
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jay Dondani | -- | 3111 | 2023-03-15 02:39:55 | | | |
| 2 | Catherine Yang | -4 word(s) | 3107 | 2023-03-15 02:43:20 | | |
Video Upload Options
Polymers, in general, and Poly (Ether-Ether-Ketone) (PEEK) have emerged as potential alternatives to conventional osseous implant biomaterials. Due to its distinct advantages over metallic implants, PEEK has been gaining increasing attention as a prime candidate for orthopaedic and dental implants. Although a myriad of permutations and combinations of different surface treatments are employed to alter the surface topography of PEEK, for the sake of simplicity, these treatments have been classified into the following categories: physical treatment, chemical treatment, surface coating, and composite preparation, with the first surface treatment in the combination determining the classification. Though these terms are arbitrary and could lead to considerable overlap, physical and chemical treatments can be grouped into a subtractive form of surface modification while surface coating can be regarded as an additive form.
1. Physical Treatment
1.1. Plasma Treatment
| Treatment | Results | Author |
|---|---|---|
| Plasma | ||
| Oxygen/Ammonia | In-vitro: Increased adhesion, proliferation, and osteogenic differentiation of cells as compared to control | Althaus et al. [1] |
| Nitrogen | In-vitro: Increase in bioactivity and antibacterial properties with reference to S. aureus. | Gan et al. [2] |
| Oxygen/Argon | In-vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of SAOS-2 osteoblasts | Han et al. [3] |
| Oxygen/Nitrogen | In-vitro: Decrease in contact angle and no disadvantageous effect on cytocompatibility; | Ha et al. [4] |
| Nitrogen/Argon/(Nitrogen + Argon) | In-vitro: Increase in osteogenic activity (Highest: Nitrogen) and antibacterial property (Highest: Nitrogen + Argon) | Liu et al. [5] |
| Oxygen | In-vitro: Decrease in contact angle | Tsougeni et al. [6] |
| Oxygen | In-vitro: Increased cell adhesion and spreading of U2-OS osteoblasts in the presence of S. epidermidis | Rochford et al. [7] |
| Water vapour/Argon | In-vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of osteoblast precursor cell line derived from Mus musculus (mouse) calvaria (MC3T3-E1). | Wang et al. [8] |
| Plasma treatment + Radiation | ||
| EUV + (low temperature Nitrogen/Oxygen) | In-vitro: Decreased contact angle and increased cell adhesion of MG63 cells, Cell adhesion higher with Nitrogen plasma | Czwartos et al. [9] |
| Oxygen/UV | In-vitro: Increase in the bond strength to TiO2 sol solution after exposure to O2 plasma/UV radiation | Kizuki et al. [10] |
| Plasma + Chemical treatment | ||
| Argon + Hydrofluoric acid | In-vitro: Decreased contact angle and increased cell proliferation and differentiation of rBMS cells (Higher with Nitrogen) In-vivo: Increased resistance to Porphyromonas gingivalis (P. gingivalis) |
