Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Zuha Imtiyaz | -- | 3266 | 2022-11-21 23:54:39 | | | |
| 2 | Dean Liu | -19 word(s) | 3247 | 2022-11-28 05:00:42 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Imtiyaz, Z.; He, J.; Leng, Q.; Agrawal, A.K.; Mixson, A.J. Chemotherapeutic Targeting of Tumors with Imidazole-Enriched Nanoparticles. Encyclopedia. Available online: https://encyclopedia.pub/entry/36679 (accessed on 07 February 2026).
Imtiyaz Z, He J, Leng Q, Agrawal AK, Mixson AJ. Chemotherapeutic Targeting of Tumors with Imidazole-Enriched Nanoparticles. Encyclopedia. Available at: https://encyclopedia.pub/entry/36679. Accessed February 07, 2026.
Imtiyaz, Zuha, Jiaxi He, Qixin Leng, Atul K. Agrawal, A. James Mixson. "Chemotherapeutic Targeting of Tumors with Imidazole-Enriched Nanoparticles" Encyclopedia, https://encyclopedia.pub/entry/36679 (accessed February 07, 2026).
Imtiyaz, Z., He, J., Leng, Q., Agrawal, A.K., & Mixson, A.J. (2022, November 27). Chemotherapeutic Targeting of Tumors with Imidazole-Enriched Nanoparticles. In Encyclopedia. https://encyclopedia.pub/entry/36679
Imtiyaz, Zuha, et al. "Chemotherapeutic Targeting of Tumors with Imidazole-Enriched Nanoparticles." Encyclopedia. Web. 27 November, 2022.
Copy Citation
Accumulating chemotherapeutic drugs such as doxorubicin within a tumor while limiting the drug dose to normal tissues is a central goal of drug delivery with nanoparticles. Liposomal products such as Doxil® represent one of the marked successes of nanoparticle-based strategies. To replicate this success for cancer treatment, many approaches with nanoparticles are being explored in order to direct and release chemotherapeutic agents to achieve higher accumulation in tumors.
polymers
histidine
imidazole
doxorubicin
1. Introduction
Nanoparticles and the drugs they carry are exposed to dramatically different pH ranges once they leave the blood vessels that feed the tumor [1]. While the extracellular environment and the endosomes are acidic, the intracellular pH of a tumor cell is alkaline. The extracellular acidic environment of a tumor (TE) offers the potential to target the tumor. There are relatively few other tissues (e.g., renal proximal tubule, gastric lumen) or diseases (e.g., arthritic joints) that have an acidic environment [2][3][4][5] The acidity of the TE ranges from a pH of 6.5 to 7.2, and several mechanisms contribute to this acidity. Although this extracellular tumor acidity, first noted by Warburg, was initially thought to be due to enhanced glycolysis (aerobic and anaerobic) and increased levels of lactic acid [6][7], the reason for the acidity is still being examined. Increased glycolytic pathway activity is intrinsic to almost all cancer cells, whether they are located near or far from the blood vessels. Because of activating mutations, some cancers have a higher rate of glycolysis than others and this can affect the TE. Interestingly, due to increased glycolysis and enhanced glucose transport, the administration of glucose may further lower the extracellular pH of a tumor [8][9][10]. In addition to the production of lactic acid, the pentose pathway, sodium–hydrogen exchanges (particularly NHE1), and carbonic acid anhydrase activity may have important roles lowering the extracellular pH [11][12][13].
Because of the increased acidity of tumors, a pH gradient exists between normal tissues and perivascular tumor cells, enabling targeting of the tumor by pH-sensitive nanoparticles. Within a tumor, however, spatial–temporal differences in the extracellular pH of the tumor exist and these differences are dependent on the size of the tumor, the blood vessel density, the quality and organization of the blood vessels, and the lymphatics [14][15]. While the extracellular pH in necrotic areas of tumors has been studiously avoided in many studies, the pH of hypoxic (non-necrotic) regions has been found to be more acidic than that of regions adjacent to the vessels, primarily because of the increased production of CO2 and protons (lactic acid) associated with poor perfusion [16].
Although some pH-dependent nanoparticles have been designed to disintegrate in the extracellular environment, many particles remain partially intact. With their increased charge, these particles likely have enhanced absorption onto the negatively charged surface of tumor cells, resulting in greater endosomal uptake. After the uptake of the particles into the cell’s endosomes, the vesicles become progressively more acidic, with late endosomes reaching a pH of 5. With this lower pH, the likelihood that the pH-dependent particles will be disrupted (i.e., charge–charge repulsion) increases, resulting in the release of the hydrophobic drug. The second function that pH-dependent polymers may have in drug release is the disruption of endosomes. Two mechanisms have been proffered, and they are not mutually exclusive. Upon protonation of pH-dependent polymers (and nanoparticles), endosomes burst through osmotic swelling or by direct interaction of the endosomal membrane with the charged polymers [17][18][19].
