Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alexandra Lazăr | -- | 1175 | 2022-11-16 08:05:42 | | | |
| 2 | Sirius Huang | Meta information modification | 1175 | 2022-11-17 02:57:26 | | | | |
| 3 | Sirius Huang | Meta information modification | 1175 | 2022-11-21 02:07:43 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Lazar, A.E.; Gherghinescu, M.C. Airway Ultrasound for Anesthesia and Intensive Care Patients. Encyclopedia. Available online: https://encyclopedia.pub/entry/34828 (accessed on 07 February 2026).
Lazar AE, Gherghinescu MC. Airway Ultrasound for Anesthesia and Intensive Care Patients. Encyclopedia. Available at: https://encyclopedia.pub/entry/34828. Accessed February 07, 2026.
Lazar, Alexandra Elena, Mircea Constantin Gherghinescu. "Airway Ultrasound for Anesthesia and Intensive Care Patients" Encyclopedia, https://encyclopedia.pub/entry/34828 (accessed February 07, 2026).
Lazar, A.E., & Gherghinescu, M.C. (2022, November 16). Airway Ultrasound for Anesthesia and Intensive Care Patients. In Encyclopedia. https://encyclopedia.pub/entry/34828
Lazar, Alexandra Elena and Mircea Constantin Gherghinescu. "Airway Ultrasound for Anesthesia and Intensive Care Patients." Encyclopedia. Web. 16 November, 2022.
Copy Citation
Ultrasound is an everyday diagnostic tool. In anesthesia and intensive care, it has a role as an adjuvant for many procedures, including the evaluation of the airway. Ultrasound airway evaluation can help predict a difficult airway, visualize the proper positioning of an intubation cannula, or evaluate the airway post-intubation.
ultrasound
airway
difficult intubation
anesthesia
intensive care
1. Introduction
Ultrasound became a tool used by all specialists, regardless of their field of practice. There are very few medical fields where ultrasound is not used. Its non-invasive character and the possibility of visualizing deep structures and tissues allow specialists to provide better and safer care for their patients [1]. The ultrasound equipment is both suitable for emergent and scheduled procedures, although its exact role in emergencies is not well established [1].
Ultrasound devices are becoming more and more suitable for every procedure, and the producers have significantly improved the design and portability. These features, along with the possibility to connect the ultrasound to smart devices, allow the specialists to have their “pocket ultrasound” on hand every time, and most importantly, everywhere it might be needed [2].
However, possessing an advanced device is not the key to a correct image interpretation. A not-so-steep learning curve allows the specialists to choose the right window or transducer to obtain the best from the ultrasound machine [3].
Airway ultrasound is implemented more and more in the daily practice of clinicians, and it is proven to be useful even in some emergencies, such as finding the right position for performing an emergent cricothyrotomy [4].
The evaluation of the airway patency is based mainly on clinical signs and some paraclinical investigations. Their scope is to predict a difficult airway before any medical gesture upon the airway is performed, so the proper tools and maneuvers can be taken ahead by the specialists. Among the clinical signs used, is the Mallampati scale, the thyromental distance, the distance between the incisors, mouth opening, and neck mobility. Studies concluded that alone, these signs have a poor predictability of a difficult airway, but combined, their power of prediction increases [5][6][7][8]. However, these signs are subjective and prone to mistakes, hence a better assessment tool is sought for a difficult airway prediction.
2. Perioperative Ultrasound Airway Evaluation Utility
Difficult airway prediction still presents biases nowadays, and although the worse situation when the patient cannot be ventilated or intubated is rare, the impact can be disastrous [9]. The preoperative meeting with the anesthesiologist can uncover a few signs related to a possible difficult intubation, such as a reduced mouth opening, a reduced thyromental distance, the impossibility to bite the upper lip, or a high Mallampati grade [10]. However, these are prone to subjectivism and sometimes they do not describe the real situation which can be visible in a direct laryngoscopy, the Cormack–Lehane grading, or after the induction of the anesthesia, when the patient cannot be ventilated [8]. These are just a few situations where ultrasound can be of use, because it offers the possibility of an anatomy evaluation, which may uncover possible anatomical modifications that impede the proper ventilation or intubation.