Chen et al. [11] |
| Argon/(Argon + Hydrogen peroxide) | In-vitro: Increased cell adhesion, collagen secretion, and extra-cellular matrix deposition (Higher with Argon, Peroxide combination) In-vivo: Increased fibrous tissue filtration inhibition and osseointegration with Argon, Peroxide combination |
Ouyang et al. [12] |
| Plasma + Laser | ||
| Oxygen + Nd:YAG | In vitro: Decrease in contact angle | Akkan et al. [13] |
| Plasma + Biomolecules/Inorganic coating | ||
| Argon + Polydopamine (PDA) + Vancomycin gelatin nanoparticles | In vitro: No cytotoxicity and increased antibacterial resistance to Staphylococcus aureus (S. aureus) and Streptococcus mutans (S. mutans) | Chen et al. [14] |
| Nitrogen + Tropoelastin | In vitro: Increased bioactivity of osteogenic cells | Wakelin et al. [15] |
| Nitrogen + PDA + Poly (lactic-co-glycolic acid) carrying Bone Morphogenic Protein-2 (BMP-2) gene | In vitro: Increased osteogenic activity | Qin et al. [16] |
| (Argon/Oxygen) + Acrylic acid vapours + Polystyrene sulfonate (PSS) and polyallylamine hydrochloride (PAH) multilayers | In vitro: Increased adhesion and proliferation of bone marrow stromal cells In vivo: Increased osseointegration |
Liu et al. [17] |
1.2. Accelerated Neutral Atom Beam (ANAB)
| Treatment | Result | Author |
|---|---|---|
| ANAB | In vitro: Decreased contact angle and increased bioactivity of osteogenic cells | Khoury et al. [21] |
| ANAB | In vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of SAOS-2 osteoblasts In vivo: Increased bond strength to bone |
Khoury et al. [22] |
| ANAB | In vitro: Improved osteoblastic response and decrease in bacterial colonization of MRSA, S. epidermidis, and E. coli | Webster et al. [23] |
| ANAB | In vitro: Decreased contact angle and increased bioactivity of osteogenic cells | Ajami et al. [24] |
1.3. Photodynamic Treatment
1.4. Sandblasting
1.5. Laser
| Treatment | Result | Author |
|---|---|---|
| Photodynamic therapy | ||
| (Temporfin/Ampicillin) + Diode laser | In vitro: Increase in resistance to microbial load | Peng et al. [26] |
| PDT/Sulphuric acid (H2SO4)/Air abrasion (Al/Diamond) | In vitro: Lower shear bond strength and microroughness of samples treated with PDT as compared to H2SO4 and Alumina particle air abrasion (Highest: H2SO4) | Binhasan et al. [25] |
| Sandblasting | ||
| Alumina particles | In vitro: Increased proliferation and differentiation of rat MSCs and mitigation of inflammatory chemokine (C-C motif) Ligand 2 (CCL2) | Sunarso et al. [27] |
| Laser | ||
| Femtosecond laser | In vitro: Increased adhesion, proliferation and differentiation of mBMSC cells and increased expression and activity of alkaline phosphatase | Xie et al. [28] |
2. Chemical Treatment
2.1. Sulphonation
2.2. Phosphonation
2.3. Silanization