2. Linear Imidazole-Modified Peptides and Polymers
Using block copolymers with a poly-L-histidine (PLH) domain, the Bae group conducted a series of seminal studies on the release of hydrophobic drugs from micelles in the acidic extracellular environment of tumors [20][21][22][23]. After comparing different molecular weights of the PLH segments (prepared by ring-opening polymerization), the molecular weight of 5000 was selected for the PLH component of the copolymer because of the lower critical micelle concentration (CMC) (2.3 μg/mL). Interestingly, the addition of polyethylene glycol (PEG) to the PLH domain (PEG-PLH) increased the pKa from 6.5 to 7.0. As with most of the histidine-containing micelles discussed, the CMC of the PEG-PLH micelles was inversely correlated with the pH. The pH dependence of the CMC and the transmittance of PEG-PLH micelles were consistent with the protonation of the imidazole groups and their disruption at mildly acidic pH levels. Although many pH-buffering micelles increased in size at acidic pH levels, these micelles became smaller as the pH was lowered [20]. The PEG-PLH micelles released about 42%, 75%, and 85% of the Dox at pH 7.4, 6.8, and 5.0, respectively, over twenty-four hours at 37 °C [21]. The enhanced release of Dox from micelles at lower pH levels was further corroborated by the increased inhibition of MCF-7 cancer cells in more acidic media [21][22]. The group also determined that Dox-loaded PEG-PLH micelles had improved pharmacokinetics, enhanced tumor accumulation, and reduced tumor size compared to free Dox [22].
To improve the stability at physiological pH and the release of Dox at the mildly acidic pH levels found in the extracellular tumor environment, a blend of PEG-PLH and PEG- poly-L-lactide (PEG-PLA) micelles was investigated [21]. Compared to other PEG-PLH/PEG-PLA mixed micelles, the blend of PEG-PLH (75%) and PEG-PLA (25%) micelles showed improved release profiles for Dox at mildly acidic pH levels, reflective of the extracellular pH of tumors. While about 30% of the Dox was released from the optimal mixed micelle preparation at pH 7.4, nearly 75% was released at pH 6.8 over twenty-four hours. Concomitant with the release kinetics, the 75:25 mixed micelles showed enhanced cytotoxic activity toward MCF-7 cells incubated in media at pH 6.8 [21]. Furthermore, when Dox-loaded PEG-PLA/PEG-PLH micelles were decorated with the folate ligand, their inhibition of MCF-7 and drug-resistant MCF-7-DoxR cells was significantly greater than that of the untargeted micelles. Notably, free Dox had little effect on the MCF-7-DoxR xenografts. In contrast, the Dox-loaded pH-sensitive micelles, particularly the folate-targeted micelles, had a marked effect on the growth of the xenografts [23]. In a later report, the authors indicated that long-term stability was an issue for these micelles [24].
The improved kinetics of Dox release from mixed micelles with the hydrophobic poly-L-lactide (PLA) copolymer has stimulated interesting designs with triblock PLH-containing copolymers [25][26]. The Bae group designed an interesting PLA-PEG-PLH triblock copolymer that self-assembled into flower-like micelles (Figure 1 and Figure 2A). While the sandwich hydrophilic PEG segment was on the surface, the PLA and PLH segments on the ends made up the inner core. These micelles were approximately 80 nm in size at pH 7.4 and swelled to 580 nm at pH 6.6 [25]. Related to these size changes, the cumulative release of Dox from the micelles was 35% higher at pH 6.8 than the release at pH 7.4. The amounts of Dox released at various pH levels and the in vitro antitumor efficacy of these triblock micelles were similar to those of the mixed micelles [21].
