Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Chan Huang | -- | 1791 | 2023-02-09 02:30:08 | | | |
| 2 | Catherine Yang | Meta information modification | 1791 | 2023-02-09 02:32:27 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Huang, C.; Yuan, W.; Chen, J.; Wu, L.; You, T. The Application of Smart Biomaterials in Diabetic Wounds. Encyclopedia. Available online: https://encyclopedia.pub/entry/41007 (accessed on 01 March 2026).
Huang C, Yuan W, Chen J, Wu L, You T. The Application of Smart Biomaterials in Diabetic Wounds. Encyclopedia. Available at: https://encyclopedia.pub/entry/41007. Accessed March 01, 2026.
Huang, Chan, Weiyan Yuan, Jun Chen, Lin-Ping Wu, Tianhui You. "The Application of Smart Biomaterials in Diabetic Wounds" Encyclopedia, https://encyclopedia.pub/entry/41007 (accessed March 01, 2026).
Huang, C., Yuan, W., Chen, J., Wu, L., & You, T. (2023, February 09). The Application of Smart Biomaterials in Diabetic Wounds. In Encyclopedia. https://encyclopedia.pub/entry/41007
Huang, Chan, et al. "The Application of Smart Biomaterials in Diabetic Wounds." Encyclopedia. Web. 09 February, 2023.
Copy Citation
Diabetes mellitus is a complicated metabolic disease that has become one of the fastest-growing health crises in modern society. Diabetic patients may suffer from various complications, and diabetic foot is one of them. It can lead to increased rates of lower-extremity amputation and mortality, even seriously threatening the life and health of patients. Because its healing process is affected by various factors, its management and treatment are very challenging. To address these problems, smart biomaterials have been developed to expedite diabetic wound closure and improve treatment outcomes.
hydrogel
diabetic foot
wound healing
tissue engineering
1. Delivery System for Diabetic Wound Healing
Ideal wound dressings can keep conditions moist, permeate oxygen, remove wound exudates, as well as allow the delivery of drugs or growth factors to promote appropriate tissue remodeling [1]. Based on the aforementioned characteristics of smart biomaterial scaffolds, such as outstanding stability, mechanical properties, biocompatibility, and high porosity, it is shown that smart biomaterials can be used to prepare ideal wound dressings. Several researchers have employed smart biomaterials as carriers for delivering drugs with anti-inflammatory activity, bioactives, and antibacterial nanoparticles.
1.1. Drugs with Anti-Inflammatory Activity
The process of wound healing requires active intervention, and loading smart biomaterials with drugs can accelerate wound healing. For example, a range of hydrogels featuring hyaluronic acid grafted with dopamine and reduced graphene oxide were prepared using the H2O2/HPR (horseradish peroxidase) as an initiator system to release doxycycline, effectively improving wound inflammation and promoting angiogenesis [2]. As well, Liu et al. [3] used a precipitation method to add curcumin to self-assembled nanoparticles (CNPs) to improve their solubility and stability, before encasing CNPs in gelatin microspheres. Nanotechnology can effectively improve the antioxidant capacity and migration-promoting capacity of curcumin. Anti-inflammatory hydrogels encapsulating vancomycin-conjugated silver nanoclusters and pH-sensitive micelles loaded with nimesulide have been developed. This was a new type of structure that not only preserved the dynamical features of the gel, including injectability and the ability to self-heal and remodel but also enabled orderly and on-demand drug delivery at the site of diabetic wounds, with enormous potency in the treatment of chronic wounds [4].