3. Surface Coatings
3.1. Hydroxyapatite Coating
| Treatment | Result | Author |
|---|---|---|
| Surface coatings—Hydroxyapatite | ||
| Hydroxyapatite | In vivo: Increased removal torque and biocompatibility | Johansson et al. [38] |
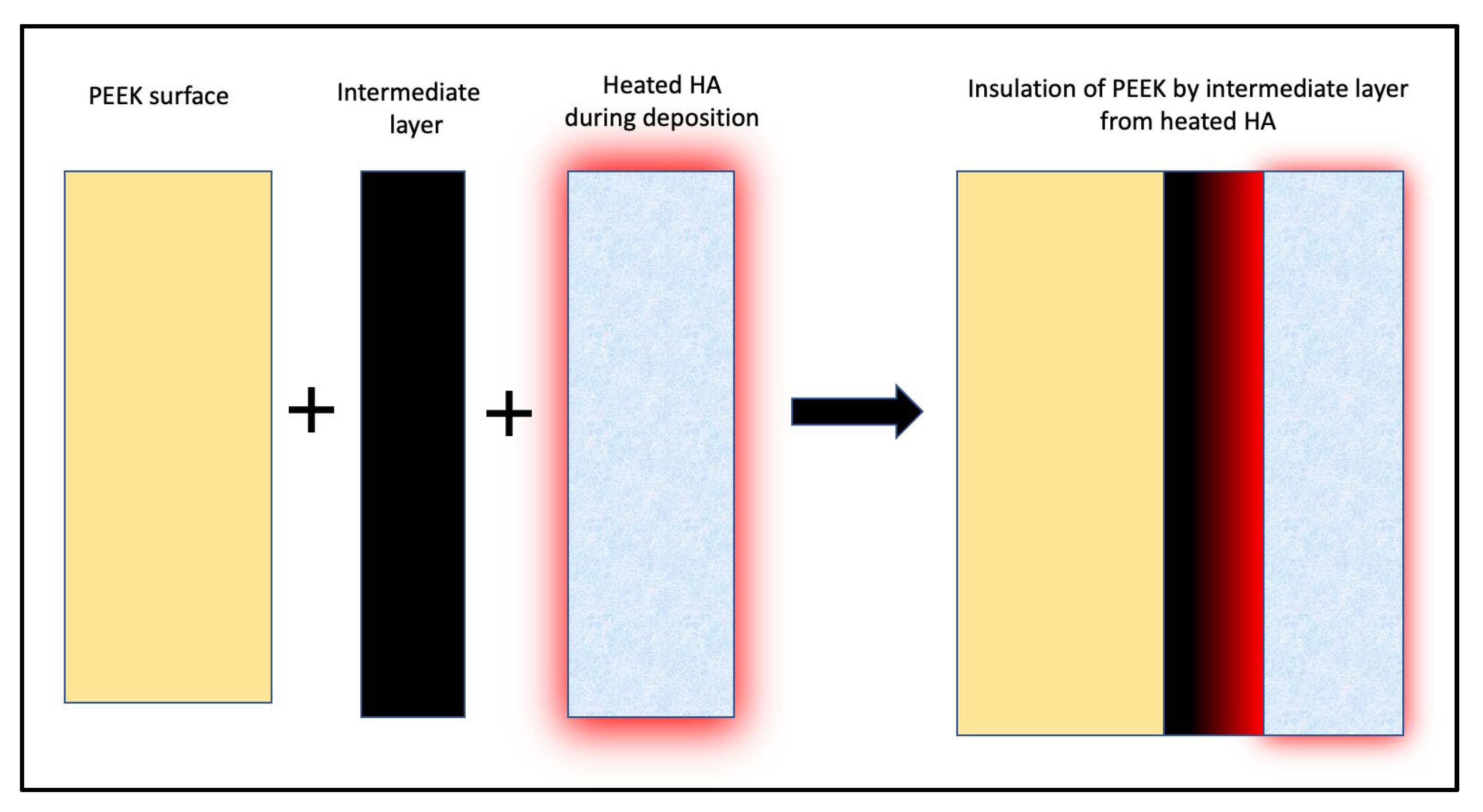
| [Hydroxyapatite/(Hydroxyapatite + Microwave annealing)] + YSZ intermediate layer | In vitro: Increased cell adhesion and proliferation with Hydroxyapatite crystallization with microwave annealing | Rabiei et al. [36] |
| Hydroxyapatite + Titanium intermediate layer + Hydrothermal treatment | In vitro: Bond strength of HA with PEEK with <10 nm Ti layer greater than that with >50 nm Ti layer | Ozeki et al. [37] |
| [Hydroxyapatite/(Hydroxyapatite + Microwave annealing + Autoclaving)] + YSZ intermediate layer | In vitro: Increased cell adhesion and proliferation with Hydroxyapatite crystallization with heat treatment | Durham et al. [35] |
3.2. Titanium Coating
| Treatment | Result | Author |
|---|---|---|
| Surface coatings: Titanium | ||
| Titanium [Pre-treated with grit blasting + Vacuum plasma (element unspecified)] | In vitro: Increased proliferation and differentiation of MC3T3-E1 cells In vivo: Increased osseointegration |
Liu et al. 2021 [42] |
| Titanium + alkali treatment | In vitro: Increased adhesion and proliferation of pre-osteoblasts | Yang et al. [43] |
| (Oxygen plasma/Sandblasting) + Titanium sol + Hydrochloric acid | In vitro: Increased cell response In vivo: Increased osseointegration |
Shimizu et al. [44] |
| Titanium dioxide (Pre-treatment: Argon ion + Titanium layer) | In vivo: Increased osseointegration and bond strength in pull-out test | Tsou et al. [45] |
3.3. Anti-Microbial Agent Coating
| Treatment | Results | Author |
|---|---|---|
| Surface coatings—Antibiotic agents with carrier | ||
| Brushite + Gentamycin sulphate | In vitro: Sustained biocompatibility and increased proliferation and differentiation of pre-osteoblastic cells In vivo: Increased antimicrobial resistance and osseointegration |
Xue et al. [46] |
| Antimicrobial peptide (AMP) of GL13K/[AMP of GL13K + 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC)] | In vitro: Increased antibacterial activity against S. aureus | Hu et al. [48] |
| Red selenium nanorods/Gray selenium nanoparticles | In vitro: Increased antimicrobial activity to P. aeruginosa | Wang et al. [47] |
3.4. Biomolecule Coating
3.5. Polymer Coating
| Treatment | Results | Author |
|---|---|---|
| Surface coatings—Biomolecules | ||
| Dexamethasone + Nitrogen plasma treatment + IL-6 | In vitro: Decreased peri-implant inflammatory mediators In vivo: Increased osseointegration |
Xie et al. [49] |
| Zn−Mg-MOF-74 + Dexamethasone | In vitro: Increased antimicrobial activity against S. aureus and E. coli and angiogenic ability In vivo: Increased antimicrobial activity and angiogenic ability and osseointegration |
