Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ravindra Prasad Aharwal | -- | 2411 | 2023-02-16 08:41:47 | | | |
| 2 | Catherine Yang | Meta information modification | 2411 | 2023-02-16 08:54:18 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kumar, S.; Mathew, S.O.; Aharwal, R.P.; Tulli, H.S.; Mohan, C.D.; Sethi, G.; Ahn, K.; Webber, K.; Sandhu, S.S.; Bishayee, A. Pleiotropic Anticancer of Withaferin A. Encyclopedia. Available online: https://encyclopedia.pub/entry/41276 (accessed on 07 February 2026).
Kumar S, Mathew SO, Aharwal RP, Tulli HS, Mohan CD, Sethi G, et al. Pleiotropic Anticancer of Withaferin A. Encyclopedia. Available at: https://encyclopedia.pub/entry/41276. Accessed February 07, 2026.
Kumar, Suneel, Stephen O. Mathew, Ravindra Prasad Aharwal, Hardeep Singh Tulli, Chakrabhavi Dhananjaya Mohan, Gautam Sethi, Kwang-Seok Ahn, Kassidy Webber, Sardul Singh Sandhu, Anupam Bishayee. "Pleiotropic Anticancer of Withaferin A" Encyclopedia, https://encyclopedia.pub/entry/41276 (accessed February 07, 2026).
Kumar, S., Mathew, S.O., Aharwal, R.P., Tulli, H.S., Mohan, C.D., Sethi, G., Ahn, K., Webber, K., Sandhu, S.S., & Bishayee, A. (2023, February 16). Pleiotropic Anticancer of Withaferin A. In Encyclopedia. https://encyclopedia.pub/entry/41276
Kumar, Suneel, et al. "Pleiotropic Anticancer of Withaferin A." Encyclopedia. Web. 16 February, 2023.
Copy Citation
Withaferin A, a natural bioactive molecule isolated from the Indian medicinal plant Withania somnifera (L.) Dunal, has been reported to impart anticancer activities against various cancer cell lines and preclinical cancer models by modulating the expression and activity of different oncogenic proteins.
withaferin A
cancer
apoptosis
angiogenesis
chemoresistance
1. Structure of Withaferin A
The bioactive compound withaferin A is a steroidal lactone primarily extracted from W. somnifera, first isolated by Israeli chemists, Asher Lavie and David Yarden, in 1962 from the leaves of the plant. The inhibitory properties of the withaferin A molecule are due to the occurrence of an unsaturated lactone in a side chain; allylic 1° alcohol is attached at position 25 and the highly oxygenated rings A and B are attached to the other side of the compound [1][2][3][4][5]. Cytotoxicity is achieved by the presence of α,β-unsaturated carbonyl moiety of the withaferin A structure of thiol adducts [6]. Withaferin A structural studies revealed that the three positions susceptible to nucleophilic attack are the unsaturated A-ring at C3, the epoxide at position five, and C24 in the E ring (Figure 1). All these sites of withaferin A are covalently attached to the cysteine residues of protein by the Michael addition alkylation reaction, resulting in a loss of the activity of the target protein [7]. However, the C27 hydroxy group is not biologically important for withaferin A activity and can be conjugated with biotin so that it may recognize various target proteins [8][9]. Withaferin A was first isolated from the ether extract of Withania plant leaves and analyzed by thin-layer chromatography (TLC) and column chromatography. The initial extraction of withaferin A was performed by repeated column chromatography using the chloroform–methanol fraction of the W. somnifera extract and partial purification of the compound using TLC and high-performance liquid chromatography. In the end, nuclear magnetic resonance and Fourier transform infrared were used to characterize the product [10][11].
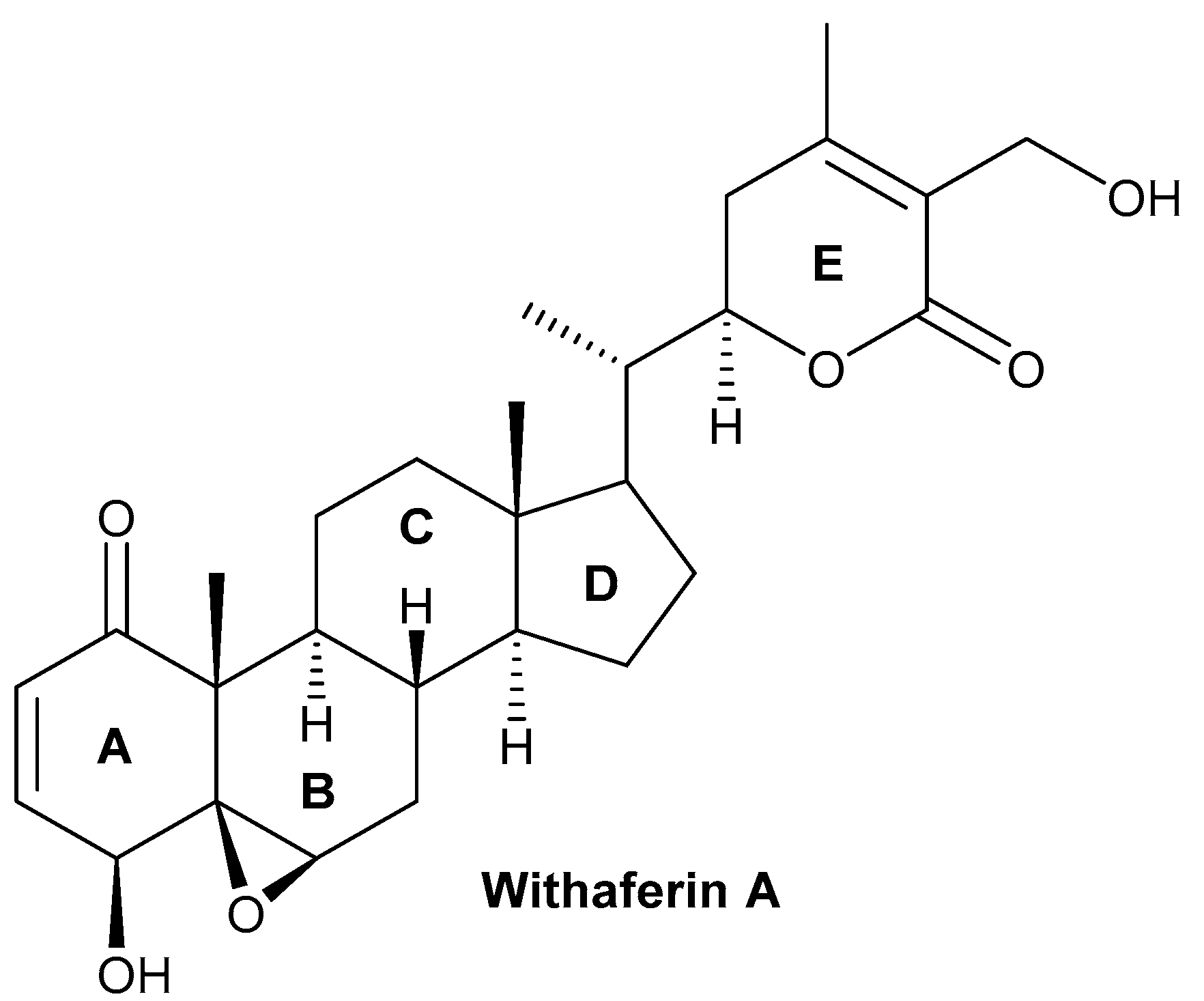
Figure 1. Chemical structure of withaferin A.
