Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Meg (Margaret) Anne Brownlow | -- | 1672 | 2023-02-17 01:34:31 | | | |
| 2 | Camila Xu | Meta information modification | 1672 | 2023-02-17 01:50:46 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Brownlow, M.; Mizzi, J.X. Exertional Heat Illness Pathophysiology in Thoroughbred Racehorses. Encyclopedia. Available online: https://encyclopedia.pub/entry/41319 (accessed on 07 February 2026).
Brownlow M, Mizzi JX. Exertional Heat Illness Pathophysiology in Thoroughbred Racehorses. Encyclopedia. Available at: https://encyclopedia.pub/entry/41319. Accessed February 07, 2026.
Brownlow, Meg, James Xavier Mizzi. "Exertional Heat Illness Pathophysiology in Thoroughbred Racehorses" Encyclopedia, https://encyclopedia.pub/entry/41319 (accessed February 07, 2026).
Brownlow, M., & Mizzi, J.X. (2023, February 17). Exertional Heat Illness Pathophysiology in Thoroughbred Racehorses. In Encyclopedia. https://encyclopedia.pub/entry/41319
Brownlow, Meg and James Xavier Mizzi. "Exertional Heat Illness Pathophysiology in Thoroughbred Racehorses." Encyclopedia. Web. 17 February, 2023.
Copy Citation
Exertional Heat Illness (EHI) occurs in all species where strenuous physical exertion takes place. It has been documented in human athletes, military personnel, firefighters and outdoor labourers, in racehorses and sporting horses, racing camels, and in working, sporting and even recreational dogs. The major symptoms of hyperthermia manifests as central nervous system (CNS) dysfunction which is typical across species, and EHI represents a significant welfare issue because it can cause significant morbidity and even fatality if allowed to progress untreated. The thoroughbred (TB) racehorse is at considerable risk because of the intensity of its exercise activity and its high rate of metabolic heat production.
exertional heat illness
thoroughbred racehorses
diagnosis of EHI
treatment EHI
1. Introduction
Strenuous exercise, especially during heat stress conditions, causes increases to metabolic heat production and a hyperthermic response, although the critical temperature at which EHI occurs tends to be inconsistent. In human subjects, experts are now recommending the presence of CNS dysfunction as the main diagnostic criterion to identify EHI [1] (p.1340). There are two suggested EHI/HS pathophysiological pathways, one due to hyperthermia and the other due to the initiation of inflammation,,various combinations of which may contribute to the clinical condition, depending upon the additional influences of environmental (extrinsic) risk factors and host (intrinsic) risk factors.
2. The Heat Toxicity Pathway
The direct effect of heat on cells is characterised by the denaturation of protein, causing irreversible damage. All cell components are affected, including the cytoskeleton, membranes, and nucleus, leading to decreases in cell viability and cell death. Thermal injury in general results in damage to vascular endothelium, initiating coagulopathies which can progress to cause widespread intravascular coagulation. A characteristic pathological finding is microthrombi deposition in the liver, lungs, heart, and kidney, creating widespread organ damage and ultimately multi-organ failure (MOF) [2] (Figure 1).
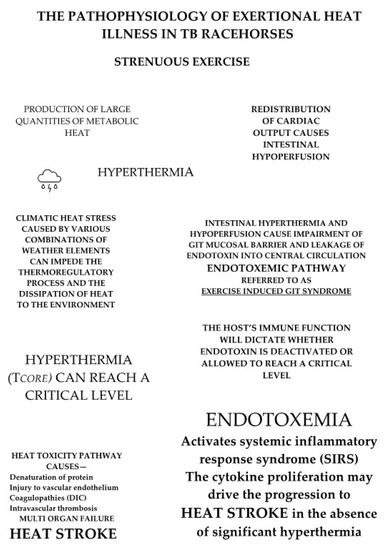
Figure 1. There are two proposed pathophysiological pathways for EHI. The strenuous exercise of racing produces a large amount of metabolic heat, most of which is stored, resulting in hyperthermia. If an individual’s ability to thermoregulate is impaired by high levels of heat and humidity, hyperthermia may reach critical levels. This can trigger the heat toxicity pathway, potentially leading to heat stroke with multi-organ failure. Strenuous exercise also causes a redistribution of cardiac output. Heat and intestinal hypoperfusion combine to cause impairment of the intestinal mucosal barrier, allowing leakage of endotoxin into the central circulation. Limitation of this endotoxemic or ‘heat sepsis’ pathway is dependent on the host’s immune system, which if functioning normally can deactivate endotoxin. If this does not occur, endotoxin can reach a critical level and may activate the systemic inflammatory response syndrome (SIRS), stimulating the production of cytokines, which might actually drive the condition and are thought to mediate many of the adverse consequences of the EHI/HS syndrome.
