Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Robert Martijn Kauling | -- | 2690 | 2023-02-03 11:42:50 | | | |
| 2 | Camila Xu | Meta information modification | 2690 | 2023-02-06 01:54:18 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kauling, R.M.; Rienks, R.; Cuypers, J.A.A.E.; Jorstad, H.T.; Roos-Hesselink, J.W. SCUBA Diving in Adult Congenital Heart Disease. Encyclopedia. Available online: https://encyclopedia.pub/entry/40807 (accessed on 08 February 2026).
Kauling RM, Rienks R, Cuypers JAAE, Jorstad HT, Roos-Hesselink JW. SCUBA Diving in Adult Congenital Heart Disease. Encyclopedia. Available at: https://encyclopedia.pub/entry/40807. Accessed February 08, 2026.
Kauling, Robert M., Rienk Rienks, Judith A. A. E. Cuypers, Harald T. Jorstad, Jolien W. Roos-Hesselink. "SCUBA Diving in Adult Congenital Heart Disease" Encyclopedia, https://encyclopedia.pub/entry/40807 (accessed February 08, 2026).
Kauling, R.M., Rienks, R., Cuypers, J.A.A.E., Jorstad, H.T., & Roos-Hesselink, J.W. (2023, February 03). SCUBA Diving in Adult Congenital Heart Disease. In Encyclopedia. https://encyclopedia.pub/entry/40807
Kauling, Robert M., et al. "SCUBA Diving in Adult Congenital Heart Disease." Encyclopedia. Web. 03 February, 2023.
Copy Citation
The classification of scuba diving as a skill sport has profound implications for the evaluation of fitness-to-dive in adult patients with congenital heart disease (ACHD). The spectrum of ACHD and its associated complications range from conditions conventionally considered as incompatible with scuba diving (e.g., pulmonary hypertension, cyanosis and ventricular hypertrophy) to other conditions which may be compatible with recreational scuba diving.
scuba diving
congenital heart disease
1. Introduction
Scuba diving is an increasingly popular activity. The Professional Association of Diving instructors (PADI) which covers 60–70% of the global scuba diving market, has issued more than 28 million diver certifications globally since 1976 [1]. Because of this increased popularity, there has also been an increase in people with cardiovascular disease who wish to start diving, including patients with (repaired) congenital heart disease (CHD). This topic has become more relevant as the number of adults with CHD (ACHD) is expanding, with more than 90% of children born with CHD reaching adulthood nowadays [2][3][4]. Most of these patients experience a good quality of life, and want to live a normal life, including sports participation, and a growing number of ACHD patients consider scuba diving [5][6]. As such, cardiologists are frequently confronted with ACHD patients seeking advice whether they are fit to dive.
Recently, the Task Force on Sports Cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC) published updated guidelines regarding the participation in competitive sports of patients with cardiovascular disease [7]. Although some general contra-indications for diving are included in this guideline, eligibility for scuba diving is only mentioned briefly. More specific recommendations regarding participation in competitive sports in ACHD patients were recently published in a position paper by the Working Group on Adult Congenital Heart Disease and on Sports Cardiology [8]. In this document, scuba diving has been classified as a “skill sports discipline”, due to its presumed limited effects on heart rate and blood pressure, but with an intrinsic risk of serious harm or death for the athlete in the event of syncope.
The classification of scuba diving as a skill sport has profound implications for the evaluation of fitness-to-dive in patients with ACHD. The spectrum of ACHD and its associated complications range from conditions conventionally considered as incompatible with scuba diving (e.g., pulmonary hypertension, cyanosis and ventricular hypertrophy) to other conditions which may be compatible with recreational scuba diving. Severity of ACHD differs substantially amongst and within different diagnosis groups.
2. Diving Physiology: Cardiovascular and General Aspects
Immersion and submersion have profound effects on the cardiovascular, respiratory, endocrinal, renal and central nervous systems. In healthy individuals, immersion leads to an increase in hydrostatic pressure, resulting in a fluid-shift towards the central circulation, consequently increasing the preload of the left ventricle augmenting cardiac output via the Frank–Starling mechanism. This volume loading of the ventricles leads to right atrial and ventricular dilatation, with a compensatory increase in the secretion of natriuretic peptide. Throughout the dive, this will gradually increase diuresis (“diver’s pee”), resulting in a relatively hypovolemic state at the end of the dive [9]. Secondly, even in tropical waters, immersion and submersion will induce peripheral vasoconstriction, resulting in a rise in systolic blood pressure and ventricular afterload.