Xiao et al. [50] |
| Surface coatings: Polymers | ||
| 2-methacryloyloxyethyl phosphorylcholine (MPC) | In vitro: Decrease in contact angle | Kyomoto et al. [51] |
4. Composites of Poly (Ether-Ether-Ketone)
| Treatment | Results | Author |
|---|---|---|
| PEEK + Poly (ether imide) +Titanium dioxide coating | In vitro: Antibacterial resistance against gram-positive and gram-negative bacteria | Díez-Pascual et al. [52] |
| 3D printed PEEK + crystalline Hydroxyapatite | In vitro: Increased adhesion, proliferation and differentiation of pre-osteoblasts and osteogenesis | Oladapo et al. [53] |
| Carbon reinforced PEEK + Zirconium ions using PIII | In vitro: Increased bioactivity of mBMSC cells and increased expression and activity of alkaline phosphatase, increased antibacterial activity against S. aureus, no effect against E. coli | Li et al. [54] |
| Carbon reinforced PEEK + H2SO4 + Oxygen plasma + Calcium phosphate | In vitro: Increased precipitation of apatite nuclei in SBF medium | Yamane et al. [55] |
| Carbon reinforced PEEK + H2SO4 + Dopamine HCl + Titanium carbide | In vitro: Evidence of photothermal antibacterial activity and cytocompatibility In vivo: Evidence of osseointegration |
Du et al. [56] |
| Carbon reinforced PEEK + H2SO4 + Calcium chloride | In vitro: Increased precipitation of apatite nuclei in SBF | Miyasaki et al. [57] |
| Carbon reinforced PEEK + H2SO4 + Oxygen plasma + amorphous Calcium phosphate | In vitro: Increased precipitation of apatite nuclei in SBF medium | Yabutsuka et al. [58] |
| Carbon reinforced PEEK + H2SO4 + Hydroxyapatite | In vitro: Decrease in contact angle | Asante et al. [59] |
References
- Waser-Althaus, J.; Salamon, A.; Waser, M.; Padeste, C.; Kreutzer, M.; Pieles, U.; Müller, B.; Peters, K. Differentiation of human mesenchymal stem cells on plasma-treated polyetheretherketone. J. Mater. Sci. Mater. Med. 2014, 25, 515–525.
- Gan, K.; Liu, H.; Jiang, L.; Liu, X.; Song, X.; Niu, D.; Chen, T.; Liu, C. Bioactivity and antibacterial effect of nitrogen plasma immersion ion implantation on polyetheretherketone. Dent. Mater. 2016, 32, e263–e274.
- Han, X.; Sharma, N.; Spintzyk, S.; Zhou, Y.; Xu, Z.; Thieringer, F.M.; Rupp, F. Tailoring the biologic responses of 3D printed PEEK medical implants by plasma functionalization. Dent. Mater. 2022, 38, 1083–1098.
- Ha, S.-W.; Kirch, M.; Birchler, F.; Eckert, K.-L.; Mayer, J.; Wintermantel, E.; Sittig, C.; Pfund-Klingenfuss, I.; Textor, M.; Spencer, N.D.; et al. Surface activation of polyetheretherketone (PEEK) and formation of calcium phosphate coatings by precipitation. J. Mater. Sci. Mater. Med. 1997, 8, 683–690.
- Liu, C.; Bai, J.; Wang, Y.; Chen, L.; Wang, D.; Ni, S.; Liu, H. The effects of three cold plasma treatments on the osteogenic activity and antibacterial property of PEEK. Dent. Mater. 2021, 37, 81–93.
