Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Venugopal Rao Soma | -- | 5240 | 2023-03-06 16:29:13 | | | |
| 2 | Camila Xu | Meta information modification | 5240 | 2023-03-07 01:25:27 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Beeram, R.; Vepa, K.R.; Soma, V.R. SERS-Based Plasmonic Sensors for Biosensing Applications. Encyclopedia. Available online: https://encyclopedia.pub/entry/41906 (accessed on 03 March 2026).
Beeram R, Vepa KR, Soma VR. SERS-Based Plasmonic Sensors for Biosensing Applications. Encyclopedia. Available at: https://encyclopedia.pub/entry/41906. Accessed March 03, 2026.
Beeram, Reshma, Kameswara Rao Vepa, Venugopal Rao Soma. "SERS-Based Plasmonic Sensors for Biosensing Applications" Encyclopedia, https://encyclopedia.pub/entry/41906 (accessed March 03, 2026).
Beeram, R., Vepa, K.R., & Soma, V.R. (2023, March 06). SERS-Based Plasmonic Sensors for Biosensing Applications. In Encyclopedia. https://encyclopedia.pub/entry/41906
Beeram, Reshma, et al. "SERS-Based Plasmonic Sensors for Biosensing Applications." Encyclopedia. Web. 06 March, 2023.
Copy Citation
Surface-enhanced Raman spectroscopy/scattering (SERS) has evolved into a popular tool for applications in biology and medicine owing to its ease-of-use, non-destructive, and label-free approach. Advances in plasmonics and instrumentation have enabled the realization of SERS’s full potential for the trace detection of biomolecules, disease diagnostics, and monitoring.
biosensing
SERS
plasmonics
disease diagnosis
1. Introduction
Plasmonics is the study of electron oscillations in metal nanostructures and their interaction with electromagnetic radiation. Since its conception in the 1950s, researchers have been interested in studying the fundamentals of the effects of shape, surrounding medium, material, and their interaction with light of different wavelengths [1]. With this well-established knowledge, plasmonics is witnessing an enormous potential for applications in different fields, including forensics [2]; environmental safety [3]; biosensing [4][5][6][7][8][9][10][11], e.g., SARS-CoV-2 detection [12]; and homeland security [13]. The applications of plasmonics majorly rely on surface plasmon resonance (SPR) or localized surface plasmon resonance (LSPR) effects [14]. Some of the significant techniques that were developed using these include higher-order harmonic generation, microscopy, drug delivery, photovoltaics, surface-enhanced Raman spectroscopy (SERS) and fluorescence, and surface-enhanced infrared absorption spectroscopy (SEIAS) and waveguides. The use of plasmonics in these techniques has significantly improved their efficiency over existing conventional techniques, offering flexibility, signal enhancement, and ease of use [15]. Advents in plasmonics have led to the emergence of SERS with impressive signal enhancements over traditional Raman spectroscopy [16]. SERS-based sensing is being widely used for the trace detection of different molecules, such as explosives [17], pesticides [18][19], food adulterants [20][21], drugs [22], biomolecules [23][24][25][26][27], medicine [28][29][30], and microorganisms [31].
SERS typically utilizes localized surface plasmon resonances in metal nanostructures to enhance the weak Raman signal significantly. The phenomenon was first observed by Fleischmann in 1974 while studying pyridine adsorbed on a roughened silver electrode [32]. However, the enhancement was attributed to increased surface area for adsorption. It took further experiments in 1977 by two independent groups, Jeanmaire and van Duyne [33] and Albrecht and Creighton [34], to understand the origin of the enhancement. Now it is established that the enhancement predominantly comes from two mechanisms: electromagnetic enhancement (EE) and chemical enhancement (CE) [35]. The electromagnetic enhancement in SERS is a two-step process, and the total enhancement is multiplicative. When a molecule of interest is in the vicinity of a plasmonic nanostructure, it experiences an enhanced field called local field enhancement (LFE). The molecule then radiates with increased efficiency, referred to as radiation enhancement [36][37]. In addition, there is chemical enhancement which occurs because of charge-transfer mechanisms between nanoparticles and the analyte. Figure 1 summarizes the two enhancement mechanisms in SERS. The type of the plasmonic material, choice of wavelength, surface coverage of the molecules, and concentration of the analyte are the factors that influence SERS’s efficiency [38]. This technique is label-free, rapid, non-destructive, and water compatible and offers the fingerprint of the molecule, making it suitable for numerous applications. Nobel metals such as Au, Ag, and Cu and their alloys are the widely used materials for SERS for their tunability in the visible and IR region, inertness, sensitivity, and compatibility [39][40]. Despite the superior performance of Ag owing to its high-quality resonance in the visible region, Au is the preferred material, as it is known to be biocompatible and non-reactive in an oxygen atmosphere. The near-field enhancement in SERS is dependent on the shape and size of the nanostructures, in addition to the distance between the nanoparticles and distribution of probe molecules around the nanoparticles [41]. The different morphologies of nanoparticles, such as core–shell, rods, spherical, triangular, stars, and nanopyramids, are synthesized by widely reported chemical routes in bottom-up or top-down approaches [42]. Anisotropic nanostructures such as dendrites, rods, stars, and triangle are considered highly desirable for SERS since they enable lower detection limits owing to the lightening-rod effect [43][44]. The performance of SERS is also dependent on the choice of wavelength, and most biological tissues are transparent in the IR region, making it a preferred choice [45]. Recently, there is also growing interest in the UV and deep UV SERS for applications concerning biomolecules such as amino acids and DNA bases because they have electronic transitions in the UV region [39].
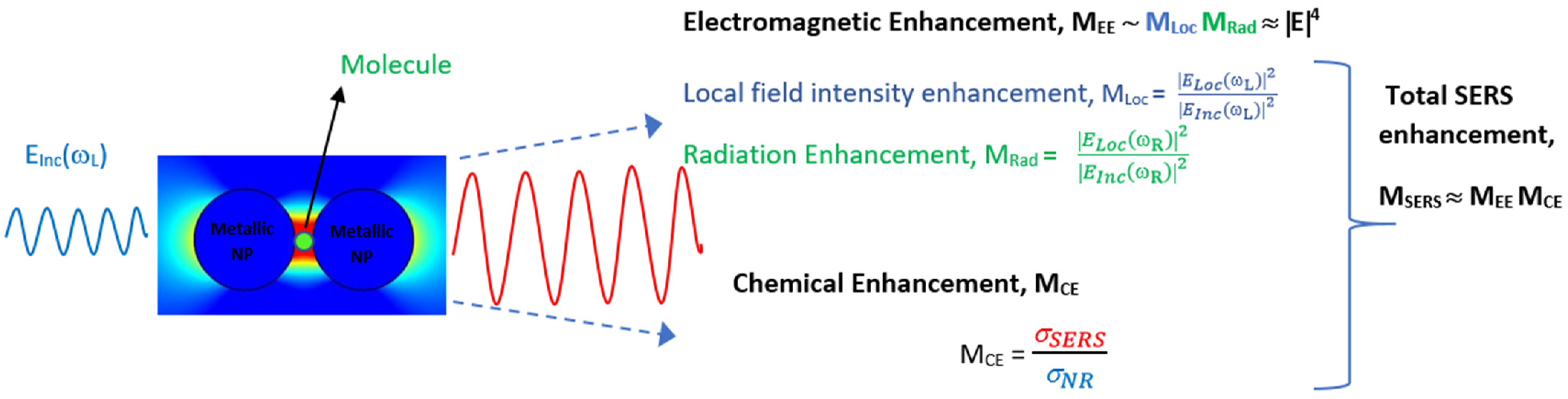
Figure 1. Schematic of total enhancement in SERS via electromagnetic and chemical enhancement mechanisms.
With a growing population and, consequently, the diseases worldwide, there is a need to develop point-of-care (POC) devices that are easy to use, reliable, rapid, and low cost. Over the years, SERS has been proven to possess all of these advantages, including trace detection with sub-picomolar sensitivity. Particularly, there are many reasons for the surge of using SERS for biosensing. Firstly, given the low scattering cross-section of water, SERS is extremely compatible with liquid samples, paving the way for use in biology applications, including liquid biopsy [46][47]. SERS has been widely used for disease diagnosis using urine, blood, serum, plasma, saliva, breath, and tear samples, establishing its compatibility. Measurements in SERS can be performed using liquids, gases, solids, and powders, unlike traditional tests. Secondly, SERS gives specific molecular information, which is often a vibrational fingerprint of the molecule or cell under study. Biomarkers that are Raman active are extensively used for the identification of different diseases, using SERS [48]. Frequently, when the variations are unrecognizable to the human eye, machine learning techniques are used to extract the patterns and discriminate the samples [49]. This was successfully used to classify normal and cancer cells [50], identify microorganism species [51], and monitor disease progression [52]. Thirdly, SERS is a rapid technique, can accomplish trace detection, and has a test time of three to five minutes [53]. Combined with recent developments in flexible SERS sensors, it also offers easy sample-collection methods, such as swabbing from an uneven surface [54]. Lastly, advances in portable instrumentation and low-cost lasers leveraged the usage of SERS for real-world applications [55]. The easy availability of IR lasers that have a low damage threshold with biology samples, as well as quench fluorescence, has favored the development of SERS for biosensing. All of these advantages have made SERS a popular choice for biosensing recently.
2. SERS for Disease Diagnosis
With growing zoonotic diseases, cancers, diabetes, and other ailments, there is a pressing need to develop low-cost and POC identification techniques. Early and rapid diagnosis is the key to saving a life and prevent the rapid transmission of diseases. A trace detection technique such as SERS will aid in tracking the minute changes in cells or biomarkers, thus enabling early diagnosis. SERS is being extensively used for the same in both labeled and label-free approaches, often targeting specific biomarkers of the disease expression [30]. In the label-free approach, the sample is directly studied in contact with the plasmonic material, whereas in the labeled approach, a Raman reporter, such as fluorophores, antibodies, or ligands, is attached to the sample for detection and imaging [56][57]. Different biomarkers, such as proteins, antibodies, miRNAs, exosomes, and DNA, are used as indicators for the presence of the disease. In researchers observation, where full cells, tissues, or body fluids are studied, a machine learning algorithm is used hand in hand for accurate identification. SERS has been used for the detection of conditions such as Alzheimer’s [58][59][60][61], PCOS [62], diabetes [63][64], inflammation [64], Crohn’s disease [65], and single Hb molecule [66], to name a few.
2.1. Cancer Diagnosis and Theranostics
Cancer is the new pandemic and a leading cause of deaths in the modern world [67]. There is an increase in the incidence of various types of cancers, including mouth, gastric, lungs, ovaries, skin, and blood cancer. Numerous factors, such as environment, diet, lifestyle, and smoking, can trigger cancer. The early diagnosis of cancer is extremely important, as it is lifesaving with existing treatment protocols. Conventional cancer diagnosis is often performed using imaging techniques such as X-ray, computerized tomography scan (CT), positron emission tomography (PET), ultrasound, and magnetic resonance imaging (MRI). These techniques are often destructive, posing the risk of radiation ionization, and are often not compatible with patients with pre-existing conditions and medical devices such as pacemakers [68]. These are also expensive, involve sophisticated instruments, are time-consuming, and are often performed with multiple tests to avoid ambiguity [69]. Recently, there has been an increase in using plasmonic biosensing for cancer diagnosis and therapy, with review articles summarizing the progress in the same [70][71][72][73][74][75][76]. They are established to be minimally invasive, rapid, low cost, and offer point-of-care testing [77][78]. Of all plasmonic-based detection techniques, SERS is being extensively used for cancer identification, monitoring, and other theranostics, including imaging and chemo/photothermal therapy [79][80][81][82][83][84][85][86]. SERS facilitates liquid biopsy [86] by using urine, saliva, and serum, thus making it low cost and enabling easier frequent sampling compared to the existing tissue-biopsy techniques, which are often destructive [87]. Different cancer biomarkers, such as miRNA [88][89], proteins, exosomes [90][91], circulating tumor DNA (ctDNA), genes [92], peptides [93], and blood plasma [94], are studied using SERS for disease identification. SERS tags that specifically bind to the targets under study are widely used for analyzing cancer samples [95][96][97][98][99]. Machine learning algorithms are used to analyze complex patterns and recognize buried signals overcoming noise from undesirable constituents of cells and other bio-fluids.
2.2. SARS-CoV-2 and Other Respiratory Diseases
With the onset of the pandemic and the fast-spreading variants, there was a need to rapidly identify, detect, and quarantine the infected population. Surveying the presence of antibodies in large populations, often called a serological survey, was important to access the percentage of population infected and to monitor community transmission [100]. The dominant existing technique for the identification of SARS-CoV was PCR, which relies on analyzing the genetic material of the virus [101]. However, the test is expensive, thus preventing wide usage and also is time consuming. The Raman spectrum of a whole organism, including viruses, is contributed to by the proteins, carbohydrates, and nucleic acids that make up the organism [102]. The expression of these building blocks is controlled by the genetic material of the organism, hence helping in the unique identification [103]. SERS has enabled trace, point-of-care (POC), sample-collection-friendly, rapid, flexible, and cost-effective covid detection alternatives with the use of diverse nanomaterials [10][104][105][106]. In addition, both portable and handheld systems have indeed enabled point-of-care testing based on Raman spectroscopy [107][108]. SERS has also been widely used for the detection of other respiratory zoonotic diseases, such as H1N1, H7N9, H3N2, and H5N1; and other coronaviruses, such as MERS-CoV [109][110]. Often, machine learning algorithms are used in combination to enable the identification of patterns that are not apparent to the human eye [111][112]. The availability of large data and the ease of collection have accelerated the potential of machine learning algorithms in identifying viruses and their variants with reliable accuracies for POC devices [113][114]. In addition to trace identification, SERS has also enabled quantification of viral load to access the severity of the infection [115][116].