Finally, exposure of the trigeminus nerve to cold water will stimulate the diving reflex. This will induce inhibition of the cardio-respiratory center in the medulla oblongata, resulting in bradycardia (decrease in the heart rate of up to 60%), QT interval prolongation and vasoconstriction [10]. The combination of sympathetic and parasympathetic stimulation may in rare cases lead to an “autonomic conflict”, which has been associated with the onset of ventricular arrhythmias [11]. This might lead to life-threatening arrhythmias in vulnerable hearts, for instance with hypertrophy, ischemia, pre-existing arrhythmias and channelopathies [11].
In patients with cardiovascular disease, diving-associated hemodynamic alterations potentially disturb a previously well-tolerated cardiac condition. In particular in patients with diminished right or left ventricular systolic function, restrictive diastolic function or patients with moderate to severe valvular disease, these volume shifts might lead to cardiac decompensation, and pulmonary oedema may develop (immersion pulmonary oedema (IPE)) [12]. The development of a bradycardia by the diving reflex might be especially relevant in patients with a depressed systolic left or right ventricular function, resulting in a decrease in cardiac output. In addition, peripheral vasoconstriction will result in an increase in systemic afterload and may challenge divers with a left ventricular outflow tract (LVOT) obstruction or depressed left ventricular function.
In addition to these cardiovascular effects, several general aspects are important in all divers. Water is in principle an unforgiving environment. To survive, one needs an air supply, whether from the surface (with an “umbilical”), or from a carried tank filled with air (or another gas mixture). In the water there are hyperbaric conditions. At every 10 meters of increasing depth, the ambient pressure increases by 1 atmosphere. As a result, inhalation gases become denser, increasing the respiratory work [13]. Additionally, the solubility of the gases increases. This results in storage of especially nitrogen from the air in the blood and tissues.
The main factors for this build-up are the nitrogen content of the inhaled gas, depth of the dive and duration of the dive. One can calculate how much nitrogen is being stored in the tissues during the dive, and how long and how deep one can dive without extra stops to wash-out the nitrogen from the tissues. These calculations are available as “no decompression dive tables” (no-deco dives). When exceeding the limits as to depth and time indicated by these tables, chances of decompression sickness (DCS) increase. All patients are advised to remain within the limits of these decompression tables.
After the dive, when ambient pressure has been reduced to normal (1 atmosphere), this nitrogen is released from the tissues. This may cause local bubble formation, resulting in local DCS (for instance in the joints, “the bends”). The nitrogen may also be transported through the blood to the lungs, where it is exhaled. When there is too much nitrogen in the blood, bubble formation may result. These bubbles cause a temporary increase in pulmonary artery pressure [14]. When there is a connection between the pulmonic and systemic circulation, for instance by means of a patent foramen ovale (PFO), these bubbles may enter the systemic circulation and cause DCS. The symptoms of shunt-related DCS are dependent on the organ involved, for instance, neurological syndromes, unconsciousness, vertigo or cutis marmorata. DCS should be differentiated from Arterial Gas Embolism (AGE), which occurs when expanding gas stretches and ruptures alveolar capillaries (pulmonary barotrauma) allowing alveolar gas to enter the arterial circulation [15].
3. Exercise Capacity and Diving
Diving exercise intensity was recently reported to be 5 ± 2 METs in 139 experienced recreational divers (age 42 ± 10 years, total 959 dives), leading to the suggestion that maintaining an exercise capacity of >7 METs (peak VO2 24.5 mL/kg/min in men and 22.4 mL/kg/min in women) would generally be adequate for uncomplicated recreational diving [16]. However, in some circumstances, a higher energy expenditure is required, for instance in case of a difficult entry or exit from the diving place (long walk with the equipment that may weight up to 20–30 kg), waves or currents. Of particular importance is that a diver should be able to rescue his or her buddy diver, which may require a substantially higher exercise capacity. Professional diving organizations (military, police, fire brigade) usually require an exercise capacity of 13 METs (peak VO2 40 mL/kg/min) [17]. Patients (whether with ACHD) who do not meet an exercise capacity of 25 mL/min/kg are conventionally advised not to dive, while patients with a VO2 max between 25 and 40 (men) or 25 and 35 (women) are advised to engage in non-strenuous diving or fitness optimization prior to commencing diving [18].
4. Evaluating Fitness to Dive in Patients with ACHD
Many patients with ACHD will be under regular follow-up by their own congenital cardiologist. Medical Examiners of Divers (MED) should obtain information from the treating physician during the evaluation process. Topics that should be discussed are the medical history, current cardiovascular status (including exercise capacity and echocardiography), medication use and any cardiovascular complications disqualifying the candidate for diving. The focus of this information should be on how diving physiology potentially may lead to a deterioration in cardiac function and thus threaten the patient or his/her diving-buddy. Patients with ACHD who are approved fit-to-dive after thorough evaluation should have an annual reassessment by their MED, to rule out any onset of new symptoms or signs of cardiac deterioration.