1.2. Bioactive Agency
Exosomes
Angiogenesis is an important element that determines the result of diabetic wound healing. Exosomes have been reported to improve wound repair by accelerating blood vessel formation, which has broad application prospects for diabetic wound therapy [5]. Exosomes are cell-based vesicles, 50–200 nm in diameter, which can control angiogenesis and contribute to the regeneration of chronic wounds. However, their short half-life and rapid elimination are not conducive to their application. Therefore, to enable the prolonged release of exosomes, they are used in hydrogels and provide an interim extracellular matrix for cell infiltration and adhesion [6]. Shiekh et al. [7] prepared OxOBand, a highly porous low-temperature/lyophilized gel composed of antioxidant polyurethane with sustained oxygen release properties, embedded into exosomes from ADSCs. The material provided a substrate for cell migration, which increased the migration of human keratinocytes and fibroblasts and improved the survival rate of human neuroblasts under high glucose conditions. Moreover, it not only provided continuous oxygen to regenerative tissue, alleviated oxidative stress, and promoted rapid wound closure but also increased the development of new blood vessels and enhanced collagen deposition to speed up re-epithelialization. In addition, a natural methylcellulose–chitosan hydrogel with excellent self-healing and biocompatibility was utilized to load bio-exosome nanoparticles to synergistically improve wound recovery and restore tissue structure and function in a diabetic mouse by contributing to the neovascular formation and suppressing apoptosis, suggesting that novel composite hydrogels loaded with exosomes offer promise for severe wound repair [8]. Overall, smart biomaterials loaded with exosomes can serve as wound dressings with excellent performance, which can not only prolong the time of exosome function but also deliver active substances to damaged tissues around diabetic wounds, effectively promoting the proliferation and migration of cells around wounds.
Growth Factors
Growth factors are therapeutic agents that play a vital role in the healing of injured tissue. These are secreted by activated keratin-forming cells, endothelial cells, fibroblasts, macrophages, and platelets during wound reconstruction and help to expedite the regeneration process [9] (Figure 1). In Zhu et al. of study [10], insulin-loaded micelles (ILM) and epidermal growth factor (EGF) were inserted into oxidized hyaluronic acid and succinyl chitosan (OHA/SCS) hybrid hydrogels for wound repair in diabetic model rat skin wounds. The composite hydrogel loaded with ILM and EGF showed good wound repair properties in terms of promoting fibroblast proliferation and structural integrity within the tissue and improving collagen and myofibril deposition. Moreover, Lin et al. designed a silk fibrin membrane (SF) to deliver insulin-like growth factor-1 to diabetic wounds; the results of in vivo examination showed the increased epithelial tissue area and micro-vessel formation by insulin-like growth factor-1 in a dose-dependent manner at a low dose range (3.25 pmol) [11]. Therefore, smart biomaterials loaded with growth factors can be considered promising wound dressings for the treatment of diabetic wounds.
