There are several classifications for vertebral bone lesions. By itself, vertebral bone lesions are a form of spinal lesion that only affects the osseous portion; thus, they are referred to as spinal osseous lesions, spinal neoplasms, vertebral lesions, or vertebral tumors. A vertebral primary bone lesion is a general term describing any abnormal change to the bone originating from disease or injury to healthy bone. In this context, primary is an oncological term that indicates the lesion originates from the bone, whereas secondary lesions are when the lesion metastasizes to the bone from another region of the body. When cells in the bone undergo uncontrolled growth, these lesions are referred to as bone tumors, and when the abnormal tissue closely resembles the healthy bone structure, the lesion is considered benign. Examples of benign lesions include hemangiomas, lipomas, sclerosis, aneurysmal bone cysts, osteoid osteomas, and osteoblastomas. Malignant lesions are similar to bone tumors but demonstrate a growth capable of metastasis. Malignant vertebral lesions include chondrosarcoma, chordoma, Ewing’s sarcoma, neuroblastoma, and osteosarcoma. Classification of a lesion depends on the spinal level, location of the lesion on the vertebra, layer of bone affected, number of lesions, and morphology. Typically, since lesion type determines treatment, correct identification of the lesion can have a major role in clinical outcomes.
1. Introduction
Vertebral primary bone lesions have long presented a challenge to spinal care specialists. Not only is there a wide variety of spinal lesions described in the literature, the treatment of these tumors, benign or otherwise, is often complex and complicated by factors such as neural compression
[1]. Vertebral lesions are also frequently found incidentally when the patient presents with back pain, weakness, or myelopathy, and if management is delayed, vertebral lesions can lead to a complete loss of sensory and motor function
[2]. A thorough, comprehensive understanding of the assessment and treatment of these lesions is needed.
2. Incidence Rates
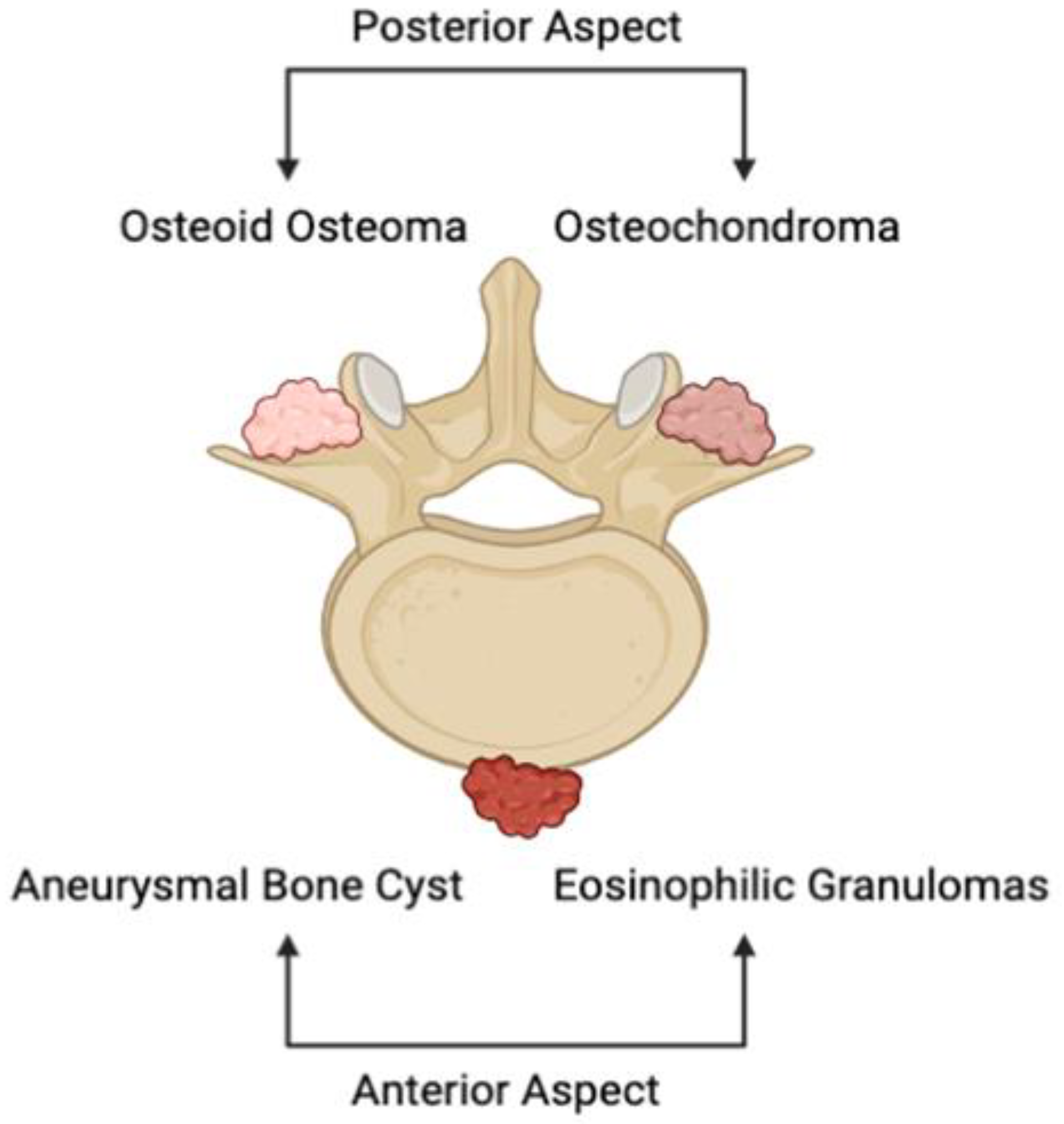
Primary osseous lesions of the spine encompass a divergent series of malignant and benign tumors. The majority, which are non-cancerous, can be primarily found in the anterior portion of the vertebral body (
Figure 1)
[3]. Examples of benign tumors of the vertebrae include aneurysmal bone cysts, eosinophilic granulomas, and hemangiomas. Others, notably osteoid osteomas and osteochondromas, are more commonly witnessed in the posterior elements of the vertebral body (
Figure 1). While the growths in question are considerably less prevalent than the occurrence of metastases, primary bone tumors of the vertebrae constitute the most prevalent category of primary osseous lesions
[4]. Nevertheless, the true incidence of primary tumors of the spine is unclear due to their infrequency and the fact that the majority of these growths present asymptomatically
[5]. Primary vertebral tumors are seen to comprise approximately 0.2% of all cancers that are newly identified each year, further accounting for 5% of the overarching bone tumors category
