Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Edward A Bittner | -- | 1844 | 2022-11-08 13:42:22 | | | |
| 2 | Rita Xu | Meta information modification | 1844 | 2022-11-09 02:47:31 | | | | |
| 3 | Rita Xu | Meta information modification | 1844 | 2022-11-10 07:57:24 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Tankard, K.A.; Sharifpour, M.; Chang, M.G.; Bittner, E.A. Emergency Airway Management. Encyclopedia. Available online: https://encyclopedia.pub/entry/33531 (accessed on 07 February 2026).
Tankard KA, Sharifpour M, Chang MG, Bittner EA. Emergency Airway Management. Encyclopedia. Available at: https://encyclopedia.pub/entry/33531. Accessed February 07, 2026.
Tankard, Kelly A., Milad Sharifpour, Marvin G. Chang, Edward A. Bittner. "Emergency Airway Management" Encyclopedia, https://encyclopedia.pub/entry/33531 (accessed February 07, 2026).
Tankard, K.A., Sharifpour, M., Chang, M.G., & Bittner, E.A. (2022, November 08). Emergency Airway Management. In Encyclopedia. https://encyclopedia.pub/entry/33531
Tankard, Kelly A., et al. "Emergency Airway Management." Encyclopedia. Web. 08 November, 2022.
Copy Citation
Emergency airway management (EAM) is a commonly performed procedure in the critical care setting. Despite clinical advances that help practitioners identify patients at risk for having a difficult airway, improved airway management tools, and algorithms that guide clinical decision-making, there remains significant morbidity and mortality associated with EAM.
airway response team
emergency airway management
intubation-related complications
1. Introduction
Emergency airway management (EAM) is commonly performed in the hospital setting. However, despite advances in identifying patients at increased risk for having a difficult airway, improved airway management tools, and algorithms to assist with EAM decision-making, there remains significant morbidity and mortality associated with EAM [1][2]. Evidence suggest that a dedicated airway response team (ART) can reduce the risks associated with EAM and improve patient outcomes [3][4][5][6]. Here, researchers review the risks and challenges related to EAM and describe strategies and key elements to improve patient care via implementation of an ART (Figure 1).
2. Risks Associated with EAM
Risks associated with EAM include physiological complications (e.g., hypoxemia and hemodynamic instability), traumatic complications (e.g., dental and soft tissue injury) and procedure-related complications (e.g., esophageal intubation and aspiration) (Table 1) [9][10]. The complication rate of EAM outside of the operating room (OR) setting exceeds 45% [1]. Hypotension and hypoxemia occur frequently during EAM and have been associated with increased mortality even after adjusting for other variables [1][11][12]. In 2011, the 4th National Audit Project of the Royal College of Anaesthetists (NAP4) published a comprehensive examination of major complications associated with airway management in the United Kingdom which found 40- and 50-fold higher risks of hypoxic brain injury and mortality for airway management performed in the emergency room and intensive care unit (ICU), respectively, when compared to routine intubation in the OR [2]. Subsequent analysis by the NAP4 investigators identified provider inexperience, lack of adherence to EAM guidelines, and absence of a clear contingency plan in the event of failed initial attempts as factors responsible for 40% of the adverse outcomes [9]. While a follow-up survey showed that many UK hospitals had instituted changes based on the NAP4 findings, a “safety gap” remains between ideal practice and what occurs in actual practice [13]. A recent analysis of EAM related complications included in the American Society of Anesthesiologists (ASA) closed-claims database also showed that human factors played a prominent role in EAM-related complications [14]. The closed claims analysis concluded that the majority of death or permanent brain damage related to difficult endotracheal intubation occurred due to insufficient knowledge (not recognizing risk factors for difficult airway management or not knowing the guidelines), systems failures (rescue equipment or personnel not being available), and delays in decision-making (such as progression to cricothyrotomy), and were preventable [15]. Based on these findings, strategies to reduce the risks of EAM are urgently needed.
