
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Subham Preetam | -- | 3005 | 2023-05-24 10:15:42 | | | |
| 2 | Lindsay Dong | Meta information modification | 3005 | 2023-05-25 02:19:59 | | |
Video Upload Options
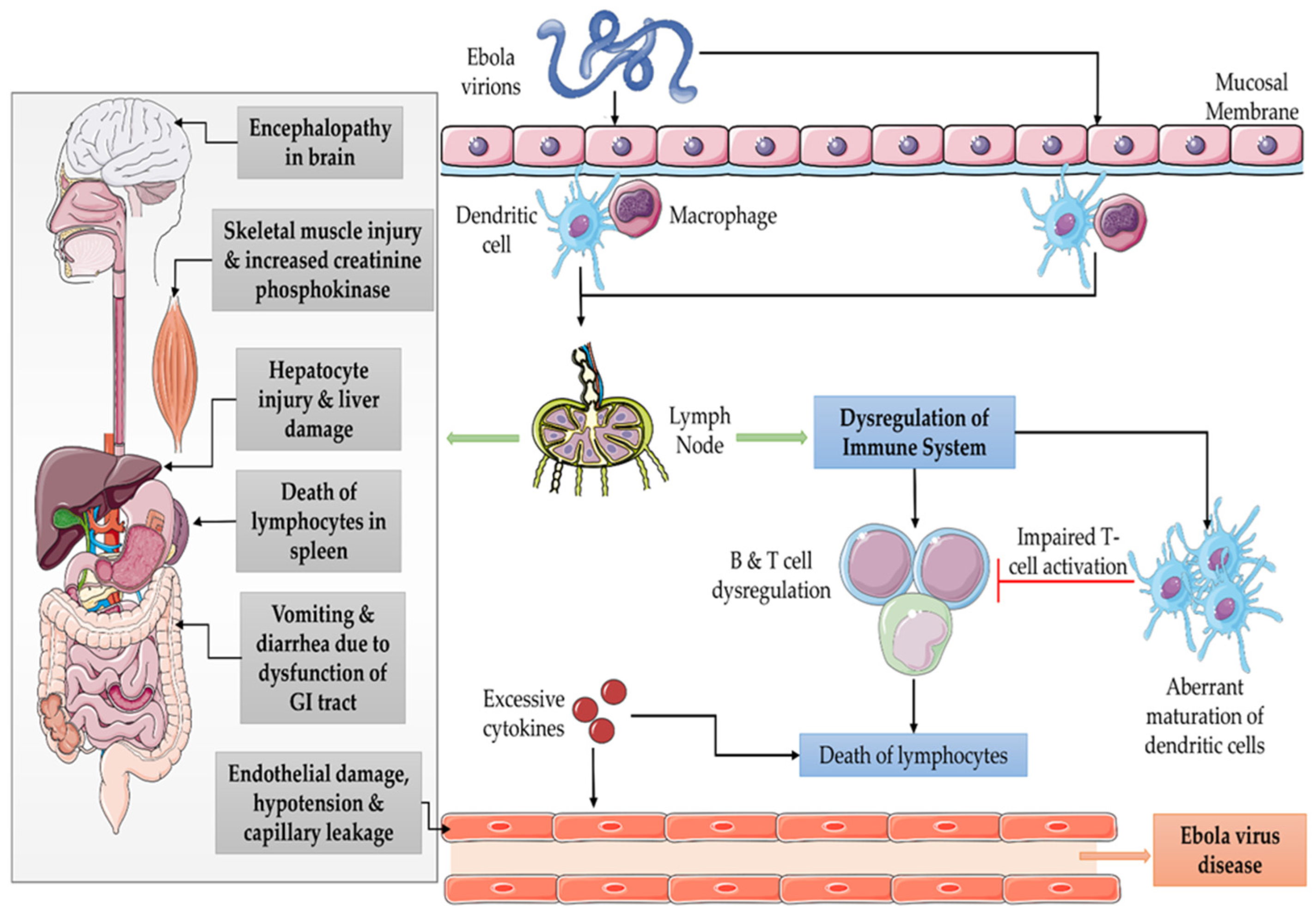
The global outgoing outbreaks of Ebola virus disease (EVD) in different regions of Sudan, Uganda, and Western Africa have brought into focus the inadequacies and restrictions of pre-designed vaccines for use in the battle against EVD, which has affirmed the urgent need for the development of a systematic protocol to produce Ebola vaccines prior to an outbreak. There are several vaccines available being developed by preclinical trials and human-based clinical trials. The group of vaccines includes virus-like particle-based vaccines, DNA-based vaccines, whole virus recombinant vaccines, incompetent replication originated vaccines, and competent replication vaccines. The limitations and challenges faced in the development of Ebola vaccines are the selection of immunogenic, rapid-responsive, cross-protective immunity-based vaccinations with assurances of prolonged protection.