Comparable to a general cardiovascular diving evaluation, a detailed history-taking and physical examination should be performed. Chest pain, dyspnea, dizziness, palpitations or loss of consciousness, especially during exercise, disqualify candidate-divers pending further evaluation.
Many ACHD patients have undergone one or more surgical procedures involving a sternal and/or lateral thoracotomy. If the surgery involved the pleura, the risk of persisting pleural adhesions remains. Patients after thoracotomy should undergo pulmonary function testing and when abnormal should also have a CT thorax, and in case of abnormalities (for instance adhesions) be referred to a pulmonologist. Patients who have undergone a lateral thoracotomy are advised to have a CT thorax in any case, because of the perceived risk of pleural adhesions. Patients with any pleural adhesions should be advised against diving [19][20].
Physical examination should include at least office blood-pressure and cardiac examination, focusing on signs of heart failure and the presence of (new) cardiac murmurs. As hypertension is associated with IPE, patients with a blood pressure exceeding 160/100 mmHg at rest should be advised against diving until adequate treatment of blood pressure has been achieved [21][22]. Any signs of heart failure or the presence of previously unknown cardiac murmurs should prompt further evaluation before certification.
A recent 12-lead electrocardiogram is mandatory. New onset supraventricular arrhythmia temporally disqualifies a patient from diving pending further analysis and adequate treatment. If the ECG shows new signs of left or right ventricular hypertrophy, especially in patients known to have abnormal loading conditions, echocardiographic evaluation is indicated to rule out any progression in valvular abnormalities or the development of hypertrophic cardiomyopathy. In addition, new onset AV block or bundle branch block warrants further analysis with advanced AV block being a contra-indication for diving [23].
Specific recommendations in patients with cardiac arrhythmias are provided in the section below covering specific conditions.
Transthoracic echocardiography is essential in the evaluation of candidate-divers with ACHD, and a recent (<12 months) echo study should be available in all patients. Basic chamber quantification with assessment of the left and right ventricular dimensions and function, aortic dimensions, valvular function and estimation of the pulmonary pressures should be performed [24][25][26]. Echocardiography of the right ventricle in ACHD patients can be challenging. The right ventricle’s unique crescent shape complicates quantification of its size and function by echocardiography. By using multiple acoustic windows, both qualitative and quantitative parameters could be examined [24]. Specific considerations with respect to echocardiographic assessment of several common forms of congenital heart disease are discussed separately in the section on specific conditions. Echocardiographic aspects and cut-offs that are important in all ACHD patients are summarized in Table 1. In this table, results compatible with diving are marked green while results that are incompatible with diving are marked red. Results marked orange are conditionally compatible with diving.
| Parameter | Definitions | ||
|---|---|---|---|
| Ventricular dysfunction | No dysfunction: LVEF > 55%, RV TAPSE > 17 mm, S’ > 10 cm/s, FAC > 35% |
Mild dysfunction: 45% ≥ EF < 55% (or normal sRV function) |
Moderate–severe dysfunction: EF < 45% or impaired sRV function |
| Ventricular hypertrophy | No hypertrophy: Wall thickness (cm): <1.1 (male) or <1.0 (female) |
Mild hypertrophy: Wall thickness (cm): 1.1–1.3 (male) or 1.0–1.2 (female) |
Moderate–severe hypertrophy: Wall thickness (cm) ≥ 1.3 (male) or ≥1.3 (female) |
| Ventricular pressure overload | No pressure overload: No RVOT or LVOT obstruction (PSV < 2.6 m/s), no coarctation |
Mild pressure overload: 2.6 m/s ≤ PSV < 3 m/s for LVOT and RVOT obstructions and PPS; for CA, peak arm-leg gradient < 20 mmHg |
Moderate–severe pressure overload: PSV > 3 m/s for LVOT and RVOT obstruction and PPS, CA peak arm-leg gradient ≥ 20 mmHg |
| Ventricular volume overload | No volume overload: Absent or mild to moderate valve regurgitation without LV/RV dilatation |
Mild volume overload: Mild to moderate valve regurgitation with mild LV/RV dilatation (LVEDD < 61 mm/RVEDD < 42 mm with preserved systolic function) |