- Tsougeni, K.; Vourdas, N.; Tserepi, A.; Gogolides, E.; Cardinaud, C. Mechanisms of Oxygen Plasma Nanotexturing of Organic Polymer Surfaces: From Stable Super Hydrophilic to Super Hydrophobic Surfaces. Langmuir 2009, 25, 11748–11759.
- Rochford, E.T.J.; Subbiahdoss, G.; Moriarty, T.F.; Poulsson, A.H.C.; van der Mei, H.C.; Busscher, H.J.; Richards, R.G. An in vitro investigation of bacteria-osteoblast competition on oxygen plasma-modified PEEK: An in vitro investigation of bacteria-osteoblast competition. J. Biomed. Mater. Res. A 2014, 102, 4427–4434.
- Wang, H.; Lu, T.; Meng, F.; Zhu, H.; Liu, X. Enhanced osteoblast responses to poly ether ether ketone surface modified by water plasma immersion ion implantation. Colloids Surf. B Biointerfaces 2014, 117, 89–97.
- Czwartos, J.; Budner, B.; Bartnik, A.; Wachulak, P.; Butruk-Raszeja, B.A.; Lech, A.; Ciach, T.; Fiedorowicz, H. Effect of Extreme Ultraviolet (EUV) Radiation and EUV Induced, N2 and O2 Based Plasmas on a PEEK Surface’s Physico-Chemical Properties and MG63 Cell Adhesion. Int. J. Mol. Sci. 2021, 22, 8455.
- Kizuki, T.; Matsushita, T.; Kokubo, T. Apatite-forming PEEK with TiO2 surface layer coating. J. Mater. Sci. Mater. Med. 2015, 26, 41.
- Chen, M.; Ouyang, L.; Lu, T.; Wang, H.; Meng, F.; Yang, Y.; Ning, C.; Ma, J.; Liu, X. Enhanced Bioactivity and Bacteriostasis of Surface Fluorinated Polyetheretherketone. ACS Appl. Mater. Interfaces 2017, 9, 16824–16833.
- Ouyang, L.; Chen, M.; Wang, D.; Lu, T.; Wang, H.; Meng, F.; Yang, Y.; Ma, J.; Yeung, K.W.K.; Liu, X. Nano Textured PEEK Surface for Enhanced Osseointegration. ACS Biomater. Sci. Eng. 2019, 5, 1279–1289.
- Akkan, C.K.; Hammadeh, M.E.; May, A.; Park, H.-W.; Abdul-Khaliq, H.; Strunskus, T.; Aktas, O.C. Surface topography and wetting modifications of PEEK for implant applications. Lasers Med. Sci. 2014, 29, 1633–1639.
- Chen, T.; Chen, Q.; Fu, H.; Wang, D.; Gao, Y.; Zhang, M.; Liu, H. Construction and performance evaluation of a sustained release implant material polyetheretherketone with antibacterial properties. Mater. Sci. Eng. C 2021, 126, 112109.
- Wakelin, E.A.; Yeo, G.C.; McKenzie, D.R.; Bilek, M.M.M.; Weiss, A.S. Plasma ion implantation enabled bio-functionalization of PEEK improves osteoblastic activity. APL Bioeng. 2018, 2, 026109.
- Qin, S.; Lu, Z.; Gan, K.; Qiao, C.; Li, B.; Chen, T.; Gao, Y.; Jiang, L.; Liu, H. Construction of a BMP -2 gene delivery system for polyetheretherketone bone implant material and its effect on bone formation in vitro. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 2075–2088.
- Liu, X.; Han, F.; Zhao, P.; Lin, C.; Wen, X.; Ye, X. Layer-by-layer self-assembled multilayers on PEEK implants improve osseointegration in an osteoporosis rabbit model. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1423–1433.
- Jemat, A.; Ghazali, M.J.; Razali, M.; Otsuka, Y. Surface Modifications and Their Effects on Titanium Dental Implants. BioMed Res. Int. 2015, 2015, 791725.
- Albrektsson, T.; Becker, W.; Coli, P.; Jemt, T.; Mölne, J.; Sennerby, L. Bone loss around oral and orthopedic implants: An immunologically based condition. Clin. Implant. Dent. Relat. Res. 2019, 21, 786–795.