Moreover, withaferin A may also be extracted from the root of W. frutescens, a plant native to Europe with a high content of withaferin A in its leaves, which has shown a similar phytochemical profile to W. somnifera [12]. In another study, in vitro and in situ grown W. somnifera plants underwent morphological and phytochemical screening for the optimization of withaferin A extraction. The highest amount of withaferin A obtained under in vitro conditions was a concentration of 0.27 to 7.64 mg/g dry weight, while under in situ conditions the concentration was 8.06 to 36.31 mg/g dry weight [13]. The evaluation of structure–activity relationships in 56 withanolides using 2D and 3D coculture models revealed withanolide D (2) as a compound that has high antiproliferative activity against multiple myeloma [14].
2. Biosynthesis of Withanolides
Withaferin A contains five important chemical groups: an epoxide ring between carbons 5 and carbon 6, a hydroxyl group at carbon 27, a 6-membered lactone ring (E) with an α, a β-unsaturated carbonyl group, an α,β-unsaturated ketone group in ring A, and a secondary hydroxyl group at carbon 4. Several studies have shown that changing a few of the aforementioned chemical groups aids in the synthesis of bioactive semisynthetic analogs of withaferin A [15][16][17][18].
Various types of withanolides are synthesized through mevalonate and non-mevalonate routes often known as the isoprenoid pathway and a range of enzymes, such as cycloartenol synthase, (S)-2, 3-epoxysqualene mutase belongs to the 2–3 oxidosqualene cyclases (OCSs) gene family along with α-amyrin synthase (AAS), β-amyrin synthase (BAS), lupeol synthase (LS), and lanosterol synthase (LAS) [19][20]. Withanolides are formed biosynthetically by cycloartenol synthase (CAS). The cyclization of 2,3-oxidosqualene into cycloartenol by the enzyme CAS is a crucial step in the formation of all withanolides in W. somnifera plants. A step-by-step process that includes desaturation, hydroxylation, epoxidations, cyclization, chain elongation, and glycosylation, is preceded by cycloartenol molecules that serve as a precursor for the synthesis of withanolides. The biosynthesis of withanolides began with the cyclization of epoxysqualene to produce the triterpenoid compound C30H50O.
Plants contain various types of oxidosqualene cyclases that are essential for the synthesis of sterols and many types of triterpenoids from 2,3-oxidosqualene. In the first step of mevalonate pathways, the enzyme acetoacetyl (AcAc)-CoA thiolase is involved in the condensation of two acetyl CoA molecules into AcAc-CoA to form 3-hydroxy-3-methylglutaryl-coenzyme (HMG-CoA) [21]. In the second step, AcAc-CoA is condensed with one molecule of acetyl-CoA to form HMG-CoA with the help of an enzyme HMG-CoA synthase [22]. In the third step, a nicotinamide adenine dinucleotide (phosphate)-dependent (NAD(P)H) enzyme and HMG-CoA reductase biosynthesized mevalonate (MVA) from HMG-CoA (Benveniste, 2002). MVA is converted further into isopentyl pyrophosphate (IPP) via phosphorylation and decarboxylation, which are carried out by a series of enzymes, including MVA kinase, phosphomevalonate kinase, and MVA diphosphate decarboxylase. The IPP resulting from the cytosolic MVA pathway changes into dimethylallyl diphosphate (DMAPP) (Hunter, 2007). The IPP and DMAPP are further involved in the formation of farnesyl pyrophosphate (FPP), which is the main precursor for the synthesis of triterpenoids [23][24].
When withanolides are produced by the methylerythritol 4-phosphate (MEP) route, an enzyme 1-deoxy-D-xylulose 5-phosphate synthase converts the major substrates, pyruvate, and glyceraldehydes 3-phosphate, into 1-deoxy-D-xylulose 5-phosphate (DXP) [25][26]. In the next step, the DXP changes into the MEP and it further changes into the 1-hydroxy-2-methyl-2-€- butenyl 4-diphosphate, with the help of enzymes DXP reductoisomerase and successive action of other enzymes, such as 2-C-methyl-D-erythritol 4-phosphate cytidylyltransferase, 4-diphosphocytidyl-2-C-methyl-D-erythritol kinase, 2-C- methyl-D-erythritol 2,4-cyclodiphosphate synthase, and (E)-4-hydroxy-3-methylbut-2-enyl diphosphate synthase (HMBPP). The last step of this pathway involved the branching of HMBPP to IPP and DMAPP catalyzed by an enzyme, (E)-4-hydroxy-3-methyl but-2-enyl diphosphate reductase. The IPP further leads the development of the main precursor of FPP for triterpenoids biosynthesis [23][24]. The FPP reaction is promoted into the condensation of IPP with DMAPP to form 10-C intermediate geranyl diphosphate (GPP), and the condensation of GPP with IPP results in 15-C FPP [27]. Squalene, which is produced by the action of the enzyme squalene synthase, which catalyzed the condensation of two molecules of FPP in NADPH, is one of the most important molecules for the biosynthesis of triterpenoids. Now that the squalene has undergone epoxidation to create squalene 2,3,-epoxide, cycloartenol has been biosynthesized, and it has subsequently evolved into a range of different kinds of steroidal triterpenoidal compounds [27][28][29].
3. Anti-Inflammatory and Antioxidant Activities of Withaferin A
The uncontrolled regulation of various inflammatory markers, such as chemokines and cytokines, plays a key role in the inflammatory process [30][31][32][33][34][35]. Inflammation results in the release of many free radicals, including reactive oxygen species (ROS) and reactive nitrogen species (RNS), which cause oxidative stress and contribute to the development of various pathological conditions, such as atherosclerosis, cardiovascular disease, and cancer [36][37][38][39][40][41][42]. Cancer growth, progression, and chemotherapy treatment can all induce inflammation in cancer patients [43][44][45][46][47]. Therefore, as compared to synthetic drugs and formulations, natural bioactive metabolites that target different kinds of cancer may substantially alleviate side effects and offer new alternatives to the standard of care for cancer patients [48][49][50][51]. Currently, only a few bioactive compounds isolated from various natural sources have been tested clinically for cancer treatment, and one of these bioactive compounds, withaferin A, isolated from W. somnifera, has potential anticancer, anti-inflammatory, and antioxidant properties [52][53][54].
