Polymers, in general, and Poly (Ether-Ether-Ketone) (PEEK) have emerged as potential alternatives to conventional osseous implant biomaterials. Due to its distinct advantages over metallic implants, PEEK has been gaining increasing attention as a prime candidate for orthopaedic and dental implants. Although a myriad of permutations and combinations of different surface treatments are employed to alter the surface topography of PEEK, for the sake of simplicity, these treatments have been classified into the following categories: physical treatment, chemical treatment, surface coating, and composite preparation, with the first surface treatment in the combination determining the classification. Though these terms are arbitrary and could lead to considerable overlap, physical and chemical treatments can be grouped into a subtractive form of surface modification while surface coating can be regarded as an additive form.
- dental implant
- orthopedic implant
- implant biomaterial
- polymer
1. Physical Treatment
1.1. Plasma Treatment
| Treatment | Results | Author |
|---|---|---|
| Plasma | ||
| Oxygen/Ammonia | In-vitro: Increased adhesion, proliferation, and osteogenic differentiation of cells as compared to control | Althaus et al. [22] |
| Nitrogen | In-vitro: Increase in bioactivity and antibacterial properties with reference to S. aureus. | Gan et al. [23] |
| Oxygen/Argon | In-vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of SAOS-2 osteoblasts | Han et al. [24] |
| Oxygen/Nitrogen | In-vitro: Decrease in contact angle and no disadvantageous effect on cytocompatibility; | Ha et al. [25] |
| Nitrogen/Argon/(Nitrogen + Argon) | In-vitro: Increase in osteogenic activity (Highest: Nitrogen) and antibacterial property (Highest: Nitrogen + Argon) | Liu et al. [26] |
| Oxygen | In-vitro: Decrease in contact angle | Tsougeni et al. [27] |
| Oxygen | In-vitro: Increased cell adhesion and spreading of U2-OS osteoblasts in the presence of S. epidermidis | Rochford et al. [28] |
| Water vapour/Argon | In-vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of osteoblast precursor cell line derived from Mus musculus (mouse) calvaria (MC3T3-E1). | Wang et al. [12] |
| Plasma treatment + Radiation | ||
| EUV + (low temperature Nitrogen/Oxygen) | In-vitro: Decreased contact angle and increased cell adhesion of MG63 cells, Cell adhesion higher with Nitrogen plasma | Czwartos et al. [29] |
| Oxygen/UV | In-vitro: Increase in the bond strength to TiO2 sol solution after exposure to O2 plasma/UV radiation | Kizuki et al. [30] |
| Plasma + Chemical treatment | ||
| Argon + Hydrofluoric acid | In-vitro: Decreased contact angle and increased cell proliferation and differentiation of rBMS cells (Higher with Nitrogen) In-vivo: Increased resistance to Porphyromonas gingivalis (P. gingivalis) |
Chen et al. [31] |
| Argon/(Argon + Hydrogen peroxide) | In-vitro: Increased cell adhesion, collagen secretion, and extra-cellular matrix deposition (Higher with Argon, Peroxide combination) In-vivo: Increased fibrous tissue filtration inhibition and osseointegration with Argon, Peroxide combination |
Ouyang et al. [32] |
| Plasma + Laser | ||
| Oxygen + Nd:YAG | In vitro: Decrease in contact angle | Akkan et al. [33] |
| Plasma + Biomolecules/Inorganic coating | ||
| Argon + Polydopamine (PDA) + Vancomycin gelatin nanoparticles | In vitro: No cytotoxicity and increased antibacterial resistance to Staphylococcus aureus (S. aureus) and Streptococcus mutans (S. mutans) | Chen et al. [34] |