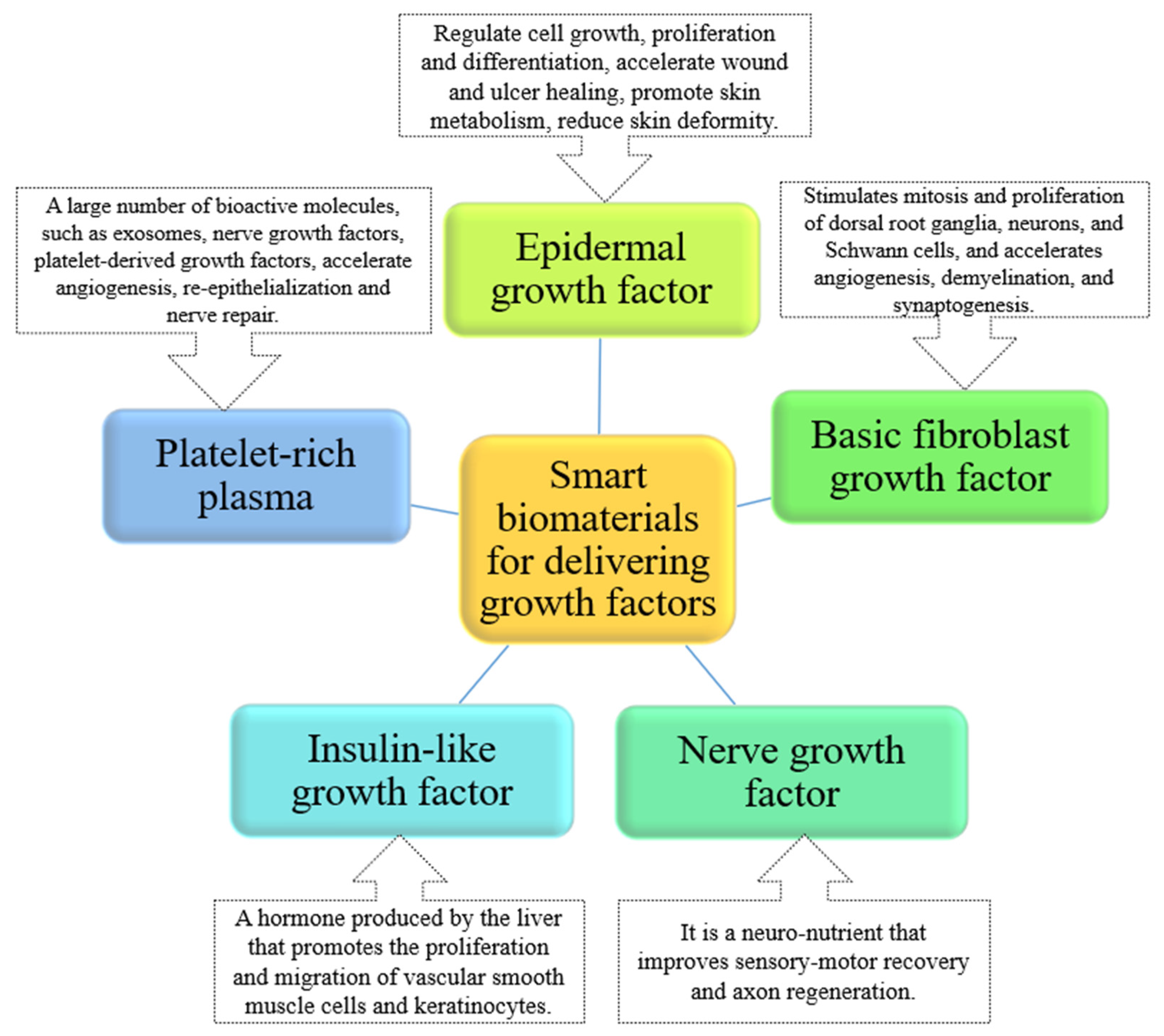
Figure 1. Summary of the key role of bio-intelligent materials in delivering growth factors in healing.
Probiotics
Probiotics are non-pathogenic strains of bacteria that have beneficial effects on the host, and the topical use of some probiotic strains can be very effective in the restoration of skin wounds [12]. For example, in Lu’s group [13], a delivery system composed of live lactic acid bacteria incorporated into a heparin polyoxyethylene ether thermosensitive hydrogel was developed with the aim of improving the biological tissue engineering of wound circumstances and enhancing angiogenesis. This in vivo system generated and protected vascular endothelial growth factor (VEGF), as well as secreted lactic acid to promote macrophage migration. Furthermore, this system confined the bacterial population to the wound, thereby minimizing the risk of systemic toxicity. In addition, L. lactic acid was mixed with thermosensitive hydrogel at a volume ratio of 1:100, and lactic acid bacteria were added to the thermosensitive hydrogel, which was applied to the wound of diabetic mice with full-thickness skin defects. The in situ production and delivery of lactic acid promoted the polarization of macrophages and reshaped the wound repair microenvironment, supporting wound recovery [14].
1.3. Antibacterial Nanoparticles
Silver nanoparticles (AgNP), gold nanoparticles (MNP), copper nanoparticles (CuNP), and nano-bioactive glass particles are together served as antibacterial nanoparticles to enhance wound recovery (Figure 2). Among the aforementioned nanoparticles, AgNP is the most active nanoparticle in promoting wound healing owing to antimicrobial actions against natural and in-hospital multidrug-resistant (MDR) microbial strains [15]. In a study by Badhwar et al. [16], a hydrogel matrix of silver nanoparticles (AgNPs) loaded with quercetin (QCT) (QCT-AgNPs) was prepared for the administration of diabetic wounds, and antibacterial studies showed that QCT-AgNPs hydrogels were more valid against Staphylococcus aureus and E. coli compared to commercially available (MRKT) gels. As well, calcium cross-linked sodium alginate hydrogels (SA-DFO/Cu) incorporating desferrioxamine (DFO) and copper nanoparticles (Cu-NPs) were successfully prepared. The study confirmed that DFO and Cu-NPs act collaboratively to facilitate the migration and vascularization of human umbilical vein endothelial cells, significantly sped up wound recovery, and decreased long-term inflammatory responses in a diabetic mouse wound through synergistically stimulating the levels of HIF-1α and VEGF [17]. Furthermore, Qi et al. [18] produced a hydrogel with thermo-reversibility encapsulated with cerium (Ce)-doped nanoparticles (Ce@ LTA-NPS) of Linde type A (LTA) zeolite to alleviate oxidative stress and inflammatory responses in the diabetic wound site microenvironment. This hydrogel displayed vigorous antibacterial and hemostatic effects, enhanced endothelial cell migration and proliferation by modulating VEGF, VEGFR2, and PI3K, and expedited diabetic wound regeneration by counteracting harmful factors and scavenging reactive oxygen species.