SERS in combination with LDA has been used for the rapid (2 min) identification of respiratory viruses, including SARS-CoV-2, human adenovirus type 7, and H1N1, using label-free silver nanoparticles [117]. Fe3O4@Ag nanoparticles tagged with specific antibodies were used for the detection of adenovirus and influenza virus [118]. Eleven different respiratory pathogens were identified using SERS, with nanoparticles tagged with nucleic acids achieving remarkable LODs in the sub-picomolar range [119]. Gold nanoparticles functionalized with a specific enzyme were used for the detection of S protein expressed by the COVID-19 viruses with SERS-based sensing in water [120]. Trace S protein detection has also been performed with SERS substrates enabling both chemical and electromagnetic enhancement [121] and using DNA-aptamer-based substrates, achieving a 0.7 fg mL−1 LOD [122]. Influenza-infected cells were identified based on proteins, using SERS and PCA [123]. Influenza and covid viruses were detected in human nasal fluid and saliva, using SERS [124], and also in untreated saliva [125]. A portable breath analyzer for covid detection based on the presence of organic volatile compounds was developed, achieving a sensitivity greater than 95% with less than 5 min of detection time [53]. A lateral-flow-immunoassay-based SERS was proposed for the quantitative detection of SARS-CoV-2 [126]. Similar work was performed for the trace detection of SARS-CoV-2 antibodies and spike proteins [127][128][129]. Li et al. optimized the silver nanostructures to increase the LOD for SARS-CoV-2 detection [130]. In a unique study, Kim et al. studied the efficacy of the Oxford–AstraZeneca vaccine by using SERS studies on tear samples and achieved excellent reproducibility and LOD in the femtomolar regime [131]. Machine learning algorithms such as PCA and SVM were used for the classification of normal and SARS-CoV-2 saliva samples with SERS data, with an accuracy of 95% [132]. Different respiratory viruses and their variants were identified using a silver-nanorods-based SERS sensor [133]. Different respiratory syncytial viruses have been identified and classified using SERS and classification algorithms such as PCA and HCA [134]. A deep-learning-based on-site SERS detection was developed to detect the SARS-CoV-2 virus based on the spike protein with 87% accuracy. This work also studied Raman modes of the spike protein theoretically and established a database [135]. Different variants of the SARS-CoV-2 virus, including wild-type, Alpha, Delta, and Omicron, were successfully identified using specific antibody-tagged 3D porous Ag-based SERS substrates [136]. SERS has also shown the potential of simultaneous detection of influenza virus (H1N1), SARS-CoV-2, and respiratory syncytial virus by using magnetic-tags-based SERS substrates with extended studies in throat swabs [137]. Label-free SERS was performed on serum samples of patients after 4 to 16 days of testing positive for COVID-19, and chemometric techniques were used to find significant difference in the SERS spectral features [138].
3. SERS-Based Detection of Microorganisms
3.1. Bacteria Sensing
A bacterium is a living cell and falls under the class of prokaryotic microorganisms. Bacteria come in different shapes, including spheres, rods, spiral, and comma, and have a typical size of few micrometers [139]. Bacterial cells are omnipresent, as they are found in water, food, soil, air, and the human body, and, interestingly, the human body contains 10 times more bacterial cells than human cells. However, only 3% of the bacteria are pathogenic, while the other 97% are essential for the survival of different life forms on the earth [140]. The identification of bacteria is important to assess the quality and contamination of food, soil, and water as a measure of public health. In some cases, the presence of bacteria is also desirable to ensure the decomposition of undesirable contaminants through a process called bioremediation [141][142][143]. Conventionally, PCR, plate culture, and flow cytometry are used for the detection of bacteria. However, all of them are time-consuming and need 2 to 3 days to arrive at conclusions [144]. SERS-based sensing for bacteria is extensively used for its proven advantages of being specific, sensitive [145][146][147], rapid [148], and water compatible to perform in situ measurements [149], as well as having the ability to quantify [150][151][152] and potential for trace detection [153][154][155][156][157][158]. Point-of-care devices for detection of bacteria can also be realized through SERS [159][160]. The sensitivity of SERS even enabled the detection of the single bacterium [160]. It is even possible to distinguish between live and dead bacteria cells by using SERS [161]. With the use of appropriate machine learning techniques, researchers achieved strain-level distinction using SERS spectra [162].
A SERS biosensor using aptamer (aptamer–Fe3O4@Au) and antibiotic (Vancomycin–Au@MBA) molecules has been used for the detection and quantification of pathogenic bacteria achieving a LOD of 3 cells/mL [163]. Vancomycin tagged NPs were also used in fabricating a sandwich such as SERS substrate for identification and photothermal elimination of bacteria in blood samples [164]. Different bacteria species such as S. typhi, E. coli, and L. mono were identified using SERS with Fe3O4@Au magnetic nanoparticles and demonstrated good accuracy in real world samples such as beef, saliva, and urine [165]. Wang et al. have also used magnetic nanoparticles for the detection of S. aureus [166][167]. Inspired by polyphenolic chemistry, SERS substrates with metal phenolic networks were designed for the detection of E. coli and S. aureus [168]. In addition to E. coli detection, antibiotic susceptibility was studied using core–shell Au@Ag nanorods. This study was also extended to mice blood, implying practical usage [169]. Bacteria present in serum and human blood sampl was identified using SERS based sensing [170][171]. Polymer mats prepared by force spinning were used for the detection of S. aureus, P. aeruginosa, and S. Typhimurium in blood plasma [172]. Using external magnetic field and plasmonic magnetic nanoparticles, the sensitive detection of Gram-negative bacteria was performed by concentrating the sample to a small area [173]. Similar work was accomplished using a microfluidic device to analyze drinking water for bacterial contamination [174]. The quantification of Salmonella typhimurium was performed using 3D DNA-based SERS substrates [175]. SERS-based immunoassay was used for the ultrasensitive and quantitative detection of different bacteria species simultaneously [176]. Multiplexing was also demonstrated by Hayleigh et al. [177] and Gracie et al., who then went on to conduct quantification in multiplexing [178]. A ceramic-filter-based SERS substrate, along with metal nanoparticles, was used for the detection of E. coli and Shewanella putrefaciens [179]. Nine different species of E. coli were studied using a SERS microfluidic device and discriminated with 92% accuracy, using support vector machine analysis [180]. The label-free and portable detection of various foodborne bacteria was studied using SERS and different chemometric techniques, e.g., PCA and PLS-DA [181]. Silver nanoparticles synthesized using leaf extract were used for the detection of two bacteria species [182]. SERS, in combination with deep learning techniques, was used for the accurate identification of Staphylococcus aureus to achieve an accuracy of ~98% [183].
3.2. Sensing of Biohazardous Molecules for Homeland Security
Bioterrorism is the new threat facing the world and is equally potent to cause large-scale destruction of civil, animal, and plant life. Often, biological agents are easy to prepare and scale up; can be contaminated in food, water, and soil; and are easy to carry, making them the future weapons. Many countries keep them in their military stockpiles despite the regulations [184]. According to the Centre for Disease Control and Prevention (CDC), a biohazardous material is defined as any infectious agent or biological material that poses a threat to human health, the environment, and animals. A review by Lister et al. summarized different biological agents that concern homeland security [185]. Different pathogens and biological agents, such as toxins, venom, and allergens, are some examples of biohazardous materials. Nerve agents are a big concern owing to their high solubility, high toxicity, and durability, with the Tokyo event in 1995 being an example [186][187]. Nerve agents can be classified into G-series, representing agents developed by Germans; V-series for venomous agents; GV series for the combination of G- and V-series; and Novichock series [188]. It is imperative to have a detection system that is sensitive, rapid, portable, and functional for different background media, such as liquids and gases, for the detection of these nerve agents. Plasmonic sensors are widely used for the detection of chemical and biological war threats [189][190]. Of all, SERS has its own advantages for the reasons discussed in the Introduction section and hence is widely used for the detection of biological threats, with a potential for field applications using portable devices [191] and chemometrics [192].
A sensitive and selective identification of the nerve agents Tabun, Cyclosarin, and VX was performed using gold- and silver-coated Si nanostructures both without [193] and with a tag (antidote) [194] in two different studies. VX and its hydrolysis products were studied elsewhere, too [195][196]. Sarin, an organophosphorus nerve agent, was detected using plasmonic Si nanocone structures [197]. Three nerve agents, i.e., isopropyl methylphosphonofluoridate (GB), pinacolyl methylphosphonofluoridate (GD), and cyclohexyl methylphosphonofluoridate (GF), were identified, and their hydrolysis degradation was distinguished using SERS [187]. A mustard simulant, pathogenic bacteria, and cyanide were detected using SERS [198]. A reproducible (7%), rapid (30 s), and sensitive (1 ppb) was used for the detection of a nerve simulant, pinacolyl methyl phosphonic acid (PMPA) [199]. Gaseous warfare agents such as dimethyl methylphosphonate were identified using SERS on LiCl microlenses [200]. Various G-series and VX nerve agents were identified using novel pinhole shell-isolated Au nanoparticles substrates achieving sensitivity of 10 ng/L and 20 ng/L, respectively [201]. Using plasmonic 3D fractal structures, a G-series nerve agent called dimethyl methylphosphonate (DMMP) was detected in the gaseous state, with a sensitivity of 12 ppmV [202]. Bacillus anthracis is a highly infectious bacteria that causes the fatal disease anthrax in humans. It is a cause for concern because of its recent usage as a biowarfare agent by many countries [203]. Farrell et al. summarized different anthrax biomarkers and existing detection techniques [204]. Plasmonic metal decorated anisotropic Ni nanostructures were used for detection of dipicolinic acid (DPA), a biomarker for anthrax [205]. Specifically, tagged SERS substrates were used for the detection of anthrax protective antigens, achieving a remarkable LOD of 1 pg/mL [206]. A magnetic microfluidic SERS sensor using specifically tagged Au nanoparticles was used for the detection of the anthrax biomarker poly-γ-D-glutamic acid, with an LOD of 100 pg/mL [207]. Reusable and sensitive laser-ablated Au nanostructures were used for the detection of dipicolinic acid (DPA) with a LOD of 0.83 pg/L and signal enhancement of ~1012 [208]. A selective SERS substrate that can discriminate between different strains of bacteria by specifically binding to Bacillus anthracis was designed with DPA as a biomarker [209]. Gold nanorods were also employed for the sensitive detection of DPA and anthrax-protective antigen [210][211]. The trace detection of DPA, equivalent to nearly 18 spores, was achieved using super-hydrophobic SERS sensors [212]. The effects of aggregation of NPs and pH on the SERS performance for the detection of components of cell wall and endospores of Bacillus thuringiensis were studied extensively [213]. Different chemical and biological warfare agents were classified using techniques such as PCA, PLS-DA, as well as hierarchical classification techniques based on the SERS spectra [193][214].
4. Machine Learning in SERS-Based Biosensing
4.1. Introduction to Machine Learning
In recent times, machine learning is widely being used for many applications including spectroscopy for both data pre- and postprocessing. Machine learning (ML), as the name suggests, is a technique in which the algorithm learns patterns from the existing data and will attempt to make accurate predictions on the unknown based on the trained data. The potential for its ability to find complex patterns from big data sets has given an opportunity to extract and model data purposefully. There are different existing algorithms, both supervised and unsupervised, depending on the problem at hand. Deep learning is a subdomain of machine learning inspired by the human brain that uses multilayered neural networks for modeling data. Throughout this article, machine learning also implies deep learning techniques. Advances in computation facilities and with increasing availability and complexity of big data, deep learning, which is a kind of machine learning, has found its place. Some popular and relevant examples of ML being classification of emails as span and not span, identifying cancer in early stage using medical images, face recognition and weather prediction. ML algorithms can be broadly classified into three types, namely supervised for labeled observations, unsupervised for unlabeled observations, and reinforcement learning for models that learn from the errors to improve accuracy [215], as summarized in the Figure 2 below.
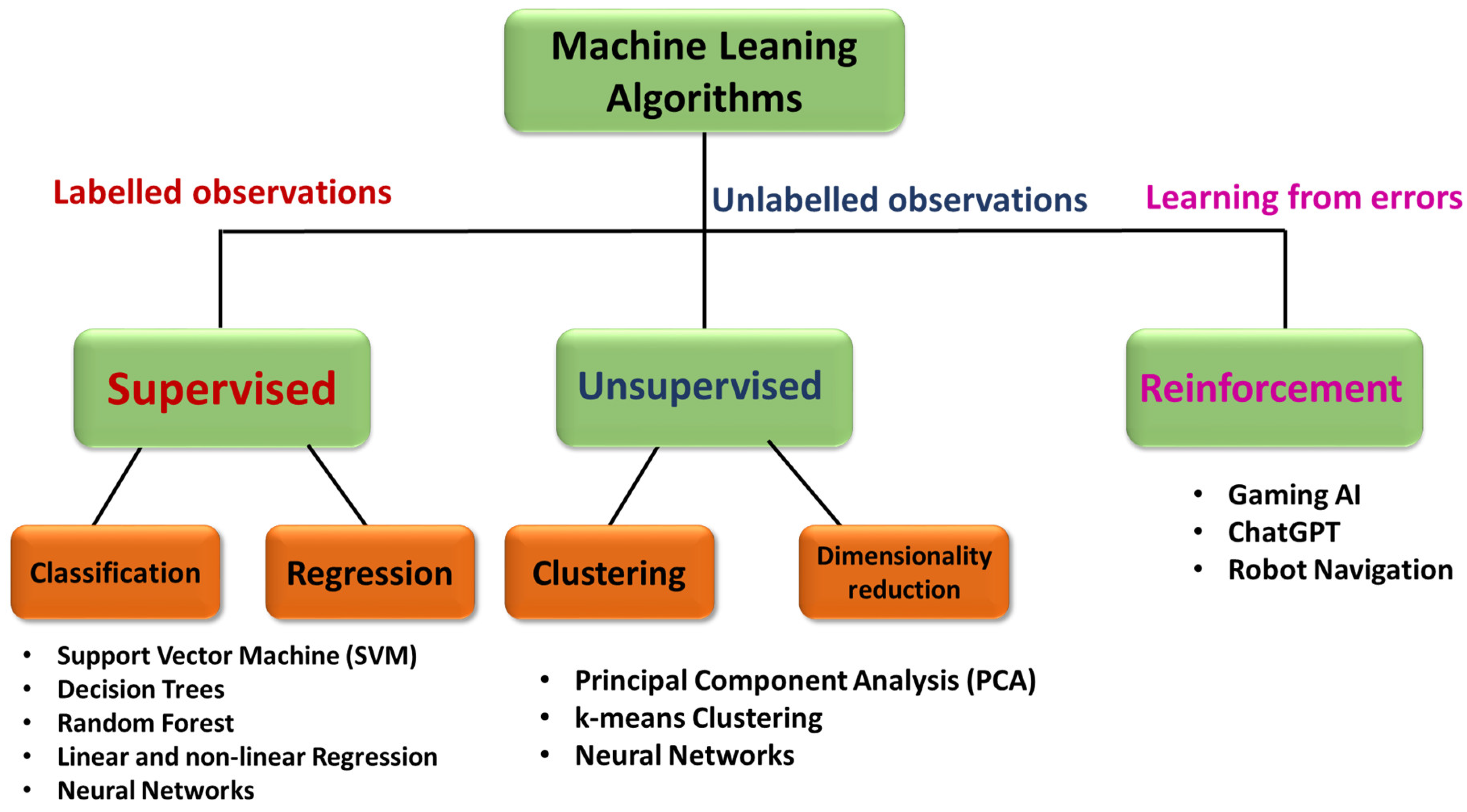
Figure 2. Flow chart illustrating the classification of different machine learning algorithms as supervised, unsupervised, and reinforcement models.