Moderate–severe volume overload: Severe valve regurgitation or moderate–severe LV/RV dilatation (LVEDD > 61 mm/RVEDD > 42 mm) |
| Pulmonary artery pressure | Low probability PH: TVRVc ≤ 2.8 m/s and no additional echocardiographic findings suggestive of PH or invasive mPAP < 20 mmHg |
Intermediate–high probability PH: TVRVc > 2.8 m/s or additional echocardiographic findings suggestive of PH or invasive mPAP > 20 mmHg |
|
| Aorta (non-syndromic) | No dilatation: Aorta size ≤ 35 mm, z-score < 3 |
Mild dilatation: Aorta size ≤ 45 mm, z-score ≤ 4 |
Moderate–severe dilatation: Aorta size ≥ 45 mm, z-score >4 Any syndromic aorta syndrome |
| Arrhythmia | No arrhythmia: Absence of arrhythmia or infrequent PVCs (<500/24 h) that do not worsen during exercise |
Mild arrhythmia: Frequent PVC not worsening during exercise Controlled AF/AFl or other SVT without incapacitating symptoms |
Clinically important arrythmia: Any ventricular arrhythmia Any previously incapacitating SVT Pre-excitation pattern without EP study |
| Arterial oxygen saturation at rest/during exercise | Normal: SaO2 > 95% in rest or during exercise |
Abnormal: SaO2 < 95% in rest or during exercise |
|
| Shunts | No shunt: No residual ASD or VSD after closure |
Shunt: Small, restrictive VSD without LV dilatation PFO |
Shunt: ASD with R—L shunt VSD with LV dilatation |
Abbreviations: LVEF: left ventricular ejection fraction; RV: right ventricle; TAPSE: tricuspid annular plane systolic excursion; FAC: fractional area change; EF: ejection fraction; sRV: systemic right ventricle; LVOT: left ventricular outflow tract; RVOT: right ventricular outflow tract; PPS: peripheral pulmonary stenosis; CA: aortic coarctation; LVEDD: left ventricular end-diastolic diameter; RVEDD: right ventricular end-diastolic diameter; TVRVc: tricuspid valve regurgitation velocity; PH: pulmonary hypertension; mPAP: mean pulmonary artery pressure; PVC: premature ventricular complex; AF: atrial fibrillation; AFl: atrial flutter; SVT: supraventricular tachycardia; EP: electrophysiology; ASD: atrial septal defect; VSD: ventricular septal defect; PFO: persistent foramen ovale.
In all patients with suspected aortic dilatation, performing CT or MR angiography to determine exact aortic dimensions and evaluate the parts of the thoracic aorta that are poorly visualized by echocardiography is recommended.
Cardiopulmonary exercise testing is recommended in all patients with ACHD, with a recommended minimum functional capacity of 8 METs to allow diving. In general, most ACHD patients report normal or only mild limitations in self-reported exercise capacity [28][29][30]. However, self-reported exercise capacity is unreliable in ACHD patients because patients are used to this situation and judge their exercise as normal, while in fact being suboptimal to poor, depending on the diagnosis [28][29][31][32][33]. In general, ACHD patients demonstrate a lower peak VO2 compared with the predicted peak VO2 for sedentary individuals of the same age and gender, ranging from 12.2 ± 3.8 mL/min/kg in patients with Eisenmenger syndrome to 31.9 ± 9.2 mL/min/kg in transposition of the great arteries (TGA) after arterial switch [33]. Interestingly, even adults with CHD in New York Heart Association (NYHA) class 1 showed an impaired exercise capacity compared with healthy subjects of a similar age (peak VO2 21.7 ± 8.5 versus 45.1 ± 8.6 mL/min/kg) [32]. General disqualifying features for diving during exercise testing, such as rhythm or conduction disorders, insufficient increase in blood pressure and ischemic changes also apply for patients with ACHD. Specific attention should be paid to an abnormal (hypertensive) blood pressure response (>250 mmHg), which disqualifies from diving. A drop in transcutaneous arterial oxygen saturations during exercise below 95% should prompt attention to previously unknown cardiac shunts or relevant pulmonary disease and disqualifies a patient for diving.
ACHD patients with a reduced exercise capacity should realize that they are not suitable for participating in all types of diving at all places. They should be advised to avoid diving in circumstances requiring strenuous exercise, such as when there are strong currents, cold water, difficult entry into and exit from the water, carrying heavy equipment such as twinsets and decompression cylinders, stress dives, cave and wreck diving, technical diving and being an instructor for other divers [18].
