45286 (accessed on 07 February 2026).
Sjøgaard G, Søgaard K, Hansen AF, Oestergaard AS, Teljigovic S, Dalager T. Intelligent Physical Exercise Training. Encyclopedia. Available at: https://encyclopedia.pub/entry/45286. Accessed February 07, 2026.
Sjøgaard, Gisela, Karen Søgaard, Anne Faber Hansen, Anne Skov Oestergaard, Sanel Teljigovic, Tina Dalager. "Intelligent Physical Exercise Training" Encyclopedia, https://encyclopedia.pub/entry/45286 (accessed February 07, 2026).
Sjøgaard, G., Søgaard, K., Hansen, A.F., Oestergaard, A.S., Teljigovic, S., & Dalager, T. (2023, June 07). Intelligent Physical Exercise Training. In Encyclopedia. https://encyclopedia.pub/entry/45286
Sjøgaard, Gisela, et al. "Intelligent Physical Exercise Training." Encyclopedia. Web. 07 June, 2023.
Copy Citation
The background for this research concerns a high frequency of work-related disorders that may result from physical exposure at work being highly sedentary, repetitive–monotonous, or physically demanding. This may result in levels of physical inactivity or strenuous activity impairing health.
exercise interventions
workplace health promotion
musculoskeletal disorders
musculoskeletal pain
physical capacity
1. Introduction
Physical activity, PA, has convincingly been demonstrated to maintain health and prevent lifestyle diseases, such as cardiovascular and metabolic diseases. Leisure time PA, LTPA, has been studied extensively and proven beneficial for the prevention and treatment of musculoskeletal disorders that often may be work-related due to strenuous PA or prolonged inactivity during occupational tasks [1][2]. Large epidemiological studies show that LTPA is beneficial among workers with sedentary as well as strenuous jobs [3][4].
LTPA usually includes various sports, jogging, walking, fitness training, etc. Physical exercise training, a subset of LTPA that is planned, structured, repetitive, and performed with the intent to improve health or fitness, demonstrates the greatest benefits [5]. In sports exercise training, the programs are developed to increase capacity and function in order to optimize performance for a specific discipline, while in contrast, the physical activity at the work focuses on optimal job or task performance that may imply an adverse loading of the body [6][7]. In a health perspective it is important to perform exercises that are matched to the individual regarding daily life activity, e.g., occupational exposure–physical capacities, and health status, such as musculoskeletal disorders or other diseases. Researchers have termed this subset of LTPA for Intelligent Physical Exercise Training, IPET [8].
The aim of IPET is to implement the knowledge from health-enhancing exercise training into work–life. IPET is novel, as such, it is optimal and composed of a 1 h exercise training program per week that is customized individually, rather than identical for all participants, as specified below. Another unique feature of IPET is that it is designed to be effective for populations in different kinds of occupations, and is currently under evaluation for populations beyond work–life due to age or health status.
Extensive literature is available for optimizing exercise training programs to increase physical capacities, such as cardiovascular fitness (CVF), muscle strength, muscle endurance, dynamic power, etc. [9]. This evidence—available from exercise physiology and sports science—is a perfect basis for planning IPET in relation to specific job demands or other daily life activities, and for designing individual training programs to attain specific outcomes by targeting, e.g., aerobic training for CVF, strength training for musculoskeletal health, and/or functional training for coordination and balance. In general, to attain such positive effects, the training intensity must be highly relative to the individual’s capacity. Implementing IPET at worksites allows sustained workability and good health, as well as prevention of sickness absence and wear and tear by increasing workers’ capacity and resilience to lifelong work exposure and beyond.
Physical exercise training increases physical capacities such as CVF, and studies since the 1980s have shown an exponential increase in the risk of mortality and death from cardiovascular diseases with decreasing CVF [10][11]. Fitness training, also termed aerobic training, positively impacts on CVF and specific health risk factors, such as BMI, body fat, waist/hip-ratio, blood pressure, blood sugar and -fat, as well as inflammatory markers (e.g., micro-CRP or CRP in blood), while strength training, also termed resistance training, additionally impacts on musculoskeletal health and balance (the latter decreasing the risk of falling). The health effects, thus, can be targeted by adjusting the combination of various training components at a sufficiently high intensity. Of note, the most recent recommendations by the World Health Organization, WHO, include moderate to high intensity aerobic and strength training [12].