Withaferin A has shown cytotoxic properties against various cancers, such as leukemia, liver, oral, colon, pancreas, prostate, breast, ovarian, and bladder cancer [55][56]. The anti-inflammatory qualities of withaferin A are specifically attributed to its inhibition of pro-inflammatory molecules, α-2 macroglobulin, NF-κB, activator protein 1 (AP-1), and cyclooxygenase-2 (COX-2) inhibition, observed in various in vitro models [57]. Human and mouse islets treated with withaferin A demonstrated the inhibition of NF-ĸB signaling, preventing cytokine-induced death by reducing the secretion of cytokines, thereby effectively protecting the islet [58] (Figure 2).
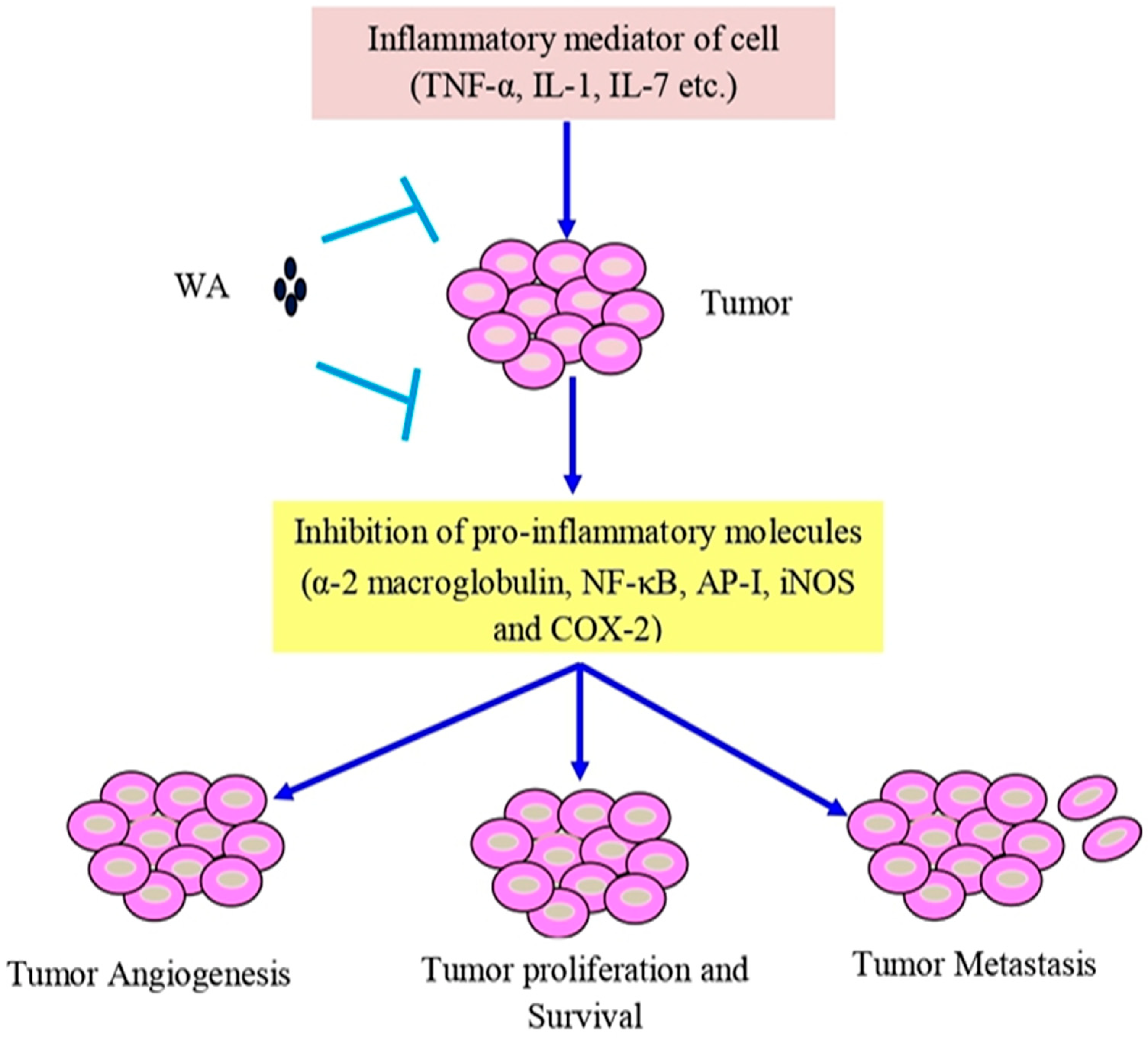
Figure 2. Withaferin A intercedes in anti-inflammatory function in tumor cells via TNF-α, IL-1, and IL-7. Abbreviations: IL-1, interleukin-1; IL-7, interleukin-7; and TNF-α, tumor necrosis factor-α.
In another study, it was observed that the activation of the Toll-like receptor 4 (TLR4) in spinal cord astrocytes triggers a signal flow that leads to the commencement of NF-ĸB, which further initiates the expression of TNF-α, COX-2, and inducible nitric oxide synthase (iNOS), and pro-inflammatory and stress-response moderators that may cause CNS disorders, such as neural cell death. However, withaferin A is highly effective in inhibiting the transcriptional activity of NF-ĸB and pro-inflammatory and stress-response mediators in astrocytes, exhibiting the potential for withaferin A to combat neurodegenerative disorders [59][60][61][62][63]. Other studies also revealed that withaferin A reduced NADPH oxidase as well as superoxide levels, which prevented the aging-induced neurodegeneration of the dopaminergic neurons in the brain of a rat model [64][65].
Withaferin A also acts as a key mediator in the prevention of inflammation during chronic kidney disease (CKD), seen in the unilateral urethral obstruction (UUO) renal injury animal model (unilateral obstruction). The levels of TGF-β and downstream signaling molecules p-Smad2, p-Smad3, total Smad4, p-Akt, and p-ERK were attenuated by withaferin A, showing strong evidence of the renoprotective potential of withaferin A due to its anti-inflammatory activity [66]. Withaferin A can also display antioxidant effects in liver fibrosis, by attenuating the BB-(PDGF-BB) platelet growth factor and promoting PDGF-BB-induced SIRT3 expression and action in the case of JS1 cells. It also prevented carbon tetrachloride (CCl4)-induced liver damage, fibrosis, and collagen deposition by increasing the sirtuin3 (SIRT3) expression and suppressing CCl4-induced oxidative stress in the fibrotic liver of C57/BL6 mice [67]. Studies have shown that withaferin A is capable of restoring the structure of the liver by increasing antioxidant action in hepatocarcinogenic rats by lowering the level of liver marker enzymes and reducing the oxidative stress of various oxidants [68]. Another study observed that withaferin-A activated LXR-α, which inhibits NF-κB transcriptional activity and suppresses the proliferation, invasion, migration, and anchorage-independent growth of hepatocellular carcinoma (HCC) cells, confirming withaferin A to be a potent anticancer compound that suppresses various angiogenesis and inflammatory markers linked to the development and progression of HCC.