As previously stated, the degree of heat-related tissue damage is dependent upon temperature and time. If the time to reach a certain level of thermal injury is plotted as a function of temperature, a biphasic linear response is seen that has common slopes across all species and mortality endpoints. Thus, for most mammalian tissues the body temperature at which the curve changes slope is between 43.0 and 43.5 °C. According to Goldstein [3], 240 min at 42 °C causes the same level of thermal damage as 60 min. at 43 °C, 30 min. at 44 °C, or 15 min. at 45 °C. This has important ramifications for the management of affected individuals. Most racehorses compete, are cooled, and then left in their tie-up stalls for a period before being transported to their point of origin, which in Australia can sometimes be several hours away from the racetrack, and horse transporters are not always air conditioned. If a particular horse has not cooled adequately, it is quite possible that a temperature of 41.0 to 42.0 °C may persist for some hours and theoretically result in significant thermal damage to tissue at temperature levels not usually considered to be pathologically significant.
The traditional viewpoint is that all cases of EHI occur when horses or human athletes perform strenuous exercise in conditions of extreme heat/humidity. Clearly, a single overwhelming exposure is responsible for many cases, but a recent epidemiological study in TB racehorses in eastern Australia [4] revealed that environmental conditions were responsible for only 43% of the EHI cases recorded. This has significant implications for understanding EHI, suggesting that factors other than environmental ones may be involved, which might have compromised the individual’s ability to regulate heat strain and control the exercise-associated hyperthermic response.
3. The Endotoxemic or ‘Heat Sepsis’ Pathway
By itself, the heat toxicity pathway could not fully explain why in some instances the pathology associated with fatal heat stroke cases was more characteristic of sepsis, like that seen in acute bacterial infections. In 2002, clinical researchers Bouchama and Knochel [5] proposed that EHI/HS could be represented by another pathophysiology, which they termed the ‘heat sepsis’ or endotoxemic pathway. This was supported by others who experimentally showed in human subjects that strenuous exercise, especially under adverse environmental conditions, caused intestinal hypoperfusion and hypoxemia, disrupting the integrity of the mucosal gastrointestinal (GIT) barrier [6] and allowing endotoxins to gain access to the central circulation. It was suggested that under certain circumstances and particularly in cases of immune dysfunction, endotoxemia could reach critical levels and trigger a systemic inflammatory response syndrome (SIRS) characterized by cytokine proliferation, where the latter became the major driver for the progression of EHI. Importantly, within this description there was a lack of inclusion of a specific Tc value above which this occurred, reflecting the reports of substantial variability for temperature measurement in clinical cases [7].