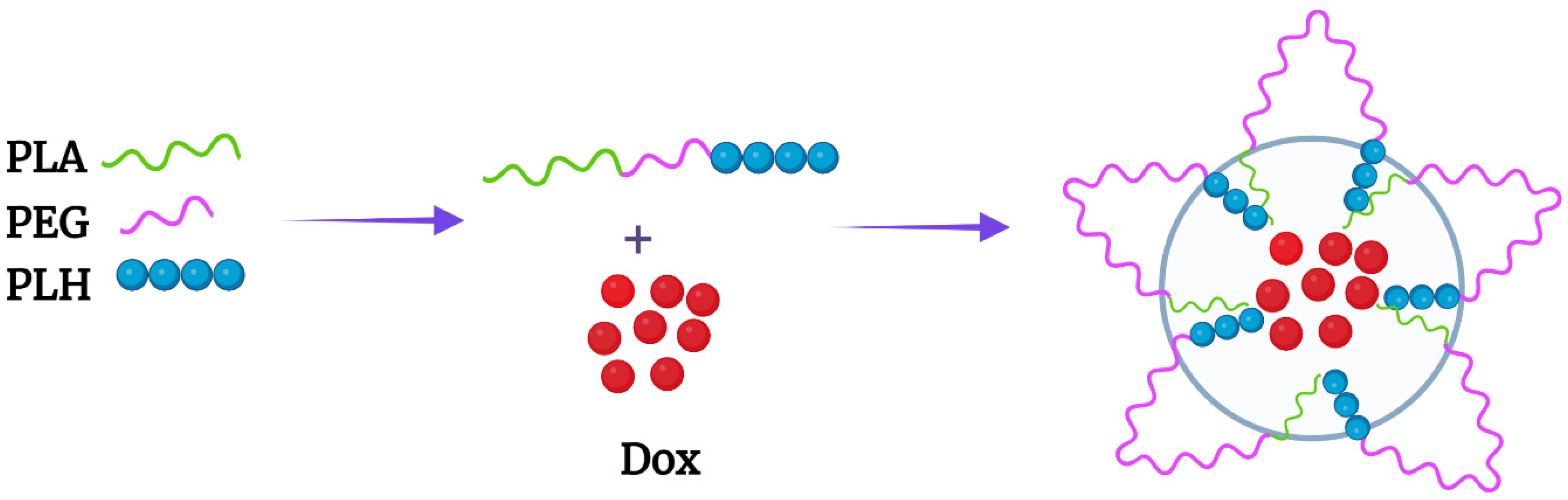
Figure 1. Flower-like micelle formed by the PLA-b-PEG-b-PLH triblock copolymer. Dox was incorporated within the PLA and PLH hydrophobic core.

Figure 2. Chemical structures of the (A) triblock copolymer and (B) the block copolymers mPEG-PLH and PEG-DSPE, which formed micelles. The numbers of monomeric units in the block copolymer are represented by X, Y, and Z.
Liu et al. reported somewhat different findings for micelles prepared with the same components but in a different order, a triblock mPEG-b-PLH-PLA copolymer [26]. In contrast to the PEG being sandwiched between two hydrophobic polymers, PEG was external to these domains. In a twenty-four hour period, about 35% and 80% of the Dox was released from the micelles at pH 7.4 and pH 5.0, respectively. Because there was no quick release of Dox from these micelles at pH 5, the authors speculated that Dox was primarily located in the hydrophobic PLA core at this acidic pH. The greater degree of polymerization of PLA compared to other block polymers [25][27] may have played a role in the entrapment of Dox at the lower pH. Significant amounts of Dox were unlikely to have been released from these micelles at pH values between 6.3 and 7.0 since no burst release was observed at pH 5.0. In any event, no release data were reported at a pH of 6.3, even though the micelles reached their maximum size at this pH prior to their becoming smaller. In contrast, there was a burst release of Dox at pH 6.5 and 5.0 in which PLH formed the inner core of the micelle (mPEG-PLA-PLH) [28]. Therefore, the order of the triblock polymer and perhaps the length of the polymeric block components may be important in determining whether micelles release Dox at mildly acidic pH levels between 6.5 and 7.0.
Compared to PLA, the copolymer poly(lactide-co-glycolide) (PLGA) is generally preferred because its biocompatibility, biodegradability, and mechanical strength can be controlled by varying the ratios of its monomers. Li et al. synthesized block copolymers of PLGA and tocopheryl polyethylene glycol succinate (TPGS-PLGA) with or without poly-L-histidine (TPGS-PLGA-PLH) [27]. Among these components, the PEG-containing TPGS segment formed the outer shell, improving the stability of the nanoparticles and inhibiting the multidrug resistance (MDR) transporter, while both the hydrophobic PLGA middle and PLH inner shell components entrapped Dox efficiently. Moreover, the Dox-loaded particles with PLH showed enhanced release of Dox at acidic pH and more significant cytotoxicity toward Dox-sensitive and -resistant breast cancer cells compared to particles without histidine. Although these results demonstrated the importance of PLH in the release of Dox [27], the Dox readily leaked from the cores of the two nanoparticles at pH 7.4 (TPGS-PLGA-PLH, TPGS-PLGA, ~55% in twelve hours).
To reduce the release of Dox from nanoparticles, Johnson et al. synthesized a diblock copolymer composed of poly(2-hydroxyethyl methacrylate (pHEMA) and PLH domains (p(HEMA)-b-PLH) [29]. The number of monomeric histidines in the PLH domain markedly affected the biophysical characteristics of the micelle and the release profile of the Dox. The pHEMA component formed a hydrophilic shield, whereas the polyhistidine formed a hydrophobic core incorporating the Dox. Upon varying the number of histidines (15, 25, 35, and 45) in the PLH domain, the size of the Dox-loaded micelle was affected, ranging in size from about 124 to 194 nm. The more histidines in the diblock copolymer, the larger the Dox-loaded micelle and the greater the release rate of Dox at physiological pH and acidic pH. Despite the differences in size and release rates of Dox at different pH levels, the micelles with varying histidine content showed similar cytotoxicity for cancer cells yet reduced cytotoxicity compared to free Dox. Notably, cytotoxicity was progressively increased when the Dox-loaded micelles were incubated with the cells at lower pH levels. In a later study from the same group, a similar pH-dependent enhanced release of Dox was observed from micelles formed from the triblock copolymer (PEG- p(Lys)25-p(His)100) [30][31]. Although nucleic acids could presumably have been loaded into these micelles, only Dox was. It is possible that the nearly 50% release of Dox from the micelles at pH 7.4 was due to the self-repelling poly-L-lysine layer, and, with the addition of siRNA to neutralize the poly-L-lysine component, the release of the drug might have been reduced, as reported by others [31].