Despite the well-known positive health effects of PA, a major part of the population does not meet the guidelines on moderate to high PA. According to statistics from Nordic Council of Ministers, NMR, around 60–70% of the population in the Nordic countries do not meet the recommendations [13], and similar data are available for the US and other developed countries worldwide [14][15]. A major part of the adult population spends around half of their time awake at work or commuting to work. Thus, work–life accounts for a large time fraction of that populations’ PA profile. Importantly, the PA profile must be evaluated as a collective profile across work, leisure, and sleep (Figure 1). Therefore, in general, a balance between activity and recovery is vital [6]. A major body of evidence regarding the health enhancing effects of PA has focused on LTPA and less so on occupational PA, OPA. In contrast, sedentarism at work has drawn special attention to its negative health effects, and accordingly, the focus has mainly been on physical exercise training among workers with sedentary jobs [16][17]. However, a balance between activity and recovery is likewise important among workers with heavy OPA, who may even benefit from some sedentary work tasks in combination with exercise training to strengthen their bodies to cope with the occupational exposures [18].
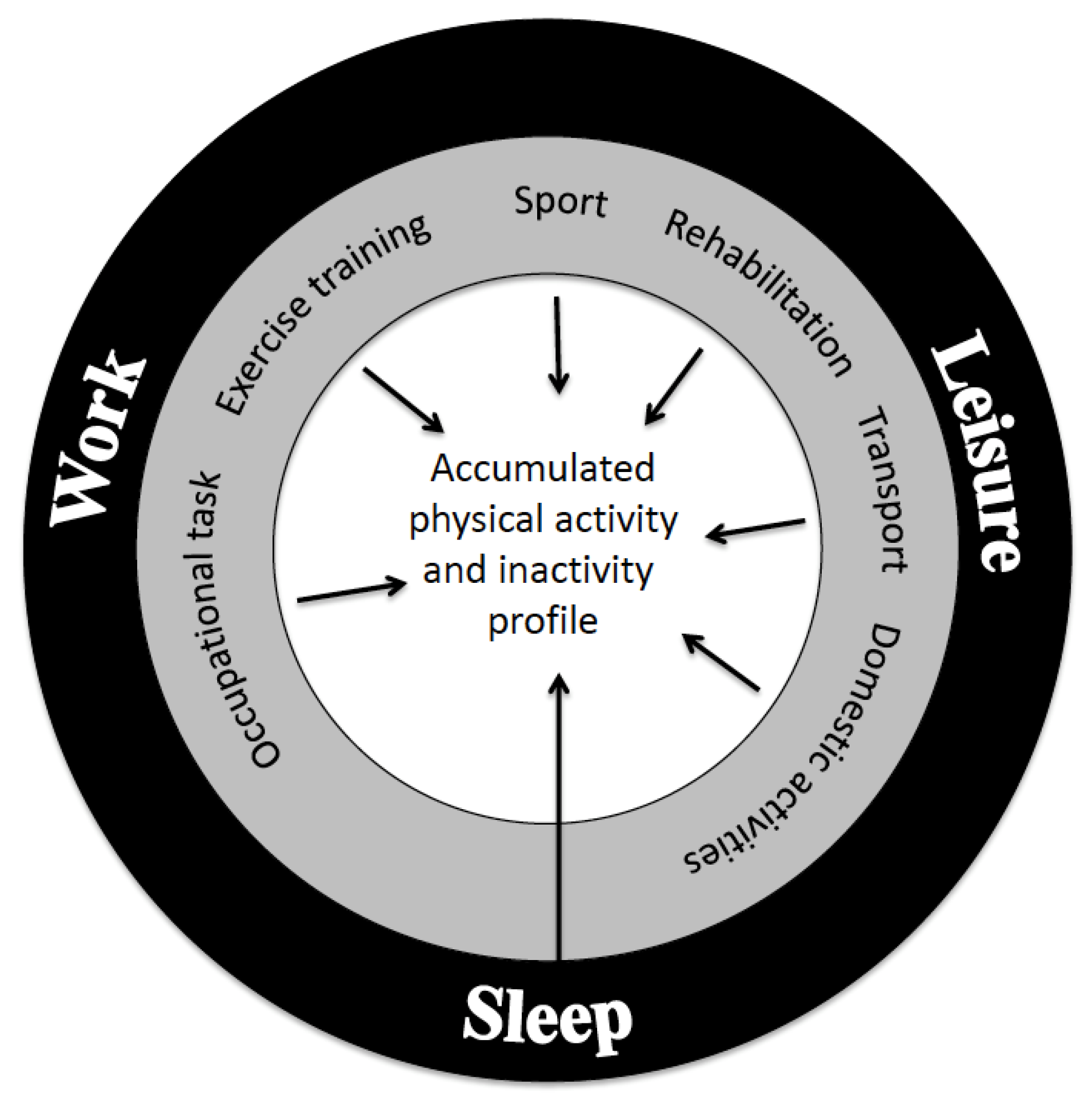
Figure 1. The daily profile of physical activity (PA) consists of three domains of work, leisure time, and sleep alongside with their subdivisions, each with its positive or negative contributions to health and physical capacity.