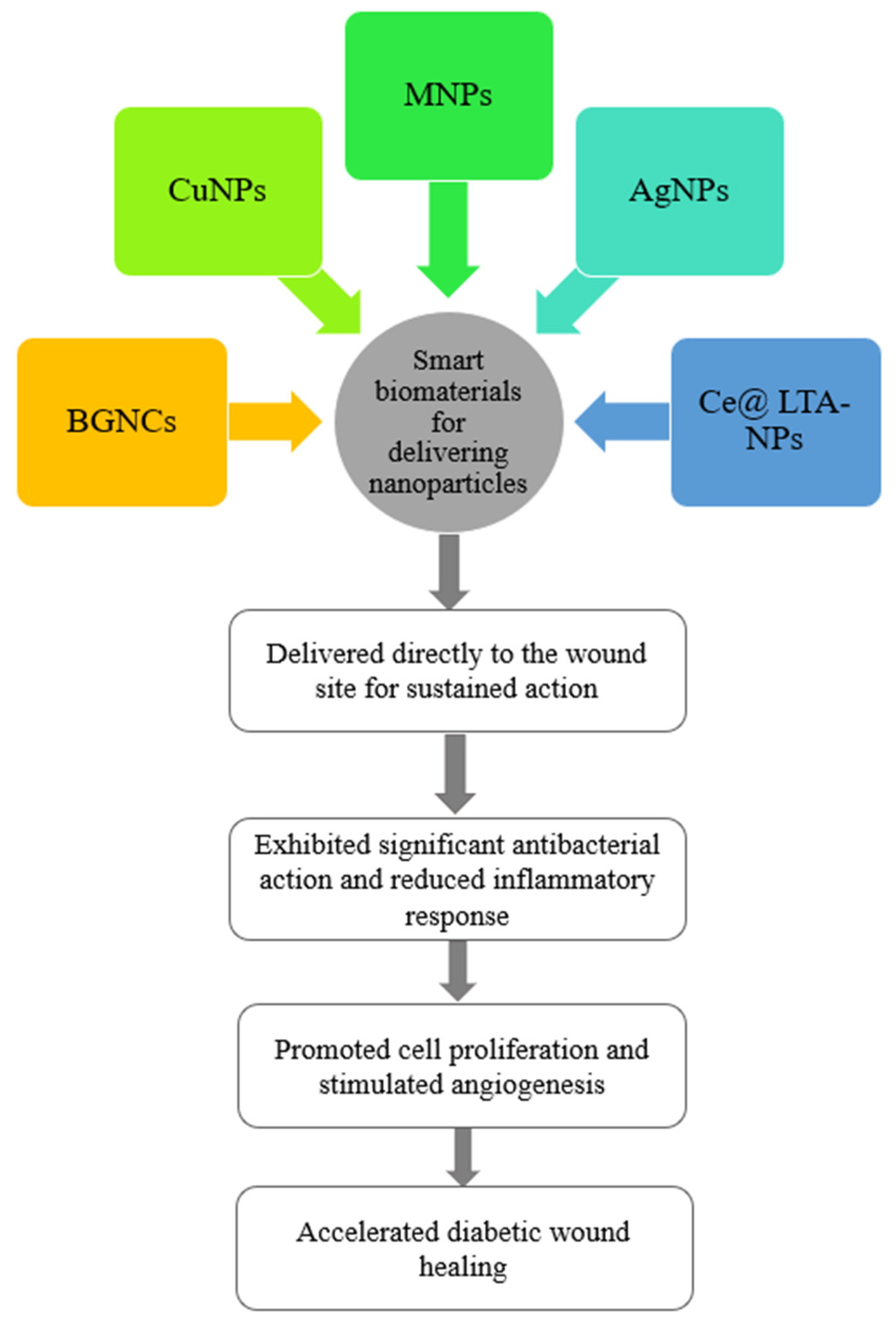
Figure 2. The application of smart biomaterials loaded with nanoparticles in diabetic wound healing.