With their high numbers of hydroxyl groups, polysaccharides such as dextran likely behave similarly to PEG in reducing nonspecific interactions of serum proteins with nanoparticles. Dextran is a neutral, biodegradable polysaccharide made up of glucose molecules of 1,6-glycosidic linkages with varying degrees of length and branching. The lower the degree of branching of dextran, the fewer the allergic side effects [32]. Moreover, dextran may have advantages over PEG, since severe allergic side effects may occur less frequently [33][34].
A dextran-b-poly(L-histidine) (Dex-b-PLH) block copolymer was synthesized by Hwang and his colleagues [35]. Poly-L-histidine of two molecular weights (~5800 and ~12,600) was conjugated to the reductive end of the low-molecular-weight dextran (~6000). There were modest differences in the drug loading capacity, pH-dependent size, and release of Dox between these two Dex-b-PLH particles. The release of Dox at both neutral and acidic pH levels from particles containing the higher-molecular-weight (MW) PLH segment was reduced compared to those with the lower-MW PLH segment. This was in contrast to the micelles formed from the diblock polymer (p(HEMA)-b-PLH), in which the higher-MW PLH domain enhanced the release of Dox [29]. Whether this was due to the different block copolymers conjugated to the PLH domain in the two studies is not known. Still, with Dex-b-PLH micelles at pH 7.4, about 40% of Dox was released from the particles with the high-MW PLH in twenty-four hours. Additionally, the cellular uptake rate of Dox-loaded Dex-PLH was higher than that of free Dox, particularly at the lower pH. Consistent with these uptake studies, the cytotoxicity of Dox-loaded particles toward cholangiocarcinoma cells (HuCC-T1) was pH-dependent and greater than that of free Dox [35].
Similarly to dextran, the auricularia auricula polymer (AAP) is a water-soluble polysaccharide that is biodegradable and has potential as a drug carrier. In contrast to dextran, AAP has not been as well characterized as dextran and may be immunogenic [36]. Wang and colleagues formed a nanoparticle named AAP-His by conjugating histidines to a high-molecular-weight AAP. Unlike most polymers described which contain PLH, the hydroxyl groups on the monomeric unit of AAP were modified by a single histidine. The poorly water-soluble drug paclitaxel (PTX) was incorporated within the hydrophobic unprotonated histidine segment of the micelles. The size and the in vitro cytotoxicity of the PTX-loaded AAP-His micelles were pH-responsive. With longer incubation times (seventy-two hours) and at lower drug dosages (0.01 μg/mL), the PTX micelles inhibited the viability of MCF-7 cells to a greater degree than the free drug (MTT assay). The cumulative release rates over a twelve-hour period at pH 7.4 and 5.0 at 37 °C were about 65% and 85%, respectively. If more than a single histidine was conjugated to the monomeric unit of AAP, improved retention at pH 7.4 and greater pH-dependent release of PTX may occur. Notably, in tumor-bearing (sarcoma-180) mouse models, these PTX-loaded micelles significantly inhibited the tumor weight by about 60% more than free PTX (p < 0.01) [37]. Although aspects of the design of these AAP-His nanoparticles may be helpful for future drug delivery systems, the use of AAP may be limited because of the induction of cytokines [36]. The CMC was not given in this or the prior dextran study.
It has been suggested that negatively charged nanoparticles have fewer undesirable effects than positively charged nanoparticles. In an interesting report, it was noted that negatively charged micelles at physiological pH that progressively become positive in a slightly acidic environment may target tumors [38]. Specifically, if the charge-reversed micelles become positive (or at least more positive) between 6.5 and 7.0, cellular uptake by tumor cells could be increased significantly. Kim et al. developed one of the two charge-reversed micelles discussed. After the diblock PEG-PAsp (polyaspartic) copolymer was synthesized, 60% of the PAsp groups were modified with imidazole groups (PEG-PAsp-(im). These PEG-PAsp-(im) micelles, formed via the thin-film rehydration method, had zeta potentials ranging from −16 at pH 7.4 to +1 at pH 4.0. Furthermore, the CMC changed dramatically between pH 7.0 and 6.5, going from about 5 to 65 μg/mL. Consistent with the CMC changes, the size increased from 110 to 275 nm between pH 7.4 and 6.5, respectively. As a result, these micelles have the potential to release hydrophobic drugs at pH levels consistent with the extracellular pH levels of tumors. Although no uptake studies were done with these micelles, researchers think that the less negative zeta potential of the micelles at pH 6.5 would increase their uptake.