Interestingly, low concentrations of withaferin A treatment for 24 h did not show cytotoxicity against Ca9–22 oral cancer cells, but did cause the release of ROS, wound healing, and the migration of cells. At the molecular level, withaferin A inhibits matrix metalloproteinase-2 (MMP-2) and MMP-9, but also provokes mRNA stimulation for a set of antioxidant genes, such as NADPH quinone dehydrogenase 1 (NQO1), glutathione-disulfide reductase (GSR), Nrf2, heme oxygenase 1 (HMOX1), and induced mild phosphorylation in the MAPK family, including extracellular signal-regulated kinases 1/2 (ERK1/2), c-Jun N-terminal kinase (JNK), and p38 expression in Ca9–22 cells. All these alterations were suppressed by the presence of the ROS scavenger N-acetylcysteine (NAC), suggesting that low concentrations of withaferin A can maintain potent ROS-mediated antimigration and invasion capabilities of oropharyngeal squamous cancer cells [69]. Withaferin A improved the ability of H9c2 cells to survive against simulated ischemia/reperfusion (SI/R) or hydrogen peroxide (H2O2)-induced cell death in a cardiac ischemia-reperfusion injury model. Withaferin A triggered the upregulation of superoxide dismutase SOD2, SOD3, and peroxiredoxin 1(Prdx-1). Additionally, withaferin A inhibited the H2O2-induced upregulation of SOD2, SOD3, and Prdx-1, and ameliorated cardiomyocyte caspase-3 activity via an Akt-dependent pathway [70].
Chaudhary et al. [71] reported that an overproduction of ROS accelerated by withaferin A was responsible for the inhibition of the cell cycle in CRC cells and that it decreased the potential of the mitochondrial membrane, causing mitochondrial dysfunction. Withaferin A promoted radiation-induced apoptosis in human kidney carcinoma (Caki) cells by producing reactive oxygen species and inhibiting Bcl-2 and Akt dephosphorylation [72]. Withaferin A, in combination with doxorubicin (DOX), is also responsible for the excessive generation of ROS that can cause concentration-dependent DNA damage and stimulate autophagy in an ovarian cancer cell line (Figure 3). The histochemical observation of tumor tissues treated with withaferin A and DOX showed a reduction in the cell proliferation and micro-vessel development, an increase in light chain 3β (LC3B) levels, DNA destruction, and the cleavage of caspase-3 [73][74][75].
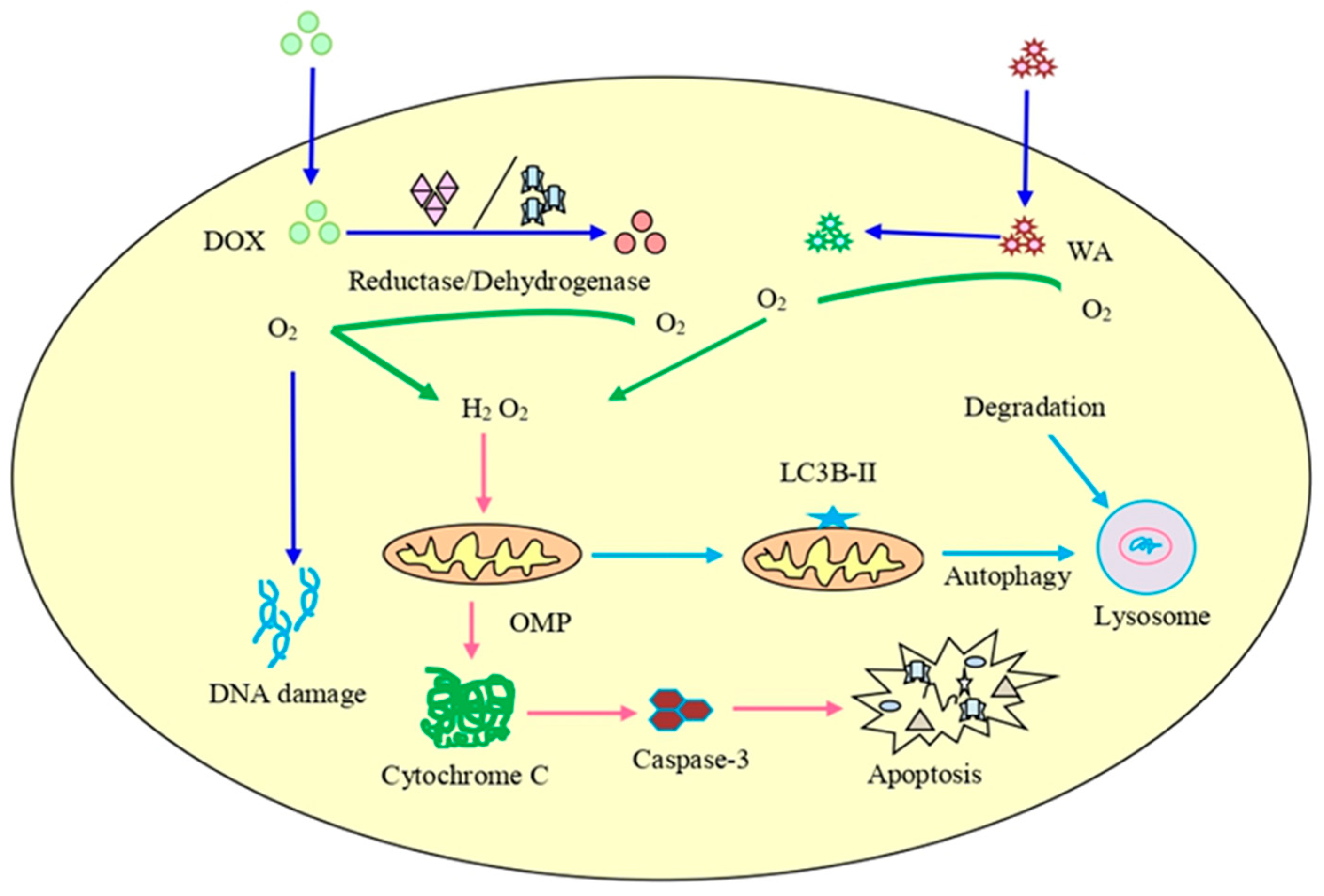
Figure 3. The combined treatment of doxorubicin (DOX) and withaferin A on cancer cells. It can lead to enhanced ROS production, destruction of DNA, initiation of autophagy, and increased expression of LC3B autophagy marker as well as cleavage of caspase-3.