3. Technical Aspects of an Airway Ultrasound
A quick ultrasound scan of the airway can be used to visualize the anatomy of the airway, before a laryngoscopy, to exclude possible difficult intubation. To obtain a good view of the airway, the recommended ultrasound probes are the linear low-frequency probes for structures closer to the skin, and the curved high-frequency probes are preferred for deeper situated structures, [11].
The proper patient position for an ultrasound airway evaluation is supine, with the neck extended.
The ultrasound airway identifiable structures of interest, for the anesthesiologist, are the mouth, tongue, the oro-, and hypopharynx, hyoid bone, larynx, vocal cords, cricothyroid membrane, cricoid cartilages, trachea, and esophagus. (Figure 1)
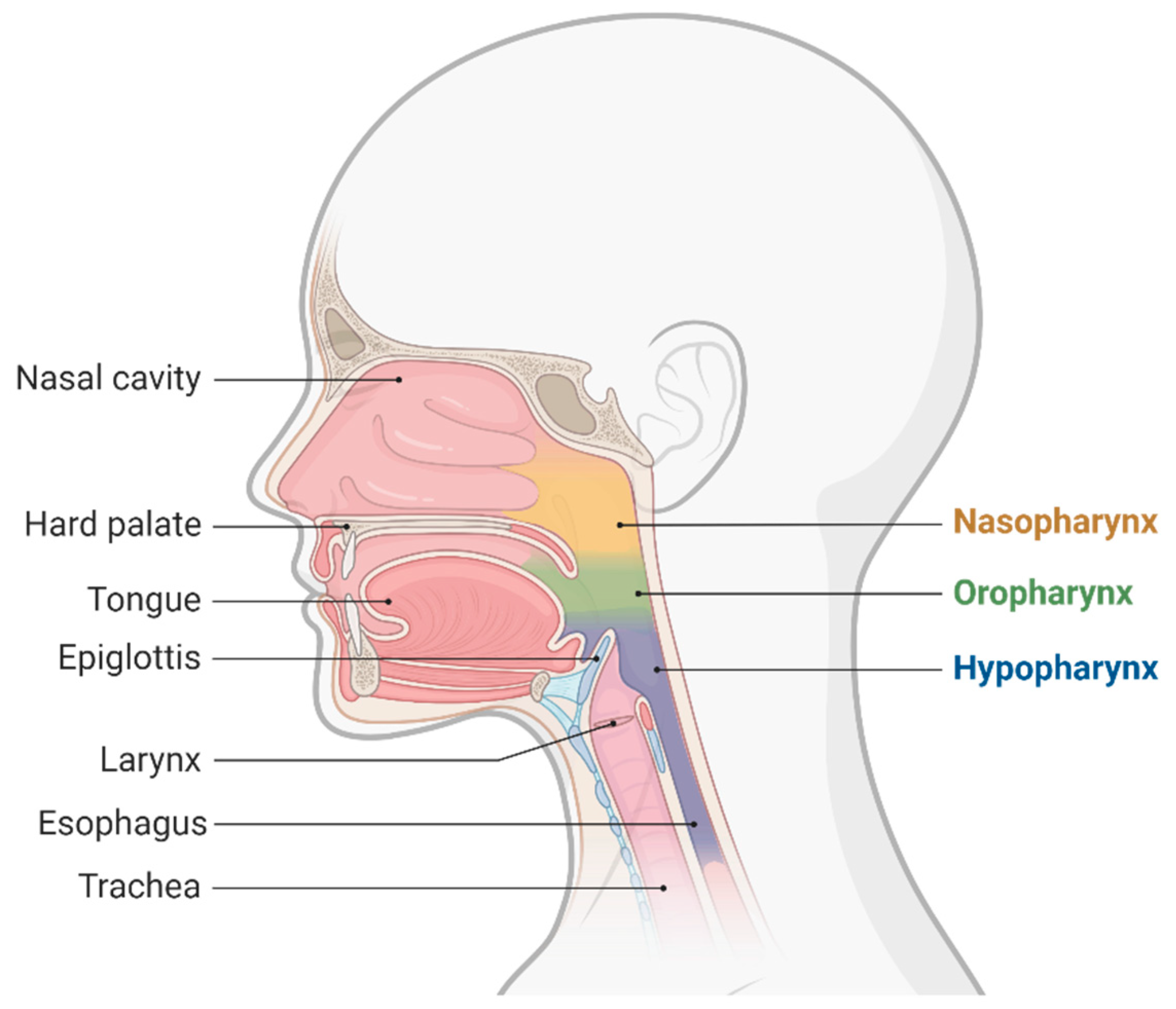
Figure 1. Upper airway anatomy.