With the ease of data collection and availability of open source Raman spectroscopy data, SERS has also seen a surge in machine learning models [49][216][217]. The trend is welcoming and desirable as the nature of existing challenges in SERS involving trace detection, signal fluctuations, quantification and identification are complex with many variables calling for an analytical tool that has the ability to capture the patterns devoid of experts [218]. Trace detection implies identifying signal from a noisy background where ML could be aided. SERS is also known to have inherent signal fluctuations owing to localization of hotspots. Especially in the case of bio samples, they have background contribution from different undesirable components thus interfering with the signal and need ML algorithms to extract the useful information [2][219][220][221][222]. The process of data collection, identification of chemical composition and quantification is non-linear and is highly dependent on human intelligence making it a barrier to carry the benefits of SERS to onsite [223]. Some of the widely used techniques include Principal Component Analysis (PCA), Support Vector Machine (SVM), Partial Least Squares (PLS), Decision Trees (DTs) and Convolutional Neural Networks (CNNs). PCA is a dimensionality reduction technique where components representative of the data with large variance are preserved. This is extensively used a preprocessing step in order to reduce complexity of the models or also as a classification technique [224][225][226]. SVM is a nonlinear ML technique that can be used for both regression and classification [225]. It works by finding a hyperplane that distinguishes two or more classes using a kernel function [227]. If the data set is small and the number of variables is large, PLS is useful for its ability to still extract useful information and is often used for quantitative studies [228][229]. DTs are widely used for classification of the data using a method bootstrapping [230]. CNNs are a kind of neural networks which employ filters and pooled layers in the architecture and often used if the size of the data set is large enough and if images are involved in the modeling [231]. Specifically, in the field of biophotonics, machine learning models using SERS can be efficiently classified into three domains: identification, classification, and quantification, with interests such as disease and molecular diagnosis [232][233]; microorganism classification, identification, etc. [234][235][236][237]; and cancer diagnosis [238], as shown in Figure 3. In addition, machine learning was also used to improve data collection to overcome signal fluctuations and enhance the usability on site [239], to estimate the effect of scattering [240] and for the SERS signal enhancement itself [241].
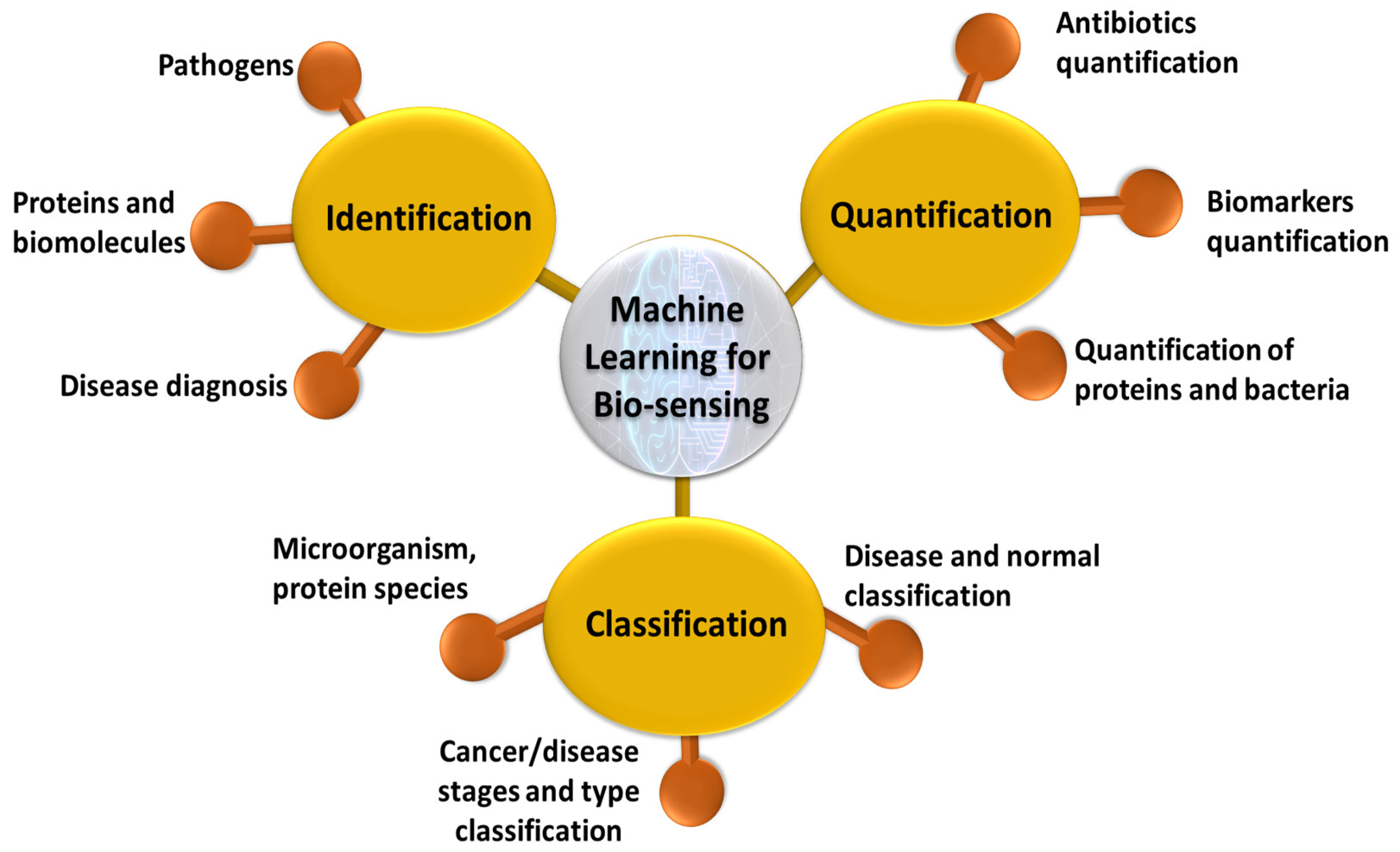
Figure 3. Schematic of applications of machine learning for biosensing using SERS based plasmonic sensors.
4.2. Identification
SERS provides the vibrational fingerprint of many biomolecules, including amino acids, peptides, carbohydrates, pathogens, and nuclei acids [242]. It is also label free and non-destructive, making it desirable for in situ and rapid identification. Often in real-world situations of biology sample analysis, there are undesirable effects from background cell signals or with the similarity of spectra from two subspecies. Machine learning models can be successfully trained to capture these complex differences and distinguish two similar spectra devoid of the background helping in identification of the sample. CNNs were used for identification of cancer using SERS with gold multi-branched nanoparticles (AuMs), functionalized with different chemical groups, and achieved 100% accuracy in identifying the structural changes [243]. Drug-sensitive and drug-resistant bacterial strains were identified using SERS with a combination of CNNs and achieved 100% accuracy [244]. Different classification algorithms such as LDA, SVM, and KNN were used for the classification of bacterial extracellular vesicles for E. coli by strain and culture time using label-free approach of SERS [245]. SVM was successfully used for the identification of different drugs in human urine at trace levels with an accuracy greater than 92% [246]. A SERS chip was designed to identify a cancer marker, TIMP-1, and combined it with ML to identify lung and colon cancer in patients [247]. A label-free SERS, in combination with different machine learning algorithms, such as random forest, PCA-LDA, and decision trees, was used for the identification of colon cancer using serum samples. It was found that the random forest model outperformed the other two models in terms of accuracy and specificity [248]. SERS combined with ANN was used for the identification of different pollen samples despite many spectral contributions using Au NPs [249]. A microfluidic-chip-based SERS substrate with Au nanoparticles was used for the identification of l Jurkat, THP-1, and MONO-MAC-6 leukemia cell lysates, using SVM, and achieved 99% accuracy [250]. A lab-on-chip SERS device was fabricated and used for the successful identification of different species of mycobacteria [251]. The machine learning models PLS-DA and CNN were used to identify different stages of kidney malfunction in dialysis patients by using serum analysis by SERS. The CNN model achieved an accuracy of 96%, which is better than that of PLS-DA, with 84% [252]. The SVM outperformed other techniques in the identification of cyanobacteria, using SERS spectra of mutant and wild-type strains [253]. Using a dimensionality reduction technique, followed by a probabilistic ML model, SARS-CoV-2 identification was performed with an accuracy of ~85% [254]. SERS coupled with SVM was also used for the identification of lung cancers [86].
4.3. Quantification
One of the interests of using SERS for sensing also lies in its ability to detect trace and ultra-trace molecules. The intensity and concentration relation for a peak of choice in the SERS spectrum is often non-linear due to many factors, such as the inhomogeneous distribution of hotspots, non-uniform adsorption of molecules, and localization of the hotspots [226][255]. This calls for machine learning models that have the ability to capture non-linear patterns of intensity and concentration relation and further predict the unknown concentration. As the problem demands, regression ML models such as PCR, PLSR, SVR, and XGBR are used for the quantification of trace biomolecules.
A quantitative analysis of antibiotics and a mixture of antibiotics was performed using PLSR with an accuracy of 96% [256]. An SERS-based lateral flow assay was used for the quantification of E. coli in milk and beef, using the Bayesian ridge regression (BRR), support vector regression (SVR), elastic net regression (ENR), and extreme gradient boosting regression (XGBR) algorithm [257]. A SERS substrate with plasmonic nanogaps was fabricated and used for the trace sensing of pyocyanin, a secondary metabolite of Pseudomonas aeruginosa, from a complex background. Furthermore, using machine learning algorithms, the quantification of pyocyanin was performed with an accuracy until five significant digits, using PLS [258]. The quantification of very low concentrations of fumonicins in maize was performed using different chemometric techniques such as PCR and PLSR and achieved an accuracy above 90% [259]. Thiols found in the whole blood of umbilical cords were quantified using a PLSR model on SERS spectra collected using silver nanoparticles as plasmonic substrates [260]. PCA, followed by SVR, was used for the quantification of histamine, an allergen, in seafood, using spectral data from a combination of TLS and SERS [261].
4.4. Classification
The goal of the classification algorithms employed for data analysis in SERS for biosensing is often differentiating different classes, species, and spectra corresponding to different stages of the disease or different diseases themselves. So far, classification algorithms such as SVM, KNN, and PCA; and different neural networks, such as CNN, were used for the problems stated.
Different bacteria species were classified and identified using SVM, with an accuracy of 87% by using SERS with bacterial cellulose nanocrystals (BCNCs) decorated with Au nanoparticles [262]. K-nearest neighbor and decision trees were used for the classification of SERS-based liquid biopsy assay to identify five protein biomarkers (CA19-9, HE4, MUC4, MMP7, and mesothelin) in pancreatic cancer patients, ovarian cancer patients, pancreatitis patients, and healthy individuals [263]. The direct serum analysis of liver cancer samples is performed using Au-Ag nano complex-decorated ZnO nanopillars on paper for the classification of different stages of cancer using CNNs. This method achieved an accuracy of 97.78% [264]. SERS combined with machine learning was also used for the screening of PCOS, using classification algorithms on SERS data. Samples of follicular fluids and plasma from healthy and PCOS patients were successfully classified, with an accuracy of 89%, using stacked models for both [265]. Protein species with similar spectral profiles were classified using principal component analysis (PCA) applied to SERS spectra [266]. CNNs without any preprocessing steps were used for the classification of different grades of bladder cancer tissue, using Raman spectra, and different species of E. coli, using SERS spectra. Different classification algorithms, such as KNN, PCA, SVM, and ANN, were used, but CNN was found to outperform the others in terms of accuracy [267]. Using Non-Structural Protein 1 (NS1) as a biomarker for dengue, extreme learning machine and PCA models were used for the classification of dengue patients with 100% accuracy towards a goal of early diagnosis [268]. Bacterial endotoxins of twelve different species were identified and classified using SERS spectra and machine learning algorithms such as KNN, RF, SVM, and RamanNet. While the other algorithms achieved accuracy greater than 90%, RamanNet outperformed them, with 100% accuracy [269]. With a goal to identify cancer at an early stage, a point-of-care diagnosis system using a novel hydrophobic SERS substrate combined with machine learning techniques was used [50]. The SERS spectra of serum samples collected from nearly 690 patients, including normal and different cancers (breast cancer, leukemia, and hepatitis B virus), were collected and analyzed using deep learning techniques to achieve 100% accuracy in successfully classifying the data. They performed external testing with an accuracy of 98%, indicating potential usage in the real world.
References
- Stewart, M.E.; Anderton, C.R.; Thompson, L.B.; Maria, J.; Gray, S.K.; Rogers, J.A.; Nuzzo, R.G. Nanostructured Plasmonic Sensors. Chem. Rev. 2008, 108, 494–521.
- Costanzo, H.; Gooch, J.; Frascione, N. Nanomaterials for Optical Biosensors in Forensic Analysis. Talanta 2023, 253, 123945.
- Chen, G.; Chen, Y.; Huang, W.; Shi, Y. Plasmonic Nanobiosensors for Detection of Different Targets. In Proceedings of the Second International Conference on Medical Imaging and Additive Manufacturing (ICMIAM 2022), Xiamen, China, 25–27 February 2022.
- Sadani, K.; Nag, P.; Thian, X.Y.; Mukherji, S. Enzymatic Optical Biosensors for Healthcare Applications. Biosens. Bioelectron. X 2022, 12, 100278.
- Erkmen, C.; Selcuk, O.; Unal, D.N.; Kurbanoglu, S.; Uslu, B. Layer-by-Layer Modification Strategies for Electrochemical Detection of Biomarkers. Biosens. Bioelectron. X 2022, 12, 100270.
- Spillman, W.B. Fiber Optic Biosensors; Elsevier: Amsterdam, The Netherlands, 2011; Volume 3, ISBN 9780470126844.
- Kazanskiy, N.L.; Khonina, S.N.; Butt, M.A.; Kaźmierczak, A.; Piramidowicz, R. State-of-the-Art Optical Devices for Biomedical Sensing Applications—A Review. Electronics 2021, 10, 973.
- Ramirez, J.C.; Grajales García, D.; Maldonado, J.; Fernández-Gavela, A. Current Trends in Photonic Biosensors: Advances towards Multiplexed Integration. Chemosensors 2022, 10, 398.
- Chadha, U.; Bhardwaj, P.; Agarwal, R.; Rawat, P.; Agarwal, R.; Gupta, I.; Panjwani, M.; Singh, S.; Ahuja, C.; Selvaraj, S.K.; et al. Recent Progress and Growth in Biosensors Technology: A Critical Review. J. Ind. Eng. Chem. 2022, 109, 21–51.
- Dutta, G. Next-Generation Nanobiosensor Devices for Point-of-Care Diagnostics; Springer: Singapore, 2023; ISBN 9789811971303.
- Ahangari, A.; Mahmoodi, P.; Mohammadzadeh, A. Advanced Nano Biosensors for Rapid Detection of Zoonotic Bacteria. Biotechnol. Bioeng. 2022, 120, 41–56.