Table 1. Complications of Emergency Airway Management.
| Physiologic Complications | Traumatic Complications | Procedure-Related Complications |
|---|---|---|
|
|
|
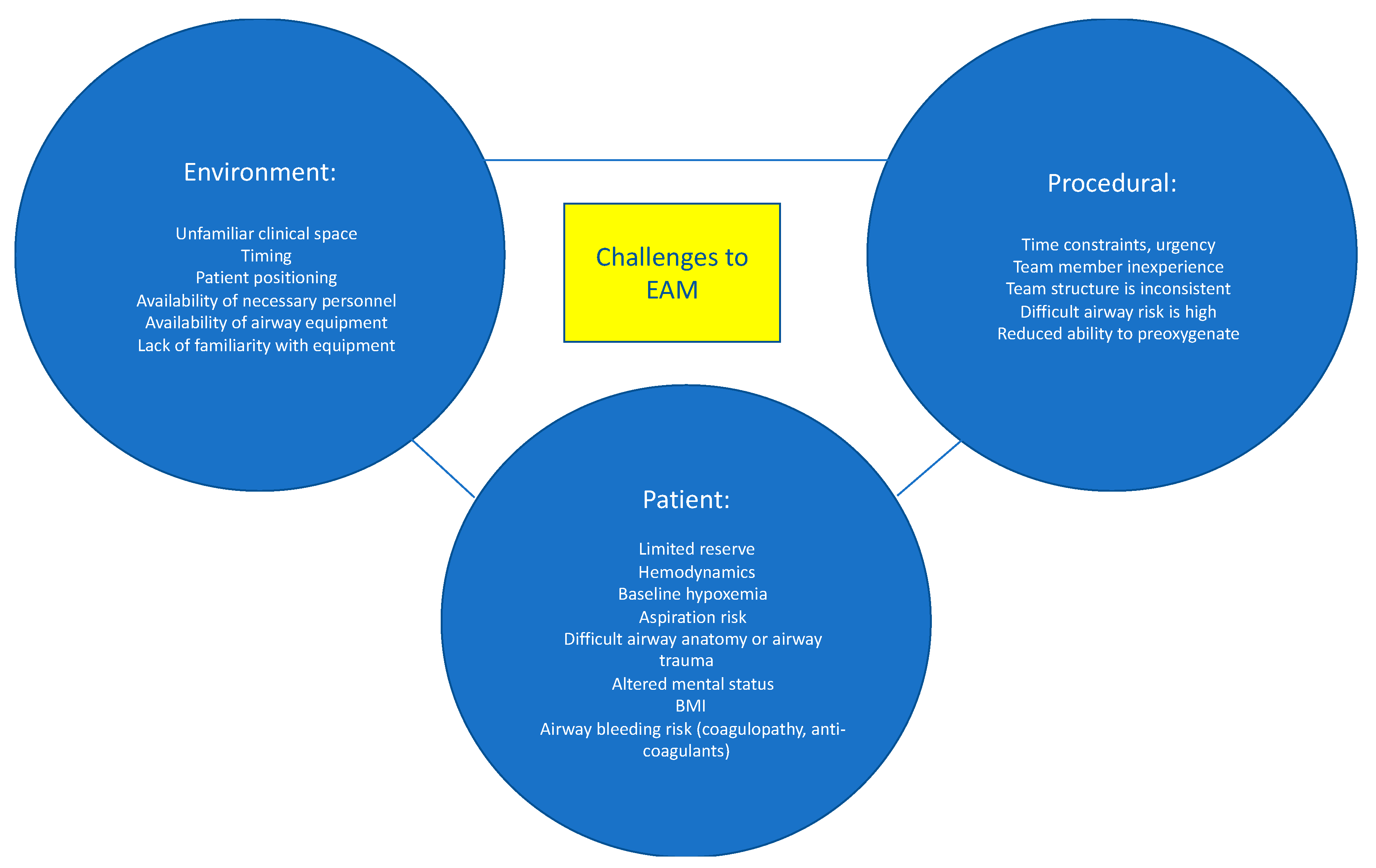
3. Challenges in EAM
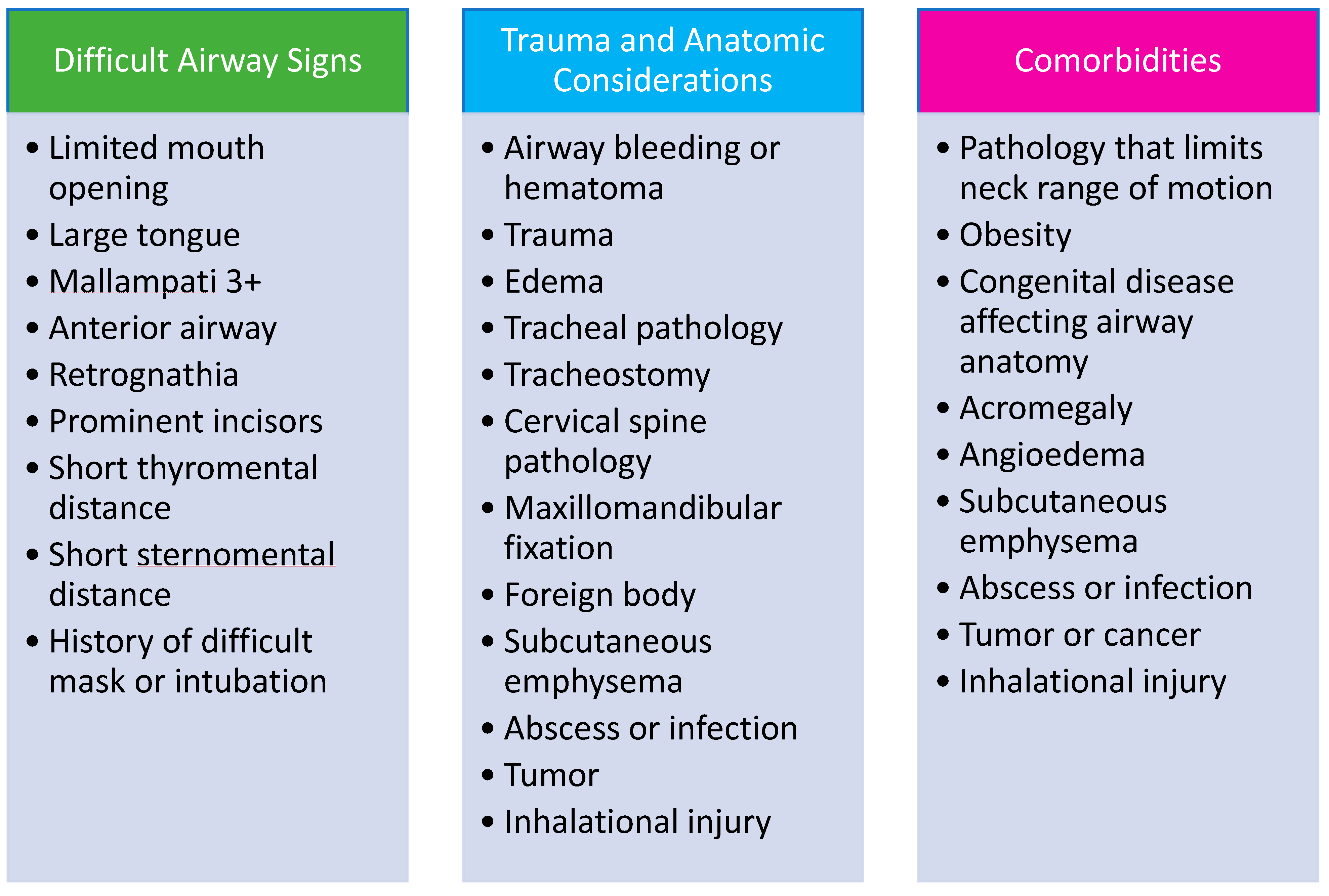
The risks associated with EAM are multifactorial and are attributed to patient-related, procedure-related, and environmental-related factors (Figure 1) [7]. Patients who require EAM are often hemodynamically unstable and may not tolerate the hemodynamic perturbations associated with endotracheal intubation. Efforts to provide preoxygenation prior to intubation may be difficult or less effective due to patient agitation, hemodynamic instability, and ventilation-perfusion mismatch. Less effective preoxygenation limits the amount of time available to secure the airway before the development of dangerously low oxygen saturation levels and cardiopulmonary collapse. Poor tissue perfusion may result in inaccurate or unmeasurable oxygen saturation (SpO2) readings, which further confound patient assessment and monitoring. Hypoxemia, hypercarbia, and respiratory distress result in increased sympathetic outflow, which elevates blood pressure and may result in a false sense of “hemodynamic stability”, followed by an exaggerated drop in blood pressure once the airway is secured. Induction medications, given to facilitate intubation, can worsen hypotension by decreasing systemic vascular resistance and depressing myocardial contractility. Patients requiring EAM often have full stomachs and are at increased risk for aspiration of gastric contents. Anatomical abnormalities such as cervical spine instability, orotracheal or laryngeal tumors, history of neck radiation, airway edema or stenosis, or prior airway instrumentation are additional risk factors for adverse events during EAM. Lastly, the increasing prevalence of obesity and the number of patients who receive anticoagulation increase the risk of EAM-related complications.