One significant problem has been the poor retention of hydrophobic drugs within histidine-containing nanoparticles or micelles at pH 7.4. This was partially addressed in a study by Kim et al. in which a copolymer of histidine and phenylalanine was conjugated to the hydrophilic PEG (PEG-PLH/F) [39]. Notably, the pKa of the polymer varied based on the percentage of phenylalanine and the presence or absence of PEG. As the percentage of phenylalanine increased, the pKa of the diblock PEG-PLH/F decreased. The micelles in which the peptide segment of the block copolymer had a higher molecular weight (Mw of peptide: 5600) released about 5% of pyrene after two days at physiological pH. In contrast, the micelles released about 45% and 60% of the pyrene at pH 6.4 and 6.0, respectively. Unfortunately, these investigations do not seem to have explored this particle further. As a result, it is not known whether the release of pyrene from these micelles correlates with the release of Dox, PTX, or other hydrophobic drugs. More studies are needed to discover whether these histidine-containing micelles stably incorporate hydrophobic drugs at physiological pH.
Of the co-block polymers, only the PTX-loaded micelles developed by Wu et al. were tested for long-term stability [40]. These mixed micelles, made of mPEG-PLH and PEG-1,2-distearoylphostidylethanolamine (PEG-DSPE) copolymers in a ~1:1 weight ratio, delivered PTX effectively (Figure 2B and Figure 3). Notably, these micelles were stable and released about 10% of PTX at pH 7.4, whereas the micelles released nearly 50% and 65% of PTX at pH 6.0 and 5.0, respectively, over the same time period (twenty-four hours). The release of PTX at pH 5.0 was dramatic, with a burst release of 60% (twelve hours). Consistent with the PTX release data, 4T1 cells incubated in media at pH 5.8 were very sensitive to the cytotoxic effects of the PTX-loaded micelles compared to cells incubated in media at the same pH with free PTX. Since the pH 5.8 medium had no cytotoxic effect on 4T1 cells, the toxicity was attributed to the PTX or the PTX-loaded mixed micelles. Moreover, the inclusion of an antinucleosomal antibody (2C5-PEG-DSPE) on the surface of the micelles further enhanced their cytotoxicity. Notably, with PLH and DSPE forming the hydrophobic core, the PTX-containing micelles were stable for several months at 4 °C. Since these micelles have several attractive properties, this formulation deserves further study. However, because of the size of the 2C5 monoclonal antibody and its possible lack of tumor specificity [41], single-chain antibodies, as well as other small tumor-specific ligands, should be investigated with this mixed micelle preparation.
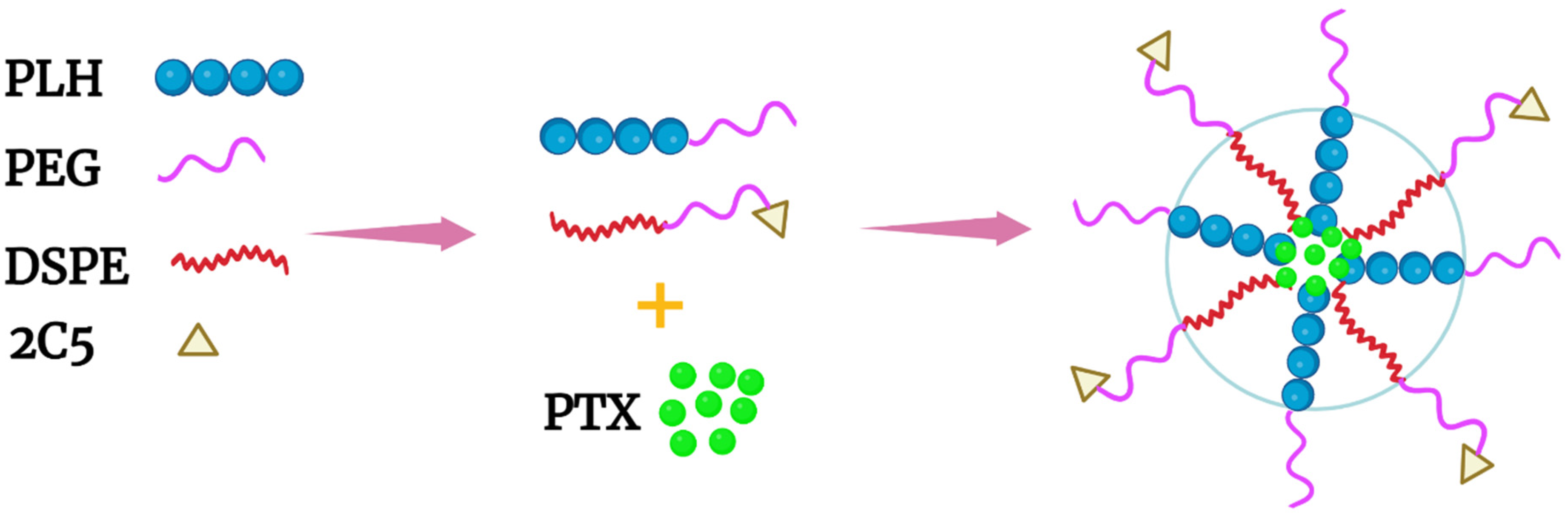
Figure 3. Schematic of a mixed micelle formed with the copolymers PEG-PLH, PEG-DSPE, and 2C5-PEG-DSPE. The hydrophobic drug PTX was incorporated within the inner core, which comprised PLH and DSPE.