3.1. Ultrasound Approaches Which Are Practical for the Airway
Several ultrasonographic approaches are known and used to evaluate the airway: the transcutaneous ultrasound of the airway, the endobronchial evaluation, and the transoral or sublingual approach [12].
The transcutaneous approach comprises the trans laryngeal and transtracheal ultrasound windows used to evaluate the upper airway and can be performed using either a low- or a high-frequency transducer. The orientation of the probes can be one of the following: sagittal, parasagittal, oblique, or transverse [12][13][14] (Scheme 1).
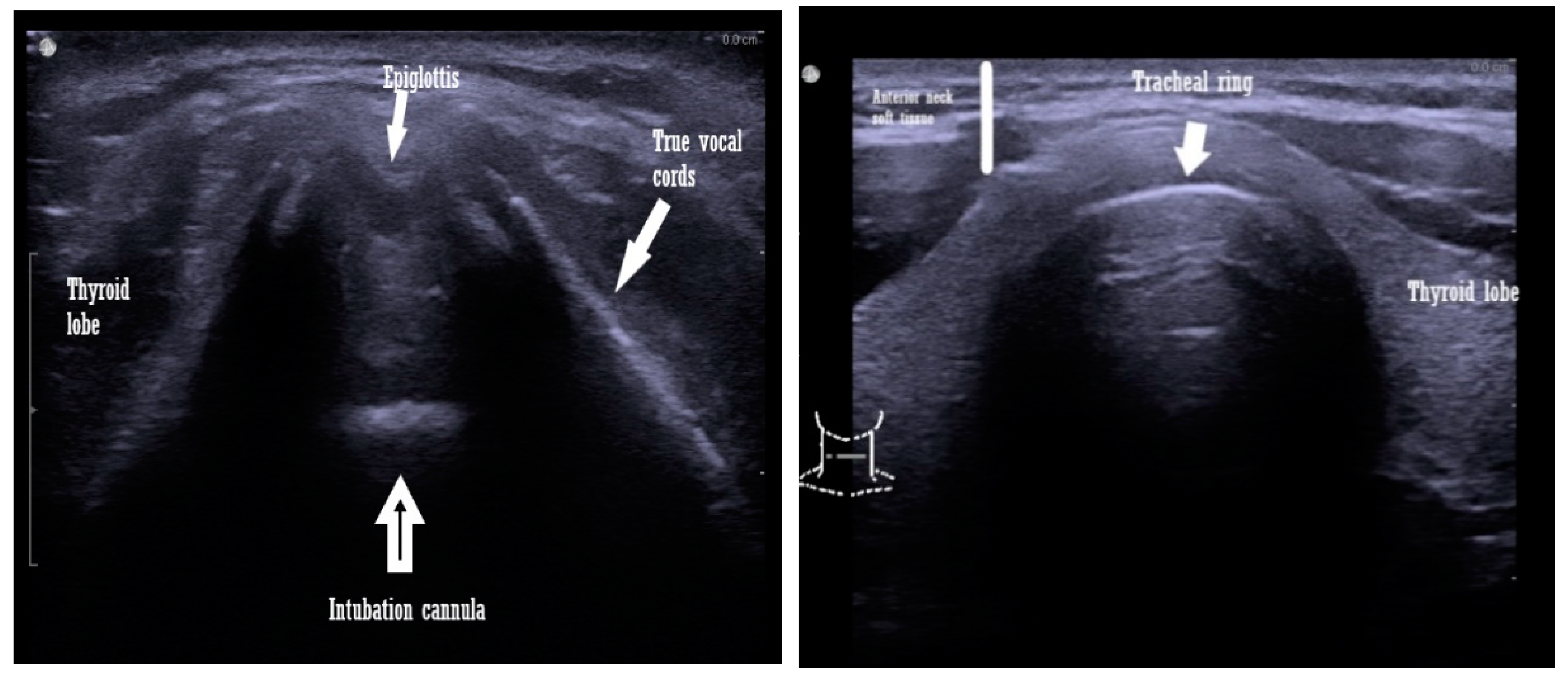
Scheme 1. Transcutaneous view with a linear ultrasound probe of an intubated patient airway (left image) and a non intubated patient (right image).