[6]. A thorough inspection of these incidence rates has led to the identification of an emergent trend: more than 90% of lesions can be found to be benign when a person is in their first decade of life, around 50% when they are in the fourth decade, and fewer than 10% when they are in the seventh decade
[7]. Of those found cancerous, the rates of recurrence and mortality are elevated up to 48% and 58%, respectively
[4]. In spite of the fact that these spinal growths are largely heterogeneous, it is still possible to arrive at an appropriate differential diagnosis and treatment through the methodical consideration of a patient’s full history of the present illness and radiological pattern.
Figure 1. Illustrative depiction of the anatomical location of common primary osseous lesions of the vertebrae. Aneurysmal bone cysts and eosinophilic granulomas depict prevalent primary vertebral tumors of the anterior portion of the spine, while osteoid osteomas and osteochondromas represent lesions that represent those witnessed on the posterior portion of the vertebrae.
3. Clinical Considerations
When examining individuals with spine tumors, the history of present and prospective lesions, as well as carcinogen exposure, must be assessed. Previously, accounts of oncological patients that harbored spinal metastases years after effective treatment have been reported
[5]. As such, it is crucial to consider that benign skeletal lesions in any region of the body may culminate in spine metastasis following malignant or sarcomatous transformation
[8]. In individuals with vertebral growths, pain is perhaps the most prevalent and predominant symptom
[9][10]. As seen with the vast majority of skeletal system tumors, patients may attribute their pain to a factual or hypothesized traumatic event that occurred in the recent past
[5]. Occasionally, this situation implies a pathological fracture resulting from the collapse of a vertebral body due to physical trauma
[11]. In the same realm, the most consistent characteristic of primary osseous lesions is discomfort that develops gradually, intensifies with time, and persists at night, ultimately impacting sleeping behavior
[10]. Acute pain that develops in the absence of trauma in a patient with no preceding symptoms should also be regarded as a pathological fracture in such a clinical context
[5].
4. Imaging Considerations
Despite the fact that the majority of presentations of low back pain heal with conservative therapy, radiographs are frequently employed as an initial preventive screening. The quick availability and inexpensive cost of radiographs prove useful when assessing for fractures, vertebral degeneration, and bone density
[12][13]. For patients presenting with more severe symptoms, suspected underlying infection, or implications of the cauda equina, CT and MRI are the superior imaging modalities employed
[14]. CT allows for better visualization of the tumor microenvironment, even to a greater extent than MRI
[9]. Furthermore, it enhances the visibility of pathological degenerative developments and fractures, especially in the posterior components
[12]. On the other hand, MRIs are more frequently utilized in the presence of secondary neurological symptoms, providing increased soft tissue contrast to CT to characterize intervertebral disks, spinal bone marrow, and contents of the vertebral foramen
[9][13]. Together, however, CT and MRI are utilized in unison to depict a full picture of the issue.