Another promising approach for delivering Dox was reported by Liang et al., who entrapped a histidine–arginine co-peptide within their NPs [42]. The PEG-Dox conjugate, together with the hydrophobic PDPA polymer (also named PDPAEMA), was mixed with various ratios of the H4R4 co-peptide (HHHHRRRR) (Figure 4). The H4R4 was incorporated into the NPs to enhance endosomal escape/lysis of the PEG-Dox conjugate. Importantly, the H4R4 did not affect the release of the PEG-Dox conjugate. The PDPA, with a pKa of 6.4, was the primary factor in disrupting the NPs and releasing the H4R4 co-peptide and the PEG-Dox conjugate. At a weight percentage of 14%, the incorporated H4R4 increased the cytotoxicity 30-fold compared to the Dox-loaded NPs. This underscores how vital endosomal lysis was in enhancing the efficacy of Dox. Notably, the Dox-loaded NPs were quite stable and released about 10% of the Peg-Dox at pH 7.4, while the NPs released about 90% of the PEG-Dox at pH 5.5 over the same time (thirty-six hours). It is likely that most of the Dox was bioavailable from the PEG-Dox conjugate, since the Dox-loaded NPs showed markedly more cytotoxicity than the free Dox toward HeLa cells (IC50: 0.063 vs. 1 μM). An interesting comparison would perhaps be to examine the non-pH-dependent amide bond between PEG and Dox using a pH-dependent linkage [43]. Nonetheless, the amide bond seemed to be readily cleaved in HeLa cells.

Figure 4. Micelle formed with PEG-Dox conjugate and the hydrophobic PDPA polymer. The H4R4 peptide enhanced endosomal lysis, increasing Dox release into the cytosol.
Several questions arise by reserchers. Would incorporating the H4R4 peptide into histidine-rich or other pH-dependent micelles enhance the cytosolic delivery of the drug? Since the R4 peptide was likely on the surface, would a longer histidine segment add greater stability to the micelle? Why did the pH-sensitive PDPA not effectively lyse endosomes? It is of note that most block or grafted PLH polymers discussed were not tested for their endosomal lysis potential.
References
- Zhang, X.; Lin, Y.; Gillies, R.J. Tumor pH and its measurement. J. Nucl. Med. 2010, 51, 1167–1170.
- DuBose, T.D., Jr.; Pucacco, L.R.; Seldin, D.W.; Carter, N.W.; Kokko, J.P. Microelectrode determination of pH and PCO2 in rat proximal tubule after benzolamide: Evidence for hydrogen ion secretion. Kidney Int. 1979, 15, 624–629.
- Fallingborg, J. Intraluminal pH of the human gastrointestinal tract. Dan. Med. Bull. 1999, 46, 183–196.
- Goldie, I.; Nachemson, A. Synovial pH in rheumatoid knee joints. II. The effect of local corticosteroid treatment. Acta Orthop. Scand. 1970, 41, 354–362.
- Xiong, F.; Qin, Z.; Chen, H.; Lan, Q.; Wang, Z.; Lan, N.; Yang, Y.; Zheng, L.; Zhao, J.; Kai, D. pH-responsive and hyaluronic acid-functionalized metal–organic frameworks for therapy of osteoarthritis. J. Nanobiotechnol. 2020, 18, 139.
- Warburg, O. On the origin of cancer cells. Science 1956, 123, 309–314.
- Warburg, O.; Posener, K.; Negelein, E. Uber den Stoffwechsel der Carcinomzelle. Biochem. Zeitsch 1924, 152, 309–344.
- Naeslund, J.; Swenson, K.E. Investigations on the pH of malignant tumors in mice and humans after the administration of glucose. Acta Obstet. Gynecol. Scand. 1953, 32, 359–367.
- Eden, M.; Haines, B.; Kahler, H. The pH of rat tumors measured in vivo. J. Natl. Cancer Inst. 1955, 16, 541–556.
- Volk, T.; Jahde, E.; Fortmeyer, H.P.; Glusenkamp, K.H.; Rajewsky, M.F. pH in human tumour xenografts: Effect of intravenous administration of glucose. Br. J. Cancer 1993, 68, 492–500.