- Taha, B.A.; Al Mashhadany, Y.; Bachok, N.N.; Ashrif, A.; Bakar, A.; Hafiz Mokhtar, M.H.; Dzulkefly Bin Zan, M.S.; Arsad, N. Detection of COVID-19 Virus on Surfaces Using Photonics: Challenges and Perspectives. Diagnostics 2021, 11, 1119.
- Soma, V.R.; Podagatlapalli, G.K.; Hamad, S.; Mechanics, F. Ultrafast Laser Ablation in Liquids for Nanomaterials and Applications. J. Nanosci. Nanotechnol. 2014, 14, 1364–1388.
- Soler, M.; Lechuga, L.M. Principles, Technologies, and Applications of Plasmonic Biosensors. J. Appl. Phys. 2021, 129, 111102.
- Barbillon, G. Plasmonics and Its Applications. Materials 2019, 12, 1502.
- Michaels, A.M.; Jiang, J.; Brus, L. Ag Nanocrystal Junctions as the Site for Surface-Enhanced Raman Scattering of Single Rhodamine 6G Molecules. J. Phys. Chem. B 2000, 104, 11965–11971.
- Golightly, R.S.; Doering, W.E.; Natan, M.J. Surface-Enhanced Raman Spectroscopy and Homeland Security: A Perfect Match? ACS Nano 2009, 3, 2859–2869.
- Vendamani, V.S.; Beeram, R.; Nageswara Rao, S.V.S.; Pathak, A.P.; Soma, V.R. Trace Level Detection of Explosives and Pesticides Using Robust, Low-Cost, Free-Standing Silver Nanoparticles Decorated Porous Silicon. Opt. Express 2021, 29, 30045.
- Liu, C.; Xu, D.; Dong, X.; Huang, Q. A Review: Research Progress of SERS-Based Sensors for Agricultural Applications. Trends Food Sci. Technol. 2022, 128, 90–101.
- Zhang, D.; Pu, H.; Huang, L.; Sun, D.W. Advances in Flexible Surface-Enhanced Raman Scattering (SERS) Substrates for Nondestructive Food Detection: Fundamentals and Recent Applications. Trends Food Sci. Technol. 2021, 109, 690–701.
- Li, Y.; Liu, X.; Lin, Z. Recent Developments and Applications of Surface Plasmon Resonance Biosensors for the Detection of Mycotoxins in Foodstuffs. Food Chem. 2012, 132, 1549–1554.
- Dies, H.; Raveendran, J.; Escobedo, C.; Docoslis, A. Rapid Identification and Quantification of Illicit Drugs on Nanodendritic Surface-Enhanced Raman Scattering Substrates. Sens. Actuators B Chem. 2018, 257, 382–388.
- Vendamani, V.S.; Beeram, R.; Rao, S.V.S.N.; Rao, S.V. Protocol for Designing AuNP-Capped Ag Dendrites as Surface-Enhanced Raman Scattering Sensors for Trace Molecular Detection Protocol for Designing AuNP-Capped Ag Dendrites as Surface-Enhanced Raman Scattering Sensors for Trace Molecular Detection. STAR Protoc. 2023, 4, 102068.
- He, L.; Rodda, T.; Haynes, C.L.; Deschaines, T.; Strother, T.; Diez-Gonzalez, F.; Labuza, T.P. Detection of a Foreign Protein in Milk Using Surface-Enhanced Raman Spectroscopy Coupled with Antibody-Modified Silver Dendrites. Anal. Chem. 2011, 83, 1510–1513.
- Jebakumari, K.A.E.; Murugasenapathi, N.K. Engineered Two-Dimensional Nanostructures as SERS Substrates for Biomolecule Sensing: A Review. Biosensors 2023, 13, 102.
- Bantz, K.C.; Meyer, A.F.; Wittenberg, N.J.; Im, H.; Kurtuluş, Ö.; Lee, S.H.; Lindquist, N.C.; Oh, S.H.; Haynes, C.L. Recent Progress in SERS Biosensing. Phys. Chem. Chem. Phys. 2011, 13, 11551–11567.
- Vendamani, V.S.; Nageswara Rao, S.V.S.; Venugopal Rao, S.; Kanjilal, D.; Pathak, A.P. Three-Dimensional Hybrid Silicon Nanostructures for Surface Enhanced Raman Spectroscopy Based Molecular Detection. J. Appl. Phys. 2018, 123, 014301.
- Huang, Z.; Zhang, A.; Zhang, Q.; Cui, D. Nanomaterial-Based SERS Sensing Technology for Biomedical Application. J. Mater. Chem. B 2019, 7, 3755–3774.
- Szaniawska, A.; Kudelski, A. Applications of Surface-Enhanced Raman Scattering in Biochemical and Medical Analysis. Front. Chem. 2021, 9, 664134.
- Chen, Y.; An, Q.; Teng, K.; Liu, C.; Sun, F.; Li, G. Application of SERS in In-Vitro Biomedical Detection. Chem. Asian J. 2022, 18, e202201194.
- Hegde, M.; Pai, P.; Gangadhar Shetty, M.; Sundara Babitha, K. Gold Nanoparticle Based Biosensors for Rapid Pathogen Detection: A Review. Environ. Nanotechnol. Monit. Manag. 2022, 18, 100756.
- Fleischmann, M.; Hendra, P.J.; McQuillan, A.J. Raman Spectra of Pyridine Adsorbed at a Silver Electrode. Chem. Phys. Lett. 1974, 26, 163–166.
- Jeanmaire, D.L.; Duyne, R.P.V.A.N. Surface Raman spectroelectrochemistry: Part I. Heterocyclic, aromatic, and aliphatic amines adsorbed on the anodized silver electrode. J. Electroanal. Chem. Interfacial Electrochem. 1977, 84, 1–20.
- Albrecht, M.G.; Creighton, J.A. Anomalously Intense Raman Spectra of Pyridine at a Silver Electrode. J. Am. Chem. Soc. 1977, 99, 5215–5217.
- Pilot, R.; Signorini, R.; Durante, C.; Orian, L.; Bhamidipati, M.; Fabris, L. A Review on Surface-Enhanced Raman Scattering. Biosensors 2019, 9, 57.
- Le Ru, E.; Etchegoin, P. Principles of Surface Enhanced Raman Spectroscopy and Related Plasmonic Effects; Elseveir: Amsterdam, The Netherlands, 2008.
- Etchegoin, P.G.; Ru, E.C.L. Basic Electromagnetic Theory of SERS. In Surface Enhanced Raman Spectroscopy: Analytical, Biophysical and Life Science Applications; John Wiley & Sons: Hoboken, NJ, USA, 2011; pp. 1–37. ISBN 9783527325672.
- Le Ru, E.C.; Blackie, E.; Meyer, M.; Etchegoint, P.G. Surface Enhanced Raman Scattering Enhancement Factors: A Comprehensive Study. J. Phys. Chem. C 2007, 111, 13794–13803.
- Sharma, B.; Frontiera, R.R.; Henry, A.I.; Ringe, E.; Van Duyne, R.P. SERS: Materials, Applications, and the Future. Mater. Today 2012, 15, 16–25.
- Li, Q.; Huo, H.; Wu, Y.; Chen, L.; Su, L.; Zhang, X.; Song, J.; Yang, H. Design and Synthesis of SERS Materials for In Vivo Molecular Imaging and Biosensing. Adv. Sci. 2023, 2023, 2202051.
- Israelsen, N.D.; Hanson, C.; Vargis, E. Nanoparticle Properties and Synthesis Effects on Surface-Enhanced Raman Scattering Enhancement Factor: An Introduction. Sci. World J. 2015, 2015, 124582.
- Wang, A.X.; Kong, X. Review of Recent Progress of Plasmonic Materials and Nano-Structures for Surface-Enhanced Raman Scattering. Materials 2015, 8, 3024–3052.
- Moram, S.S.B.; Byram, C.; Soma, V.R. Gold-Nanoparticle- and Nanostar-Loaded Paper-Based SERS Substrates for Sensing Nanogram-Level Picric Acid with a Portable Raman Spectrometer. Bull. Mater. Sci. 2020, 43, 53.
- Zhang, Z.; Guan, R.; Li, J. Engineering Rational SERS Nanotags for Parallel Detection of Multiple Cancer Circulating Biomarkers. Chemosensors. 2023, 11, 110.
- Pilot, R.; Massari, M. Silver Nanoparticle Aggregates: Wavelength Dependence of Their SERS Properties in the First Transparency Window of Biological Tissues. Chem. Phys. Impact 2021, 2, 100014.
- Zhang, Y.; Mi, X.; Tan, X.; Xiang, R. Recent Progress on Liquid Biopsy Analysis Using Surface-Enhanced Raman Spectroscopy. Theranostics 2019, 9, 491–525.
- Aitekenov, S.; Sultangaziyev, A.; Ilyas, A.; Dyussupova, A.; Boranova, A.; Gaipov, A.; Bukasov, R. Surface-Enhanced Raman Spectroscopy (SERS) for Protein Determination in Human Urine. Sens. Bio-Sens. Res. 2022, 38, 100535.
- Akgönüllü, S.; Denizli, A. Recent Advances in Optical Biosensing Approaches for Biomarkers Detection. Biosens. Bioelectron. X 2022, 12, 100269.
- Lussier, F.; Thibault, V.; Charron, B.; Wallace, G.Q.; Masson, J.F. Deep Learning and Artificial Intelligence Methods for Raman and Surface-Enhanced Raman Scattering. TrAC Trends Anal. Chem. 2020, 124, 115796.
- Lin, X.; Lin, D.; Chen, Y.; Lin, J.; Weng, S.; Song, J.; Feng, S. High Throughput Blood Analysis Based on Deep Learning Algorithm and Self-Positioning Super-Hydrophobic SERS Platform for Non-Invasive Multi-Disease Screening. Adv. Funct. Mater. 2021, 31, 2103382.
- Breuch, R.; Klein, D.; Siefke, E.; Hebel, M.; Herbert, U.; Wickleder, C.; Kaul, P. Differentiation of Meat-Related Microorganisms Using Paper-Based Surface-Enhanced Raman Spectroscopy Combined with Multivariate Statistical Analysis. Talanta 2020, 219, 121315.
- Ilkhani, H.; Hughes, T.; Li, J.; Zhong, C.J.; Hepel, M. Nanostructured SERS-Electrochemical Biosensors for Testing of Anticancer Drug Interactions with DNA. Biosens. Bioelectron. 2016, 80, 257–264.
- Leong, S.X.; Leong, Y.X.; Tan, E.X.; Sim, H.Y.F.; Koh, C.S.L.; Lee, Y.H.; Chong, C.; Ng, L.S.; Chen, J.R.T.; Pang, D.W.C.; et al. Noninvasive and Point-of-Care Surface-Enhanced Raman Scattering (SERS)-Based Breathalyzer for Mass Screening of Coronavirus Disease 2019 (COVID-19) under 5 Min. ACS Nano 2022, 16, 2629–2639.
- Bharati, M.S.S.; Soma, V.R. Flexible SERS Substrates for Hazardous Materials Detection: Recent Advances. Opto-Electron. Adv. 2021, 4, 210048.
- Ali, A.; Nettey-Oppong, E.E.; Effah, E.; Yu, C.Y.; Muhammad, R.; Soomro, T.A.; Byun, K.M.; Choi, S.H. Miniaturized Raman Instruments for SERS-Based Point-of-Care Testing on Respiratory Viruses. Biosensors 2022, 12, 590.
- Moore, T.J.; Moody, A.S.; Payne, T.D.; Sarabia, G.M.; Daniel, A.R.; Sharma, B. In Vitro and in Vivo Sers Biosensing for Disease Diagnosis. Biosensors 2018, 8, 46.
- Alvarez-Puebla, R.A.; Liz-Marzán, L.M. SERS-Based Diagnosis and Biodetection. Small 2010, 6, 604–610.
- Zhang, X.; Liu, S.; Song, X.; Wang, H.; Wang, J.; Wang, Y.; Huang, J.; Yu, J. Robust and Universal SERS Sensing Platform for Multiplexed Detection of Alzheimer’s Disease Core Biomarkers Using PAapt-AuNPs Conjugates. ACS Sens. 2019, 4, 2140–2149.
- Park, H.J.; Cho, S.; Kim, M.; Jung, Y.S. Carboxylic Acid-Functionalized, Graphitic Layer-Coated Three-Dimensional SERS Substrate for Label-Free Analysis of Alzheimer’s Disease Biomarkers. Nano Lett. 2020, 20, 2576–2584.
- Dang, H.; Joung, Y.; Jeong, C.; Jeon, C.S.; Pyun, S.H.; Park, S.-G.; Choo, J. Nanoplasmonic Assay Platforms for Reproducible SERS Detection of Alzheimer’s Disease Biomarker. Bull. Korean Chem. Soc. 2023, 2023, 1.
- Momenpour, A.; Lima, P.D.A.; Chen, Y.-A.; Tzeng, C.-R.; Tsang, B.K.; Anis, H. Surface-Enhanced Raman Scattering for the Detection of Polycystic Ovary Syndrome. Biomed. Opt. Express 2018, 9, 801.
- Lyandres, O.; Shah, N.C.; Yonzon, C.R.; Walsh, J.T.; Glucksberg, M.R.; Van Duyne, R.P. Real-Time Glucose Sensing by Surface-Enhanced Raman Spectroscopy in Bovine Plasma Facilitated by a Mixed Decanethiol/Mercaptohexanol Partition Layer. Anal. Chem. 2005, 77, 6134–6139.
- Qi, G.; Jia, K.; Fu, C.; Xu, S.; Xu, W. A Highly Sensitive SERS Sensor for Quantitative Analysis of Glucose Based on the Chemical Etching of Silver Nanoparticles. J. Opt. 2015, 17, 114020.
- Rong, Z.; Xiao, R.; Xing, S.; Xiong, G.; Yu, Z.; Wang, L.; Jia, X.; Wang, K.; Cong, Y.; Wang, S. SERS-Based Lateral Flow Assay for Quantitative Detection of C-Reactive Protein as an Early Bio-Indicator of a Radiation-Induced Inflammatory Response in Nonhuman Primates. Analyst 2018, 143, 2115–2121.
- Li, B.; Wu, Y.; Wang, Z.; Xing, M.; Xu, W.; Zhu, Y.; Du, P.; Wang, X.; Yang, H. Non-Invasive Diagnosis of Crohn’s Disease Based on SERS Combined with PCA-SVM. Anal. Methods 2021, 13, 5264–5273.
- Xu, H.; Bjerneld, E.J.; Käll, M.; Börjesson, L. Spectroscopy of Single Hemoglobin Molecules by Surface Enhanced Raman Scattering. Phys. Rev. Lett. 1999, 83, 4357–4360.
- World Health Organization Report. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 30 January 2023).
- Blanco-Formoso, M.; Alvarez-Puebla, R.A. Cancer Diagnosis through Sers and Other Related Techniques. Int. J. Mol. Sci. 2020, 21, 2253.