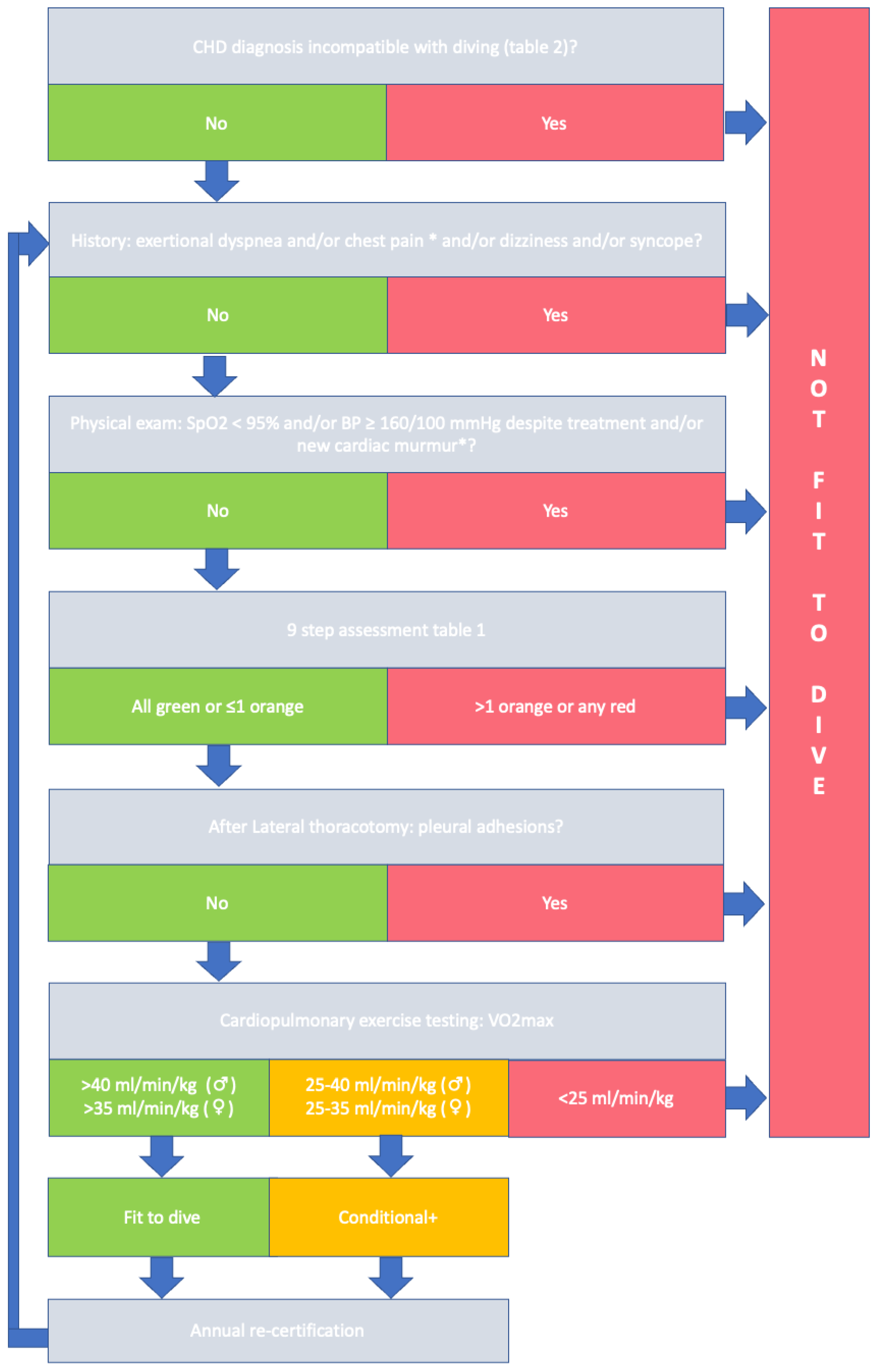
In accordance with the recently published ESC guidelines on sports cardiology and recommendations of the working group of Adult Congenital Heart Disease, candidate-divers should be evaluated according to a stepwise approach [7][8]. In concordance with this approach, in Figure 1 a flow-chart is provided describing the framework for evaluation of a candidate-diver with ACHD.
