
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | daniela d'agnano | -- | 1748 | 2023-04-27 17:35:54 | | | |
| 2 | Beatrix Zheng | + 3 word(s) | 1751 | 2023-05-04 03:43:07 | | |
Video Upload Options
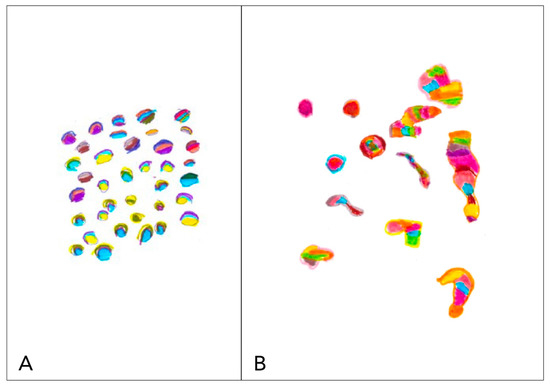
Since the earliest descriptions of the simple visual hallucinations in migraine patients and in subjects suffering from occipital lobe epilepsy, several important issues have arisen in recognizing epileptic seizures of the occipital lobe, which often present with symptoms mimicking migraine. A detailed quantitative and qualitative clinical scrutiny of timing and characteristics of visual impairment can contribute to avoiding mistakes. Differential diagnosis, in children, might be challenging because of the partial clinical, therapeutic, and pathophysiological overlaps between the two diseases that often coexist. Ictal elementary visual hallucinations are defined by color, shape, size, location, movement, speed of appearance and duration, frequency, and associated symptoms and their progression. The evaluation of the distinctive clinical features of visual aura in migraine and visual hallucinations in occipital epilepsy could contribute to understanding the pathogenetic mechanisms of these two conditions.
1. Visual Symptoms in Migraine
2. Visual Symptoms in Epilepsy
3. Visual Symptoms in Both Conditions: Epilepsy and Migraine
3.1. Visual Loss

3.2. Palinopsia and Polioplia
3.3. Visual Snow
3.4. Other Complex Positive Symptoms
References
- Victor, T.; Hu, X.; Campbell, J.; Buse, D.; Lipton, R. Migraine Prevalence by Age and Sex in the United States: A Life-Span Study. Cephalalgia 2010, 30, 1065–1072.
- Tarasco, V.; Grasso, G.; Versace, A.; Castagno, E.; Ricceri, F.; Urbino, A.F.; Pagliero, R. Epidemiological and Clinical Features of Migraine in the Pediatric Population of Northern Italy. Cephalalgia 2016, 36, 510–517.
- Genizi, J.; Khourieh Matar, A.; Zelnik, N.; Schertz, M.; Srugo, I. Frequency of Pediatric Migraine with Aura in a Clinic-Based Sample. Headache 2016, 56, 113–117.
- Shevell, M.I. Acephalgic Migraines of Childhood. Pediatr. Neurol. 1996, 14, 211–215.
- Pacheva, I.H.; Ivanov, I.S. Migraine Variants--Occurrence in Pediatric Neurology Practice. Clin. Neurol. Neurosurg. 2013, 115, 1775–1783.
- Ziegler, D.K.; Hassanein, R.S. Specific Headache Phenomena: Their Frequency and Coincidence. Headache 1990, 30, 152–156.
- Agessi, L.M.; Villa, T.R. Vestibular Migraine with Visual Aura and Olfactory Hallucination in Children: Two Case Reports. Neuropediatrics 2018, 49, 414–416.
- Raieli, V.; Capizzi, M.; Marino, A.; Di Nardo, G.; Raucci, U.; Parisi, P. Study on “Atypical” Migraine Auras in the Pediatric Age: The Role of Cortical Spreading Depression and the Physiopathogenetic Hypothesis Arising from Our Clinical Cases. Life 2022, 12, 450.