4. Safety and Toxicity of Withaferin A
During the review of the bioactive compound withaferin A, it was recognized that one of its most important attributes is its safety for normal cells and tissues, which allows for the continuation of this drug in clinical trials. In an in vivo study, W. somnifera extract containing withaferin A was orally administered to Wistar rats at a dose of 2000 mg/kg/day and had no adverse effects on the animals [76]. Moreover, withaferin A is also responsible for the reduction of acetaminophen-induced liver toxicity in mice through the stress-responsive transcription factor Nrf2. Similarly, another study found that withaferin A increased the expression of SIRT3 and suppressed CCl4-induced oxidative stress in the fibrotic liver of a C57/BL6 mice model, assisting in reduced liver injury, collagen deposition, and fibrosis caused by CCl4 [67]. Withaferin A was also shown to decrease severe cerulein-induced pancreatitis caused by inflammation and oxidative stress. The treatment of scleroderma with withaferin A initiated antifibrotic activity, which was repressed by the proinflammatory fibrosis related to TGF-β/Smad signaling and the FOXO3a-Akt-dependent NF-κβ/IKK-mediated inflammatory mechanism [77][78][79][80][81]. In addition, withaferin A has also exerted potential cytotoxicity effects at a low range (up to 5 μM) in melanoma cells, as compared to non-malignant cells [82]. Withaferin A significantly inhibited the burden of breast cancer in two different subtypes, HER2-driven breast cancer, and luminal-type breast cancer-bearing rodent models, when administered through the intraperitoneal route [83]. Most of the findings related to the general safety of withaferin A support the pharmacological and pharmaceutical studies of this natural bioactive compound. However, more research and pharmacokinetic studies of withaferin A and its derivatives are required for the development of chemotherapeutic drugs in the future.
5. Clinical Studies of Withaferin A
Based on impressive preclinical results, the potential of withaferin to treat a wide range of disorders is significant. However, presently there is only one ongoing clinical trial to examine the efficacy of withaferin A in cancer patients. A phase-I/II clinical trial is initiated in which the combination of DOXIL and withaferin A is examined in patients with recurrent ovarian cancer. This study aims to determine the feasibility and maximum tolerance dose of withaferin A with DOXIL and to examine the complete response, partial response, and stable disease (NCT05610735). Although there is a huge amount of preclinical data available on the anticancer potential of withaferin A, these studies are yet to substantiate its antitumor efficacy in the clinical setting. Therefore, withaferin A needs to be investigated rigorously in randomized controlled trials to understand its therapeutic efficacy against human malignancies.
References
- Motiwala, H.F.; Bazzill, J.; Samadi, A.; Zhang, H.; Timmermann, B.N.; Cohen, M.S.; Aubé, J. Synthesis and cytotoxicity of semisynthetic Withalongolide A analogues. ACS Med. Chem. Lett. 2013, 4, 1069–1073.
- Budhiraja, R.D.; Krishan, P.; Sudhir, S. Biological activity of withanolides. J. Sci. Ind. Res. 2000, 59, 904–911.
- Fuska, J.; Proska, B.; Williamson, J.; Rosazza, J.P. Microbiological and chemical dehydrogenation of withaferin A. Folia Microbiol. 1987, 32, 112–115.
- Fuska, J.; Fusková, A.; Rosazza, J.P.; Nicholas, A.W. Novel cytotoxic and antitumor agents. IV. Withaferin A: Relation of its structure to the in vitro cytotoxic effects on P388 cells. Neoplasma 1984, 31, 31–36.
- Singh, A.; Raza, A.; Amin, S.; Damodaran, C.; Sharma, A.K. Recent Advances in the chemistry and therapeutic evaluation of naturally occurring and synthetic Withanolides. Molecules 2022, 27, 886.
- Santagata, S.; Xu, Y.M.; Wijeratne, E.M.; Kontnik, R.; Rooney, C.; Perley, C.C.; Kwon, H.; Clardy, J.; Kesari, S.; Whitesell, L.; et al. Using the heat-shock response to discover anticancer compounds that target protein homeostasis. ACS Chem. Biol. 2012, 7, 340–349.
- Vanden Berghe, W.; Sabbe, L.; Kaileh, M.; Haegeman, G.; Heyninck, K. Molecular insight in the multifunctional activities of Withaferin A. Biochem. Pharmacol. 2012, 84, 1282–1291.
- Yokota, Y.; Bargagna-Mohan, P.; Ravindranath, P.P.; Kim, K.B.; Mohan, R. Development of withaferin A analogs as probes of angiogenesis. Bioorg. Med. Chem. Lett. 2006, 16, 2603–2607.
- Dom, M.; Offner, F.; Vanden Berghe, W.; Van Ostade, X. Proteomic characterization of Withaferin A-targeted protein networks for the treatment of monoclonal myeloma gammopathies. J. Proteomics 2018, 179, 17–29.
- Madhu, S.; Komala, M.; Pandian, P. Isolation and identification of Withaferin A (Steroidal Lactone) from Withania somnifera (Ashwagandha). Drug Invent. Today 2019, 11, 595–600.
- Meena, A.K.; Rekha, P.; Perumal, A.; Gokul, M.; Swathi, K.N.; Ilavarasan, R. Estimation of Withaferin-A by HPLC and standardization of the Ashwagandhadi lehyam formulation. Heliyon 2021, 7, e06116.
- Zomborszki, Z.P.; Peschel, W.; Boros, K.; Hohmann, J.; Dezső, C. Development of an optimized processing method for Withania frutescens. Acta Aliment. 2016, 45, 452–456.
- Johny, L.; Conlan, X.; Cahill, D.; Adholeya, A. In vitro and in situ screening systems for morphological and phytochemical analysis of Withania somnifera germplasms. Plant Cell Tissue Organ Cult. (PCTOC) 2015, 120, 1191–1202.
- Freitas Misakyan, M.F.; Wijeratne, E.M.K.; Issa, M.E.; Xu, Y.M.; Monteillier, A.; Gunatilaka, A.A.L.; Cuendet, M. Structure-activity relationships of withanolides as antiproliferative agents for multiple myeloma: Comparison of activity in 2D models and a 3D coculture model. J. Nat. Prod. 2021, 84, 2321–2335.
- Bharitkar, Y.P.; Kanhar, S.; Suneel, N.; Mondal, S.K.; Hazra, A.; Mondal, N.B. Chemistry of withaferin-A: Chemo, regio, and stereoselective synthesis of novel spiro-pyrrolizidino-oxindole adducts of withaferin-A via one-pot three-component azomethine ylide cycloaddition and their cytotoxicity evaluation. Mol. Divers. 2015, 19, 251–261.
- Hirayama, M.; Gamoh, K.; Ikekawa, N. Stereoselective synthesis of withafein A and 27-deoxywithaferin A1. Tetrahedron Letters 1982, 23, 4725–4728.
- Joshi, P.; Misra, L.; Siddique, A.A.; Srivastava, M.; Kumar, S.; Darokar, M.P. Epoxide group relationship with cytotoxicity in withanolide derivatives from Withania somnifera. Steroids 2014, 79, 19–27.