- Guerrini, L.; Pazos-Perez, N.; Garcia-Rico, E.; Alvarez-Puebla, R. Cancer Characterization and Diagnosis with SERS-Encoded Particles. Cancer Nanotechnol. 2017, 8, 5.
- Kaur, B.; Kumar, S.; Kaushik, B.K. Recent Advancements in Optical Biosensors for Cancer Detection. Biosens. Bioelectron. 2022, 197, 113805.
- Thenrajan, T.; Wilson, J. Biosensors for Cancer Theranostics. Biosens. Bioelectron. X 2022, 12, 100232.
- Falkowski, P.; Lukaszewski, Z.; Gorodkiewicz, E. Potential of Surface Plasmon Resonance Biosensors in Cancer Detection. J. Pharm. Biomed. Anal. 2021, 194, 113802.
- Fu, Q.; Zhang, X.; Song, J.; Yang, H. Plasmonic Gold Nanoagents for Cancer Imaging and Therapy. View 2021, 2, 20200149.
- Azzouz, A.; Hejji, L.; Kim, K.H.; Kukkar, D.; Souhail, B.; Bhardwaj, N.; Brown, R.J.C.; Zhang, W. Advances in Surface Plasmon Resonance–Based Biosensor Technologies for Cancer Biomarker Detection. Biosens. Bioelectron. 2022, 197, 113767.
- Sugumaran, S.; Jamlos, M.F.; Ahmad, M.N.; Bellan, C.S.; Schreurs, D. Nanostructured Materials with Plasmonic Nanobiosensors for Early Cancer Detection: A Past and Future Prospect. Biosens. Bioelectron. 2018, 100, 361–373.
- Fattahi, Z.; Khosroushahi, A.Y.; Hasanzadeh, M. Recent Progress on Developing of Plasmon Biosensing of Tumor Biomarkers: Efficient Method towards Early Stage Recognition of Cancer. Biomed. Pharmacother. 2020, 132, 110850.
- Bellassai, N.; D’Agata, R.; Jungbluth, V.; Spoto, G. Surface Plasmon Resonance for Biomarker Detection: Advances in Non-Invasive Cancer Diagnosis. Front. Chem. 2019, 7, 570.
- Usman, F.; Dennis, J.O.; Aljameel, A.I.; Ali, M.K.M.; Aldaghri, O.; Ibnaouf, K.H.; Zango, Z.U.; Beygisangchin, M.; Alsadig, A.; Meriaudeau, F. Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review. Chemosensors 2021, 9, 326.
- Yin, B.; Ho, W.K.H.; Xia, X.; Chan, C.K.W.; Zhang, Q.; Ng, Y.M.; Lam, C.Y.K.; Cheung, J.C.W.; Wang, J.; Yang, M.; et al. A Multilayered Mesoporous Gold Nanoarchitecture for Ultraeffective Near-Infrared Light-Controlled Chemo/Photothermal Therapy for Cancer Guided by SERS Imaging. Small 2023, 2023, 2206762.
- Constantinou, M.; Hadjigeorgiou, K.; Abalde-cela, S.; Andreou, C. Label-Free Sensing with Metal Nanostructure-Based Surface- Enhanced Raman Spectroscopy for Cancer Diagnosis. ACS Appl. Nano Mater. 2022, 5, 12276–12299.
- Rajput, S.; Pink, D.; Findlay, S.; Woolner, E.; Lewis, J.D.; McDermott, M.T. Application of Surface-Enhanced Raman Spectroscopy to Guide Therapy for Advanced Prostate Cancer Patients. ACS Sens. 2022, 7, 827–838.
- Avci, E.; Yilmaz, H.; Sahiner, N.; Tuna, B.G.; Cicekdal, M.B.; Eser, M.; Basak, K.; Altıntoprak, F.; Zengin, I.; Dogan, S.; et al. Label-Free Surface Enhanced Raman Spectroscopy for Cancer Detection. Cancers 2022, 14, 5021.
- Guerrini, L.; Alvarez-puebla, R.A. Surface-Enhanced Raman Spectroscopy in Cancer Diagnosis, Prognosis and Monitoring. Cancers 2019, 11, 748.
- Pollap, A.; Paweł, S. Recent Advances in Sandwich SERS Immunosensors for Cancer Detection. Int. J. Mol. Sci. 2022, 23, 4740.
- Vendrell, M.; Maiti, K.K.; Dhaliwal, K.; Chang, Y.T. Surface-Enhanced Raman Scattering in Cancer Detection and Imaging. Trends Biotechnol. 2013, 31, 249–257.
- Moisoiu, V.; Iancu, S.D.; Stefancu, A.; Moisoiu, T.; Pardini, B.; Dragomir, M.P.; Crisan, N.; Avram, L.; Crisan, D.; Andras, I.; et al. SERS Liquid Biopsy: An Emerging Tool for Medical Diagnosis. Colloids Surfaces B Biointerfaces 2021, 208, 112064.
- Shanmugasundaram, K.B.; Li, J.; Sina, A.I.; Wuethrich, A.; Trau, M. Toward Precision Oncology: SERS Microfluidic Systems for Multiplex Biomarker Analysis in Liquid Biopsy. Mater. Adv. 2022, 3, 1459–1471.
- Song, C.Y.; Yang, Y.J.; Yang, B.Y.; Sun, Y.Z.; Zhao, Y.P.; Wang, L.H. An Ultrasensitive SERS Sensor for Simultaneous Detection of Multiple Cancer-Related MiRNAs. Nanoscale 2016, 8, 17365–17373.
- Wang, H.N.; Crawford, B.M.; Norton, S.J.; Vo-Dinh, T. Direct and Label-Free Detection of MicroRNA Cancer Biomarkers Using SERS-Based Plasmonic Coupling Interference (PCI) Nanoprobes. J. Phys. Chem. B 2019, 123, 10245–10251.
- Guerrini, L.; Garcia-Rico, E.; O’loghlen, A.; Giannini, V.; Alvarez-Puebla, R.A. Surface-Enhanced Raman Scattering (Sers) Spectroscopy for Sensing and Characterization of Exosomes in Cancer Diagnosis. Cancers. 2021, 13, 2179.
- Lee, J.U.; Kim, S.; Sim, S.J. SERS-Based Nanoplasmonic Exosome Analysis: Enabling Liquid Biopsy for Cancer Diagnosis and Monitoring Progression. BioChip J. 2020, 14, 231–241.
- Vo-Dinh, T.; Allain, L.R.; Stokes, D.L. Cancer Gene Detection Using Surface-Enhanced Raman Scattering (SERS). J. Raman Spectrosc. 2002, 33, 511–516.
- Zhu, D.; Li, A.; Di, Y.; Wang, Z.; Shi, J.; Ni, X.; Wang, Y. Interference-Free SERS Nanoprobes for Labeling and Imaging of MT1-MMP in Breast Cancer Cells. Nanotechnology 2022, 33, 115702.
- Lin, J.; Chen, R.; Feng, S.; Pan, J.; Li, Y.; Chen, G.; Cheng, M.; Huang, Z.; Yu, Y.; Zeng, H. A Novel Blood Plasma Analysis Technique Combining Membrane Electrophoresis with Silver Nanoparticle-Based SERS Spectroscopy for Potential Applications in Noninvasive Cancer Detection. Nanomed. Nanotechnol. Biol. Med. 2011, 7, 655–663.
- Fabris, L. SERS Tags: The Next Promising Tool for Personalized Cancer Detection? ChemNanoMat 2016, 2, 249–258.
- Davis, R.M.; Campbell, J.L.; Burkitt, S.; Qiu, Z.; Kang, S.; Mehraein, M.; Miyasato, D.; Salinas, H.; Liu, J.T.C.; Zavaleta, C. A Raman Imaging Approach Using CD47 Antibody-Labeled SERS Nanoparticles for Identifying Breast Cancer and Its Potential to Guide Surgical Resection. Nanomaterials 2018, 8, 953.
- Yang, J.; Wang, Z.; Zong, S.; Song, C.; Zhang, R.; Cui, Y. Distinguishing Breast Cancer Cells Using Surface-Enhanced Raman Scattering. Anal. Bioanal. Chem. 2012, 402, 1093–1100.
- Dinish, U.S.; Balasundaram, G.; Chang, Y.T.; Olivo, M. Actively Targeted in Vivo Multiplex Detection of Intrinsic Cancer Biomarkers Using Biocompatible SERS Nanotags. Sci. Rep. 2014, 4, 4075.
- Liu, H.; Gao, X.; Xu, C.; Liu, D. SERS Tags for Biomedical Detection and Bioimaging. Theranostics 2022, 12, 1870–1903.
- Lu, S.; Lin, S.; Zhang, H.; Liang, L.; Shen, S. Methods of Respiratory Virus Detection: Advances towards Point-of-Care for Early Intervention. Micromachines 2021, 12, 697.
- Omidifar, N.; Lankarani, K.B.; Moghadami, M.; Shokripour, M.; Chashmpoosh, M.; Mousavi, S.M.; Hashemi, S.A.; Gholami, A. Different Laboratory Diagnosis Methods of COVID-19: A Systematic Review. Arch. Clin. Infect. Dis. 2021, 16, e110667.
- Mousavi, S.M.; Hashemi, S.A.; Rahmanian, V.; Kalashgrani, M.Y. Highly Sensitive Flexible SERS-Based Sensing Platform for Detection of Biosensors Highly Sensitive Flexible SERS-Based Sensing Platform for Detection of COVID-19. Biosensors 2022, 12, 466.
- Stöckel, S.; Kirchhoff, J.; Neugebauer, U.; Rösch, P.; Popp, J. The Application of Raman Spectroscopy for the Detection and Identification of Microorganisms. J. Raman Spectrosc. 2016, 47, 89–109.
- Soler, M.; Estevez, M.C.; Cardenosa-Rubio, M.; Astua, A.; Lechuga, L.M. How Nanophotonic Label-Free Biosensors Can Contribute to Rapid and Massive Diagnostics of Respiratory Virus Infections: COVID-19 Case. ACS Sens. 2020, 5, 2663–2678.
- Iravani, S. Nano- And Biosensors for the Detection of SARS-CoV-2: Challenges and Opportunities. Mater. Adv. 2020, 1, 3092–3103.
- Zhang, D.; Zhang, X.; Ma, R.; Deng, S.; Wang, X.; Wang, X.; Zhang, X.; Huang, X.; Liu, Y.; Li, G.; et al. Ultra-Fast and Onsite Interrogation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Waters via Surface Enhanced Raman Scattering (SERS). Water Res. 2021, 200, 117243.
- Mejía-Salazar, J.R.; Oliveira, O.N. Plasmonic Biosensing. Chem. Rev. 2018, 118, 10617–10625.
- Joung, Y.; Kim, K.; Lee, S.; Chun, B.-S.; Lee, S.; Hwang, J.; Choi, S.; Kang, T.; Lee, M.-K.; Chen, L.; et al. Rapid and Accurate On-Site Immunodiagnostics of Highly Contagious Severe Acute Respiratory Syndrome Coronavirus 2 Using Portable Surface-Enhanced Raman Scattering-Lateral Flow Assay Reader. ACS Sens. 2022, 7, 3470–3480.
- Saviñon-Flores, F.; Méndez, E.; López-Castaños, M.; Carabarin-Lima, A.; López-Castaños, K.A.; González-Fuentes, M.A.; Méndez-Albores, A. A Review on Sers-Based Detection of Human Virus Infections: Influenza and Coronavirus. Biosensors 2021, 11, 66.
- Lim, J.Y.; Nam, J.S.; Yang, S.E.; Shin, H.; Jang, Y.H.; Bae, G.U.; Kang, T.; Lim, K.I.; Choi, Y. Identification of Newly Emerging Influenza Viruses by Surface-Enhanced Raman Spectroscopy. Anal. Chem. 2015, 87, 11652–11659.
- Zhang, K.; Wang, Z.; Liu, H.; Perea-López, N.; Ranasinghe, J.C.; Bepete, G.; Minns, A.M.; Rossi, R.M.; Lindner, S.E.; Huang, S.X.; et al. Understanding the Excitation Wavelength Dependence and Thermal Stability of the SARS-CoV-2 Receptor-Binding Domain Using Surface-Enhanced Raman Scattering and Machine Learning. ACS Photonics 2022, 9, 2963–2972.
- Yang, Y.; Xu, B.; Murray, J.; Haverstick, J.; Chen, X.; Tripp, R.A.; Zhao, Y. Rapid and Quantitative Detection of Respiratory Viruses Using Surface-Enhanced Raman Spectroscopy and Machine Learning. Biosens. Bioelectron. 2022, 217, 114721.
- Ye, J.; Yeh, Y.; Xue, Y.; Wang, Z.; Zhang, N.; Liu, H.; Zhang, K.; Ricker, R.; Yu, Z.; Roder, A. Accurate Virus Identi Fi Cation with Interpretable Raman Signatures by Machine Learning. Proc. Natl. Acad. Sci. USA 2022, 199, e2118836119.
- Carlomagno, C.; Bertazioli, D.; Gualerzi, A.; Picciolini, S.; Banfi, P.I.; Lax, A.; Messina, E.; Navarro, J.; Bianchi, L.; Caronni, A.; et al. COVID-19 Salivary Raman Fingerprint: Innovative Approach for the Detection of Current and Past SARS-CoV-2 Infections. Sci. Rep. 2021, 11, 4943.
- Zavyalova, E.; Ambartsumyan, O.; Zhdanov, G.; Gribanyov, D.; Gushchin, V.; Tkachuk, A.; Rudakova, E.; Nikiforova, M.; Kuznetsova, N.; Popova, L.; et al. Sers-Based Aptasensor for Rapid Quantitative Detection of Sars-Cov-2. Nanomaterials 2021, 11, 1394.
- Hwang, C.S.H.; Lee, S.; Lee, S.; Kim, H.; Kang, T.; Lee, D.; Jeong, K.H. Highly Adsorptive Au-TiO2 Nanocomposites for the SERS Face Mask Allow the Machine-Learning-Based Quantitative Assay of SARS-CoV-2 in Artificial Breath Aerosols. ACS Appl. Mater. Interfaces 2022, 14, 54550–54557.
- Zhang, Z.; Jiang, S.; Wang, X.; Dong, T.; Wang, Y.; Li, D.; Gao, X.; Qu, Z.; Li, Y. A Novel Enhanced Substrate for Label-Free Detection of SARS-CoV-2 Based on Surface-Enhanced Raman Scattering. Sens. Actuators B Chem. 2022, 359, 131568.
- Wang, C.; Wang, C.; Wang, X.; Wang, K.; Zhu, Y.; Rong, Z.; Wang, W.; Xiao, R.; Wang, S. Magnetic SERS Strip for Sensitive and Simultaneous Detection of Respiratory Viruses. ACS Appl. Mater. Interfaces 2019, 11, 19495–19505.