| Nitrogen + Tropoelastin | In vitro: Increased bioactivity of osteogenic cells | Wakelin et al. [35] |
| Nitrogen + PDA + Poly (lactic-co-glycolic acid) carrying Bone Morphogenic Protein-2 (BMP-2) gene | In vitro: Increased osteogenic activity | Qin et al. [36] |
| (Argon/Oxygen) + Acrylic acid vapours + Polystyrene sulfonate (PSS) and polyallylamine hydrochloride (PAH) multilayers | In vitro: Increased adhesion and proliferation of bone marrow stromal cells In vivo: Increased osseointegration |
Liu et al. [37] |
1.2. Accelerated Neutral Atom Beam (ANAB)
| Treatment | Result | Author |
|---|---|---|
| ANAB | In vitro: Decreased contact angle and increased bioactivity of osteogenic cells | Khoury et al. [41] |
| ANAB | In vitro: Increased wettability and cell adhesion, spreading, proliferation, and differentiation of SAOS-2 osteoblasts In vivo: Increased bond strength to bone |
Khoury et al. [42] |
| ANAB | In vitro: Improved osteoblastic response and decrease in bacterial colonization of MRSA, S. epidermidis, and E. coli | Webster et al. [43] |
| ANAB | In vitro: Decreased contact angle and increased bioactivity of osteogenic cells | Ajami et al. [44] |
1.3. Photodynamic Treatment
1.4. Sandblasting
1.5. Laser
| Treatment | Result | Author |
|---|---|---|
| Photodynamic therapy | ||
| (Temporfin/Ampicillin) + Diode laser | In vitro: Increase in resistance to microbial load | Peng et al. [46] |
| PDT/Sulphuric acid (H2SO4)/Air abrasion (Al/Diamond) | In vitro: Lower shear bond strength and microroughness of samples treated with PDT as compared to H2SO4 and Alumina particle air abrasion (Highest: H2SO4) | Binhasan et al. [45] |
| Sandblasting | ||
| Alumina particles | In vitro: Increased proliferation and differentiation of rat MSCs and mitigation of inflammatory chemokine (C-C motif) Ligand 2 (CCL2) | Sunarso et al. [47] |
| Laser | ||
| Femtosecond laser | In vitro: Increased adhesion, proliferation and differentiation of mBMSC cells and increased expression and activity of alkaline phosphatase | Xie et al. [48] |
2. Chemical Treatment
2.1. Sulphonation
2.2. Phosphonation
2.3. Silanization
3. Surface Coatings
3.1. Hydroxyapatite Coating
| Treatment | Result | Author |
|---|---|---|
| Surface coatings—Hydroxyapatite | ||
| Hydroxyapatite | In vivo: Increased removal torque and biocompatibility | Johansson et al. [73] |
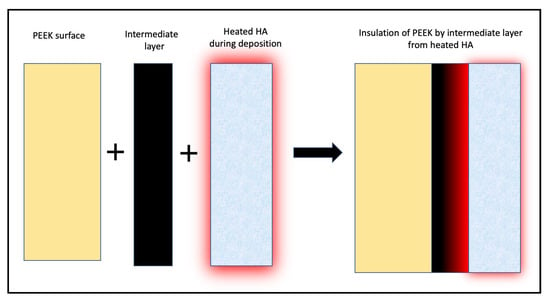
| [Hydroxyapatite/(Hydroxyapatite + Microwave annealing)] + YSZ intermediate layer | In vitro: Increased cell adhesion and proliferation with Hydroxyapatite crystallization with microwave annealing | Rabiei et al. [71] |
| Hydroxyapatite + Titanium intermediate layer + Hydrothermal treatment | In vitro: Bond strength of HA with PEEK with <10 nm Ti layer greater than that with >50 nm Ti layer | Ozeki et al. [72] |
| [Hydroxyapatite/(Hydroxyapatite + Microwave annealing + Autoclaving)] + YSZ intermediate layer | In vitro: Increased cell adhesion and proliferation with Hydroxyapatite crystallization with heat treatment | Durham et al. [70] |
3.2. Titanium Coating
| Treatment | Result | Author |
|---|---|---|
| Surface coatings: Titanium | ||
| Titanium [Pre-treated with grit blasting + Vacuum plasma (element unspecified)] | In vitro: Increased proliferation and differentiation of MC3T3-E1 cells In vivo: Increased osseointegration |