- Misra, L.; Lal, P.; Chaurasia, N.D.; Sangwan, R.S.; Sinha, S.; Tuli, R. Selective reactivity of 2-mercaptoethanol with 5β, 6β-epoxide in steroids from Withania somnifera. Steroids 2008, 73, 245–251.
- Gas-Pascual, E.; Berna, A.; Bach, T.J.; Schaller, H. Plant oxidosqualene metabolism: Cycloartenol synthase–dependent sterol biosynthesis in Nicotiana benthamiana. PLoS ONE 2014, 9, e109156.
- Xue, Z.; Duan, L.; Liu, D.; Guo, J.; Ge, S.; Dicks, J.; ÓMáille, P.; Osbourn, A.; Qi, X. Divergent evolution of oxidosqualene cyclases in plants. New Phytol. 2012, 193, 1022–1038.
- Vranová, E.; Coman, D.; Gruissem, W. Network analysis of the MVA and MEP pathways for isoprenoid synthesis. Annu. Rev. Plant Biol. 2013, 64, 665–700.
- Nagegowda, D.A.; Bach, T.J.; Chye, M.-L. Brassica juncea 3-hydroxy-3-methylglutaryl (HMG)-CoA synthase 1: Expression and characterization of recombinant wild-type and mutant enzymes. Biochem. J. 2004, 383, 517–527.
- Kuzuyama, T. Mevalonate and nonmevalonate pathways for the biosynthesis of isoprene units. Biosci. Biotechnol. Biochem. 2002, 66, 1619–1627.
- Chaurasiya, N.D.; Sangwan, N.S.; Sabir, F.; Misra, L.; Sangwan, R.S. Withanolide biosynthesis recruits both mevalonate and DOXP pathways of isoprenogenesis in Ashwagandha Withania somnifera L. (Dunal). Plant Cell Rep. 2012, 31, 1889–1897.
- Sprenger, G.A.; Schörken, U.; Wiegert, T.; Grolle, S.; De Graaf, A.A.; Taylor, S.V.; Begley, T.P.; Bringer-Meyer, S.; Sahm, H. Identification of a thiamin-dependent synthase in Escherichia coli required for the formation of the 1-deoxy-D-xylulose 5-phosphate precursor to isoprenoids, thiamin, and pyridoxol. Proc. Natl. Acad. Sci. USA 1997, 94, 12857–12862.
- Cordoba, E.; Salmi, M.; León, P. Unravelling the regulatory mechanisms that modulate the MEP pathway in higher plants. J. Exp. Bot. 2009, 60, 2933–2943.
- Ohnuma, S.-i.; Narita, K.; Nakazawa, T.; Ishida, C.; Takeuchi, Y.; Ohto, C.; Nishino, T. A role of the amino acid residue located on the fifth position before the first aspartate-rich motif of farnesyl diphosphate synthase on determination of the final product. J. Biol. Chem. 1996, 271, 30748–30754.
- Zhao, Z.-J.; Song, Y.-G.; Liu, Y.-L.; Qiao, M.; Zhai, X.-L.; Xiang, F.-N. The effect of elicitors on oleanolic acid accumulation and expression of triterpenoid synthesis genes in Gentiana straminea. Biol. Plant. 2013, 57, 139–143.
- Dhar, N.; Razdan, S.; Rana, S.; Bhat, W.W.; Vishwakarma, R.; Lattoo, S.K. A decade of molecular understanding of withanolide biosynthesis and in vitro studies in Withania somnifera (L.) Dunal: Prospects and perspectives for pathway engineering. Front. Plant Sci. 2015, 6, 1031.
- Shukla, S.; Shukla, H.; Kumar, S.; Aharwal, R.P.; Gupta, V.K.; Sandhu, S.S. Allergy and inflammation: An immunological and therapeutic approach. Recent Pat. Inflamm. Allergy Drug Discov. 2013, 7, 135–150.
- Shin, E.M.; Hay, H.S.; Lee, M.H.; Goh, J.N.; Tan, T.Z.; Sen, Y.P.; Lim, S.W.; Yousef, E.M.; Ong, H.T.; Thike, A.A.; et al. DEAD-box helicase DP103 defines metastatic potential of human breast cancers. J. Clin. Investig. 2014, 124, 3807–3824.
- Mastron, J.K.; Siveen, K.S.; Sethi, G.; Bishayee, A. Silymarin and hepatocellular carcinoma: A systematic, comprehensive, and critical review. Anticancer Drugs 2015, 26, 475–486.
- Raghunath, A.; Sundarraj, K.; Arfuso, F.; Sethi, G.; Perumal, E. Dysregulation of Nrf2 in hepatocellular carcinoma: Role in cancer progression and chemoresistance. Cancers 2018, 10, 481.
- Deldar Abad Paskeh, M.; Asadi, S.; Zabolian, A.; Saleki, H.; Khoshbakht, M.A.; Sabet, S.; Naghdi, M.J.; Hashemi, M.; Hushmandi, K.; Ashrafizadeh, M.; et al. Targeting cancer stem cells by dietary agents: An important therapeutic strategy against human malignancies. Int. J. Mol. Sci. 2021, 22, 11669.
- Ma, Z.; Wang, Y.Y.; Xin, H.W.; Wang, L.; Arfuso, F.; Dharmarajan, A.; Kumar, A.P.; Wang, H.; Tang, F.R.; Warrier, S.; et al. The expanding roles of long non-coding RNAs in the regulation of cancer stem cells. Int. J. Biochem. Cell Biol. 2019, 108, 17–20.
- Choudhury, B.; Kandimalla, R.; Elancheran, R.; Bharali, R.; Kotoky, J. Garcinia morella fruit, a promising source of antioxidant and anti-inflammatory agents induces breast cancer cell death via triggering apoptotic pathway. Biomed Pharmacother. 2018, 103, 562–573.
- Aggarwal, V.; Tuli, H.S.; Thakral, F.; Singhal, P.; Aggarwal, D.; Srivastava, S.; Pandey, A.; Sak, K.; Varol, M.; Khan, M.A.; et al. Molecular mechanisms of action of hesperidin in cancer: Recent trends and advancements. Exp. Biol. Med. 2020, 245, 486–497.
- Aggarwal, S.; Das, S.N. Garcinol inhibits tumour cell proliferation, angiogenesis, cell cycle progression and induces apoptosis via NF-κB inhibition in oral cancer. Tumor Biol. 2016, 37, 7175–7184.
- Morgan, D.; Garg, M.; Tergaonkar, V.; Tan, S.Y.; Sethi, G. Pharmacological significance of the non-canonical NF-κB pathway in tumorigenesis. Biochim. Biophys. Acta Rev. Cancer 2020, 1874, 188449.
- Ong, P.S.; Wang, L.Z.; Dai, X.; Tseng, S.H.; Loo, S.J.; Sethi, G. Judicious toggling of mTOR activity to combat insulin resistance and cancer: Current evidence and perspectives. Front. Pharmacol. 2016, 7, 395.