- Lu, T.; Wen, J.; Qian, S.; Cao, H.; Ning, C.; Pan, X.; Jiang, X.; Liu, X.; Chu, P.K. Enhanced osteointegration on tantalum-implanted polyetheretherketone surface with bone-like elastic modulus. Biomaterials 2015, 51, 173–183.
- Khoury, J.; Selezneva, I.; Pestov, S.; Tarassov, V.; Ermakov, A.; Mikheev, A.; Lazov, M.; Kirkpatrick, S.R.; Shashkov, D.; Smolkov, A. Surface bioactivation of PEEK by neutral atom beam technology. Bioact. Mater. 2019, 4, 132–141.
- Khoury, J.; Maxwell, M.; Cherian, R.E.; Bachand, J.; Kurz, A.C.; Walsh, M.; Assad, M.; Svrluga, R.C. Enhanced bioactivity and osseointegration of PEEK with accelerated neutral atom beam technology: Enhanced Bioactivity and Osseointegration of Peek. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 531–543.
- Webster, T.J.; Shallenberger, J.R.; Edelman, E.R.; Khoury, J. Accelerated Neutral Atom Beam (ANAB) Modified Poly-Ether-Ether-Ketone for Increasing In Vitro Bone Cell Functions and Reducing Bacteria Colonization without Drugs or Antibiotics. J. Biomed. Nanotechnol. 2022, 18, 788–795.
- Ajami, S.; Coathup, M.J.; Khoury, J.; Blunn, G.W. Augmenting the bioactivity of polyetheretherketone using a novel accelerated neutral atom beam technique: Bioactivity of polyetheretherketone. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 1438–1446.
- Binhasan, M.; Alhamdan, M.M.; Al-Aali, K.A.; Vohra, F.; Abduljabbar, T. Shear bond characteristics and surface roughness of poly-ether-ether-ketone treated with contemporary surface treatment regimes bonded to composite resin. Photodiagnosis Photodyn. Ther. 2022, 38, 102765.
- Peng, T.-Y.; Lin, D.-J.; Mine, Y.; Tasi, C.-Y.; Li, P.-J.; Shih, Y.-H.; Chiu, K.-C.; Wang, T.-H.; Hsia, S.-M.; Shieh, T.-M. Biofilm Formation on the Surface of (Poly)Ether-Ether-Ketone and In Vitro Antimicrobial Efficacy of Photodynamic Therapy on Peri-Implant Mucositis. Polymers 2021, 13, 940.
- Sunarso; Tsuchiya, A.; Fukuda, N.; Toita, R.; Tsuru, K.; Ishikawa, K. Effect of micro-roughening of poly(ether ether ketone) on bone marrow derived stem cell and macrophage responses, and osseointegration. J. Biomater. Sci. Polym. Ed. 2018, 29, 1375–1388.
- Xie, H.; Zhang, C.; Wang, R.; Tang, H.; Mu, M.; Li, H.; Guo, Y.; Yang, L.; Tang, K. Femtosecond laser-induced periodic grooves and nanopore clusters make a synergistic effect on osteogenic differentiation. Colloids Surf. B Biointerfaces 2021, 208, 112021.
- Ma, R.; Wang, J.; Li, C.; Ma, K.; Wei, J.; Yang, P.; Guo, D.; Wang, K.; Wang, W. Effects of different sulfonation times and post-treatment methods on the characterization and cytocompatibility of sulfonated PEEK. J. Biomater. Appl. 2020, 35, 342–352.
- Cheng, Q.; Yuan, B.; Chen, X.; Yang, X.; Lin, H.; Zhu, X.; Zhang, K.; Zhang, X. Regulation of surface micro/nano structure and composition of polyetheretherketone and their influence on the behavior of MC3T3-E1 pre-osteoblasts. J. Mater. Chem. B 2019, 7, 5713–5724.
- Wang, W.; Luo, C.J.; Huang, J.; Edirisinghe, M. PEEK surface modification by fast ambient-temperature sulfonation for bone implant applications. J. R. Soc. Interface 2019, 16, 20180955.
- Liu, L.; Zheng, Y.; Zhang, Q.; Yu, L.; Hu, Z.; Liu, Y. Surface phosphonation treatment shows dose-dependent enhancement of the bioactivity of polyetheretherketone. RSC Adv. 2019, 9, 30076–30086.