- Payen, V.L.; Porporato, P.E.; Baselet, B.; Sonveaux, P. Metabolic changes associated with tumor metastasis, part 1: Tumor pH, glycolysis and the pentose phosphate pathway. Cell. Mol. Life Sci. 2016, 73, 1333–1348.
- Gillies, R.J. Cancer heterogeneity and metastasis: Life at the edge. Clin. Exp. Metastasis 2021, 39, 15–19.
- Perez-Herrero, E.; Fernandez-Medarde, A. The reversed intra- and extracellular pH in tumors as a unified strategy to chemotherapeutic delivery using targeted nanocarriers. Acta Pharm. Sin. B 2021, 11, 2243–2264.
- Van Sluis, R.; Bhujwalla, Z.M.; Raghunand, N.; Ballesteros, P.; Alvarez, J.; Cerdan, S.; Galons, J.P.; Gillies, R.J. In vivo imaging of extracellular pH using 1H MRSI. Magn. Reson. Med. 1999, 41, 743–750.
- Gillies, R.J.; Raghunand, N.; Karczmar, G.S.; Bhujwalla, Z.M. MRI of the tumor microenvironment. J. Magn. Reson. Imaging 2002, 16, 430–450.
- Parks, S.K.; Cormerais, Y.; Pouyssegur, J. Hypoxia and cellular metabolism in tumour pathophysiology. J. Physiol. 2017, 595, 2439–2450.
- Behr, J.P.; Demeneix, B.; Loeffler, J.P.; Perez-Mutul, J. Efficient gene transfer into mammalian primary endocrine cells with lipopolyamine-coated DNA. Proc. Natl. Acad. Sci. USA 1989, 86, 6982–6986.
- Vermeulen, L.M.P.; De Smedt, S.C.; Remaut, K.; Braeckmans, K. The proton sponge hypothesis: Fable or fact? Eur. J. Pharm. Biopharm. 2018, 129, 184–190.
- Chen, Q.R.; Zhang, L.; Luther, P.W.; Mixson, A.J. Optimal transfection with the HK polymer depends on its degree of branching and the pH of endocytic vesicles. Nucleic Acids Res. 2002, 30, 1338–1345.
- Lee, E.S.; Shin, H.J.; Na, K.; Bae, Y.H. Poly(L-histidine)-PEG block copolymer micelles and pH-induced destabilization. J. Control. Release 2003, 90, 363–374.
- Lee, E.S.; Na, K.; Bae, Y.H. Polymeric micelle for tumor pH and folate-mediated targeting. J. Control. Release 2003, 91, 103–113.
- Gao, Z.G.; Lee, D.H.; Kim, D.I.; Bae, Y.H. Doxorubicin loaded pH-sensitive micelle targeting acidic extracellular pH of human ovarian A2780 tumor in mice. J. Drug Target. 2005, 13, 391–397.
- Lee, E.S.; Na, K.; Bae, Y.H. Doxorubicin loaded pH-sensitive polymeric micelles for reversal of resistant MCF-7 tumor. J. Control. Release 2005, 103, 405–418.
- Oh, K.T.; Lee, E.S.; Kim, D.; Bae, Y.H. L-histidine-based pH-sensitive anticancer drug carrier micelle: Reconstitution and brief evaluation of its systemic toxicity. Int. J. Pharm. 2008, 358, 177–183.
- Lee, E.S.; Oh, K.T.; Kim, D.; Youn, Y.S.; Bae, Y.H. Tumor pH-responsive flower-like micelles of poly(L-lactic acid)-b-poly(ethylene glycol)-b-poly(L-histidine). J. Control. Release 2007, 123, 19–26.
- Liu, R.; Li, D.; He, B.; Xu, X.; Sheng, M.; Lai, Y.; Wang, G.; Gu, Z. Anti-tumor drug delivery of pH-sensitive poly(ethylene glycol)-poly(L-histidine-)-poly(L-lactide) nanoparticles. J. Control. Release 2011, 152, 49–56.
- Li, Z.; Qiu, L.; Chen, Q.; Hao, T.; Qiao, M.; Zhao, H.; Zhang, J.; Hu, H.; Zhao, X.; Chen, D.; et al. pH-sensitive nanoparticles of poly(L-histidine)-poly(lactide-co-glycolide)-tocopheryl polyethylene glycol succinate for anti-tumor drug delivery. Acta Biomater. 2015, 11, 137–150.
- Jia, L.; Jia, N.; Gao, Y.; Hu, H.; Zhao, X.; Chen, D.; Qiao, M. Multi-Modulation of Doxorubicin Resistance in Breast Cancer Cells by Poly(l-histidine)-Based Multifunctional Micelles. Pharmaceutics 2019, 11, 385.