- Mirzaei, S.; Saghari, S.; Bassiri, F.; Raesi, R.; Zarrabi, A.; Hushmandi, K.; Sethi, G.; Tergaonkar, V. NF-κB as a regulator of cancer metastasis and therapy response: A focus on epithelial-mesenchymal transition. J. Cell Physiol. 2022, 237, 2770–2795.
- Banik, K.; Harsha, C.; Bordoloi, D.; Lalduhsaki Sailo, B.; Sethi, G.; Leong, H.C.; Arfuso, F.; Mishra, S.; Wang, L.; Kumar, A.P.; et al. Therapeutic potential of gambogic acid, a caged xanthone, to target cancer. Cancer Lett. 2018, 416, 75–86.
- Ghate, N.B.; Chaudhuri, D.; Das, A.; Panja, S.; Mandal, N. An Antioxidant extract of the insectivorous plant drosera burmannii vahl. Alleviates iron-induced oxidative stress and hepatic injury in mice. PLoS ONE 2015, 10, e0128221.
- Lee, J.H.; Kim, C.; Kim, S.H.; Sethi, G.; Ahn, K.S. Farnesol inhibits tumor growth and enhances the anticancer effects of bortezomib in multiple myeloma xenograft mouse model through the modulation of STAT3 signaling pathway. Cancer Lett. 2015, 360, 280–293.
- Behl, T.; Sharma, A.; Sharma, L.; Sehgal, A.; Zengin, G.; Brata, R.; Fratila, O.; Bungau, S. Exploring the multifaceted therapeutic potential of Withaferin A and its derivatives. Biomedicines 2020, 8, 571.
- Ranaware, A.M.; Banik, K.; Deshpande, V.; Padmavathi, G.; Roy, N.K.; Sethi, G.; Fan, L.; Kumar, A.P.; Kunnumakkara, A.B. Magnolol: A Neolignan from the Magnolia Family for the Prevention and Treatment of Cancer. Int. J. Mol. Sci. 2018, 19, 2362.
- Khwairakpam, A.D.; Bordoloi, D.; Thakur, K.K.; Monisha, J.; Arfuso, F.; Sethi, G.; Mishra, S.; Kumar, A.P.; Kunnumakkara, A.B. Possible use of Punica granatum (Pomegranate) in cancer therapy. Pharmacol. Res. 2018, 133, 53–64.
- Rayburn, E.R.; Ezell, S.J.; Zhang, R. Anti-inflammatory agents for cancer therapy. Mol. Cell Pharmacol. 2009, 1, 29–43.
- Sailo, B.L.; Banik, K.; Girisa, S.; Bordoloi, D.; Fan, L.; Halim, C.E.; Wang, H.; Kumar, A.P.; Zheng, D.; Mao, X. FBXW7 in cancer: What has been unraveled thus far? Cancers 2019, 11, 246.
- Ashrafizadeh, M.; Zarrabi, A.; Mostafavi, E.; Aref, A.R.; Sethi, G.; Wang, L.; Tergaonkar, V. Non-coding RNA-based regulation of inflammation. Semin. Immunol. 2022, 59, 101606.
- Roy, N.K.; Deka, A.; Bordoloi, D.; Mishra, S.; Kumar, A.P.; Sethi, G.; Kunnumakkara, A.B. The potential role of boswellic acids in cancer prevention and treatment. Cancer Lett. 2016, 377, 74–86.
- Batumalaie, K.; Amin, M.A.; Murugan, D.D.; Sattar, M.Z.; Abdullah, N.A. Withaferin A protects against palmitic acid-induced endothelial insulin resistance and dysfunction through suppression of oxidative stress and inflammation. Sci. Rep. 2016, 6, 27236.
- Choi, J.I.; Lee, S.G.; Han, S.J.; Cho, M.; Lee, P.C. Effect of gamma irradiation on the structure of fucoidan. Radiat. Phys. Chem. 2014, 100, 54–58.
- Dubey, S.; Yoon, H.; Cohen, M.S.; Nagarkatti, P.; Nagarkatti, M.; Karan, D. Withaferin A associated differential regulation of inflammatory cytokines. Front. Immunol. 2018, 9, 195.
- Chien, T.M.; Wu, K.H.; Chuang, Y.T.; Yeh, Y.C.; Wang, H.R.; Yeh, B.W.; Yen, C.H.; Yu, T.J.; Wu, W.J.; Chang, H.W. Withaferin A triggers apoptosis and DNA damage in bladder cancer J82 cells through oxidative stress. Antioxidants 2021, 10, 1063.
- Shin, J.A.; Kim, L.H.; Ryu, M.H.; Choi, S.Y.; Jin, B.; Lee, W.; Jung, Y.C.; Ahn, C.H.; Ahn, M.H.; Hong, K.O.; et al. Withaferin A mitigates metastatic traits in human oral squamous cell carcinoma caused by aberrant claudin-1 expression. Cell Biol. Toxicol. 2022, 38, 147–165.
- Braun, L.; Cohen, M. Herbs and Natural Supplements: An Evidence-Based Guide, 4th ed.; Elsevier Health Sciences: Sydney, Australia; Churchill Livingstone: London, UK, 2015.
- Baker, D.J.; Wijshake, T.; Tchkonia, T.; LeBrasseur, N.K.; Childs, B.G.; van de Sluis, B.; Kirkland, J.L.; van Deursen, J.M. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 2011, 479, 232–236.
- Brambilla, R.; Bracchi-Ricard, V.; Hu, W.H.; Frydel, B.; Bramwell, A.; Karmally, S.; Green, E.J.; Bethea, J.R. Inhibition of astroglial nuclear factor kappaB reduces inflammation and improves functional recovery after spinal cord injury. J. Exp. Med. 2005, 202, 145–156.
- Brambilla, R.; Persaud, T.; Hu, X.; Karmally, S.; Shestopalov, V.I.; Dvoriantchikova, G.; Ivanov, D.; Nathanson, L.; Barnum, S.R.; Bethea, J.R. Transgenic inhibition of astroglial NF-kappa B improves functional outcome in experimental autoimmune encephalomyelitis by suppressing chronic central nervous system inflammation. J. Immunol. 2009, 182, 2628–2640.
- Brambilla, R.; Dvoriantchikova, G.; Barakat, D.; Ivanov, D.; Bethea, J.R.; Shestopalov, V.I. Transgenic inhibition of astroglial NF-κB protects from optic nerve damage and retinal ganglion cell loss in experimental optic neuritis. J. Neuroinflammation 2012, 9, 213.
- Fu, E.S.; Zhang, Y.P.; Sagen, J.; Candiotti, K.A.; Morton, P.D.; Liebl, D.J.; Bethea, J.R.; Brambilla, R. Transgenic inhibition of glial NF-kappa B reduces pain behavior and inflammation after peripheral nerve injury. Pain 2010, 148, 509–518.