- Zhang, D.; Huang, L.; Liu, B.; Ge, Q.; Dong, J.; Zhao, X. Rapid and Ultrasensitive Quantification of Multiplex Respiratory Tract Infection Pathogen via Lateral Flow Microarray Based on SERS Nanotags. Theranostics 2019, 9, 4849–4859.
- Yang, Y.; Peng, Y.; Lin, C.; Long, L.; Hu, J.; He, J.; Zeng, H.; Huang, Z.; Li, Z.Y.; Tanemura, M.; et al. Human ACE2-Functionalized Gold “Virus-Trap” Nanostructures for Accurate Capture of SARS-CoV-2 and Single-Virus SERS Detection. Nano-Micro Lett. 2021, 13, 109.
- Peng, Y.; Lin, C.; Long, L.; Masaki, T.; Tang, M.; Yang, L.; Liu, J.; Huang, Z.; Li, Z.; Luo, X.; et al. Charge-Transfer Resonance and Electromagnetic Enhancement Synergistically Enabling MXenes with Excellent SERS Sensitivity for SARS-CoV-2 S Protein Detection. Nano-Micro Lett. 2021, 13, 52.
- Gu, M.M.; Guan, P.C.; Xu, S.S.; Li, H.M.; Kou, Y.C.; Lin, X.D.; Kathiresan, M.; Song, Y.; Zhang, Y.J.; Jin, S.Z.; et al. Ultrasensitive Detection of SARS-CoV-2 S Protein with Aptamers Biosensor Based on Surface-Enhanced Raman Scattering. J. Chem. Phys. 2023, 158, 024203.
- Lim, J.Y.; Nam, J.S.; Shin, H.; Park, J.; Song, H.I.; Kang, M.; Lim, K.I.; Choi, Y. Identification of Newly Emerging Influenza Viruses by Detecting the Virally Infected Cells Based on Surface Enhanced Raman Spectroscopy and Principal Component Analysis. Anal. Chem. 2019, 91, 5677–5684.
- Eom, G.; Hwang, A.; Kim, H.; Yang, S.; Lee, D.K.; Song, S.; Ha, K.; Jeong, J.; Jung, J.; Lim, E.K.; et al. Diagnosis of Tamiflu-Resistant Influenza Virus in Human Nasal Fluid and Saliva Using Surface-Enhanced Raman Scattering. ACS Sens. 2019, 4, 2282–2287.
- Zhang, M.; Li, X.; Pan, J.; Zhang, Y.; Zhang, L.; Wang, C.; Yan, X.; Liu, X.; Lu, G. Ultrasensitive Detection of SARS-CoV-2 Spike Protein in Untreated Saliva Using SERS-Based Biosensor. Biosens. Bioelectron. 2021, 190, 113421.
- Yadav, S.; Sadique, M.A.; Ranjan, P.; Kumar, N.; Singhal, A.; Srivastava, A.K.; Khan, R. Sers Based Lateral Flow Immunoassay for Point-of-Care Detection of Sars-Cov-2 in Clinical Samples. ACS Appl. Bio Mater. 2021, 4, 2974–2995.
- Chen, S.; Meng, L.; Wang, L.; Huang, X.; Ali, S.; Chen, X.; Yu, M.; Yi, M.; Li, L.; Chen, X.; et al. SERS-Based Lateral Flow Immunoassay for Sensitive and Simultaneous Detection of Anti-SARS-CoV-2 IgM and IgG Antibodies by Using Gap-Enhanced Raman Nanotags. Sens. Actuators B Chem. 2021, 348, 130706.
- Liu, H.; Dai, E.; Xiao, R.; Zhou, Z.; Zhang, M.; Bai, Z.; Shao, Y.; Qi, K.; Tu, J.; Wang, C.; et al. Development of a SERS-Based Lateral Flow Immunoassay for Rapid and Ultra-Sensitive Detection of Anti-SARS-CoV-2 IgM/IgG in Clinical Samples. Sens. Actuators B Chem. 2021, 329, 129196.
- Antoine, D.; Mohammadi, M.; Vitt, M.; Dickie, J.M.; Jyoti, S.S.; Tilbury, M.A.; Johnson, P.A.; Wawrousek, K.E.; Wall, J.G. Rapid, Point-of-Care ScFv-SERS Assay for Femtogram Level Detection of SARS-CoV-2. ACS Sens. 2022, 7, 866–873.
- Li, Z.; Luo, Y.; Song, Y.; Zhu, Q.; Xu, T.; Zhang, X. One-Click Investigation of Shape Influence of Silver Nanostructures on SERS Performance for Sensitive Detection of COVID-19. Anal. Chim. Acta 2022, 1234, 340523.
- Kim, W.; Kim, S.; Han, J.; Kim, T.G.; Bang, A.; Choi, H.W.; Min, G.E.; Shin, J.H.; Moon, S.W.; Choi, S. An Excitation Wavelength-Optimized, Stable SERS Biosensing Nanoplatform for Analyzing Adenoviral and AstraZeneca COVID-19 Vaccination Efficacy Status Using Tear Samples of Vaccinated Individuals. Biosens. Bioelectron. 2022, 204, 114079.
- Karunakaran, V.; Joseph, M.M.; Yadev, I.; Sharma, H.; Shamna, K.; Saurav, S.; Sreejith, R.P.; Anand, V.; Beegum, R.; Regi David, S.; et al. A Non-Invasive Ultrasensitive Diagnostic Approach for COVID-19 Infection Using Salivary Label-Free SERS Fingerprinting and Artificial Intelligence. J. Photochem. Photobiol. B Biol. 2022, 234, 112545.
- Shanmukh, S.; Jones, L.; Driskell, J.; Zhao, Y.; Dluhy, R.; Tripp, R.A. Rapid and Sensitive Detection of Respiratory Virus Molecular Signatures Using a Silver Nanorod Array SERS Substrate. Nano Lett. 2006, 6, 2630–2636.
- Dluhy, R.A.; Shanmukh, S.; Jones, L.; Zhao, Y.P.; Driskell, J.D.; Tripp, R.A. Identification and Classification of Respiratory Syncytial Virus (RSV) Strains by Surface-Enhanced Raman Spectroscopy and Multivariate Statistical Techniques. Anal. Bioanal. Chem. 2008, 390, 1551–1555.
- Huang, J.; Wen, J.; Zhou, M.; Ni, S.; Le, W.; Chen, G.; Wei, L.; Zeng, Y.; Qi, D.; Pan, M.; et al. On-Site Detection of SARS-CoV-2 Antigen by Deep Learning-Based Surface-Enhanced Raman Spectroscopy and Its Biochemical Foundations. Anal. Chem. 2021, 93, 9174–9182.
- Yeh, Y.J.; Le, T.N.; Hsiao, W.W.W.; Tung, K.L.; Ostrikov, K.; Chiang, W.H. Plasmonic Nanostructure-Enhanced Raman Scattering for Detection of SARS-CoV-2 Nucleocapsid Protein and Spike Protein Variants. Anal. Chim. Acta 2023, 1239, 340651.
- Liu, Z.; Wang, C.; Zheng, S.; Yang, X.; Han, H.; Dai, Y.; Xiao, R. Simultaneously Ultrasensitive and Quantitative Detection of Influenza A Virus, SARS-CoV-2, and Respiratory Syncytial Virus via Multichannel Magnetic SERS-Based Lateral Flow Immunoassay. Nanomed. Nanotechnol. Biol. Med. 2023, 47, 102624.
- Chisanga, M.; Williams, H.; Boudreau, D.; Pelletier, J.N.; Trottier, S. Label-Free SERS for Rapid Differentiation of SARS-CoV-2-Induced Serum Metabolic Profiles in Non-Hospitalized Adults. Anal. Chem. 2023, 95, 3638–3646.
- Bacteria. Available online: https://microbiologysociety.org/why-microbiology-matters/what-is-microbiology/bacteria.html#:~:text=Bacteria%20are%20classified%20into%20five,)%20or%20corkscrew%20(spirochaetes) (accessed on 30 January 2023).
- Bacteria as Pathogens. Available online: https://sphweb.bumc.bu.edu/otlt/mph-modules/ph/ph709_infectiousagents/PH709_InfectiousAgents4.html#:~:text=While%20only%20about%205%25%20of,of%20human%20disease%20and%20death (accessed on 30 January 2023).
- Nanda, M.; Kumar, V.; Sharma, D.K. Multimetal Tolerance Mechanisms in Bacteria: The Resistance Strategies Acquired by Bacteria That Can Be Exploited to ‘Clean-up’ Heavy Metal Contaminants from Water. Aquat. Toxicol. 2019, 212, 1–10.
- Glick, B.R. Phytoremediation: Synergistic Use of Plants and Bacteria to Clean up the Environment. Biotechnol. Adv. 2003, 21, 383–393.
- Kulshreshtha, A.; Agrawal, R.; Barar, M.; Saxena, S. A Review on Bioremediation of Heavy Metals in Contaminated Water. IOSR J. Environ. Sci. Toxicol. Food Technol. 2014, 8, 44–50.
- Zhou, X.; Hu, Z.; Yang, D.; Xie, S.; Jiang, Z.; Niessner, R.; Haisch, C.; Zhou, H.; Sun, P. Bacteria Detection: From Powerful SERS to Its Advanced Compatible Techniques. Adv. Sci. 2020, 7, 2001739.
- Wang, R.; Kim, K.; Choi, N.; Wang, X.; Lee, J.; Jeon, J.H.; Rhie, G.E.; Choo, J. Highly Sensitive Detection of High-Risk Bacterial Pathogens Using SERS-Based Lateral Flow Assay Strips. Sens. Actuators B Chem. 2018, 270, 72–79.
- Zhu, T.; Hu, Y.; Yang, K.; Dong, N.; Yu, M.; Jiang, N. A Novel SERS Nanoprobe Based on the Use of Core-Shell Nanoparticles with Embedded Reporter Molecule to Detect E. coli O157:H7 with High Sensitivity. Microchim. Acta 2018, 185, 30.
- Chisanga, M.; Muhamadali, H.; Ellis, D.I.; Goodacre, R. Surface-Enhanced Raman Scattering (SERS) in Microbiology: Illumination and Enhancement of the Microbial World. Appl. Spectrosc. 2018, 72, 987–1000.
- Kim, J.A.; Wales, D.J.; Thompson, A.J.; Yang, G.Z. Fiber-optic SERS probes fabricated using two-photon polymerization for rapid detection of bacteria. Adv. Opt. Mater. 2020, 8, 1901934.
- Zhou, H.; Yang, D.; Ivleva, N.P.; Mircescu, N.E.; Niessner, R.; Haisch, C. SERS Detection of Bacteria in Water by in Situ Coating with Ag Nanoparticles. Anal. Chem. 2014, 86, 1525–1533.
- Yang, Y.; Zeng, C.; Huang, J.; Wang, M.; Qi, W.; Wang, H.; He, Z. Specific and Quantitative Detection of Bacteria Based on Surface Cell Imprinted SERS Mapping Platform. Biosens. Bioelectron. 2022, 215, 114524.
- Pearson, B.; Wang, P.; Mills, A.; Pang, S.; McLandsborough, L.; He, L. Innovative Sandwich Assay with Dual Optical and SERS Sensing Mechanisms for Bacterial Detection. Anal. Methods 2017, 9, 4732–4739.
- Hudson, S.D.; Chumanov, G. Bioanalytical Applications of SERS (Surface-Enhanced Raman Spectroscopy). Anal. Bioanal. Chem. 2009, 394, 679–686.
- Mosier-Boss, P.A. Review on SERS of Bacteria. Biosensors 2017, 7, 51.
- Jarvis, R.M.; Goodacre, R. Characterisation and Identification of Bacteria Using SERS. Chem. Soc. Rev. 2008, 37, 931–936.
- Xia, J.; Li, W.; Sun, M.; Wang, H. Application of SERS in the Detection of Fungi, Bacteria and Viruses. Nanomaterials 2022, 12, 3572.
- Wang, C.; Meloni, M.M.; Wu, X.; Zhuo, M.; He, T.; Wang, J.; Wang, C.; Dong, P. Magnetic Plasmonic Particles for SERS-Based Bacteria Sensing: A Review. AIP Adv. 2019, 9, 010701.
- Efrima, S.; Zeiri, L. Understanding SERS of Bacteria. J. Raman Spectrosc. 2009, 40, 277–288.
- Liu, H.B.; Du, X.J.; Zang, Y.X.; Li, P.; Wang, S. SERS-Based Lateral Flow Strip Biosensor for Simultaneous Detection of Listeria Monocytogenes and Salmonella Enterica Serotype Enteritidis. J. Agric. Food Chem. 2017, 65, 10290–10299.
- Mungroo, N.A.; Oliveira, G.; Neethirajan, S. SERS Based Point-of-Care Detection of Food-Borne Pathogens. Microchim. Acta 2016, 183, 697–707.
- Lin, H.Y.; Huang, C.H.; Hsieh, W.H.; Liu, L.H.; Lin, Y.C.; Chu, C.C.; Wang, S.T.; Kuo, I.T.; Chau, L.K.; Yang, C.Y. On-Line SERS Detection of Single Bacterium Using Novel SERS Nanoprobes and a Microfl Uidic Dielectrophoresis Device. Small 2014, 10, 4700–4710.
- Wang, Y.; Lee, K.; Irudayaraj, J. Silver Nanosphere SERS Probes for Sensitive Identification of Pathogens. J. Phys. Chem. C 2010, 114, 16122–16128.
- Witkowska, E.; Korsak, D.; Kowalska, A.; Janeczek, A.; Kamińska, A. Strain-Level Typing and Identification of Bacteria—A Novel Approach for SERS Active Plasmonic Nanostructures. Anal. Bioanal. Chem. 2018, 410, 5019–5031.
- Pang, Y.; Wan, N.; Shi, L.; Wang, C.; Sun, Z.; Xiao, R.; Wang, S. Dual-Recognition Surface-Enhanced Raman Scattering (SERS)Biosensor for Pathogenic Bacteria Detection by Using Vancomycin-SERS Tags and Anal. Chim. Acta 2019, 1077, 288–296.
- Gao, X.; Yin, Y.; Wu, H.; Hao, Z.; Li, J.; Wang, S.; Liu, Y. Integrated SERS Platform for Reliable Detection and Photothermal Elimination of Bacteria in Whole Blood Samples. Anal. Chem. 2021, 93, 1569–1577.
- Zhou, Z.; Xiao, R.; Cheng, S.; Wang, S.; Shi, L.; Wang, C.; Qi, K.; Wang, S. A Universal SERS-Label Immunoassay for Pathogen Bacteria Detection Based on Separation and Antibody-Protein A Orientation Recognition. Anal. Chim. Acta 2021, 1160, 338421.
- Wang, J.; Wu, X.; Wang, C.; Rong, Z.; Ding, H.; Li, H.; Li, S.; Shao, N.; Dong, P.; Xiao, R.; et al. Facile Synthesis of Au-Coated Magnetic Nanoparticles and Their Application in Bacteria Detection via a SERS Method. ACS Appl. Mater. Interfaces 2016, 8, 19958–19967.