- Johnson, R.P.; Jeong, Y.I.; Choi, E.; Chung, C.W.; Kang, D.H.; Oh, S.O.; Suh, H.; Kim, I. Biocompatible Poly (2-hydroxyethyl methacrylate)-b-poly(L-histidine) Hybrid Materials for pH-Sensitive Intracellular Anticancer Drug Delivery. Adv. Funct. Mater. 2012, 22, 1058–1068.
- Johnson, R.P.; Uthaman, S.; John, J.V.; Lee, H.R.; Lee, S.J.; Park, H.; Park, I.-K.; Suh, H.; Kim, I. Poly(PEGA)-b-poly(l-lysine)-b-poly(l-histidine) Hybrid Vesicles for Tumoral pH-Triggered Intracellular Delivery of Doxorubicin Hydrochloride. ACS Appl. Mater. Interfaces 2015, 7, 21770–21779.
- Zhu, W.J.; Yang, S.D.; Qu, C.X.; Zhu, Q.L.; Chen, W.L.; Li, F.; Yuan, Z.Q.; Liu, Y.; You, B.G.; Zhang, X.N. Low-density lipoprotein-coupled micelles with reduction and pH dual sensitivity for intelligent co-delivery of paclitaxel and siRNA to breast tumor. Int. J. Nanomed. 2017, 12, 3375–3393.
- Ljungström, K.G.; Renck, H.; Strandberg, K.; Hedin, H.; Richter, W.; Widerlöv, E. Adverse reactions to dextran in Sweden 1970–1979. Acta Chir. Scand. 1983, 149, 253–262.
- Wylon, K.; Dölle, S.; Worm, M. Polyethylene glycol as a cause of anaphylaxis. Allergy Asthma Clin. Immunol. 2016, 12, 67.
- Renck, H.; Ljungström, K.G.; Hedin, H.; Richter, W. Prevention of dextran-induced anaphylactic reactions by hapten inhibition. III. A Scandinavian multicenter study on the effects of 20 mL dextran 1, 15%, administered before dextran 70 or dextran 40. Acta Chir. Scand. 1983, 149, 355–360.
- Hwang, J.H.; Choi, C.W.; Kim, H.W.; Kim, D.H.; Kwak, T.W.; Lee, H.M.; Kim, C.H.; Chung, C.W.; Jeong, Y.I.; Kang, D.H. Dextran-b-poly(L-histidine) copolymer nanoparticles for ph-responsive drug delivery to tumor cells. Int. J. Nanomed. 2013, 8, 3197–3207.
- Bao, Z.; Yao, L.; Zhang, X.; Lin, S. Isolation, purification, characterization, and immunomodulatory effects of polysaccharide from Auricularia auricula on RAW264.7 macrophages. J. Food Biochem. 2020, 44, e13516.
- Wang, Y.; Li, P.; Chen, F.; Jia, L.; Xu, Q.; Gai, X.; Yu, Y.; Di, Y.; Zhu, Z.; Liang, Y.; et al. A novel pH-sensitive carrier for the delivery of antitumor drugs: Histidine-modified auricularia auricular polysaccharide nano-micelles. Sci. Rep. 2017, 7, 4751.
- Kim, J.H.; Oh, Y.T.; Lee, K.S.; Yun, J.M.; Park, B.T.; Oh, K.T. Development of a pH-sensitive polymer using poly(aspartic acid-graft-imidazole)-block-poly(ethylene glycol) for acidic pH targeting systems. Macromol. Res. 2011, 19, 453–460.
- Kim, G.M.; Bae, Y.H.; Jo, W.H. pH-induced Micelle Formation of Poly(histidine-co-phenylalanine)-block-Poly(ethylene glycol) in Aqueous Media. Macromol. Biosci. 2005, 5, 1118–1124.
- Wu, H.; Zhu, L.; Torchilin, V.P. pH-sensitive poly(histidine)-PEG/DSPE-PEG co-polymer micelles for cytosolic drug delivery. Biomaterials 2013, 34, 1213–1222.
- Mendes, L.P.; Rostamizadeh, K.; Gollomp, K.; Myerson, J.W.; Marcos-Contreras, O.A.; Zamora, M.; Luther, E.; Brenner, J.S.; Filipczak, N.; Li, X.; et al. Monoclonal antibody 2C5 specifically targets neutrophil extracellular traps. mAbs 2020, 12, 1850394.
- Liang, K.; Richardson, J.J.; Ejima, H.; Such, G.K.; Cui, J.; Caruso, F. Peptide-tunable drug cytotoxicity via one-step assembled polymer nanoparticles. Adv. Mater. 2014, 26, 2398–2402.
- Lee, C.C.; Gillies, E.R.; Fox, M.E.; Guillaudeu, S.J.; Frechet, J.M.; Dy, E.E.; Szoka, F.C. A single dose of doxorubicin-functionalized bow-tie dendrimer cures mice bearing C-26 colon carcinomas. Proc. Natl. Acad. Sci. USA 2006, 103, 16649–16654.
More
Information
Subjects:
Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
2 times
(View History)
Update Date:
28 Nov 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




