Airway management is a common and critical procedure in acute settings, such as the Emergency Department (ED) or Intensive Care Unit (ICU) of hospitals. Many of the traditional physical examination methods have limitations in airway assessment. Point-of-care ultrasound (POCUS) has emerged as a promising tool for airway management due to its familiarity, accessibility, safety, and non-invasive nature. It can assist physicians in identifying relevant anatomy of the upper airway with objective measurements of airway parameters, and it can guide airway interventions with dynamic real-time images. To date, ultrasound has been considered highly accurate for assessment of the difficult airway, confirmation of proper endotracheal intubation, prediction of post-extubation laryngeal edema, and preparation for cricothyrotomy by identifying the cricothyroid membrane. The researchers aim to provide a comprehensive overview of the use of POCUS on upper airway sono-anatomy. In conclusion, POCUS is a valuable tool with multiple applications ranging from pre- and post-intubation management. Clinicians should consider using POCUS in conjunction with traditional exam techniques to manage the airway more efficiently in the acute setting.
1. Introduction
Upper airway ultrasound allows for the identification of important upper airway structures such as the trachea, esophagus, tracheal rings, cricoid cartilage, CTM, thyroid cartilage, vocal cords, hyoid bone, epiglottis, and tongue
[1]. In addition, ultrasound measurements of the upper airway have been shown to have both high inter- and intra-operator reliability as well as accuracy when compared to cadaver models
[2].
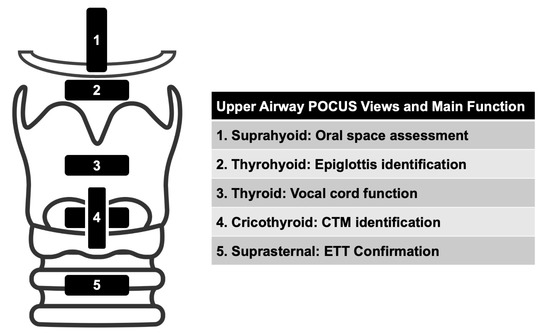
The following five views can be used to assess the upper airway: suprahyoid, thyrohyoid, thyroid, cricothyroid, and suprasternal (Figure 1). Depending on the specific reason for upper airway evaluation, fewer views can be selected to answer a focused question.
Figure 1. Views to Assess the Upper Airway.
2. Suprahyoid View
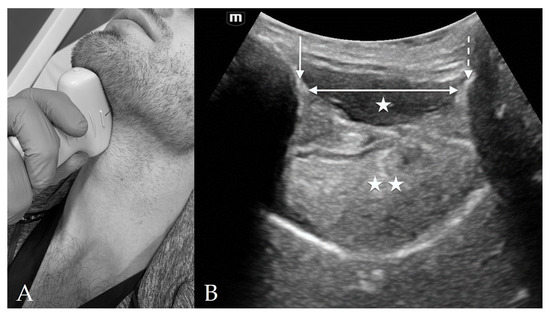
The suprahyoid view is located above the hyoid, from the hyoid to the mentum, and is used to measure hyomental distance (HMD), distance to tongue, and tongue thickness (
Figure 2). The measurements on this view may vary with changes in patient positioning
[3]. The main structures seen on this view include the hyoid, mentum, tongue, mylohyoid muscle, and geniohyoid muscle.
Figure 2. Suprahyoid View. (A) Suprahyoid probe placement on the subject’s neck in sagittal orientation. (B) Suprahyoid view of anterior neck with curvilinear probe in sagittal orientation and probe indicator directed cranially. The mentum of the mandible is indicated by the solid arrow and the hyoid bone is indicated by the dashed arrow. Deep to the hypoechoic mylohyoid and geniohyoid muscles (single star) lies the tongue (double star). The hyomental distance (HMD) is spanned by the double-headed arrow.
On sagittal view, with the indicator towards the mentum, the hyoid is seen on the right of the image as a hyperechoic protuberance with posterior shadowing. To the left of the image is the symphysis menti, which also appears as hyperechoic with posterior shadowing. The hypoechoic tongue lies in between, just above the palate. Superficial to the tongue are the hypoechoic mylohyoid and geniohyoid muscles
[4].