The endobronchial evaluation is a combination of the transcutaneous approach and bronchoscopy. It is more elaborate and requires complex equipment [14].
The transoral or sublingual approach is the least favored by both the anesthesiologists and the patients. It implies the insertion of the probe under the patient s tongue, which makes it uncomfortable for the patient. The great advantage of this approach is that provides excellent-quality ultrasound images, due to good probe-tissue contact [15].
3.2. Airway Measurements Performed by Ultrasound
Different distances and diameters or ratios between these structures are measured to identify the best one for predicting a difficult airway. Additionally, any anatomical anomalies or masses, if present, can also be identified with an ultrasound [16].
Although the anatomical structures that need to be visualized by the ultrasound window are well established, it is not clear which of these or which combination of diameters and distances are the best predictors for a difficult airway.
The literature presents different results with many ultrasound measurements proposed. Some of these are presented below.
-
Tongue thickness and anterior neck soft tissue, at the level of the hyoid bone, are measured from the skin on the short axis [17].
-
Thyrohyoid membrane: from the hyoid bone to the thyroid membrane [17].
-
Transverse tracheal air shadow diameter in the subglottic area of the front of the neck: from the mid-front part of the neck, at the level of true vocal cords [18].
-
Soft tissue depth at the vocal cords and the suprasternal notch of the distance from the skin to the anterior part of the trachea, determined at three levels: vocal cords, thyroid isthmus, and suprasternal notch. The amount of soft tissue in each zone is considered the average of the amounts of soft tissue obtained in the central axis of the neck and ≈1.5 mm to the left and right of the central axis [19].
-
The distance from the epiglottis to the midpoint of the distance between the vocal folds (E-VC) [20].
-
Submandibular ultrasound of the hyomental distance ratio: the hyomental distance measured in neutral and in the hyperextended position of the neck [23].
-
Tongue volume is the result of the multiplication of the mid-sagittal cross-sectional area, by its width, in a transverse ultrasonogram [23].
-
Visibility of the hyoid bone [21].
-
Anterior commissure: the shortest distance from the skin to the anterior commissure [24].
-
Tongue thickness and the ratio to thyromental distance: measured in the medial sagittal plane, after asking the patient to rest the tip of the tongue on their lower incisors, since the tongue is a dynamic muscle [25].
All of these diameters and ratios were measured with the patient in the supine position, except the hyomental ratio, which was measured in the resting position of the conscious patient.
References
- Terkawi, A.; Karakitsos, D.; Elbarbary, M.; Blaivas, M.; Durieux, M.E. Ultrasound for the Anesthesiologists: Present and Future. Sci. World J. 2013, 2013, 683685.
- Lau, B.C.; Motamedi, D.; Luke, A. Use of Pocket-Sized Ultrasound Device in the Diagnosis of Shoulder Pathology. Clin. J. Sport Med. 2018, 30, 20–24.
- Sole, M.L.; Su, X.; Talbert, S.; Penoyer, D.A.; Kalita, S.; Jimenez, E.; Ludy, J.E.; Bennett, M. Evaluation of an Intervention to Maintain Endotracheal Tube Cuff Pressure Within Therapeutic Range. Am. J. Crit. Care 2011, 20, 109–118.
- Kristensen, M.S.; Teoh, W.H. Ultrasound identification of the cricothyroid membrane: The new standard in preparing for front-of-neck airway access. Br. J. Anaesth. 2020, 126, 22–27.
- Cook, T.M.; MacDougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109, i68–i85.
- Law, J.A.; Canadian Airway Focus Group; Broemling, N.; Cooper, R.M.; Drolet, P.; Duggan, L.V.; Griesdale, D.E.; Hung, O.R.; Jones, P.M.; Kovacs, G.; et al. The difficult airway with recommendations for management—Part 2—The anticipated difficult airway. Can. J. Anaesth. 2013, 60, 1119–1138.
- Yentis, S.M. Predicting difficult intubation—Worthwhile exercise or pointless ritual? Anaesthesia 2002, 57, 105–109.