Musculoskeletal disorders are the most frequent cause of absenteeism in work life, early exit from the labor market, and years lived with disability [19]. Studies from the latest decades indicate that intensive strength training focused on the relevant body parts has a large potential to prevent and rehabilitate unspecific muscle and joint pain in work life [20][21].
Cascading evidence during the latest decades has resulted in the development of an algorithm for recommendation of individually tailored IPET [22][23]. The exercise training can be conducted in many different ways and, importantly, the employees must find the intervention to be “just right”, i.e., satisfy their needs and motivation for training independently, whether it is part of their work time or planned in association with their work. The allocation of a trainer or instructor to guide in planning, performing, and progressing exercises will highly facilitate the effectiveness. Additionally, instructors can give information about, e.g., exercise soreness, that is common particularly in the beginning of training, and thereby may minimize dropouts. Later, it is recommended to educate some workers to become health ambassadors to maintain motivation and ensure IPET stays an integral part of company culture.
In addition to these practical tools, it is important to be aware that the implementation of IPET in workplaces requests cultural changes, where time, space, and other resources are allocated for training activities for each worker to attain a lasting effect. This is independent of whether training is considered part of working hours paid by the employer or if it is provided as recommendations in relation to working time with or without payment. An important issue is that all organizational layers are involved from top management to middle managers and the workers. Attention must be paid to practical planning relative to the work tasks. Dedication from the leadership in a company to make their workers participate in IPET is decisive for the workers involvement. Middle managers have the practical role of planning training with minimal impact on time for production, including, e.g., time for a health care personal to care for patients or elderly, and still make it possible for all workers to participate in IPET for a sufficient duration. In a review paper, including Danish intervention studies on 1-h exercise training per week, productivity at baseline was found to be high and a further increase was difficult to attain [22]. Importantly, however, none of the studies identified a decrease in productivity despite the training being performed during paid working hours [22]. Notably, one of the studies detected an increase in productivity, which was reported among workers participating in more than 70% of the IPET planned [24]. In an Australian study—following the principles of IPET among computer users—similar positive effects were reported regarding productivity in terms of monetary value, as well as sickness absenteeism and presenteeism [25].
2. The Concept of Intelligent Physical Exercise Training, IPET
IPET is an evidence-based conceptual model for planning individually tailored physical exercise training for people during work–life and beyond. More than 20 RCT studies published, including >4000 workers, have been conducted during the last two decades, for references see [23]. The main number of studies were performed in Denmark and listed in [6], while others are from Switzerland [26] and Australia [25][27]. Most recently, a modification of IPET for rehabilitation beyond the work–life population was developed using the same principles [28]. The IPET concept has been developed over the last two decades and a number of positive findings were evidenced, the main findings being: (1) reductions in musculoskeletal disorders; (2) reduced health risk indicators and improved physical capacities; and (3) increased productivity and monetary outcome at the company level.
IPET is based on state-of-the-art, sports science principles, and existing guidelines. The exercises are allocated to each individual based on: (1) job profile defined by work exposure in terms of OPA; (2) physical capacities in terms of CVF and muscle function; and (3) health profile assessed in terms of health risk indicators including musculoskeletal pain and discomfort. The theoretical background for IPET is illustrated in Figure 2, which demonstrates the interplay between job demands and the capacity of the human body. If the individual’s capacity is low, the relative workload of a specified absolute load will be high, and the internal adaptation will, in a long-term perspective, possibly result in muscular fatigue, pain, and degeneration. This will initiate the vicious circle, where the individual’s capacity is further reduced and the relative external loading for a designated work task is further increased, and vice versa; if there is a balance between work demands and the individual’s capacity, the virtuous circle starts with maintained or increased physical capacity and health. An individual’s capacity is determined and influenced by factors other than work demands, such as sex, age, anthropometry, and training status. In addition, sleep and the possibility for recovery after a workday will influence the level of capacity for the next workday.