In the last few decades this model of disease has become much more relevant, as has the importance of the entire GIT microbiome in maintaining mucosal integrity and overall gut health. Many researchers view the endotoxemic pathway as a probable major contributor to the pathophysiology of the EHI/HS disease complex in humans, referring to it as ‘the exercise-induced gastrointestinal syndrome’ (EIGS) [8][9]. When reviewing the literature in this area it becomes apparent that there are similarities between humans and horses in their physiological response to EHI and its clinical manifestations. In ponies, McConaghy [10] showed that there was an exercise-related decrease in intestinal blood flow, which was exacerbated by both heat and exercise intensity. Secondly, Baker [11] showed that when TBs raced there was an associated elevation in endotoxin levels and, as observed in human athletes, anti-endotoxin antibody was also present, functioning as a potential brake on its accumulation and thereby enabling heat tolerance. Finally, in another study, TB racehorses were exercised to absolute fatigue [12]. Endotoxin levels increased threefold at the point of fatigue and gradually decreased over the next two hours. Most importantly, however, it was noted that the exercise bout initiated a pro-inflammatory response with cytokine proliferation typical of that seen in human subjects with exertional heatstroke [5]. These results are indicators that a similar response to strenuous exercise may exist for TB racehorses, but further research is warranted. An important point is the extreme sensitivity of both the equine and human species to the effects of circulating endotoxin, and the similar cytokine proliferation responses in both experimental infusion models and naturally occurring clinical cases of endotoxemia [13].
From extensive field experience, the authors confirm that EHI in TB racehorses is often unpredictable, with frequent occurrences in cooler weather conditions, meaning that potentially, EHI can occur on any day that a racehorse performs strenuous exercise, a situation which does not conform to the heat-centred theory. There are also cases where horses exhibit a slow-to-cool response, creating questions about the underlying pathophysiology. If cooling modalities are optimal the clinical condition should be improving, but recently, Leon and Helwig [7] described HS cases in humans where rapid cooling initiatives and other resuscitative therapies were inadequate to prevent tissue injury. This was attributed to the heat-induced SIRS and its associated cytokine proliferation, rather than the direct effects of hyperthermia. Those authors [7], ascribed many of the adverse consequences of the HS syndrome to the peripheral and CNS actions of cytokines. EHI should therefore be regarded as a more complex medical disorder, in which the involvement of thermoregulatory and inflammatory pathways is sometimes mixed, and while hyperthermia may be the trigger, it may not always be the ultimate driver of the condition [1][7][8].
4. Central Nervous System Dysfunction Is a Common Feature in All EHI Clinical Cases and Should Be Considered the Main Diagnostic Criterion [1]
Sharma and Hoopes [14] have clarified the CNS pathophysiology of heat stroke in extensive studies using rodent and dog heat stroke models, and this provides the basis for understanding the earliest clinical signs and their corresponding CNS pathology, which is similar in most mammals (see Figure 2). Firstly, there is a hyperthermia-induced reduction in cerebral blood flow, leading to cerebral ischemia. In human subjects this is responsible for the earliest clinical signs, which are usually very vague and can include confusion, irritability, extreme restlessness, combativeness, and substantial headache. If the hyperthermia progresses, serotonin initiates an increase in permeability of the blood-brain barrier (BBB) which allows leakage of plasma proteins from cerebral capillaries, causing cerebral oedema [15].
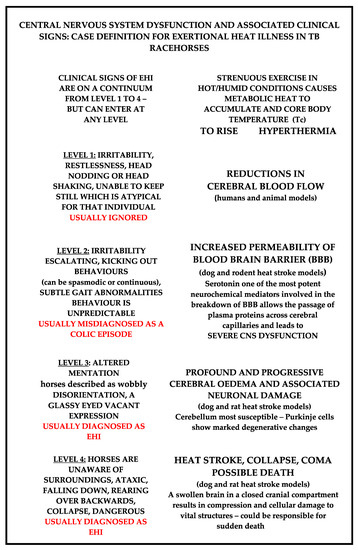
Figure 2. Case definition of EHI in TB racehorses and the postulated associated CNS pathology. Note that Levels 1 to 4 are on a continuum, but horses may enter at any level. Level 1 is the most important to recognise and is the most often misdiagnosed. Early recognition of EHI is essential because early treatment interventions enable the best outcomes [2][3][4][14][15][16][17].
Escalating CNS dysfunction ensues, and if treatment is delayed, may progress to an associated neuronal injury, specifically involving the cerebellum. This is followed by ‘heat stroke’ and involves profound clinical signs of CNS dysfunction. There is delirium and stupor, with individuals being unaware of their surroundings. End-stage HS is characterized by an oedematous, swollen, brain in a closed cranial compartment. This causes compression and cellular damage to vital structures, eventually resulting in collapse, loss of consciousness, coma, and ultimately death. Numerous researchers consider that elevated levels of CNS serotonin are the key driver in the hyperthermia-associated increase in permeability of the BBB, which leads directly to progressive cerebral oedema and neuronal injury, and possible coma and death [2][17].