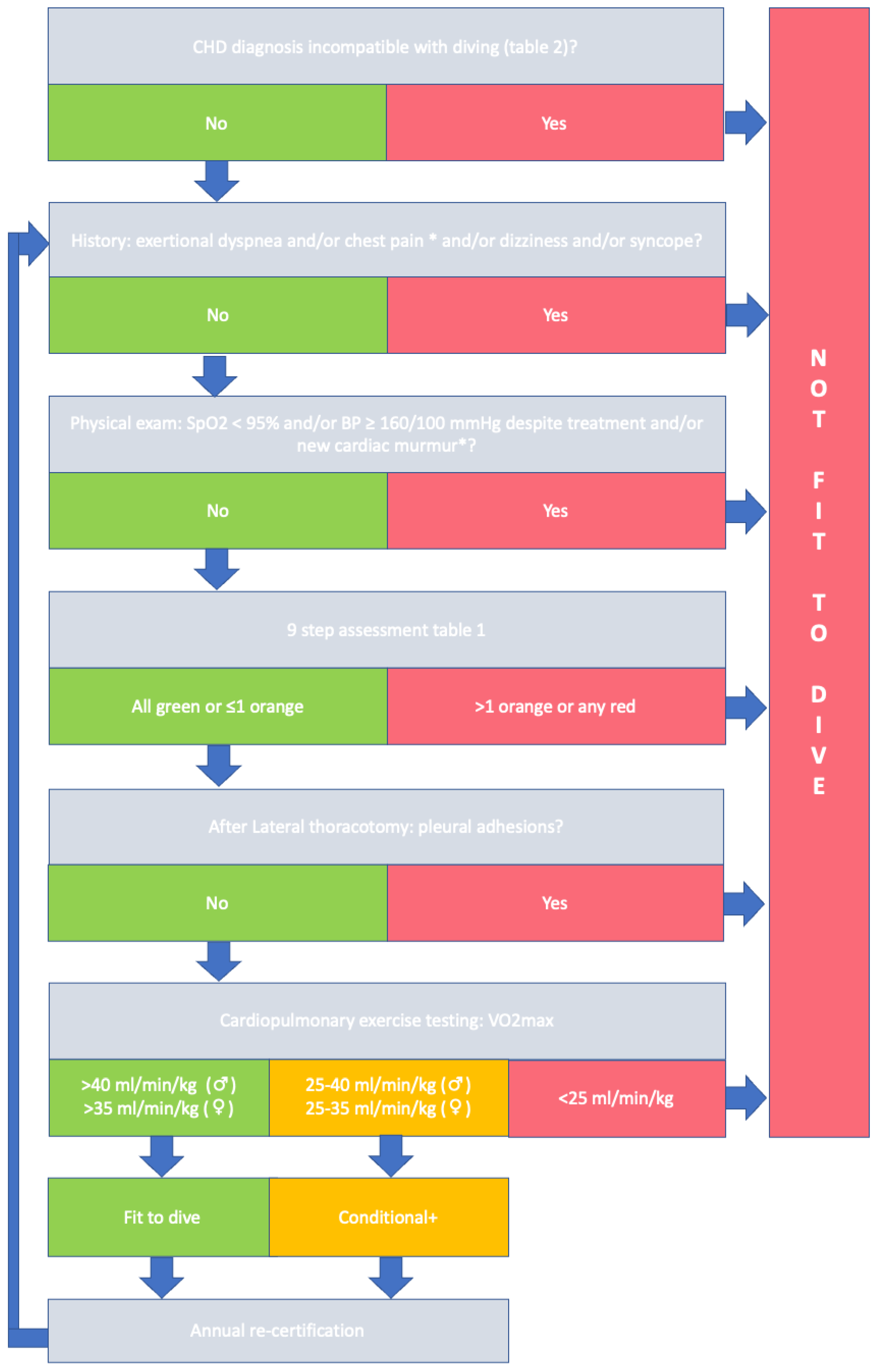
Figure 1. Evaluating fitness-to-dive in ACHD patients. * Reassessment after clinical work-up. + Conditional, non-strenuous diving.
References
- PADI. Padi Global Statistics 2016–2021. Available online: https://www.padi.com/sites/default/files/documents/2022-08/ABOUT%20PADI%20-%20Global%20Statistics%20%20%2716-%2721.pptx%20%281%29.pdf (accessed on 24 November 2022).
- Kempny, A.; Dimopoulos, K.; Uebing, A.; Diller, G.-P.; Rosendahl, U.; Belitsis, G.; Gatzoulis, M.A.; Wort, S.J. Outcome of Cardiac Surgery in Patients with Congenital Heart Disease in England between 1997 and 2015. PLoS ONE 2017, 12, e0178963.
- Khairy, P.; Ionescu-Ittu, R.; Mackie, A.S.; Abrahamowicz, M.; Pilote, L.; Marelli, A.J. Changing Mortality in Congenital Heart Disease. J. Am. Coll. Cardiol. 2010, 56, 1149–1157.