Liu et al. 2021 [79] |
| Titanium + alkali treatment | In vitro: Increased adhesion and proliferation of pre-osteoblasts | Yang et al. [80] |
| (Oxygen plasma/Sandblasting) + Titanium sol + Hydrochloric acid | In vitro: Increased cell response In vivo: Increased osseointegration |
Shimizu et al. [81] |
| Titanium dioxide (Pre-treatment: Argon ion + Titanium layer) | In vivo: Increased osseointegration and bond strength in pull-out test | Tsou et al. [82] |
3.3. Anti-Microbial Agent Coating
| Treatment | Results | Author |
|---|---|---|
| Surface coatings—Antibiotic agents with carrier | ||
| Brushite + Gentamycin sulphate | In vitro: Sustained biocompatibility and increased proliferation and differentiation of pre-osteoblastic cells In vivo: Increased antimicrobial resistance and osseointegration |
Xue et al. [83] |
| Antimicrobial peptide (AMP) of GL13K/[AMP of GL13K + 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC)] | In vitro: Increased antibacterial activity against S. aureus | Hu et al. [85] |
| Red selenium nanorods/Gray selenium nanoparticles | In vitro: Increased antimicrobial activity to P. aeruginosa | Wang et al. [84] |
3.4. Biomolecule Coating
3.5. Polymer Coating
| Treatment | Results | Author |
|---|---|---|
| Surface coatings—Biomolecules | ||
| Dexamethasone + Nitrogen plasma treatment + IL-6 | In vitro: Decreased peri-implant inflammatory mediators In vivo: Increased osseointegration |
Xie et al. [86] |
| Zn−Mg-MOF-74 + Dexamethasone | In vitro: Increased antimicrobial activity against S. aureus and E. coli and angiogenic ability In vivo: Increased antimicrobial activity and angiogenic ability and osseointegration |
Xiao et al. [87] |
| Surface coatings: Polymers | ||
| 2-methacryloyloxyethyl phosphorylcholine (MPC) | In vitro: Decrease in contact angle | Kyomoto et al. [88] |
4. Composites of Poly (Ether-Ether-Ketone)
| Treatment | Results | Author |
|---|---|---|
| PEEK + Poly (ether imide) +Titanium dioxide coating | In vitro: Antibacterial resistance against gram-positive and gram-negative bacteria | Díez-Pascual et al. [89] |
| 3D printed PEEK + crystalline Hydroxyapatite | In vitro: Increased adhesion, proliferation and differentiation of pre-osteoblasts and osteogenesis | Oladapo et al. [90] |
| Carbon reinforced PEEK + Zirconium ions using PIII | In vitro: Increased bioactivity of mBMSC cells and increased expression and activity of alkaline phosphatase, increased antibacterial activity against S. aureus, no effect against E. coli | Li et al. [91] |
| Carbon reinforced PEEK + H2SO4 + Oxygen plasma + Calcium phosphate | In vitro: Increased precipitation of apatite nuclei in SBF medium | Yamane et al. [92] |
| Carbon reinforced PEEK + H2SO4 + Dopamine HCl + Titanium carbide | In vitro: Evidence of photothermal antibacterial activity and cytocompatibility In vivo: Evidence of osseointegration |
Du et al. [93] |
| Carbon reinforced PEEK + H2SO4 + Calcium chloride | In vitro: Increased precipitation of apatite nuclei in SBF | Miyasaki et al. [94] |
| Carbon reinforced PEEK + H2SO4 + Oxygen plasma + amorphous Calcium phosphate | In vitro: Increased precipitation of apatite nuclei in SBF medium | Yabutsuka et al. [95] |
| Carbon reinforced PEEK + H2SO4 + Hydroxyapatite | In vitro: Decrease in contact angle | Asante et al. [96] |
This entry is adapted from the peer-reviewed paper 10.3390/biom13030464