- Wang, C.; Wang, J.; Li, M.; Qu, X.; Zhang, K.; Rong, Z.; Xiao, R.; Wang, S. A Rapid SERS Method for Label-Free Bacteria Detection Using Polyethylenimine-Modified Au-Coated Magnetic Microspheres and Nanoparticles. Analyst 2016, 141, 6226–6238.
- Huang, L.; Sun, D.W.; Wu, Z.; Pu, H.; Wei, Q. Reproducible, Shelf-Stable, and Bioaffinity SERS Nanotags Inspired by Multivariate Polyphenolic Chemistry for Bacterial Identification. Anal. Chim. Acta 2021, 1167, 338570.
- Bi, L.; Wang, X.; Cao, X.; Liu, L.; Bai, C.; Zheng, Q.; Choo, J.; Chen, L. SERS-Active Core-Shell Nanorod () Tags for Ultrasensitive Bacteria Detection and Antibiotic-Susceptibility Testing. Talanta 2020, 220, 121397.
- Hunter, R.; Sohi, A.N.; Khatoon, Z.; Berthiaume, V.R.; Alarcon, E.I.; Godin, M.; Anis, H. Optofluidic Label-Free SERS Platform for Rapid Bacteria Detection in Serum. Sens. Actuators B Chem. 2019, 300, 126907.
- Sivanesan, A.; Witkowska, E.; Adamkiewicz, W.; Dziewit, Ł.; Kamińska, A.; Waluk, J. Nanostructured Silver-Gold Bimetallic SERS Substrates for Selective Identification of Bacteria in Human Blood. Analyst 2014, 139, 1037–1043.
- Witkowska, E.; Szymborski, T.; Kamińska, A.; Waluk, J. Polymer Mat Prepared via ForcespinningTM as a SERS Platform for Immobilization and Detection of Bacteria from Blood Plasma. Mater. Sci. Eng. C 2017, 71, 345–350.
- Zhang, L.; Xu, J.; Mi, L.; Gong, H.; Jiang, S.; Yu, Q. Multifunctional Magnetic-Plasmonic Nanoparticles for Fast Concentration and Sensitive Detection of Bacteria Using SERS. Biosens. Bioelectron. 2012, 31, 130–136.
- Krafft, B.; Tycova, A.; Urban, R.D.; Dusny, C.; Belder, D. Microfluidic device for concentration and SERS-based detection of bacteria in drinking water. Electrophoresis 2021, 42, 86–94.
- Yang, E.; Li, D.; Yin, P.; Xie, Q.; Li, Y.; Lin, Q.; Duan, Y. A Novel Surface-Enhanced Raman Scattering (SERS) Strategy for Ultrasensitive Detection of Bacteria Based on Three-Dimensional (3D) DNA Walker. Biosens. Bioelectron. 2021, 172, 112758.
- Wang, C.; Wang, C.; Li, J.; Tu, Z.; Gu, B.; Wang, S. Ultrasensitive and Multiplex Detection of Four Pathogenic Bacteria on a Bi-Channel Lateral Flow Immunoassay Strip with Three-Dimensional Membrane-like SERS Nanostickers. Biosens. Bioelectron. 2022, 214, 114525.
- Kearns, H.; Goodacre, R.; Jamieson, L.E.; Graham, D.; Faulds, K. SERS Detection of Multiple Antimicrobial-Resistant Pathogens Using Nanosensors. Anal. Chem. 2017, 89, 12666–12673.
- Gracie, K.; Correa, E.; Mabbott, S.; Dougan, J.A.; Graham, D.; Goodacre, R.; Faulds, K. Simultaneous Detection and Quantification of Three Bacterial Meningitis Pathogens by SERS. Chem. Sci. 2014, 5, 1030–1040.
- Mosier-Boss, P.A.; Sorensen, K.C.; George, R.D.; Obraztsova, A. SERS Substrates Fabricated Using Ceramic Filters for the Detection of Bacteria. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2016, 153, 591–598.
- Walter, A.; März, A.; Schumacher, W.; Rösch, P.; Popp, J. Towards a Fast, High Specific and Reliable Discrimination of Bacteria on Strain Level by Means of SERS in a Microfluidic Device. Lab Chip 2011, 11, 1013–1021.
- Wu, X.; Xu, C.; Tripp, R.A.; Huang, Y.W.; Zhao, Y. Detection and Differentiation of Foodborne Pathogenic Bacteria in Mung Bean Sprouts Using Field Deployable Label-Free SERS Devices. Analyst 2013, 138, 3005–3012.
- Ankamwar, B.; Sur, U.K.; Das, P. SERS Study of Bacteria Using Biosynthesized Silver Nanoparticles as the SERS Substrate. Anal. Methods 2016, 8, 2335–2340.
- Ciloglu, F.U.; Caliskan, A.; Saridag, A.M.; Kilic, I.H.; Tokmakci, M.; Kahraman, M.; Aydin, O. Drug-Resistant Staphylococcus Aureus Bacteria Detection by Combining Surface-Enhanced Raman Spectroscopy (SERS) and Deep Learning Techniques. Sci. Rep. 2021, 11, 18444.
- Nerve Agents, BBC Report. Available online: https://www.bbc.com/news/uk-43431537 (accessed on 30 January 2023).
- Lister, A.P.; Sellors, W.J.; Howle, C.R.; Mahajan, S. Raman Scattering Techniques for Defense and Security Applications. Anal. Chem. 2021, 93, 417–429.
- Sadayoshi, O.H.B.U.; Yamashina, A.; Takasu, N.; Yamaguchi, T.; Murai, T.; Nakano, K.; Hinohara, S. Sarin poisoning on Tokyo subway. South. Med. J. 1997, 90, 587–593.
- Inscore, F.E.; Gift, A.D.; Maksymiuk, P.; Farquharson, S. Characterization of Chemical Warfare G-Agent Hydrolysis Products by Surface-Enhanced Raman Spectroscopy. Chem. Biol. Point Sens. Homel. Def. II 2004, 5585, 46.
- Mukherjee, S.; Gupta, R.D. Organophosphorus Nerve Agents: Types, Toxicity, and Treatments. J. Toxicol. 2020, 2020, 3007984.
- Saylan, Y.; Akgönüllü, S.; Denizli, A. Plasmonic Sensors for Monitoring Biological and Chemical Threat Agents. Biosensors 2020, 10, 142.
- Primera-Pedrozo, O.M.; Jerez-Rozo, J.I.; De La Cruz-Montoya, E.; Luna-Pineda, T.; Pacheco-Londoño, L.C.; Hernández-Rivera, S.P. Nanotechnology-Based Detection of Explosives and Biological Agents Simulants. IEEE Sens. J. 2008, 8, 963–973.
- Yan, F.; Vo-Dinh, T. Surface-Enhanced Raman Scattering Detection of Chemical and Biological Agents Using a Portable Raman Integrated Tunable Sensor. Sens. Actuators B Chem. 2007, 121, 61–66.
- Pearman, W.F.; Fountain, A.W. Classification of Chemical and Biological Warfare Agent Simulants by Surface-Enhanced Raman Spectroscopy and Multivariate Statistical Techniques. Appl. Spectrosc. 2006, 60, 356–365.
- Hakonen, A.; Rindzevicius, T.; Schmidt, M.S.; Andersson, P.O.; Juhlin, L.; Svedendahl, M.; Boisen, A.; Käll, M. Detection of Nerve Gases Using Surface-Enhanced Raman Scattering Substrates with High Droplet Adhesion. Nanoscale 2016, 8, 1305–1308.
- Juhlin, L.; Mikaelsson, T.; Hakonen, A.; Stenbæk, M. Selective Surface-Enhanced Raman Scattering Detection of Tabun, VX and Cyclosarin Nerve Agents Using 4-Pyridine Amide Oxime Functionalized Gold Nanopillars Talanta Selective Surface-Enhanced Raman Scattering Detection of Tabun, VX and Cyclosarin Nerve A. Talanta 2020, 211, 120721.
- Farquharson, S.; Gift, A.; Maksymiuk, P.; Inscore, F. Surface-Enhanced Raman Spectra of VX and Its Hydrolysis Products. Appl. Spectrosc. 2005, 59, 654–660.
- Heleg-Shabtai, V.; Sharabi, H.; Zaltsman, A.; Ron, I.; Pevzner, A. Surface-Enhanced Raman Spectroscopy (SERS) for Detection of VX and HD in the Gas Phase Using a Hand-Held Raman Spectrometer. Analyst 2020, 145, 6334–6341.
- Zhao, Q.; Liu, G.; Zhang, H.; Zhou, F.; Li, Y.; Cai, W. SERS-Based Ultrasensitive Detection of Organophosphorus Nerve Agents via Substrate’s Surface Modification. J. Hazard. Mater. 2017, 324, 194–202.
- Spencer, K.M.; Sylvia, J.M.; Clauson, S.L.; Janni, J.A. Surface-Enhanced Raman as a Water Monitor for Warfare Agents. Vib. Spectrosc. Sens. Syst. 2002, 4577, 158.
- Bertone, J.F.; Cordeiro, K.L.; Sylvia, J.M.; Spencer, K.M. A Nanoengineered Sensor to Detect Vibrational Modes of Warfare Agents/Explosives Using Surface-Enhanced Raman Scattering. Sens. Command. Control. Commun. Intell. Technol. Homel. Secur. Homel. Def. III 2004, 5403, 387.
- Kim, Y.T.; Kim, D.; Park, S.; Zhexembekova, A.; Byeon, M.; Hong, T.E.; Lee, J.; Lee, C.Y. Aqueous Microlenses for Localized Collection and Enhanced Raman Spectroscopy of Gaseous Molecules. Adv. Opt. Mater. 2021, 9, 2101209.
- Wu, J.; Zhu, Y.; Gao, J.; Chen, J.; Feng, J.; Guo, L.; Xie, J. A Simple and Sensitive Surface-Enhanced Raman Spectroscopic Discriminative Detection of Organophosphorous Nerve Agents. Anal. Bioanal. Chem. 2017, 409, 5091–5099.
- Lafuente, M.; Berenschot, E.J.W.; Tiggelaar, R.M.; Mallada, R.; Tas, N.R.; Pina, M.P. 3D Fractals as SERS Active Platforms: Preparation and Evaluation for Gas Phase Detection of G-Nerve Agents. Micromachines 2018, 9, 60.
- Goel, A.K. Anthrax: A Disease of Biowarfare and Public Health Importance. World J. Clin. Cases 2015, 3, 20.
- Farrell, M.E.; Pellegrino, P.M. Army Relevant Biological Hazards Detection with Commercial SERS Substrates. Biosen. Nanomed. V 2012, 8460, 84600J.
- Sajanlal, P.R.; Pradeep, T. Functional Hybrid Nickel Nanostructures as Recyclable SERS Substrates: Detection of Explosives and Biowarfare Agents. Nanoscale 2012, 4, 3427–3437.
- Wang, T.; Dong, P.; Zhu, C.; Sha, P.; Gao, W.; Wu, Y.; Wu, X. Trace Detection of Anthrax Protective Antigens via a Competitive Method Based on Surface-Enhanced Raman Scattering. Sens. Actuators B Chem. 2021, 346, 130467.
- Gao, R.; Ko, J.; Cha, K.; Ho Jeon, J.; Rhie, G.E.; Choi, J.; de Mello, A.J.; Choo, J. Fast and Sensitive Detection of an Anthrax Biomarker Using SERS-Based Solenoid Microfluidic Sensor. Biosens. Bioelectron. 2015, 72, 230–236.
- Naqvi, T.K.; Bajpai, A.; Bharati, M.S.S.; Kulkarni, M.M.; Siddiqui, A.M.; Soma, V.R.; Dwivedi, P.K. Ultra-Sensitive Reusable SERS Sensor for Multiple Hazardous Materials Detection on Single Platform. J. Hazard. Mater. 2021, 407, 124353.
- Sengupta, A.; Shende, C.; Farquharson, S.; Inscore, F. Detection of Bacillus Anthracis Spores Using Peptide Functionalized SERS-Active Substrates. Int. J. Spectrosc. 2012, 2012, 176851.
- Yilmaz, M.; Senlik, E.; Biskin, E.; Yavuz, M.S.; Tamer, U.; Demirel, G. Combining 3-D Plasmonic Gold Nanorod Arrays with Colloidal Nanoparticles as a Versatile Concept for Reliable, Sensitive, and Selective Molecular Detection by SERS. Phys. Chem. Chem. Phys. 2014, 16, 5563–5570.
- Li, B.; Wang, T.; Bai, W.; Su, Q.; Wu, X.; Dong, P. Label-Free and Rapid Detection of Anthrax Protective Antigen by Surface-Enhanced Raman Scattering on Au Nanorods. IEEE Sens. J. 2021, 21, 18425–18434.
- Cheung, M.; Lee, W.W.Y.; Cowcher, D.P.; Goodacre, R.; Bell, S.E.J. SERS of Meso-Droplets Supported on Superhydrophobic Wires Allows Exquisitely Sensitive Detection of Dipicolinic Acid, an Anthrax Biomarker, Considerably below the Infective Dose. Chem. Commun. 2016, 52, 9925–9928.
- Félix-Rivera, H.; González, R.; Rodríguez, G.D.M.; Primera-Pedrozo, O.M.; Ríos-Velázquez, C.; Hernández-Rivera, S.P. Improving SERS Detection of Bacillus Thuringiensis Using Silver Nanoparticles Reduced with Hydroxylamine and with Citrate Capped Borohydride. Int. J. Spectrosc. 2011, 2011, 989504.
- FountainIII, A.W.; Pearman, W.F. Multivariate Statistical Classification of Surface Enhanced Raman Spectra of Chemical and Biological Warfare Agent Simulants. Chem. Biol. Sens. Ind. Environ. Secur. 2005, 5994, 180–193.
- Arano-Martinez, J.A.; Martínez-González, C.L.; Salazar, M.I.; Torres-Torres, C. A Framework for Biosensors Assisted by Multiphoton Effects and Machine Learning. Biosensors 2022, 12, 710.
- Luo, R.; Popp, J.; Bocklitz, T. Deep Learning for Raman Spectroscopy: A Review. Analytica 2022, 3, 287–301.
- Ralbovsky, N.M.; Lednev, I.K. Towards Development of a Novel Universal Medical Diagnostic Method: Raman Spectroscopy and Machine Learning. Chem. Soc. Rev. 2020, 49, 7428–7453.
- Ding, Y.; Sun, Y.; Liu, C.; Jiang, Q.Y.; Chen, F.; Cao, Y. SERS-Based Biosensors Combined with Machine Learning for Medical Application. ChemistryOpen 2023, 12, e202200192.
- Cui, F.; Yue, Y.; Zhang, Y.; Zhang, Z.; Zhou, H.S. Advancing Biosensors with Machine Learning. ACS Sens. 2020, 5, 3346–3364.