- Lundstrøm, L.H.; Vester-Andersen, M.; Møller, A.M.; Charuluxananan, S.; L’Hermite, J.; Wetterslev, J. Poor prognostic value of the modified Mallampati score: A meta-analysis involving 177,088 patients. Br. J. Anaesth. 2011, 107, 659–667.
- Das, P.K.; Bellapukonda, S.; Nayak, B.M.; Mallick, M. Can intubate but cannot ventilate! An unexpected event in a child with stridor after accidental aspiration of the potassium permanganate solution. Saudi J. Anaesth. 2020, 14, 272–273.
- Shiga, T.; Wajima, Z.I.; Inoue, T.; Sakamoto, A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. J. Am. Soc. Anesthesiol. 2005, 103, 429–437.
- Jain, K.; Yadav, M.; Gupta, N.; Thulkar, S.; Bhatnagar, S. Ultrasonographic assessment of airway. J. Anaesthesiol. Clin. Pharmacol. 2020, 36, 5.
- Kristensen, S. Ultrasonography in the management of the airway. Acta Anaesthesiol. Scand. 2011, 55, 1155–1173.
- Patel, A.; Spychalski, P.; Aszkiełowicz, A.; Mikaszewski, B.; Kobiela, J. Transcutaneous Laryngeal Ultrasound for Vocal Cord Paralysis Assessment in Patients Undergoing Thyroid and Parathyroid Surgery—A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5393.
- Beaudoin, E.L.; Chee, A.; Stather, D.R. Interventional pulmonology: An update for internal medicine physicians. Minerva Med. 2014, 105, 197–209.
- Tsui, B.C.; Hui, C.M. Challenges in sublingual airway ultrasound interpretation. Can. J. Anesth. J. Can. D’anesthésie 2009, 56, 393–394.
- Fulkerson, J.S.; Moore, H.M.; Anderson, T.S.; Lowe, R.F. Ultrasonography in the preoperative difficult airway assessment. Int. J. Clin. Monit. Comput. 2016, 31, 513–530.
- Adhikari, S.; Zeger, W.; Schmier, C.; Crum, T.; Craven, A.; Frrokaj, I.; Pang, H.; Shostrom, V. Pilot Study to Determine the Utility of Point-of-care Ultrasound in the Assessment of Difficult Laryngoscopy. Acad. Emerg. Med. 2011, 18, 754–758.
- Aydogmus, M.T.; Erkalp, K.; Sinikoglu, S.N.; Usta, T.A.; Ulger, G.O.; Alagol, A. Is ultrasonic investigation of transverse tracheal air shadow diameter reasonable for evaluation of difficult airway in pregnant women: A prospective comparative study. Pak. J. Med. Sci. 2014, 30, 91.
- Ezri, T.; Gewürtz, G.; Sessler, D.I.; Medalion, B.; Szmuk, P.; Hagberg, C.; Susmallian, S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue*. Anaesthesia 2003, 58, 1111–1114.
- Carsetti, A.; Sorbello, M.; Adrario, E.; Donati, A.; Falcetta, S. Airway Ultrasound as Predictor of Difficult Direct Laryngoscopy: A Systematic Review and Meta-analysis. Anesth. Analg. 2022, 134, 740.
- Gupta, D.; Srirajakalidindi, A.; Ittiara, B.; Apple, L.; Toshniwal, G.; Haber, H. Ultrasonographic modification of Cormack Lehane classification for pre-anesthetic airway assessment. Middle East J. Anaesthesiol. 2012, 21, 835–842.
- Pinto, J.; Cordeiro, L.; Pereira, C.; Gama, R.; Fernandes, H.L.; Assunção, J. Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J. Crit. Care 2016, 33, 26–31.
- Wojtczak, J.A. Submandibular sonography: Assessment of hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable sonography. J. Ultrasound Med. 2012, 31, 523–528.
- Wu, J.; Dong, J.; Ding, Y.; Zheng, J. Role of anterior neck soft tissue quantifications by ultrasound in predicting difficult laryngoscopy. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2014, 20, 2343.
- Yao, W.; Wang, B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? BJA Br. J. Anaesth. 2017, 118, 601–609.
More
Information
Subjects:
Anesthesiology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.6K
Revisions:
3 times
(View History)
Update Date:
21 Nov 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