1. Introduction
2. Current Vaccines
2.1. Virus-Like Particles Vaccines
2.2. DNA Vaccines
2.3. Recombinant Whole Virus Vaccine
2.4. Replication Incompetent Vaccines
2.5. Replication Competent Vaccines
3. Human Clinical Trials of Ebola Vaccines
4. Animal Models for EVD Vaccine Development
5. Challenges for Vaccine Development
5.1. Selection of Immunogen
5.2. Rapid-Responding Vaccination
5.3. Cross-Protective Immunity
5.4. Long-Term Protection
5.5. Mechanism of Protection
6. Conclusions
References
- Kelly, J.D.; Frankfurter, R.G.; Tavs, J.M.; Barrie, M.B.; McGinnis, T.; Kamara, M.; Freeman, A.; Quiwah, K.; Davidson, M.C.; Dighero-Kemp, B.; et al. Association of Lower Exposure Risk with Paucisymptomatic/Asymptomatic Infection, Less Severe Disease, and Unrecognized Ebola Virus Disease: A Seroepidemiological Study. Open Forum Infect. Dis. 2022, 9, ofac052.
- Liu, W.B.; Li, Z.X.; Du, Y.; Cao, G.W. Ebola virus disease: From epidemiology to prophylaxis. Mil. Med. Res. 2015, 2, 7.
- Weyer, J.; Grobbelaar, A.; Blumberg, L. Ebola virus disease: History, epidemiology and outbreaks. Curr. Infect. Dis. Rep. 2015, 17, 480.
- Mondiale de la Santé, O.; World Health Organization. WHO’s Health Emergencies Programme: Acute emergencies monthly summary–October and November 2022—Programme OMS de gestion des situations d’urgence sanitaire: Résumé mensuel des situations d’urgence aiguë–octobre et novembre 2022. Wkly. Epidemiol. Rec. Relev. Épidémiol. Hebd. 2022, 97, 640–644.
- Sridhar, S. Clinical development of Ebola vaccines. Ther. Adv. Vaccines 2015, 3, 125–138.
- Warfield, K.L.; Olinger, G.; Deal, E.M.; Swenson, D.L.; Bailey, M.; Negley, D.L.; Hart, M.K.; Bavari, S. Induction of humoral and CD8+ T cell responses are required for protection against lethal Ebola virus infection. J. Immunol. 2005, 175, 1184–1191.
- Warfield, K.L.; Swenson, D.L.; Olinger, G.G.; Kalina, W.V.; Aman, M.J.; Bavari, S. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J. Infect. Dis. 2007, 196, S430–S437.
- Warfield, K.L.; Aman, M.J. Advances in virus-like particle vaccines for filoviruses. J. Infect. Dis. 2011, 204, S1053–S1059.
- Lu, S.; Wang, S.; Grimes-Serrano, J.M. Current progress of DNA vaccine studies in humans. Expert Rev. Vaccines 2008, 7, 175–191.
- Martin, J.E.; Sullivan, N.J.; Enama, M.E.; Gordon, I.J.; Roederer, M.; Koup, R.A.; Bailer, R.T.; Chakrabarti, B.K.; Bailey, M.A.; Gomez, P.L. A DNA vaccine for Ebola virus is safe and immunogenic in a phase I clinical trial. Clin. Vaccine Immunol. 2006, 13, 1267–1277.
- Halfmann, P.; Kim, J.H.; Ebihara, H.; Noda, T.; Neumann, G.; Feldmann, H.; Kawaoka, Y. Generation of biologically contained Ebola viruses. Proc. Natl. Acad. Sci. USA 2008, 105, 1129–1133.
- Marzi, A.; Feldmann, H. Ebola virus vaccines: An overview of current approaches. Expert Rev. Vaccines 2014, 13, 521–531.