- Martorana, F.; Guidotti, G.; Brambilla, L.; Rossi, D. Withaferin A inhibits nuclear factor-κB-dependent pro-inflammatory and stress response pathways in the astrocytes. Neural Plast. 2015, 2015, 381964.
- Banu, M.R.; Ibrahim, M.; Prabu, K.; Rajasankar, S. Anti-inflammatory effect of withaferin A on dopaminergic neuron of aged rat. Drug Invent. Today 2019, 12, 2352–2355.
- Dom, M.; Vanden Berghe, W.; Van Ostade, X. Broad-spectrum antitumor properties of Withaferin A: A proteomic perspective. RSC Med. Chem. 2020, 11, 30–50.
- Peddakkulappagari, C.S.; Saifi, M.A.; Khurana, A.; Anchi, P.; Singh, M.; Godugu, C. Withaferin A ameliorates renal injury due to its potent effect on inflammatory signaling. Biofactors 2019, 45, 750–762.
- Gu, J.; Chen, C.; Wang, J.; Chen, T.; Yao, W.; Yan, T.; Liu, Z. Withaferin A exerts preventive effect on liver fibrosis through oxidative stress inhibition in a sirtuin 3-dependent manner. Oxid. Med. Cell Longev. 2020, 2020, 2452848.
- Murugan, S.; Ameesh, M.; Ekambaram, G.; Devaraja, R.; Sundaram, R.; Ashok, V.K.; Shilpa, S.; Sakthisekaran, D. Isolation of WithaferinA from Withania somnifera plant root and its effects on cancer rats. Int. J. Recent Trends Sci. Technol. 2015, 15, 463–472.
- Yu, T.J.; Tang, J.Y.; Ou-Yang, F.; Wang, Y.Y.; Yuan, S.F.; Tseng, K.; Lin, L.C.; Chang, H.W. Low concentration of withaferin a inhibits oxidative stress-mediated migration and invasion in oral cancer cells. Biomolecules 2020, 10, 777.
- Yan, Z.; Guo, R.; Gan, L.; Lau, W.B.; Cao, X.; Zhao, J.; Ma, X.; Christopher, T.A.; Lopez, B.L.; Wang, Y. Withaferin A inhibits apoptosis via activated Akt-mediated inhibition of oxidative stress. Life Sci. 2018, 211, 91–101.
- Chaudhary, A.; Kalra, R.S.; Malik, V.; Katiyar, S.P.; Sundar, D.; Kaul, S.C.; Wadhwa, R. 2, 3-Dihydro-3β-methoxy Withaferin-A lacks anti-metastasis potency: Bioinformatics and experimental evidences. Sci. Rep. 2019, 9, 17344.
- Yang, E.S.; Choi, M.J.; Kim, J.H.; Choi, K.S.; Kwon, T.K. Withaferin A enhances radiation-induced apoptosis in Caki cells through induction of reactive oxygen species, Bcl-2 downregulation and Akt inhibition. Chem. Biol. Interact. 2011, 190, 9–15.
- Sethi, G.; Ahn, K.S.; Sandur, S.K.; Lin, X.; Chaturvedi, M.M.; Aggarwal, B.B. Indirubin enhances tumor necrosis factor-induced apoptosis through modulation of nuclear factor-kappa B signaling pathway. J. Biol. Chem. 2006, 281, 23425–23435.
- Cheng, J.T.; Wang, L.; Wang, H.; Tang, F.R.; Cai, W.Q.; Sethi, G.; Xin, H.W.; Ma, Z. Insights into biological role of LncRNAs in epithelial-mesenchymal transition. Cells 2019, 8, 1178.
- Nair, A.S.; Shishodia, S.; Ahn, K.S.; Kunnumakkara, A.B.; Sethi, G.; Aggarwal, B.B. Deguelin, an Akt inhibitor, suppresses IkappaBα kinase activation leading to suppression of NF-κB-regulated gene expression, potentiation of apoptosis, and inhibition of cellular invasion. J. Immunol. 2006, 177, 5612–5622.
- Patel, S.B.; Rao, N.J.; Hingorani, L.L. Safety assessment of Withania somnifera extract standardized for Withaferin A: Acute and sub-acute toxicity study. J. Ayurveda Integr. Med. 2016, 7, 30–37.
- Vedi, M.; Sabina, E.P. Assessment of hepatoprotective and nephroprotective potential of withaferin A on bromobenzene-induced injury in Swiss albino mice: Possible involvement of mitochondrial dysfunction and inflammation. Cell Biol. Toxicol. 2016, 32, 373–390.
- Palliyaguru, D.L.; Chartoumpekis, D.V.; Wakabayashi, N.; Skoko, J.J.; Yagishita, Y.; Singh, S.V.; Kensler, T.W. Withaferin A induces Nrf2-dependent protection against liver injury: Role of Keap1-independent mechanisms. Free Radic. Biol. Med. 2016, 101, 116–128.
- Tiruveedi, V.L.; Bale, S.; Khurana, A.; Godugu, C. Withaferin A, a novel compound of Indian ginseng (Withania somnifera), ameliorates Cerulein-induced acute pancreatitis: Possible role of oxidative stress and inflammation. Phytother. Res. 2018, 32, 2586–2596.
- Anwar, M.F.; Yadav, D.; Rastogi, S.; Arora, I.; Khar, R.K.; Chander, J.; Samim, M. Modulation of liver and kidney toxicity by herb Withania somnifera for silver nanoparticles: A novel approach for harmonizing between safety and use of nanoparticles. Protoplasma 2015, 252, 547–558.
- Biswal, B.M.; Sulaiman, S.A.; Ismail, H.C.; Zakaria, H.; Musa, K.I. Effect of Withania somnifera (Ashwagandha) on the development of chemotherapy-induced fatigue and quality of life in breast cancer patients. Integr. Cancer Ther. 2013, 12, 312–322.
- Nagy, Z.; Cheung, B.B.; Tsang, W.; Tan, O.; Herath, M.; Ciampa, O.C.; Shadma, F.; Carter, D.R.; Marshall, G.M. Withaferin A activates TRIM16 for its anti-cancer activity in melanoma. Sci. Rep. 2020, 10, 19724.
- Samanta, S.K.; Sehrawat, A.; Kim, S.H.; Hahm, E.R.; Shuai, Y.; Roy, R.; Pore, S.K.; Singh, K.B.; Christner, S.M.; Beumer, J.H.; et al. Disease subtype-independent biomarkers of breast cancer chemoprevention by the ayurvedic medicine phytochemical Withaferin A. J. Natl. Cancer Inst. 2017, 109, djw293.
More
Information
Subjects:
Biochemistry & Molecular Biology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.6K
Entry Collection:
Biopharmaceuticals Technology
Revisions:
2 times
(View History)
Update Date:
16 Feb 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