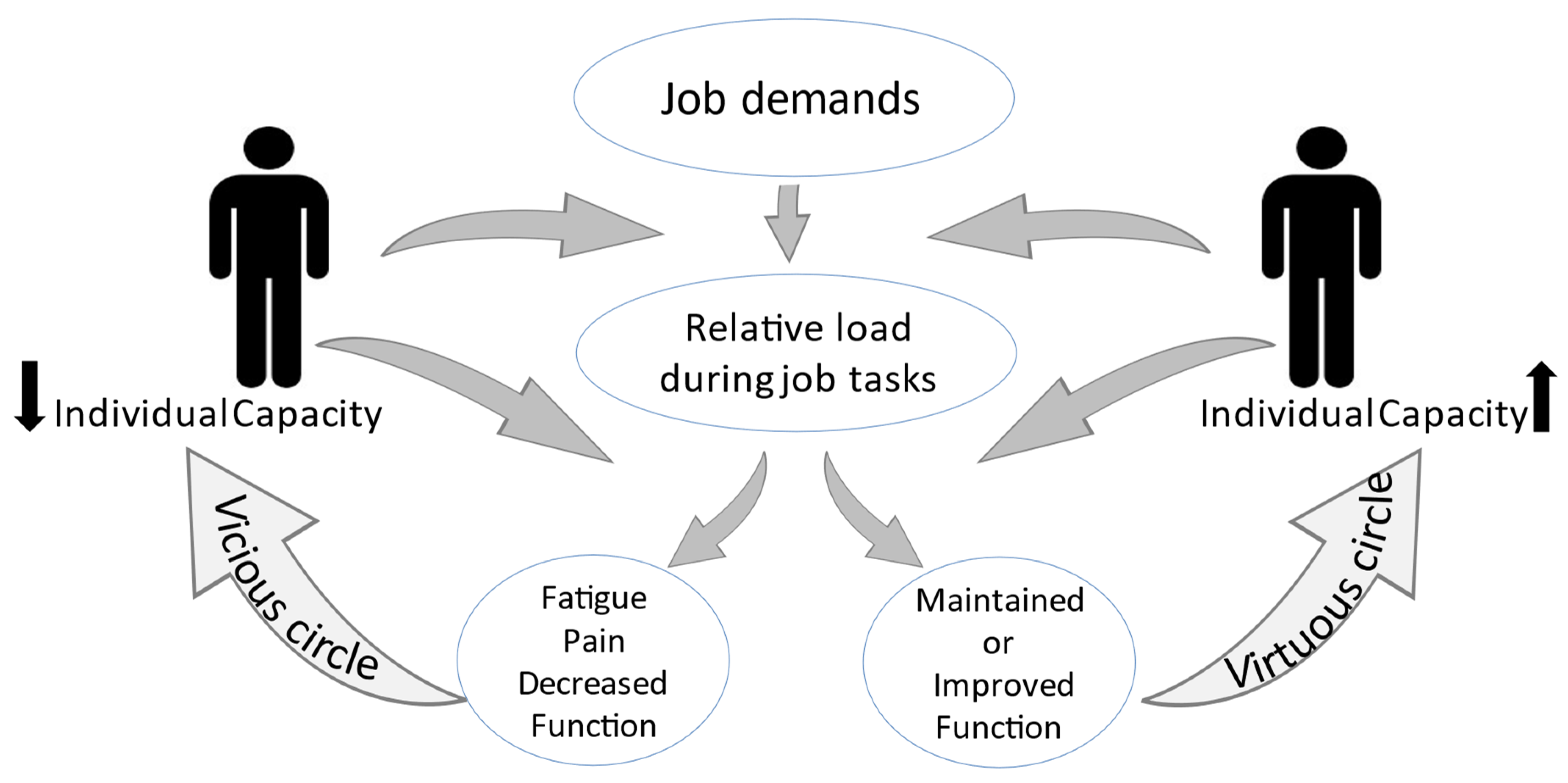
Figure 2. Vicious and virtuous circle model presents the importance of the individual’s capacity for the relation between a designated work task and its load imposed on the body. The relative load of the workdays may, in a longer term, cause either an increase or decrease in individual capacity, thereby initiating a vicious or a virtuous circle.
Physical exercise training covers all types of training (aerobic training, strength training, and functional training), and from a sports science perspective, it is well documented that the different fitness areas are linked to different physiological responses (Figure 3). Thus, depending on which physical capacities or health aspects are to be improved, different types of training modes and selected exercises are to be allocated to the training program. The exercises in IPET are selected to target relevant muscles, but not to overload muscles at a risk of developing pain, e.g., due to job demands. It is known that negative effects may occur from physical exercise training in the event of an overdose; thus, dose is important both in terms of too much and too little. Therefore, it is important to highlight that IPET corresponds to not only taking the right medicine but also in the right amount for a specific disorder. No pill helps improve all disorders, but depending on the specific disorder, specified medication is prescribed. With IPET, the specified medication depends on the individual’s strengths and weaknesses (such as the cardiorespiratory system and musculoskeletal pain). Dosage of a pill is likewise important, and for IPET this corresponds to training volume in terms of intensity and duration. Additionally, recovery is important after physical exercise training. If exercising an hour per week, according to IPET, in addition to the usual activities of daily living, ADLs, there is no need for concern. However, if an individual is very active both at work and during their leisure time, it should be considered whether an additional hour of IPET is relevant, or should replace some of the high levels of LTPA.