References
- Laitano, O.; Leon, L.R.; Roberts, W.O.; Sawka, M.N. Controversies in exertional heat stroke diagnosis, prevention, and treatment. J. Appl. Physiol. 2019, 12, 1338–1348.
- Yaqub, B.; Deeb, A.I. Heat Stroke: Aetiopathogenesis, neurological characteristics, treatment and outcome. J. Neurolog. Sci. 1998, 156, 144–151.
- Goldstein, L.S.; Dewhurst, M.W.; Repracholi, M.; Kheifets, L. Summary, conclusions and recommendations: Adverse temperature levels in the human body. Internat. J. Hyper. 2003, 9, 373–384.
- Brownlow, M.A.; Brotherhood, J.R. An investigation into environmental variables Influencing post-race exertional heat illness in Thoroughbred racehorses in eastern Australia. Aust. Vet. J. 2021, 99, 433–481.
- Bouchama, A.; Knochel, J.P. Heat Stroke. N. Engl. J. Med. 2002, 346, 1978–1988.
- Lambert, G.P. Intestinal barrier dysfunction, endotoxemia and gastrointestinal symptoms: The canary in the coal mine during exercise-heat stress. In Thermoregulation and Human Performance. Physiological and Biological Aspects; Marino, F.E.S., Karger, A.G., Eds.; Karger: Basel Switzerland, 2008; pp. 61–73.
- Leon, L.R.; Helwig, B.G. Role of endotoxin and cytokines in the systemic inflammatory response to heat injury. Front. Biosci. 2010, S2, 916–938.
- Lim, C.L. Heat sepsis precedes heat toxicity in the pathophysiology of heat stroke—A new paradigm on an ancient disease. Antioxidants 2018, 7, 149–167.
- Costa, R.J.S.; Snipe, R.; Kitic, C.; Gibson, P.R. Systemic review: Exercise-induced gastrointestinal syndrome- implication for health and disease. Aliment. Pharmacol. Ther. 2017, 46, 246–265.
- McConaghy, F.F.; Hales, J.R.S.; Hodgson, D.R. Cardiovascular responses to heat and exercise in horses. Ann. N. Y. Acad. Sci. 1997, 813, 600–603.
- Baker, J.G.; Gaffin, S.L.; Wells, M.; Wessels, B.C.; Brock-Utne, J.G. 1988. Endotoxemia in racehorses following exertion. J. S. Afr. Vet. Assoc. 1977, 59, 63–68.
- Donovan, D.C.; Jackson, C.A.; Colahan, P.T.; Norton, N.; Hurley, D. Exercise-induced alterations in pro-inflammatory cytokines and prostaglandin F2alpha in horses. Vet. Immunol. Immunopathol. 2007, 18, 263–269.
- Barton, M.H. Rats Are Not People and People Are Not Horses: Comparative Aspects of Endotoxemia; ACVIM: Denver, CO, USA, 2008.
- Sharma, H.S.; Hoopes, P.J. Hyperthermia induced pathophysiology of the central nervous system. Intern. J. Hyper. 2003, 19, 325–354.
- Sharma, H.S. Hyperthermia induced brain oedema: Current status and future perspectives. Indian J. Med. Res. 2006, 5, 629–652.
- Brownlow, M.A.; Mizzi, X.A. Exertional Heat Illness in Thoroughbred Racehorses: Pathophysiology, case definition, treatment rationale. Equine Vet. Educ. 2021, 34, 259–271.
- Sharma, H.S. Hyperthermia influences excitatory and inhibitory amino acid neurotransmitters in the central nervous system. J. Neural Trans. 2006, 113, 497–519.
More
Information
Subjects:
Physiology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
656
Revisions:
2 times
(View History)
Update Date:
17 Feb 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