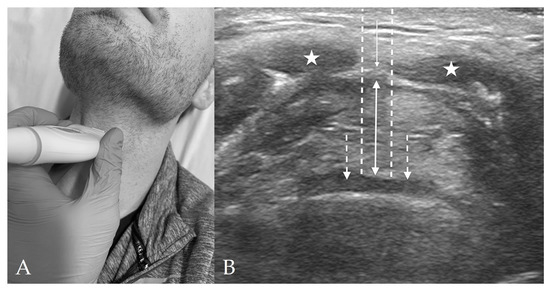
3. Thyrohyoid View
The thyrohyoid view is located through the thyrohyoid membrane and is used to visualize the epiglottis (Figure 3). The main structures seen on this view include the strap muscles, thyrohyoid membrane, pre-epiglottic space (PES), and the epiglottis.
Figure 3. Thyrohyoid View. (A) Thyrohyoid probe placement on subject’s neck. (B) Thyrohyoid view of anterior neck with linear probe in transverse orientation. The pre-epiglottic space (solid, double-headed arrow) appears between the thyrohyoid membrane (solid, single-headed arrow) and the epiglottis (dashed arrows). The strap muscles (stars) are again visible superficially to the thyrohyoid membrane. The distance from skin to epiglottis (DSE) is spanned by the two dashed lines.
At this level, the hypoechoic strap muscles converge medially and bridge over the thyrohyoid membrane, which lies in between the strap muscles and the PES. The PES is a hyperechoic collection of adipose tissue immediately deep to the strap muscles and superficial to the epiglottis. The epiglottis appears as a thin hypoechoic stripe lying just anterior to a hyperechoic air-mucosa (A-M) interface. The entire image appears as a “small face sign” where the strap muscles appear as eyes and the epiglottis appears as the mouth
[5].
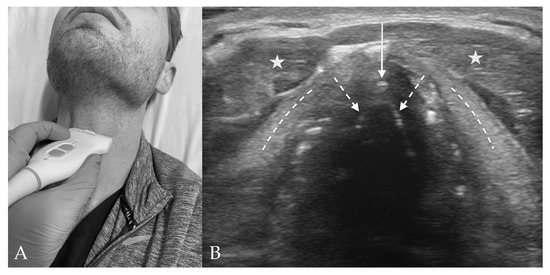
4. Thyroid View
The thyroid view is located over the thyroid cartilage and is used to visualize the vocal cords (
Figure 4). The main structures seen on this view include the vocal cords, arytenoid cartilage, and strap muscles. As the thyroid cartilage becomes more calcified with age and shadowing from calcifications may obstruct this view, visualization of the vocal cords can also be performed through the cricothyroid membrane and angling the probe skilfully
[4].
Figure 4. Thyroid View. (A) Thyroid probe placement on subject’s neck. (B) Thyroid view of anterior neck with linear probe in transverse orientation. The vocal cords (dashed arrows) join together at the anterior commissure (solid arrow). The thyroid cartilage (dashed lines) appears lateral to the vocal cords, and the strap muscles (stars) just superficial to the thyroid cartilage. Although not well visualized in this image, the arytenoids will usually appear at the posterior aspect of the bilateral vocal cords.
The strap muscles are seen superficially to the vocal cords and have a hypoechoic striated appearance. In addition, the vocal cords and arytenoid cartilage are both identifiable at the level of the thyroid cartilage. The thyroid cartilage appears just below the strap muscles and forms a triangular shape. Deep to the thyroid cartilage are the vocal cords, which form an isosceles triangle with central shadowing. The arytenoid cartilages are deep to the vocal cords and appear hyperechoic with shadowing
[4].
5. Cricothyroid View
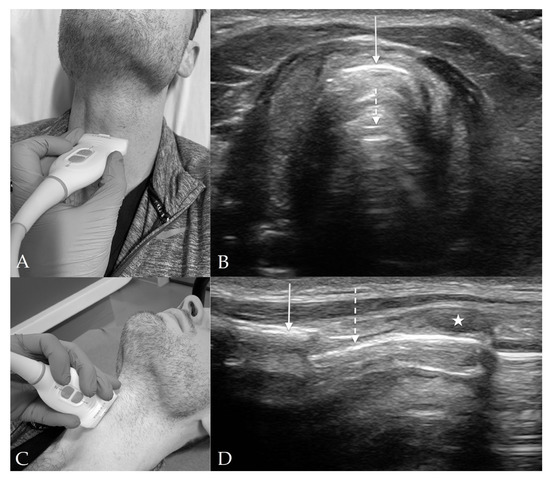
The cricothyroid view is located between the cricoid cartilage and the thyroid cartilage (Figure 5). The main clinical utility of this view is to locate the CTM and any structures overlying the CTM for cricothyrotomy. The main structures seen from this view include the cricoid cartilage, CTM, and the thyroid cartilage.