- Hensley, L.E.; Mulangu, S.; Asiedu, C.; Johnson, J.; Honko, A.N.; Stanley, D.; Fabozzi, G.; Nichol, S.T.; Ksiazek, T.G.; Rollin, P.E.; et al. Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebolavirus Species. PLoS Pathog. 2010, 6, e1000904.
- Geisbert, T.W.; Pushko, P.; Anderson, K.; Smith, J.; Davis, K.J.; Jahrling, P.B. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 2002, 8, 503–507.
- Tsuda, Y.; Caposio, P.; Parkins, C.J.; Botto, S.; Messaoudi, I.; Cicin-Sain, L.; Feldmann, H.; Jarvis, M.A. A replicating cytomegalovirus-based vaccine encoding a single Ebola virus nucleoprotein CTL epitope confers protection against Ebola virus. PLoS Negl. Trop. Dis. 2011, 5, e1275.
- Woolsey, C.; Geisbert, T.W. Current state of Ebola virus vaccines: A snapshot. PLoS Pathog. 2021, 17, e1010078.
- Matz, K.M.; Marzi, A.; Feldmann, H. Ebola vaccine trials: Progress in vaccine safety and immunogenicity. Expert Rev. Vaccines 2019, 18, 1229–1242.
- Sharma, A.R.; Lee, Y.H.; Nath, S.; Lee, S.S. Recent developments and strategies of Ebola virus vaccines. Curr. Opin. Pharmacol. 2021, 60, 46–53.
- Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatulin, A.I.; Dzharullaeva, A.S.; Tukhvatulina, N.M.; Shcheblyakov, D.V.; Shmarov, M.M.; Tokarskaya, E.A.; Simakova, Y.V.; Egorova, D.A.; et al. Safety and immunogenicity of GamEvac-Combi, a heterologous VSV- and Ad5-vectored Ebola vaccine: An open phase I/II trial in healthy adults in Russia. Hum. Vaccines Immunother. 2017, 13, 613–620.
- Yamaoka, S.; Banadyga, L.; Bray, M.; Ebihara, H. Small Animal Models for Studying Filovirus Pathogenesis. In Marburg- and Ebolaviruses: From Ecosystems to Molecules; Mühlberger, E., Hensley, L.L., Towner, J.S., Eds.; Springer International: Cham, Switzerland, 2017; pp. 195–227.
- Reynolds, P.; Marzi, A. Ebola and Marburg virus vaccines. Virus Genes 2017, 53, 501–515.
- Geisbert, T.W.; Strong, J.E.; Feldmann, H. Considerations in the Use of Nonhuman Primate Models of Ebola Virus and Marburg Virus Infection. J. Infect. Dis. 2015, 212, S91–S97.
- Feldmann, H.; Feldmann, F.; Marzi, A. Ebola: Lessons on Vaccine Development. Annu. Rev. Microbiol. 2018, 72, 423–446.
- Pavot, V. Ebola virus vaccines: Where do we stand? Clin. Immunol. 2016, 173, 44–49.
- Dowall, S.D.; Callan, J.; Zeltina, A.; Al-Abdulla, I.; Strecker, T.; Fehling, S.K.; Krähling, V.; Bosworth, A.; Rayner, E.; Taylor, I.; et al. Development of a Cost-effective Ovine Polyclonal Antibody-Based Product, EBOTAb, to Treat Ebola Virus Infection. J. Infect. Dis. 2016, 213, 1124–1133.
- Fausther-Bovendo, H.; Kobinger, G. The road to effective and accessible antibody therapies against Ebola virus. Curr. Opin. Virol. 2022, 54, 101210.
- Geisbert, T.W.; Daddario-DiCaprio, K.M.; Williams, K.J.; Geisbert, J.B.; Leung, A.; Feldmann, F.; Hensley, L.E.; Feldmann, H.; Jones, S.M. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J. Virol. 2008, 82, 5664–5668.
- Marzi, A.; Ebihara, H.; Callison, J.; Groseth, A.; Williams, K.J.; Geisbert, T.W.; Feldmann, H. Vesicular stomatitis virus-based Ebola vaccines with improved cross-protective efficacy. J. Infect. Dis. 2011, 204 (Suppl. 3), S1066–S1074.
- Groseth, A.; Feldmann, H.; Strong, J.E. The ecology of Ebola virus. Trends Microbiol. 2007, 15, 408–416.