- Moons, P.; Bovijn, L.; Budts, W.; Belmans, A.; Gewillig, M. Temporal Trends in Survival to Adulthood among Patients Born with Congenital Heart Disease from 1970 to 1992 in Belgium. Circulation 2010, 122, 2264–2272.
- Apers, S.; Kovacs, A.H.; Luyckx, K.; Thomet, C.; Budts, W.; Enomoto, J.; Sluman, M.A.; Wang, J.-K.; Jackson, J.L.; Khairy, P.; et al. Quality of Life of Adults With Congenital Heart Disease in 15 Countries: Evaluating Country-Specific Characteristics. J. Am. Coll. Cardiol. 2016, 67, 2237–2245.
- Reiner, B.; Oberhoffer, R.; Ewert, P.; Müller, J. Quality of Life in Young People with Congenital Heart Disease Is Better than Expected. Arch. Dis. Child 2019, 104, 124.
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.-P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with Cardiovascular Disease: The Task Force on Sports Cardiology and Exercise in Patients with Cardiovascular Disease of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 17–96.
- Budts, W.; Pieles, G.E.; Roos-Hesselink, J.W.; Sanz de la Garza, M.; D’Ascenzi, F.; Giannakoulas, G.; Müller, J.; Oberhoffer, R.; Ehringer-Schetitska, D.; Herceg-Cavrak, V.; et al. Recommendations for Participation in Competitive Sport in Adolescent and Adult Athletes with Congenital Heart Disease (CHD): Position Statement of the Sports Cardiology & Exercise Section of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2020, 41, 4191–4199.
- Boussuges, A.; Gole, Y.; Mourot, L.; Jammes, Y.; Melin, B.; Regnard, J.; Robinet, C. Haemodynamic Changes after Prolonged Water Immersion. J. Sport. Sci. 2009, 27, 641–649.
- Michael Panneton, W. The Mammalian Diving Response: An Enigmatic Reflex to Preserve Life? Physiology 2013, 28, 284–297.
- Shattock, M.J.; Tipton, M.J. ‘Autonomic Conflict’: A Different Way to Die during Cold Water Immersion? J. Physiol. 2012, 590, 3219–3230.
- Peacher, D.F.; Martina, S.D.; Otteni, C.E.; Wester, T.E.; Potter, J.F.; Moon, R.E. Immersion Pulmonary Edema and Comorbidities. Med. Sci. Sport. Exerc. 2015, 47, 1128–1134.
- Held, H.E.; Pendergast, D.R. Relative Effects of Submersion and Increased Pressure on Respiratory Mechanics, Work, and Energy Cost of Breathing. J. Appl. Physiol. 2013, 114, 578–591.
- Marabotti, C.; Scalzini, A.; Chiesa, F. Increase of Pulmonary Arterial Pressure in Subjects with Venous Gas Emboli after Uncomplicated Recreational SCUBA Diving. Respir. Med. 2013, 107, 596–600.
- Vann, R.D.; Butler, F.K.; Mitchell, S.J.; Moon, R.E. Decompression Illness. Lancet 2011, 377, 153–164.
- Buzzacott, P.; Pollock, N.W.; Rosenberg, M. Exercise Intensity Inferred from Air Consumption during Recreational Scuba Diving. Diving Hyperb. Med. 2014, 44, 74–78.
- Mitchell, S.J.; Bove, A.A. Medical Screening of Recreational Divers for Cardiovascular Disease: Consensus Discussion at the Divers Alert Network Fatality Workshop. Undersea Hyperb. Med. 2011, 38, 289–296.
- Rienks, R.; Buwalda, M.; Bucx, J.; Dubois, E.; Wingelaar, T.; van Hulst, R. Cardiovascular Risk Assessment in Divers: Toward Safer Diving. Undersea Hyperb. Med. 2022, 49, 355–365.
- Godden, D.; Currie, G.; Denison, D.; Farrell, P.; Ross, J.; Stephenson, R.; Watt, S.; Wilmshurst, P. British Thoracic Society Guidelines on Respiratory Aspects of Fitness for Diving. Thorax 2003, 58, 3–13.
- Nederlandse Vereniging van Artsen voor Longziekten en Tuberculose. Ademhaling Onder Bijzondere Omstandigheden—Duiken, Vliegen En Hoogte. Version 15-2-2021. Available online: https://www.nvalt.nl/kwaliteit/richtlijnen/overige-relevantedocumenten/_/Overige%20onderwerpen/Positionpaper%20Ademhaling%20onder%20bijzondere%20omstandigheden%20SLF%20feb%202021.pdf (accessed on 30 November 2022).