- Zheng, Y.; Liu, L.; Xiao, L.; Zhang, Q.; Liu, Y. Enhanced osteogenic activity of phosphorylated polyetheretherketone via surface-initiated grafting polymerization of vinylphosphonic acid. Colloids Surf. B Biointerfaces 2019, 173, 591–598.
- Mahjoubi, H.; Buck, E.; Manimunda, P.; Farivar, R.; Chromik, R.; Murshed, M.; Cerruti, M. Surface phosphonation enhances hydroxyapatite coating adhesion on polyetheretherketone and its osseointegration potential. Acta Biomater. 2017, 47, 149–158.
- Durham, J.W.; Allen, M.J.; Rabiei, A. Preparation, characterization and in vitro response of bioactive coatings on polyether ether ketone: Response Of Bioactive Coatings on Polyether Ether Ketone. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 560–567.
- Rabiei, A.; Sandukas, S. Processing and evaluation of bioactive coatings on polymeric implants: Processing and Evaluation of Bioactive HA Coatings on PEEK. J. Biomed. Mater. Res. A 2013, 101A, 2621–2629.
- Ozeki, K.; Masuzawa, T.; Aoki, H. Fabrication of hydroxyapatite thin films on polyetheretherketone substrates using a sputtering technique. Mater. Sci. Eng. C 2017, 72, 576–582.
- Johansson, P.; Jimbo, R.; Kjellin, P.; Chrcanovic, B.; Wennerberg, A.; Currie, F. Biomechanical evaluation and surface characterization of a nano-modified surface on PEEK implants: A study in the rabbit tibia. Int. J. Nanomed. 2014, 9, 3903.
- Dhinakarsamy, V.; Jayesh, R. Osseointegration. J. Pharm. Bioallied Sci. 2015, 7, 228.
- Karthik, K.; Sivakumar; Sivaraj; Thangaswamy, V. Evaluation of implant success: A review of past and present concepts. J. Pharm. Bioallied Sci. 2013, 5, 117.
- Tschernitschek, H.; Borchers, L.; Geurtsen, W. Nonalloyed titanium as a bioinert metal—A review. Quintessence Int. Berl. Ger. 2005, 36, 523–530.
- Liu, C.; Zhang, Y.; Xiao, L.; Ge, X.; Öner, F.C.; Xu, H. Vacuum plasma sprayed porous titanium coating on polyetheretherketone for ACDF improves the osteogenic ability: An in vitro and in vivo study. Biomed. Microdevices 2021, 23, 21.
- Yang, Y.; Zhang, H.; Komasa, S.; Kusumoto, T.; Kuwamoto, S.; Okunishi, T.; Kobayashi, Y.; Hashimoto, Y.; Sekino, T.; Okazaki, J. Immunomodulatory Properties and Osteogenic Activity of Polyetheretherketone Coated with Titanate Nanonetwork Structures. Int. J. Mol. Sci. 2022, 23, 612.
- Shimizu, T.; Fujibayashi, S.; Yamaguchi, S.; Yamamoto, K.; Otsuki, B.; Takemoto, M.; Tsukanaka, M.; Kizuki, T.; Matsushita, T.; Kokubo, T.; et al. Bioactivity of sol–gel-derived TiO2 coating on polyetheretherketone: In vitro and in vivo studies. Acta Biomater. 2016, 35, 305–317.
- Tsou, H.-K.; Chi, M.-H.; Hung, Y.-W.; Chung, C.-J.; He, J.-L. In Vivo Osseointegration Performance of Titanium Dioxide Coating Modified Polyetheretherketone Using Arc Ion Plating for Spinal Implant Application. BioMed Res. Int. 2015, 2015, 328943.
- Xue, Z.; Wang, Z.; Sun, A.; Huang, J.; Wu, W.; Chen, M.; Hao, X.; Huang, Z.; Lin, X.; Weng, S. Rapid construction of polyetheretherketone (PEEK) biological implants incorporated with brushite (CaHPO4·2H2O) and antibiotics for anti-infection and enhanced osseointegration. Mater. Sci. Eng. C 2020, 111, 110782.