2. Stimulus-Response System for Diabetic Wound Healing
Stimulus-responsive hydrogels are soft, hydrophilic materials that can be manufactured by applying copolymers, blends, or interpenetrating networks (IPN) and respond to different kinds of variations in the surroundings, including pH, temperature, light, and shear stress [1]. When applied in the treatment of diabetic wounds, they can react to the wound microenvironment and subsequently provide active substances required for the repair of damaged tissues. For example, a polysaccharide-based (FEP) hydrogel scaffold with thermosensitive, injectable, self-healing, and adhesive properties was designed in Wang’s group, which exhibited efficient antimicrobial activity, rapid hemostasis, outstanding UV shielding properties, and pH-responsive exosome release to promote angiogenesis and diabetic wound healing [19]. Moreover, the reaction of amino gelatin with oxidized glucan was performed to form a hydrogel cross-linked with a dynamic Schiff base, which was subsequently used to immobilize paeoniflorin-coated micelles with ROS-responsive properties to the skeleton of the hydrogel. The hydrogel showed high sensitivity to the low pH and ROS environment of refractory wounds. It exhibited antibacterial and angiogenic capabilities in vitro, and significantly accelerated the healing of chronically infected diabetic wounds through continuous hemostasis, microbial killing, and angiogenic activities [20].
In addition, glucose-responsive hydrogels have attracted much attention. Tseng’s [21] research group prepared hydrogels using reversible crosslinked polyethylene glycol diacrylate and dithiothreitol with borax as a glucose-sensitive base sequence. The hydrogels were injectable, which owned high mechanical strength and could be quickly cleared by immersion in a cell culture medium. Therefore, it can be used as a sacrificial material for glucose-sensitive self-healing hydrogels to create branched tubular channels in constructs. As well, in a study by Yang et al. [22], a versatile metal-organic drug hydrogel (DG@Gel) responsive to glucose was designed in which glucose oxidase (GOX) was loaded as programmed. When it was injected into a diabetic wound, the excess glucose was broken down by the GOX in the DG@Gel into hydrogen peroxide and glucuronic acid to alter the hyperglycemic wound microenvironment, thereby lowering the pH of the wound area. Zinc ions and DFO were released into a low pH environment, resulting in collaborative antimicrobial and angiogenic effects for diabetic wound recovery.
3. Other Types of Systems for Diabetic Wound Healing
In addition to the abovementioned details, other types of smart biomaterials have also been applied to the management of diabetic wounds. For example, Mirani [23] and Guo [24] have designed intelligent dressings that can monitor wound conditions. In their study, Mirani et al. [23] proposed a progressive multi-functional dressing (GelDerm) that can measure pH value, one of the indicators of bacterial infection, by colorimetry and release antibacterial reagents at the wound site. An internal smartphone application (iDerm) was also developed to record digital graphics of GelDerm and report pH values, which enabled patients to note the conditions of the wound at home and communicated with medical professionals who could make choices about follow-up therapeutic strategies. Guo et al. [24] designed an amphiphilic skin sensing system with a sandwich structure, capable of continuously measuring and differentiating the three stimulus-response information. This sensor system consisted of an upper and lower layer of amphoteric thermal-glucose-sensitive skin-like hydrogel and an isolated elastomeric layer in between, achieving the goal of monitoring and differentiating temperature, mechanical, and glucose information. Apart from its potential utility in wound detection, this also offers a new promising direction for artificial intelligence to distinguish between multiple signals.
References
- Gianino, E.; Miller, C.; Gilmore, J. Smart Wound Dressings for Diabetic Chronic Wounds. Bioengineering 2018, 5, 51.