- Lv, R.; Wang, Z.; Ma, Y.; Li, W.; Tian, J. Machine Learning Enhanced Optical Spectroscopy for Disease Detection. J. Phys. Chem. Lett. 2022, 13, 9238–9249.
- Schackart, K.E.; Yoon, J.Y. Machine Learning Enhances the Performance of Bioreceptor-Free Biosensors. Sensors 2021, 21, 5519.
- Lussier, F.; Missirlis, D.; Spatz, J.P.; Masson, J.F. Machine-Learning-Driven Surface-Enhanced Raman Scattering Optophysiology Reveals Multiplexed Metabolite Gradients Near Cells. ACS Nano 2019, 13, 1403–1411.
- Nguyen, P.H.L.; Hong, B.; Rubin, S.; Fainman, Y. Machine Learning for Composition Analysis of SsDNA Using Chemical Enhancement in SERS. Biomed. Opt. Express 2020, 11, 5092.
- Narla, L.M.; Rao, S.V. Identification of Metals and Alloys Using Color CCD Images of Laser-Induced Breakdown Emissions Coupled with Machine Learning. Appl. Phys. B Lasers Opt. 2020, 126, 113.
- Beeram, R.; Banerjee, D.; Narlagiri, L.M.; Soma, V.R. Machine Learning for Rapid Quantification of Trace Analyte Molecules Using SERS and Flexible Plasmonic Paper Substrates. Anal. Methods 2022, 14, 1788–1796.
- Murthy, N.L.; Abdul Salam, S.; Rao, S.V. Stand-off Femtosecond Laser Induced Breakdown Spectroscopy of Metals, Soil, Plastics and Classification Studies. In Proceedings of the 2019 Workshop on Recent Advances in Photonics (WRAP), Guwahati, India, 13–14 December 2019; pp. 1–3.
- Boehmke, B.; Greenwell, B. Hands-On Machine Learning with R; Chapman and Hall/CRC: Boca Raton, FL, USA, 2019; ISBN 9781492032649.
- Li, D.; Zhang, Q.; Deng, B.; Chen, Y.; Ye, L. Rapid, Sensitive Detection of Ganciclovir, Penciclovir and Valacyclovir-Hydrochloride by Artificial Neural Network and Partial Least Squares Combined with Surface Enhanced Raman Spectroscopy. Appl. Surf. Sci. 2021, 539, 148224.
- Boulesteix, A.L.; Strimmer, K. Partial Least Squares: A Versatile Tool for the Analysis of High-Dimensional Genomic Data. Brief. Bioinform. 2007, 8, 32–44.
- Deng, W.; Huang, Z.; Zhang, J.; Xu, J. A Data Mining Based System for Transaction Fraud Detection. In Proceedings of the 2021 IEEE International Conference on Consumer Electronics and Computer Engineering (ICCECE), Guangzhou, China, 15–17 January 2021; pp. 542–545.
- Fan, X.; Ming, W.; Zeng, H.; Zhang, Z.; Lu, H. Deep Learning-Based Component Identification for the Raman Spectra of Mixtures. Analyst 2019, 144, 1789–1798.
- Zhou, H.; Xu, L.; Ren, Z.; Zhu, J.; Lee, C. Machine Learning-Augmented Surface-Enhanced Spectroscopy toward next-Generation Molecular Diagnostics. Nanoscale Adv. 2023, 5, 538–570.
- Malinick, A.S.; Stuart, D.D.; Lambert, A.S.; Cheng, Q. Surface Plasmon Resonance Imaging (SPRi) in Combination with Machine Learning for Microarray Analysis of Multiple Sclerosis Biomarkers in Whole Serum. Biosens. Bioelectron. X 2022, 10, 100127.
- Pradhan, P.; Guo, S.; Ryabchykov, O.; Popp, J.; Bocklitz, T.W. Deep Learning a Boon for Biophotonics? J. Biophotonics 2020, 13, e201960186.
- Moon, G.; Lee, J.; Lee, H.; Yoo, H.; Ko, K.; Im, S.; Kim, D. Machine Learning and Its Applications for Plasmonics in Biology. Cell Rep. Phys. Sci. 2022, 3, 101042.
- Sun, Y.; Shi, L.; Mi, L.; Guo, R.; Li, T. Recent Progress of SERS Optical Nanosensors for MiRNA Analysis. J. Mater. Chem. B 2020, 8, 5178–5183.
- Raji, H.; Tayyab, M.; Sui, J.; Mahmoodi, S.R.; Javanmard, M. Biosensors and Machine Learning for Enhanced Detection, Stratification, and Classification of Cells: A Review. Biomed. Microdevices 2022, 24, 26.
- Banerjee, A.; Maity, S.; Mastrangelo, C.H. Nanostructures for biosensing, with a brief overview on Cancer Detection, IoT, and the Role of Machine Learning In Smart Biosensors. Sensors 2021, 21, 1253.
- Beeram, R.; Vendamani, V.S.; Soma, V.R. Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy Deep Learning Approach to Overcome Signal Fluctuations in SERS for Efficient On-Site Trace Explosives Detection. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2023, 289, 122218.
- Moon, G.; Son, T.; Lee, H.; Kim, D. Deep Learning Approach for Enhanced Detection of Surface Plasmon Scattering. Anal. Chem. 2019, 91, 9538–9545.
- Gupta, A.K.; Hsu, C.H.; Lai, C.S. Enhancement of the Au/ZnO-NA Plasmonic SERS Signal Using Principal Component Analysis as a Machine Learning Approach. IEEE Photonics J. 2020, 12, 1–11.
- Vendamani, V.S.; Beeram, R.; Neethish, M.M.; Rao, S.V.S.N.; Rao, S.V. Wafer-Scale Silver Nanodendrites with Homogeneous Distribution of Gold Nanoparticles for Biomolecules Detection. iScience 2022, 25, 104849.
- Erzina, M.; Trelin, A.; Guselnikova, O.; Dvorankova, B.; Strnadova, K.; Perminova, A.; Ulbrich, P.; Mares, D.; Jerabek, V.; Elashnikov, R.; et al. Precise Cancer Detection via the Combination of Functionalized SERS Surfaces and Convolutional Neural Network with Independent Inputs. Sens. Actuators B Chem. 2020, 308, 127660.
- Wang, S.; Dong, H.; Shen, W.; Yang, Y.; Li, Z.; Liu, Y.; Wang, C.; Gu, B.; Zhang, L. Rapid SERS Identification of Methicillin-Susceptible and Methicillin-Resistant: Staphylococcus Aureus via Aptamer Recognition and Deep Learning. RSC Adv. 2021, 11, 34425–34431.
- Kazemzadeh, M.; Hisey, C.L.; Dauros-Singorenko, P.; Swift, S.; Zargar-Shoshtari, K.; Xu, W.; Broderick, N.G.R. Label-Free Classification of Bacterial Extracellular Vesicles by Combining Nanoplasmonic Sensors with Machine Learning. IEEE Sens. J. 2022, 22, 1128–1137.
- Dong, R.; Weng, S.; Yang, L.; Liu, J. Detection and Direct Readout of Drugs in Human Urine Using Dynamic Surface-Enhanced Raman Spectroscopy and Support Vector Machines. Anal. Chem. 2015, 87, 2937–2944.
- Lin, C.; Liang, S.; Li, Y.; Peng, Y.; Huang, Z.; Li, Z.; Yang, Y.; Luo, X. Localized Plasmonic Sensor for Direct Identifying Lung and Colon Cancer from the Blood. Biosens. Bioelectron. 2022, 211, 114372.
- Peng, S.; Lu, D.; Zhang, B.; You, R.; Chen, J.; Xu, H.; Lu, Y. Machine Learning—Assisted Internal Standard Calibration Label—Free SERS Strategy for Colon Cancer Detection. Anal. Bioanal. Chem. 2023.
- Seifert, S.; Merk, V.; Kneipp, J. Identification of Aqueous Pollen Extracts Using Surface Enhanced Raman Scattering (SERS) and Pattern Recognition Methods. J. Biophotonics 2016, 9, 181–189.
- Hassoun, M.; Rüger, J.; Kirchberger-Tolstik, T.; Schie, I.W.; Henkel, T.; Weber, K.; Cialla-May, D.; Krafft, C.; Popp, J. A Droplet-Based Microfluidic Chip as a Platform for Leukemia Cell Lysate Identification Using Surface-Enhanced Raman Scattering. Anal. Bioanal. Chem. 2018, 410, 999–1006.
- Mühlig, A.; Bocklitz, T.; Labugger, I.; Dees, S.; Henk, S.; Richter, E.; Andres, S.; Merker, M.; Stöckel, S.; Weber, K.; et al. LOC-SERS: A Promising Closed System for the Identification of Mycobacteria. Anal. Chem. 2016, 88, 7998–8004.
- Bratchenko, L.A.; Al-Sammarraie, S.Z.; Tupikova, E.N.; Konovalova, D.Y.; Lebedev, P.A.; Zakharov, V.P.; Bratchenko, I.A. Analyzing the Serum of Hemodialysis Patients with End-Stage Chronic Kidney Disease by Means of the Combination of SERS and Machine Learning. Biomed. Opt. Express 2022, 13, 4926.
- Gao, K.; Zhu, H.; Charron, B.; Mochizuki, T.; Dong, C.; Ding, H.; Cui, Y.; Lu, M.; Peng, W.; Zhu, S.; et al. Combining Dense Au Nanoparticle Layers and 2D Surface-Enhanced Raman Scattering Arrays for the Identification of Mutant Cyanobacteria Using Machine Learning. J. Phys. Chem. C 2022, 126, 9446–9455.
- Ikponmwoba, E.; Ukorigho, O.; Moitra, P.; Pan, D.; Gartia, M.R.; Owoyele, O. A Machine Learning Framework for Detecting COVID-19 Infection Using Surface-Enhanced Raman Scattering. Biosensors 2022, 12, 589.
- Pérez-Jiménez, A.I.; Lyu, D.; Lu, Z.; Liu, G.; Ren, B. Surface-Enhanced Raman Spectroscopy: Benefits, Trade-Offs and Future Developments. Chem. Sci. 2020, 11, 4563–4577.
- Hou, M.; Huang, Y.; Ma, L.; Zhang, Z. Quantitative Analysis of Single and Mix Food Antiseptics Basing on SERS Spectra with PLSR Method. Nanoscale Res. Lett. 2016, 11, 296.
- Yan, S.; Liu, C.; Fang, S.; Ma, J.; Qiu, J.; Xu, D.; Li, L.; Yu, J.; Li, D.; Liu, Q. SERS-Based Lateral Flow Assay Combined with Machine Learning for Highly Sensitive Quantitative Analysis of Escherichia coli O157:H7. Anal. Bioanal. Chem. 2020, 412, 7881–7890.
- Nguyen, C.Q.; Thrift, W.J.; Bhattacharjee, A.; Ranjbar, S.; Gallagher, T.; Darvishzadeh-Varcheie, M.; Sanderson, R.N.; Capolino, F.; Whiteson, K.; Baldi, P.; et al. Longitudinal Monitoring of Biofilm Formation via Robust Surface-Enhanced Raman Scattering Quantification of Pseudomonas Aeruginosa -Produced Metabolites. ACS Appl. Mater. Interfaces 2018, 10, 12364–12373.
- Lee, K.M.; Herrman, T.J. Determination and Prediction of Fumonisin Contamination in Maize by Surface–Enhanced Raman Spectroscopy (SERS). Food Bioprocess Technol. 2016, 9, 588–603.
- Kuligowski, J.; El-Zahry, M.R.; Sánchez-Illana, Á.; Quintás, G.; Vento, M.; Lendl, B. Surface Enhanced Raman Spectroscopic Direct Determination of Low Molecular Weight Biothiols in Umbilical Cord Whole Blood. Analyst 2016, 141, 2165–2174.
- Tan, A.; Zhao, Y.; Sivashanmugan, K.; Squire, K.; Wang, A.X. Quantitative TLC-SERS Detection of Histamine in Seafood with Support Vector Machine Analysis. Food Control 2019, 103, 111–118.
- Rahman, A.; Kang, S.; Wang, W.; Huang, Q.; Kim, I.; Vikesland, P.J. Lectin-Modified Bacterial Cellulose Nanocrystals Decorated with Au Nanoparticles for Selective Detection of Bacteria Using Surface-Enhanced Raman Scattering Coupled with Machine Learning. ACS Appl. Nano Mater. 2022, 5, 259–268.
- Banaei, N.; Moshfegh, J.; Mohseni-Kabir, A.; Houghton, J.M.; Sun, Y.; Kim, B. Machine Learning Algorithms Enhance the Specificity of Cancer Biomarker Detection Using SERS-Based Immunoassays in Microfluidic Chips. RSC Adv. 2019, 9, 1859–1868.
- Cheng, N.; Chen, D.; Lou, B.; Fu, J.; Wang, H. A Biosensing Method for the Direct Serological Detection of Liver Diseases by Integrating a SERS-Based Sensor and a CNN Classifier. Biosens. Bioelectron. 2021, 186, 113246.
- Zhang, X.; Liang, B.; Zhang, J.; Hao, X.; Xu, X.; Chang, H.M.; Leung, P.C.K.; Tan, J. Raman Spectroscopy of Follicular Fluid and Plasma with Machine-Learning Algorithms for Polycystic Ovary Syndrome Screening. Mol. Cell. Endocrinol. 2021, 523, 111139.
- Barucci, A.; D’Andrea, C.; Farnesi, E.; Banchelli, M.; Amicucci, C.; De Angelis, M.; Hwang, B.; Matteini, P. Label-Free SERS Detection of Proteins Based on Machine Learning Classification of Chemo-Structural Determinants. Analyst 2021, 146, 674–682.
- Kazemzadeh, M.; Hisey, C.L.; Zargar-Shoshtari, K.; Xu, W.; Broderick, N.G.R. Deep Convolutional Neural Networks as a Unified Solution for Raman Spectroscopy-Based Classification in Biomedical Applications. Opt. Commun. 2022, 510, 127977.
- Othman, N.H.; Yoot Lee, K.; Mohd Radzol, A.R.; Mansor, W.; Amanina Yusoff, N. PCA-Polynomial-ELM Model Optimal for Detection of NS1 Adulterated Salivary SERS Spectra. J. Phys. Conf. Ser. 2019, 1372, 012064.
- Yang, Y.; Xu, B.; Haverstick, J.; Ibtehaz, N.; Muszyński, A.; Chen, X.; Chowdhury, M.E.H.; Zughaier, S.; Zhao, Y. Differentiation and Classification of Bacterial Endotoxins Based on Surface Enhanced Raman Scattering and Advanced Machine Learning. Nanoscale 2022, 14, 8806–8817.
More
Information
Subjects:
Optics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revisions:
2 times
(View History)
Update Date:
07 Mar 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