- Rastogi, R.G.; VanderPluym, J.; Lewis, K.S. Migrainous Aura, Visual Snow, and “Alice in Wonderland” Syndrome in Childhood. Semin. Pediatr. Neurol. 2016, 23, 14–17.
- Queiroz, L.P.; Friedman, D.I.; Rapoport, A.M.; Purdy, R.A. Characteristics of Migraine Visual Aura in Southern Brazil and Northern USA. Cephalalgia 2011, 31, 1652–1658.
- Russel, M.B.; Olesen, J. A Nosographic Analysis of the Migraine Aura in a General Population. Brain 1996, 119 Pt 2, 355–361.
- Schott, G.D. Exploring the Visual Hallucinations of Migraine Aura: The Tacit Contribution of Illustration. Brain 2007, 130, 1690–1703.
- Petrusic, I.; Pavlovski, V.; Vucinic, D.; Jancic, J. Features of Migraine Aura in Teenagers. J. Headache Pain 2014, 15, 87.
- Hadjikhani, N.; Vincent, M. Visual Perception in Migraine: A Narrative Review. Vision 2021, 5, 20.
- Lawden, M.C.; Cleland, P.G. Achromatopsia in the Aura of Migraine. J. Neurol. Neurosurg. Psychiatry 1993, 56, 708–709.
- Noseda, R.; Bernstein, C.A.; Nir, R.R.; Lee, A.J.; Fulton, A.B.; Bertisch, S.M.; Hovaguimian, A.; Cestari, D.M.; Saavedra-Walker, R.; Borsook, D.; et al. Migraine Photophobia Originating in Cone-Driven Retinal Pathways. Brain 2016, 139, 1971–1986.
- Olesen, J.; Bes, A.; Kunkel, R.; Lance, J.W.; Nappi, G.; Pfaffenrath, V.; Rose, F.C.; Schoenberg, B.S.; Soyka, D.; Tfelt-Hansen, P.; et al. The International Classification of Headache Disorders, 3rd Edition (Beta Version). Cephalalgia 2013, 33, 629–808.
- Caraballo, R.; Koutroumanidis, M.; Panayiotopoulos, C.P.; Fejerman, N. Idiopathic Childhood Occipital Epilepsy of Gastaut: A Review and Differentiation from Migraine and Other Epilepsies. J. Child Neurol. 2009, 24, 1536–1542.
- Gastaut, H. Benign Epilepsy of Childhood with Occipital Spike and Wave Complexes; Andermann, F., Lugaresi, E., Eds.; Butterworths: Boston, MA, USA, 1987.
- Hartl, E.; Angel, J.; Rémi, J.; Schankin, C.J.; Noachtar, S. Visual Auras in Epilepsy and Migraine–An Analysis of Clinical Characteristics. Headache 2017, 57, 908–916.
- Jobst, B.C. Focal Seizures with Auditory Hallucinations. In Atlas of Epilepsies; Springer: London, UK, 2010; pp. 447–450.
- Viana, M.; Tronvik, E.A.; Do, T.P.; Zecca, C.; Hougaard, A. Clinical Features of Visual Migraine Aura: A Systematic Review. J. Headache Pain 2019, 20, 64.
- Shapiro, H.F.J.; Lebel, A. Pediatric Episodic Migraine with Aura: A Unique Entity? Children 2021, 8, 228.
- Flanagan, D.; Ghose, K. Co-Morbidity of Migraine and Epilepsy: A Review of Clinical Features. J. Headache Pain 2000, 1, 137.
- Guerrini, R.; Genton, P. Epileptic Syndromes and Visually Induced Seizures. Epilepsia 2004, 45 (Suppl. S1), 14–18.
- Panayiotopoulos, C.P. Benign Childhood Partial Seizures and Related Epileptic Syndromes; John Libbey & Company Ltd.: London, UK, 1999.