Figure 5. Cricothyroid View: Transverse and Sagittal Orientations. (A) Cricothyroid probe placement on subject’s neck in transverse orientation. (B) Cricothyroid view of anterior neck with linear probe in transverse orientation. The cricothyroid membrane (solid arrow) overlies the trachea with prominent reverberation artifact (dashed arrow) in the tracheal lumen. (C) Cricothyroid probe placement on subject’s neck in sagittal orientation. (D) Cricothyroid view of anterior neck with linear probe in sagittal orientation. The thyroid cartilage (solid arrow) appears superior to the hypoechoic cricoid cartilage (star). The cricothyroid membrane (dashed arrow) spans between the two cartilages.
In the transverse plane, the “thyroid-airline-cricoid-airline” (TACA) protocol can be used to identify the CTM. First, the prominent, triangular thyroid cartilage is visualized. It may be partially or fully calcified depending on age and therefore has posterior shadowing. Moving caudally, the hyperechoic linear CTM can be found. More caudally, the hypoechoic lateral edges of the cricoid cartilage will appear to converge anterior to the CTM. Scanning cranially, the CTM can then be identified again
[6]. In the sagittal plane, the thyroid cartilage will plunge from superficial to deep as it moves inferiorly until its border with the CTM. The cricoid cartilage will appear inferior to the CTM as a hypoechoic ovoid structure, and the tracheal rings will appear as smaller evenly spaced intermittent hypodensities inferior to the cricoid cartilage. This appearance in sagittal view has been repeatedly described as “beads on a string”
[6].
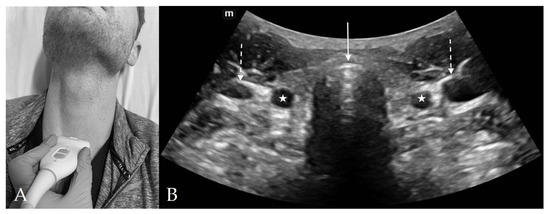
6. Suprasternal View
The suprasternal view is located just above the suprasternal notch and is the best location to visualize ETT location and placement, and to measure the tracheal diameter (Figure 6). The main structures seen on this view include the trachea, esophagus, thyroid, carotid artery and internal jugular veins, vertebra, and sternocleidomastoid muscles.
Figure 6. Suprasternal View. (A) Suprasternal probe placement on subject’s neck. (B) Suprasternal view of anterior neck with curvilinear probe. The tracheal cartilage (solid arrow) appears hyperechoic with reverberation artifact noted in the air-filled tracheal lumen posteriorly. The common carotid arteries (stars) and internal jugular veins (dashed arrow) appear laterally on each side of the trachea.
On the transverse view, the trachea appears as a curvilinear convexity with a hyperechoic air–mucosa (A–M) interface and posterior reverberation artifact. The lobes of the thyroid can be seen immediately lateral to the trachea with the thyroid isthmus bridging over the trachea anteriorly. Posterior to the lateral thyroid lobes are the common carotid arteries and internal jugular veins, with the sternocleidomastoid muscle lying superficial to the vessels. Color Doppler can be used to confirm flow within the vascular structures. The esophagus is usually located in the posterior and to the anatomical left of the trachea appearing with both hyper and hypoechoic components
[7]. Visualization of both trachea and esophagus at this level is important as the presence of a “double tract sign” with two hyperechoic (A-M) interfaces indicate the improper placement of the ETT into the esophagus during intubation
[8][9].
7. Conclusions
Airway management is a critical and high-risk procedure that may lead to severe morbidity and mortality. POCUS has been considered as an accurate and reliable tool for ETT confirmation, anatomic airway measurements, prediction of the difficult airway, post-extubation laryngeal edema, and cricothyrotomy guidance. The better understanding of upper airway sono-anatomy can facilitate the assessment and management of difficult airway in acute settings.