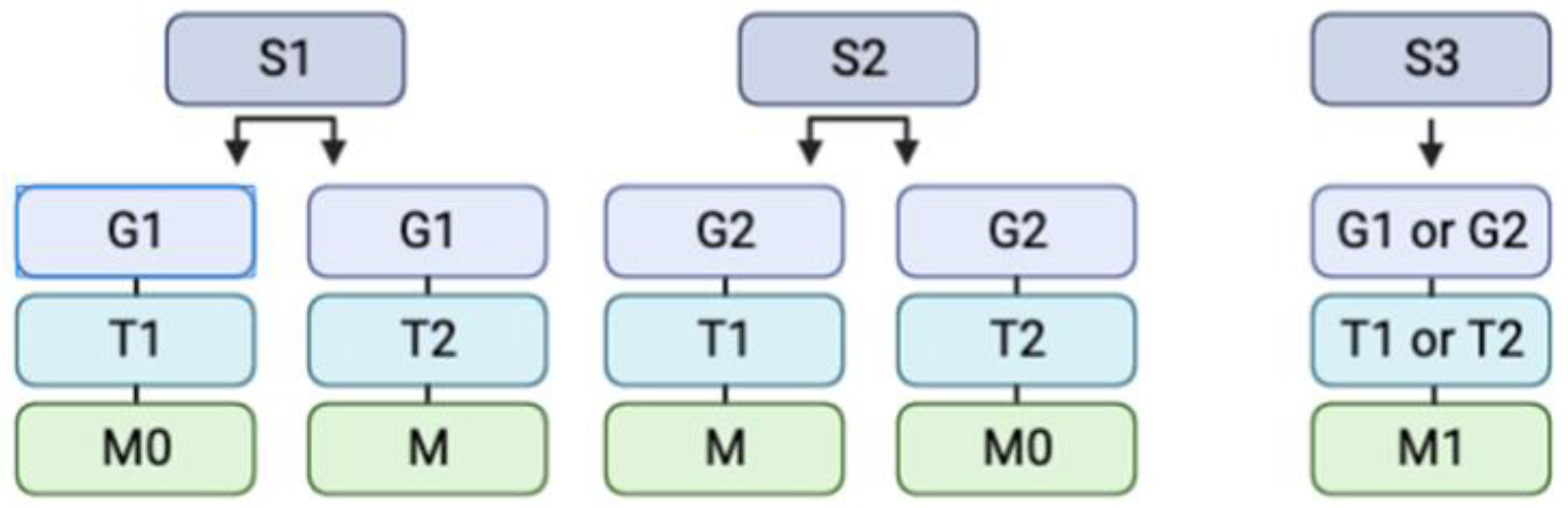
On radiographs, lesions are often classified utilizing the Enneking classification system, which aids in the assignment of tumors into two categories: benign and malignant (
Figure 2)
[14][15]. In accordance with the Enneking classification system, non-cancerous tumors are further divided into the following categories: S1 indicates that the growth is inactive, asymptomatic, developing slowly or not at all, and has a true capsule
[16]. S2 indicates that the lesion is mildly symptomatic, developing with an outline, and displays a minimal risk of recurrence
[15]. Finally, S3 indicates that the tumor is expanding fast, the capsule has been broken or is completely missing, there is an invasion of surrounding tissues, and the recurrence rate is significant
[16]. The localization of the tumors is delineated through the use of T1 and T2 designations, defining intraosseous or extraosseous growth accordingly. It should not go without consideration that the presence of metastasis is noted as well. Similarly, lesions may be categorized additionally according to their grade: 1 and 2 are indicative of a low and high grade, respectively
[17]. Ultimately, however, descriptive words help radiologists and neurosurgeons distinguish growths. For instance, hemangiomas can be described as having a “salt and pepper” look, with a high signal intensity, and exhibiting considerable contrast
[18][19]. Osteoid osteomas, in comparison, may reveal a radiolucent tumor with surrounding sclerosis, bearing a resemblance to a “sunny-side-up egg”
[20][21][22]. A full list of the salient radiographic findings for common benign and malignant bony tumors is provided in
Table 1.
Figure 2. Illustrative depiction of a simplified Enneking classification system, which categorizes tumors into stage, grade, site, and presence of metastasis. The abbreviations are as follows: S = Stage (1, 2, or 3), G = Grade (1 or 2), T = Site (1 or 2), and M = Metastasis (0 or 1). S1 indicates that the growth is inactive, asymptomatic, developing slowly or not at all, and has a true capsule. S2 indicates that the lesion is mildly symptomatic, developing with an outline, and displays a minimal risk of recurrence. S3 indicates that the tumor is expanding fast, the capsule has been broken or is completely missing, there is invasion of surrounding tissues, and the recurrence rate is significant. G1 and G2 are indicative of low and high grades, accordingly. The T1 and T2 indicate intraosseous and extraosseous growth, respectively. Finally, M0 indicates the absence of metastasis and M1 the presence of metastasis.
Table 1. Common primary benign and malignant vertebral lesions and their associated radiographic findings on Magnetic Resonance Imaging (MRI)
[19][22].