- Liang, Y.; Zhao, X.; Hu, T.; Chen, B.; Yin, Z.; Ma, P.X.; Guo, B. Adhesive Hemostatic Conducting Injectable Composite Hydrogels with Sustained Drug Release and Photothermal Antibacterial Activity to Promote Full-Thickness Skin Regeneration During Wound Healing. Small 2019, 15, 1900046.
- Liu, J.; Chen, Z.; Wang, J.; Li, R.; Li, T.; Chang, M.; Yan, F.; Wang, Y. Encapsulation of Curcumin Nanoparticles with MMP9-Responsive and Thermos-Sensitive Hydrogel Improves Diabetic Wound Healing. ACS Appl. Mater. Interfaces 2018, 10, 16315–16326.
- Wang, Y.; Wu, Y.; Long, L.; Yang, L.; Fu, D.; Hu, C.; Kong, Q.; Wang, Y. Inflammation-Responsive Drug-Loaded Hydrogels with Sequential Hemostasis, Antibacterial, and Anti-Inflammatory Behavior for Chronically Infected Diabetic Wound Treatment. ACS Appl. Mater. Interfaces 2021, 13, 33584–33599.
- Wang, C.; Wang, M.; Xu, T.; Zhang, X.; Lin, C.; Gao, W.; Xu, H.; Lei, B.; Mao, C. Engineering Bioactive Self-Healing Antibacterial Exosomes Hydrogel for Promoting Chronic Diabetic Wound Healing and Complete Skin Regeneration. Theranostics 2019, 9, 65–76.
- Henriques-Antunes, H.; Cardoso, R.M.S.; Zonari, A.; Correia, J.; Leal, E.C.; Jiménez-Balsa, A.; Lino, M.M.; Barradas, A.; Kostic, I.; Gomes, C.; et al. The Kinetics of Small Extracellular Vesicle Delivery Impacts Skin Tissue Regeneration. ACS Nano 2019, 13, 8694–8707.
- Shiekh, P.A.; Singh, A.; Kumar, A. Exosome Laden Oxygen Releasing Antioxidant and Antibacterial Cryogel Wound Dressing OxOBand Alleviate Diabetic and Infectious Wound Healing. Biomaterials 2020, 249, 120020.
- Wang, C.; Yuan, W. The Fabrication of a Highly e Ffi Cient Self-Healing Hydrogel from Natural Biopolymers Loaded with Exosomes for the Synergistic Promotion of Severe Wound Healing. Biomater. Sci. 2020, 8, 313–324.
- Kim, J.; Lee, K.M.; Han, S.H.; Ko, E.A.; Yoon, D.S.; Park, I.K.; Shin, H.C.; Park, K.H.; Lee, J.W. Development of Stabilized Dual Growth Factor-Loaded Hyaluronate Collagen Dressing Matrix. J. Tissue Eng. 2021, 12, 1999750.
- Zhu, J.; Jiang, G.; Hong, W.; Zhang, Y.; Xu, B.; Song, G.; Liu, T.; Hong, C.; Ruan, L. Rapid Gelation of Oxidized Hyaluronic Acid and Succinyl Chitosan for Integration with Insulin-Loaded Micelles and Epidermal Growth Factor on Diabetic Wound Healing. Mater. Sci. Eng. C 2020, 117, 111273.
- Lin, M.J.; Lu, M.C.; Chan, Y.C.; Huang, Y.F.; Chang, H.Y. An Insulin-like Growth Factor-1 Conjugated Bombyx Mori Silk Fibroin Film for Diabeticwound Healing: Fabrication, Physicochemical Property Characterization, and Dosage Optimization in Vitro and in Vivo. Pharmaceutics 2021, 13, 1459.
- Mohtashami, M.; Mohamadi, M.; Azimi-Nezhad, M.; Saeidi, J.; Nia, F.F.; Ghasemi, A. Lactobacillus Bulgaricus and Lactobacillus Plantarum Improve Diabetic Wound Healing through Modulating Inflammatory Factors. Biotechnol. Appl. Biochem. 2021, 68, 1421–1431.
- Lu, Y.; Li, H.; Wang, J.; Yao, M.; Peng, Y.; Liu, T.; Li, Z.; Luo, G.; Deng, J. Engineering Bacteria-Activated Multifunctionalized Hydrogel for Promoting Diabetic Wound Healing. Adv. Funct. Mater. 2021, 31, 2105749.