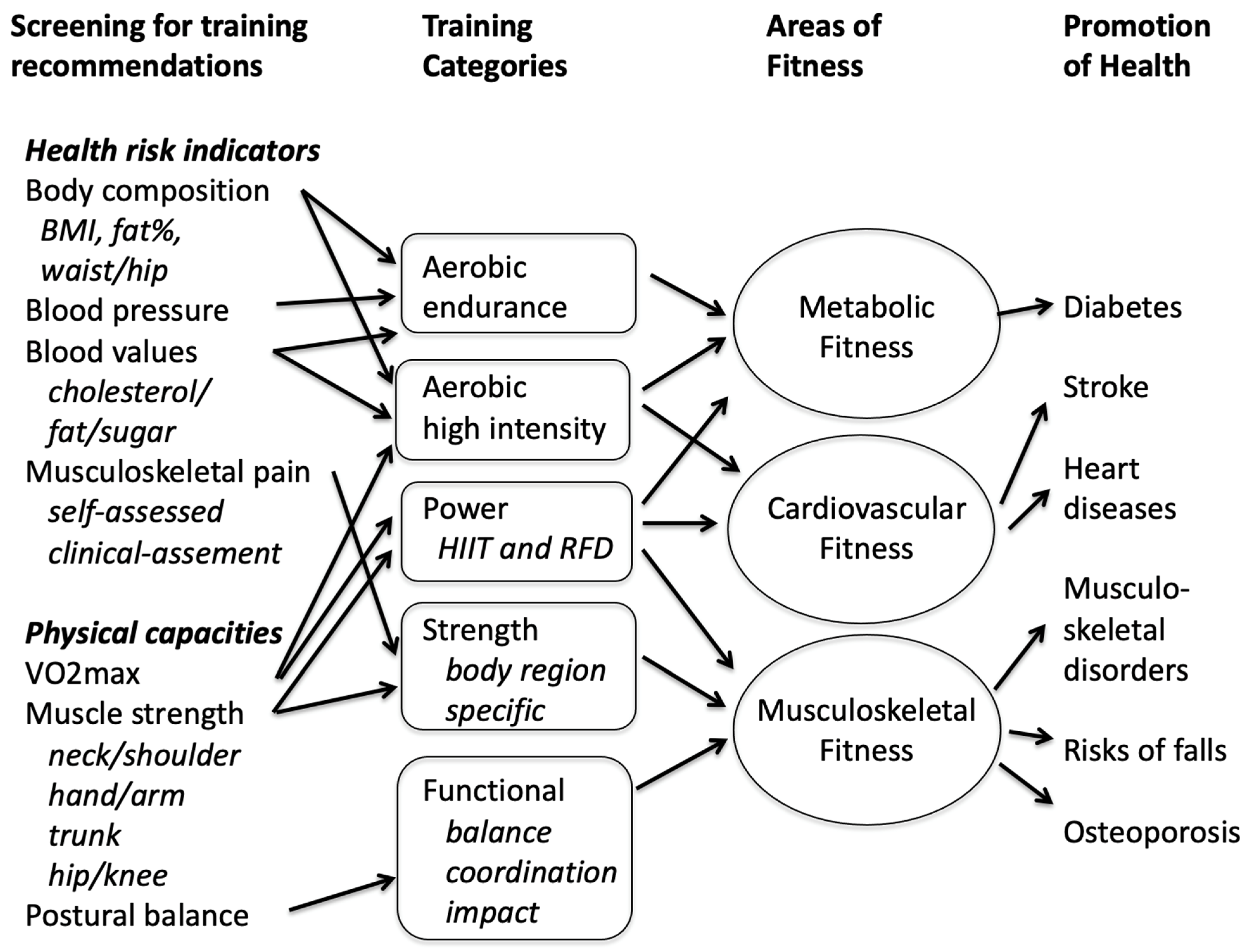
Figure 3. Overview of screening recommendations, training categories, and their effects. HIIT: High intensity interval training. RFD: Rate of Force Development.