- Panayiotopoulos, C. Benign Childhood Focal Seizures and Related Epileptic Syndromes. In The Epilepsies: Seizures, Syndromes and Management; Bladon Medical Pubblishing: Chipping Norton, UK, 2005.
- Adcock, J.E.; Panayiotopoulos, C.P. Occipital Lobe Seizures and Epilepsies. J. Clin. Neurophysiol. 2012, 29, 397–407.
- Rajapakse, T.; Buchhalter, J. The Borderland of Migraine and Epilepsy in Children. Headache 2016, 56, 1071–1080.
- Belcastro, V.; Maria Cupini, L.; Corbelli, I.; Pieroni, A.; D’Amore, C.; Caproni, S.; Gorgone, G.; Ferlazzo, E.; Di Palma, F.; Sarchielli, P.; et al. Palinopsia in Patients with Migraine: A Case-Control Study. Cephalalgia 2011, 31, 999–1004.
- Kataoka, H.; Ueno, S. Cerebral Polyopia and Palinopsia in a Patient with Occipital Lobe Epilepsy. Epilepsy Behav. 2009, 14, 684–686.
- Bender, M.B.; Rudolph, S.H.; Stacy, C. The Neurology of the Visual and Oculomotor Systems; Baker, A.B., Baker, J.R., Eds.; Harper-Row: Philadelphia, PA, USA, 1986; Volume 43.
- Raieli, V.; Eliseo, G.L.; La Franca, G.; La Vecchia, M.; Puma, D.; Eliseo, M. Cerebral Polyopia in Migraine: A Clinical Case. J. Headache Pain 2000, 1, 127–129.
- Raieli, V.; Monastero, R.; Santangelo, G.; Eliseo, G.L.; Eliseo, M.; Camarda, R. Red Ear Syndrome and Migraine: Report of Eight Cases. Headache 2002, 42, 147–151.
- Simpson, J.C.; Goadsby, P.J.; Prabhakar, P. Positive Persistent Visual Symptoms (Visual Snow) Presenting as a Migraine Variant in a 12-Year-Old Girl. Pediatr. Neurol. 2013, 49, 361–363.
- Polster, T.; Schaefer, S.; Panzer, A. Visual Snow–Two Adolescents with a New Syndrome Different from Migraine or Epilepsy. Neuropediatrics 2019, 50, GNP-FV20.
- Smith, R.A.; Wright, B.; Bennett, S. Hallucinations and Illusions in Migraine in Children and the Alice in Wonderland Syndrome. Arch. Dis. Child. 2015, 100, 296–298.
- Akiyama, O.; Kondo, A.; Akiyama, I. Paediatric Migraine with Visual Hallucination Auras Appearing in the Form of a Human Body. BMJ Case Rep. 2019, 12, e232358.
- Gloor, P.; Olivier, A.; Quesney, L.F.; Andermann, F.; Horowitz, S. The Role of the Limbic System in Experiential Phenomena of Temporal Lobe Epilepsy. Ann. Neurol. 1982, 12, 129–144.
- Sakamoto, Y.; Suzuki, R.; Ohara, T.; Miyagi, T.; Osaki, M.; Nishimura, K.; Toyoda, K. Complex Visual Hallucinations as the Sole Manifestation of Symptomatic Temporo-Occipital Lobe Epilepsy Due to Old Intracerebral Hemorrhage. Seizure 2014, 23, 244–246.
- Blom, J.D. Alice in Wonderland Syndrome: A Systematic Review. Neurol. Clin. Pract. 2016, 6, 259–270.
- Liu, A.M.; Liu, J.G.; Liu, G.W.; Liu, G.T. “Alice in Wonderland” Syndrome: Presenting and Follow-up Characteristics. Pediatr. Neurol. 2014, 51, 317–320.
- Swartwood, S.; Pham, K.; Candee, M.S. Pediatric Migraine Phenomena and Variants: Don’t Let Them Go Over Your Head. Curr. Pain. Headache Rep. 2020, 24, 47.