- Lu, Y.F.; Deng, J.; Wang, J.; Luo, G.X. Effects and Mechanism of Lactococcus Lactis Thermo-Sensitive Hydrogel on the Wound Healing of Full-Thickness Skin Defects in Diabetic Mice. Zhonghua Shao Shang Za Zhi 2020, 36, 1117–1129.
- Bai, Q.; Han, K.; Dong, K.; Zheng, C.; Zhang, Y.; Long, Q.; Lu, T. Potential Applications of Nanomaterials and Technology for Diabetic Wound Healing. Int. J. Nanomed. 2020, 15, 9717–9743.
- Badhwar, R.; Mangla, B.; Neupane, Y.R.; Khanna, K.; Popli, H. Quercetin Loaded Silver Nanoparticles in Hydrogel Matrices for Diabetic Wound Healing. Nanotechnology 2021, 32, 505102.
- Li, S.; Wang, X.; Chen, J.; Guo, J.; Yuan, M.; Wan, G.; Yan, C.; Li, W.; Machens, H.-G.; Rinkevich, Y.; et al. Calcium Ion Cross-Linked Sodium Alginate Hydrogels Containing Deferoxamine and Copper Nanoparticles for Diabetic Wound Healing. Int. J. Biol. Macromol. 2022, 202, 657–670.
- Qi, Y.; Qian, K.; Chen, J.; Yifeng, E.; Shi, Y.; Li, H.; Zhao, L. A Thermoreversible Antibacterial Zeolite-Based Nanoparticles Loaded Hydrogel Promotes Diabetic Wound Healing via Detrimental Factor Neutralization and ROS Scavenging. J. Nanobiotechnol. 2021, 19, 414.
- Wang, M.; Wang, C.; Chen, M.; Xi, Y.; Cheng, W.; Mao, C.; Xu, T.; Zhang, X.; Lin, C.; Gao, W.; et al. Efficient Angiogenesis-Based Diabetic Wound Healing/Skin Reconstruction through Bioactive Antibacterial Adhesive Ultraviolet Shielding Nanodressing with Exosome Release. ACS Nano 2019, 13, 10279–10293.
- Guo, C.; Wu, Y.; Li, W.; Wang, Y.; Kong, Q. Development of a Microenvironment-Responsive Hydrogel Promoting Chronically Infected Diabetic Wound Healing through Sequential Hemostatic, Antibacterial, and Angiogenic Activities. ACS Appl. Mater. Interfaces 2022, 14, 30480–30492.
- Tseng, T.C.; Hsieh, F.Y.; Theato, P.; Wei, Y.; Hsu, S.H. Glucose-Sensitive Self-Healing Hydrogel as Sacrificial Materials to Fabricate Vascularized Constructs. Biomaterials 2017, 133, 20–28.
- Yang, J.; Zeng, W.N.; Xu, P.; Fu, X.; Yu, X.; Chen, L.; Leng, F.; Yu, C.; Yang, Z. Glucose-Responsive Multifunctional Metal–Organic Drug-Loaded Hydrogel for Diabetic Wound Healing. Acta Biomater. 2022, 140, 206–218.
- Mirani, B.; Pagan, E.; Currie, B.; Siddiqui, M.A.; Hosseinzadeh, R.; Mostafalu, P.; Zhang, Y.S.; Ghahary, A.; Akbari, M. An Advanced Multifunctional Hydrogel-Based Dressing for Wound Monitoring and Drug Delivery. Adv. Healthc. Mater. 2017, 6, 1700718.
- Guo, H.; Bai, M.; Zhu, Y.; Liu, X.; Tian, S.; Long, Y.; Ma, Y.; Wen, C.; Li, Q.; Yang, J.; et al. Pro-Healing Zwitterionic Skin Sensor Enables Multi-Indicator Distinction and Continuous Real-Time Monitoring. Adv. Funct. Mater. 2021, 31, 2106406.
More
Information
Subjects:
Pharmacology & Pharmacy
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
767
Revisions:
2 times
(View History)
Update Date:
09 Feb 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