- Wang, Q.; Mejía Jaramillo, A.; Pavon, J.J.; Webster, T.J. Red selenium nanoparticles and gray selenium nanorods as antibacterial coatings for PEEK medical devices: Antibacterial Coatings for Peek Medical Devices. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 104, 1352–1358.
- Hu, C.-C.; Kumar, S.R.; Vi, T.T.T.; Huang, Y.-T.; Chen, D.W.; Lue, S.J. Facilitating GL13K Peptide Grafting on Polyetheretherketone via 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide: Surface Properties and Antibacterial Activity. Int. J. Mol. Sci. 2021, 23, 359.
- Xie, L.; Wang, G.; Wu, Y.; Liao, Q.; Mo, S.; Ren, X.; Tong, L.; Zhang, W.; Guan, M.; Pan, H.; et al. Programmed surface on poly(aryl-ether-ether-ketone) initiating immune mediation and fulfilling bone regeneration sequentially. Innovation 2021, 2, 100148.
- Xiao, T.; Fan, L.; Liu, R.; Huang, X.; Wang, S.; Xiao, L.; Pang, Y.; Li, D.; Liu, J.; Min, Y. Fabrication of Dexamethasone-Loaded Dual-Metal–Organic Frameworks on Polyetheretherketone Implants with Bacteriostasis and Angiogenesis Properties for Promoting Bone Regeneration. ACS Appl. Mater. Interfaces 2021, 13, 50836–50850.
- Kyomoto, M.; Moro, T.; Takatori, Y.; Kawaguchi, H.; Nakamura, K.; Ishihara, K. Self-initiated surface grafting with poly(2-methacryloyloxyethyl phosphorylcholine) on poly(ether-ether-ketone). Biomaterials 2010, 31, 1017–1024.
- Díez-Pascual, A.M.; Díez-Vicente, A.L. Nano-TiO2 Reinforced PEEK/PEI Blends as Biomaterials for Load-Bearing Implant Applications. ACS Appl. Mater. Interfaces 2015, 7, 5561–5573.
- Oladapo, B.I.; Ismail, S.O.; Bowoto, O.K.; Omigbodun, F.T.; Olawumi, M.A.; Muhammad, M.A. Lattice design and 3D-printing of PEEK with Ca10(OH)(PO4)3 and in-vitro bio-composite for bone implant. Int. J. Biol. Macromol. 2020, 165, 50–62.
- Li, J.; Qian, S.; Ning, C.; Liu, X. rBMSC and bacterial responses to isoelastic carbon fiber-reinforced poly(ether-ether-ketone) modified by zirconium implantation. J. Mater. Chem. B 2016, 4, 96–104.
- Yamane, Y.; Yabutsuka, T.; Takaoka, Y.; Ishizaki, C.; Takai, S.; Fujibayashi, S. Surface Modification of Carbon Fiber-Polyetheretherketone Composite to Impart Bioactivity by Using Apatite Nuclei. Materials 2021, 14, 6691.
- Du, T.; Zhao, S.; Dong, W.; Ma, W.; Zhou, X.; Wang, Y.; Zhang, M. Surface Modification of Carbon Fiber-Reinforced Polyetheretherketone with MXene Nanosheets for Enhanced Photothermal Antibacterial Activity and Osteogenicity. ACS Biomater. Sci. Eng. 2022, 8, 2375–2389.
- Miyazaki, T.; Matsunami, C.; Shirosaki, Y. Bioactive carbon–PEEK composites prepared by chemical surface treatment. Mater. Sci. Eng. C 2017, 70, 71–75.
- Yabutsuka, T.; Fukushima, K.; Hiruta, T.; Takai, S.; Yao, T. Fabrication of Bioactive Fiber-reinforced PEEK and MXD6 by Incorporation of Precursor of Apatite: Fabrication of bioactive fiber-reinforced peek and mxd6. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 2254–2265.
- Addai Asante, N.; Wang, Y.; Bakhet, S.; Kareem, S.; Owusu, K.A.; Hu, Y.; Appiah, M. Ambient temperature sulfonated carbon fiber reinforced PEEK with hydroxyapatite and reduced graphene oxide hydroxyapatite composite coating. J. Biomed. Mater. Res. B Appl. Biomater. 2021, 109, 2174–2183.