- Westerweel, P.E.; Rienks, R.; Sakr, A.; Taher, A. Diving with Hypertension and Antihypertensive Drugs. Diving Hyperb. Med. J. 2020, 50, 49–53.
- Gempp, E.; Demaistre, S.; Louge, P. Hypertension Is Predictive of Recurrent Immersion Pulmonary Edema in Scuba Divers. Int. J. Cardiol. 2014, 172, 528–529.
- Brouant, B.; Houriez, P.; Lafay, V.; Roche, F.; Finet, G.; Grandjean, B. Pratique de La Plongée et Des Sports Subaquatiques Par Lespatients Présentant Des Troubles de La Conduction Ou Du Rythmecardiaque: Recommendations Pour La FFESSM. Bull. Medsubhyp 2009, 19, 177–184.
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271.
- di Salvo, G.; Miller, O.; Babu Narayan, S.; Li, W.; Budts, W.; Valsangiacomo Buechel, E.R.; Frigiola, A.; van den Bosch, A.E.; Bonello, B.; Mertens, L.; et al. Imaging the Adult with Congenital Heart Disease: A Multimodality Imaging Approach—Position Paper from the EACVI. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1077–1098.
- Li, W.; West, C.; McGhie, J.; van den Bosch, A.E.; Babu-Narayan, S.V.; Meijboom, F.; Mongeon, F.P.; Khairy, P.; Kimball, T.R.; Beauchesne, L.M.; et al. Consensus recommendations for echocardiography in adults with congenital heart defects from the International Society of Adult Congenital Heart Disease (ISACHD). Int. J. Cardiol. 2018, 272, 77–83.
- van Hare, G.F.; Ackerman, M.J.; Evangelista, J.-A.K.; Kovacs, R.J.; Myerburg, R.J.; Shafer, K.M.; Warnes, C.A.; Washington, R.L.; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology; Council on Cardiovascular Disease in Young; et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 4: Congenital Heart Disease: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation 2015, 132, e281–e291.
- Menting, M.E.; Cuypers, J.A.A.E.; Opić, P.; Utens, E.M.W.J.; Witsenburg, M.; van den Bosch, A.E.; van Domburg, R.T.; Meijboom, F.J.; Boersma, E.; Bogers, A.J.J.C.; et al. The Unnatural History of the Ventricular Septal Defect: Outcome up to 40 Years after Surgical Closure. J. Am. Coll. Cardiol. 2015, 65, 1941–1951.
- Cuypers, J.A.A.E.; Menting, M.E.; Konings, E.E.M.; Opić, P.; Utens, E.M.W.J.; Helbing, W.A.; Witsenburg, M.; van den Bosch, A.E.; Ouhlous, M.; van Domburg, R.T.; et al. Unnatural History of Tetralogy of Fallot: Prospective Follow-up of 40 Years after Surgical Correction. Circulation 2014, 130, 1944–1953.
- Cuypers, J.A.A.E.; Opić, P.; Menting, M.E.; Utens, E.M.W.J.; Witsenburg, M.; Helbing, W.A.; van den Bosch, A.E.; Ouhlous, M.; van Domburg, R.T.; Meijboom, F.J.; et al. The Unnatural History of an Atrial Septal Defect: Longitudinal 35 Year Follow up after Surgical Closure at Young Age. Heart 2013, 99, 1346–1352.
- Rafiq, I.; Freeman, L.; Orzalkiewicz, M.; Hiari, N.; Lewis, C. 143 Natural History of Repaired and Unrepaired VSD—An Experience of a District General Hospital with Dedicated Adult Congenital Heart Disease Clinics. Heart 2015, 101 (Suppl. S4), A82–A83.
- Diller, G.-P.; Dimopoulos, K.; Okonko, D.; Li, W.; Babu-Narayan, S.; Broberg, C.S.; Johansson, B.; Bouzas, B.; Mullen, M.J.; Poole-Wilson, P.A.; et al. Exercise Intolerance in Adult Congenital Heart Disease. Circulation 2005, 112, 828–835.
- Kempny, A.; Dimopoulos, K.; Uebing, A.; Moceri, P.; Swan, L.; Gatzoulis, M.A.; Diller, G.-P. Reference Values for Exercise Limitations among Adults with Congenital Heart Disease. Relation to Activities of Daily Life—Single Centre Experience and Review of Published Data. Eur. Heart J. 2012, 33, 1386–1396.
More
Information
Subjects:
Health Care Sciences & Services
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.6K
Revisions:
2 times
(View History)
Update Date:
06 Feb 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