2.1. The Structure of the IPET Program
To design exercise training in terms of an IPET program, the following variables are to be identified:
-
Individual job profile: categorized into sedentary, standing/walking, or physically heavy.
-
Physical capacity profile: aerobic capacity, muscle strength, and balance.
-
Health profile
-
Body composition: BMI, or waist/hip ratio. If more sophisticated measurements are available, body fat percentage, blood pressure and blood profile may offer additional and more precise estimates.
-
Musculoskeletal pain: localization and pain intensity in one or more of six body regions (hands/elbow, neck, shoulder/upper back, lower back, hip, knee/ankle).
-
Sedentary work, for example, includes most types of office work (with or without screen work), laboratory technicians and chauffeurs. Standing/walking work includes cleaners, health care workers without lifting/carrying tasks, nurses, gardeners, and renovation workers, as examples. Job groups within construction, manufacturing, and public safety (e.g., firefighters) typically identify their OPA as physically heavy. Based on the exposure (job profile) and individual profile (physical capacity and health assessment), the amount of aerobic training, strength training, and functional training are determined. The presence of musculoskeletal pain or low muscle strength determine which specific strength training exercises should be included in the training program depending on the body part of concern. Figure 4 shows an overview of the IPET concept. Overall, IPET is composed of 1 h training a week composed of a 10 min warm-up, 20 min specific job profile training, and 30 min specific individual profile training.
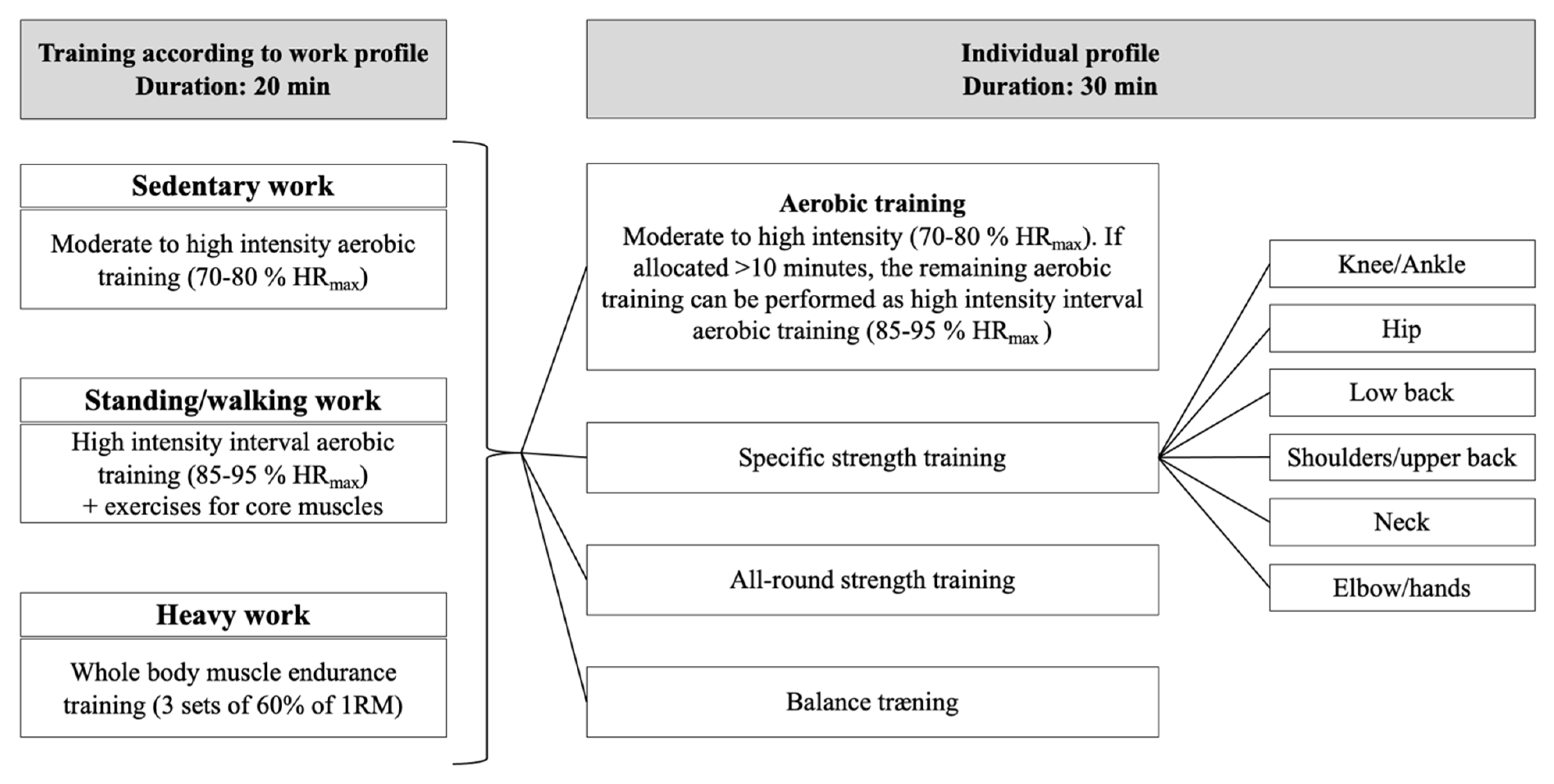
Figure 4. Cartoon of the conceptual model of IPET. The IPET concept is based on 50 min effective intelligent exercise training each week, excluding warm-up time for around 10 min. Twenty minutes is allocated to the individual’s work profile, and 30 min is allocated to target the individual’s physical capacity and health profile. In addition to the 50 min IPET, warm-up exercises are recommended to increase the body’s temperature and to start the circulation, so that the blood supply increases to the working muscles. The intensity is light, up to 60% of maximum heart rate, corresponding to 9–13 on the 6–20 Borg scale.
2.2. The IPET Algorithm
The individual exercise training program is designed based on categorization of job profile, and assessments of both physical capacity and various health parameters, including information on musculoskeletal pain. Objective assessments that are performed as an individual health check have been utilized in IPET research projects; however, simpler methods may suffice in practice.
The IPET algorithm operates in 5 min periods, allowing for up to six different aerobic, strength, or functional training exercises during the 30 min of individual profile training. However, if an exercise aggravates discomfort or some of the other suggested exercises target the experienced symptoms better, another exercise on the list may be chosen. For strength training, the algorithm maximally allows exercises prescribed for three specific body regions at the same time. Furthermore, if the individual is recommended an all-round strength training, then only two body parts are prioritized for specific body part strength training. If pain above the cut-point is reported in more than three body regions, the pain intensity defines the selection of the two most painful body regions. When the prescribed exercises have been performed for a while, they may be exchanged with other exercises for the same muscle group.
It is important to point out that suspicion of serious illness or dysfunction for which IPET will not be beneficial, will result in a consultation with a general practitioner, chiropractor, or physiotherapist, depending on the suspicion, and that reservations are possible for minor adjustments.
References
- Abdin, S.; Welch, R.K.; Byron-Daniel, J.; Meyrick, J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health 2018, 160, 70–76.
- Pedersen, B.K.; Andersen, L.B. Fysisk Aktivitet—Håndbog om Forebyggelse; Sundhedsstyrelsen: København, Denmark, 2018.
- Fimland, M.S.; Vie, G.; Holtermann, A.; Krokstad, S.; Nilsen, T.I.L. Occupational and leisure-time physical activity and risk of disability pension: Prospective data from the HUNT Study, Norway. Occup. Environ. Med. 2018, 75, 23–28.
- Holtermann, A.; Marott, J.L.; Gyntelberg, F.; Sogaard, K.; Suadicani, P.; Mortensen, O.S.; Prescott, E.; Schnohr, P. Does the benefit on survival from leisure time physical activity depend on physical activity at work? A prospective cohort study. PLoS ONE 2013, 8, e54548.
- Lavin, K.M.; Coen, P.M.; Baptista, L.C.; Bell, M.B.; Drummer, D.; Harper, S.A.; Lixandrao, M.E.; McAdam, J.S.; O’Bryan, S.M.; Ramos, S.; et al. State of Knowledge on Molecular Adaptations to Exercise in Humans: Historical Perspectives and Future Directions. Compr. Physiol. 2022, 12, 3193–3279.
- Søgaard, K.; Sjøgaard, G. Physical Activity as Cause and Cure of Muscular Pain: Evidence of Underlying Mechanisms. Exerc. Sport Sci. Rev. 2017, 45, 136–145.
- Søgaard, K.; Sjøgaard, G. Physiological Bases of Work Assessment. In Evaluation of Human Work; Sharples, J.R.W.S., Ed.; Taylor and Francis: Abingdon, UK, 2015.
- Sjøgaard, G.; Justesen, J.B.; Murray, M.; Dalager, T.; Søgaard, K. A conceptual model for worksite intelligent physical exercise training—IPET—Intervention for decreasing life style health risk indicators among employees: A randomized controlled trial. BMC Public Health 2014, 14, 652.
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sport. Exerc. 2011, 43, 1334–1359.
- Blair, S.N.; Kohl, H.W., 3rd; Paffenbarger, R.S., Jr.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 1989, 262, 2395–2401.
- Paffenbarger, R.S., Jr.; Hyde, R.T.; Wing, A.L.; Hsieh, C.C. Physical activity, all-cause mortality, and longevity of college alumni. N. Engl. J. Med. 1986, 314, 605–613.
- Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2018.
- Rasmussen, L.B.; Andersen, L.F.; Borodulin, K.; Enghardt, H.B.; Fagt, S.; Matthiessen, J.; Sveinsson, T.; Thorgeirsdottir, E.T. Nordic Monitoring of Diet, Physical Activity and Overweight: First Collection of Data in All Nordic Countries 2011; National Food Institute: Doncaster, VIC, Australia, 2011.
- Pleis, J.R.; Ward, B.W.; Lucas, J.W. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. In Vital and Health Statistics; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2010; Volume 249, pp. 1–207.
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086.
- Choi, B.; Schnall, P.L.; Yang, H.; Dobson, M.; Landsbergis, P.; Israel, L.; Karasek, R.; Baker, D. Sedentary work, low physical job demand, and obesity in US workers. Am. J. Ind. Med. 2010, 53, 1088–1101.
- Straker, L.; Mathiassen, S.E. Increased physical work loads in modern work—A necessity for better health and performance? Ergonomics 2009, 52, 1215–1225.
- Holtermann, A.; Hansen, J.V.; Burr, H.; Sogaard, K.; Sjogaard, G. The health paradox of occupational and leisure-time physical activity. Br. J. Sport. Med. 2012, 46, 291–295.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858.
- Blangsted, A.K.; Søgaard, K.; Hansen, E.A.; Hannerz, H.; Sjøgaard, G. One-year randomized controlled trial with different physical-activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scand. J. Work. Environ. Health 2008, 34, 55–65.
- Andersen, L.L.; Jorgensen, M.B.; Blangsted, A.K.; Pedersen, M.T.; Hansen, E.A.; Sjogaard, G. A randomized controlled intervention trial to relieve and prevent neck/shoulder pain. Med. Sci. Sport. Exerc. 2008, 40, 983–990.
- Sjogaard, G.; Christensen, J.R.; Justesen, J.B.; Murray, M.; Dalager, T.; Fredslund, G.H.; Sogaard, K. Exercise is more than medicine: The working age population’s well-being and productivity. J. Sport Health Sci. 2016, 5, 159–165.
- Sjogaard, G.; Mann, S.; Jensen, J.S.D.; Oestergaard, A.S.; Dalager, T. The elixir of muscle activity and kinesiology in a health perspective: Evidence of worksite tailored exercise training alleviating muscle disorders. J. Electromyogr. Kinesiol. 2021, 61, 102600.
- Justesen, J.B.; Sogaard, K.; Dalager, T.; Christensen, J.R.; Sjogaard, G. The Effect of Intelligent Physical Exercise Training on Sickness Presenteeism and Absenteeism Among Office Workers. J. Occup. Environ. Med. 2017, 59, 942–948.
- Pereira, M.; Comans, T.; Sjogaard, G.; Straker, L.; Melloh, M.; O’Leary, S.; Chen, X.; Johnston, V. The impact of workplace ergonomics and neck-specific exercise versus ergonomics and health promotion interventions on office worker productivity: A cluster-randomized trial. Scand. J. Work. Environ. Health 2019, 45, 42–52.
- Aegerter, A.M.; Deforth, M.; Volken, T.; Johnston, V.; Luomajoki, H.; Dressel, H.; Dratva, J.; Ernst, M.J.; Distler, O.; Brunner, B.; et al. A Multi-component Intervention (NEXpro) Reduces Neck Pain-Related Work Productivity Loss: A Randomized Controlled Trial Among Swiss Office Workers. J. Occup. Rehabil. 2022, 33, 288–300.
- Dalager, T.; Welch, A.; O’Leary, S.P.; Johnston, V.; Sjogaard, G. Clinically Relevant Decreases in Neck/Shoulder Pain Among Office Workers Are Associated with Strength Training Adherence and Exercise Compliance: Explorative Analyses from a Randomized Controlled Trial. Phys. Ther. 2023, 103, pzac166.
- Teljigovic, S.; Sogaard, K.; Sandal, L.F.; Dalager, T.; Nielsen, N.O.; Sjogaard, G.; Holm, L. Individualised physical exercise training and enhanced protein intake in older citizens during municipality-based rehabilitation: Protocol for a randomised controlled trial. BMJ Open 2020, 10, e041605.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
3 times
(View History)
Update Date:
08 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