Although difficult or failed orotracheal intubation is typically the focus of EAM strategies, acute airway dislodgement, bleeding, or obstruction of an existing surgical airway (e.g., tracheostomy or laryngectomy) can pose equally daunting challenges [16]. Critical airway events frequently occur in patients with previously secured airways. In one series, 82% of the critical airway events occurred after intubation, with 25% of these events contributing to patient deaths [17].
The clinical environments in which EAM is performed pose yet another challenge; airway emergencies can occur in remote places, resulting in delayed response times. Furthermore, the responding clinicians may not know the bedside providers and the resources that are available to them, which may result in suboptimal communication and division of tasks. Patient positioning is more difficult on a hospital bed or in a CT scanner compared to an OR table, resulting in limited access to the patient and suboptimal positioning, which make airway management more difficult. Similarly, EAM often occurs after hours, when fewer clinicians are available to provide assistance [18]. In addition, clinicians responding to EAM are often less experienced than providers who perform routine airway management in the OR [1][19][20]. Given the instability of many patients requiring EAM, delaying management until more experienced staff are available is often not feasible. The risks, challenges, and complications associated with EAM justify the creation of dedicated ARTs.
4. Rationale for an Airway Response Team
The importance of an organized, systematic, and team-based approach to patient care in emergency settings is well-established and serves as the basis for programs like Advanced Cardiovascular Life Support (ACLS) [21]. Nonetheless, EAM has historically been managed by a single clinician, often a trainee, rather than a team [22]. The desire to improve patient safety and mitigate the risks and complications associated with EAM, as described above, has led to creation of ARTs in many institutions [3][4][5][6][23][24][25][26][27]. There is growing evidence that the team approach to EAM can improve outcomes by reducing patient complications, death, and malpractice claims [3][4][5][6][25].
The ART model highlights the different skills that are required for successful EAM. As such, ARTs are often multidisciplinary teams that include respiratory therapists, nurses, anesthesiologists, and surgeons, and may include both trainees and attending physicians [28]. Highly effective ARTs should have the ability to immediately convert to a surgical airway without delay in the event of a failed intubation. Since anesthesiologists do not routinely perform surgical airways and many graduating surgical trainees have never performed an emergency surgical airway [15][29], a surgeon trained in performing surgical airways should be available in the event of a failed mask ventilation and intubation [27].
5. The Team Model
The main objective of the ART is to rapidly assemble team members and resources to assess and manage a patient with an airway emergency. Having a designated team of clinicians with airway expertise and a method for activation that alerts and assembles the team for EAM in advance of an intervention is a distinctly superior approach to “calling for help” in an emergency after a practitioner has unsuccessfully attempted to manage an airway. The Difficult Airway Society has proposed several models for an ART, suggesting that the team ideally includes two clinicians with advanced airway management skills (intubation) [30]. The delegation of tasks and roles depends on how many members are on the ART. For a smaller group, one team member may need to take on multiple roles. Additionally, depending on the number and clinical experience of the team members, the duties may change during EAM. For example, if there is a failed first attempt at intubation, the second (ideally more experienced) clinician may take over. There should also be a designated team leader who guides the team. As previously stated, a clinician (typically a surgeon) who is trained in emergency front of the neck access (FONA) should be readily available. However, providing 24/7 in-house coverage with a surgeon who is trained in FONA often poses a challenge to the ART model, especially in smaller hospitals with fewer resources. Depending on the institutional resources, there are a range of clinical specialists, including emergency medicine physicians, intensivists, and anesthesiologists who may be trained to be proficient in surgical airway techniques if 24/7 in-house surgical coverage is not possible. Nurses, pharmacists, respiratory therapists, and a technician capable of providing and managing the equipment required for EAM are the other vital components of the team (Figure 2). The patient’s primary nurse and medical team should also be considered part of the ART, as they can provide important contextual information relating to the patient’s history and clinical course and can communicate with and provide comfort to the patient during EAM. Lastly, hospital administrators are also considered part of the ART, and their role is to invest in resource allocation, training programs, and education of ART staff. Telemedicine may play an emerging role in managing ARTs in settings where expertise is not readily available [31][32].
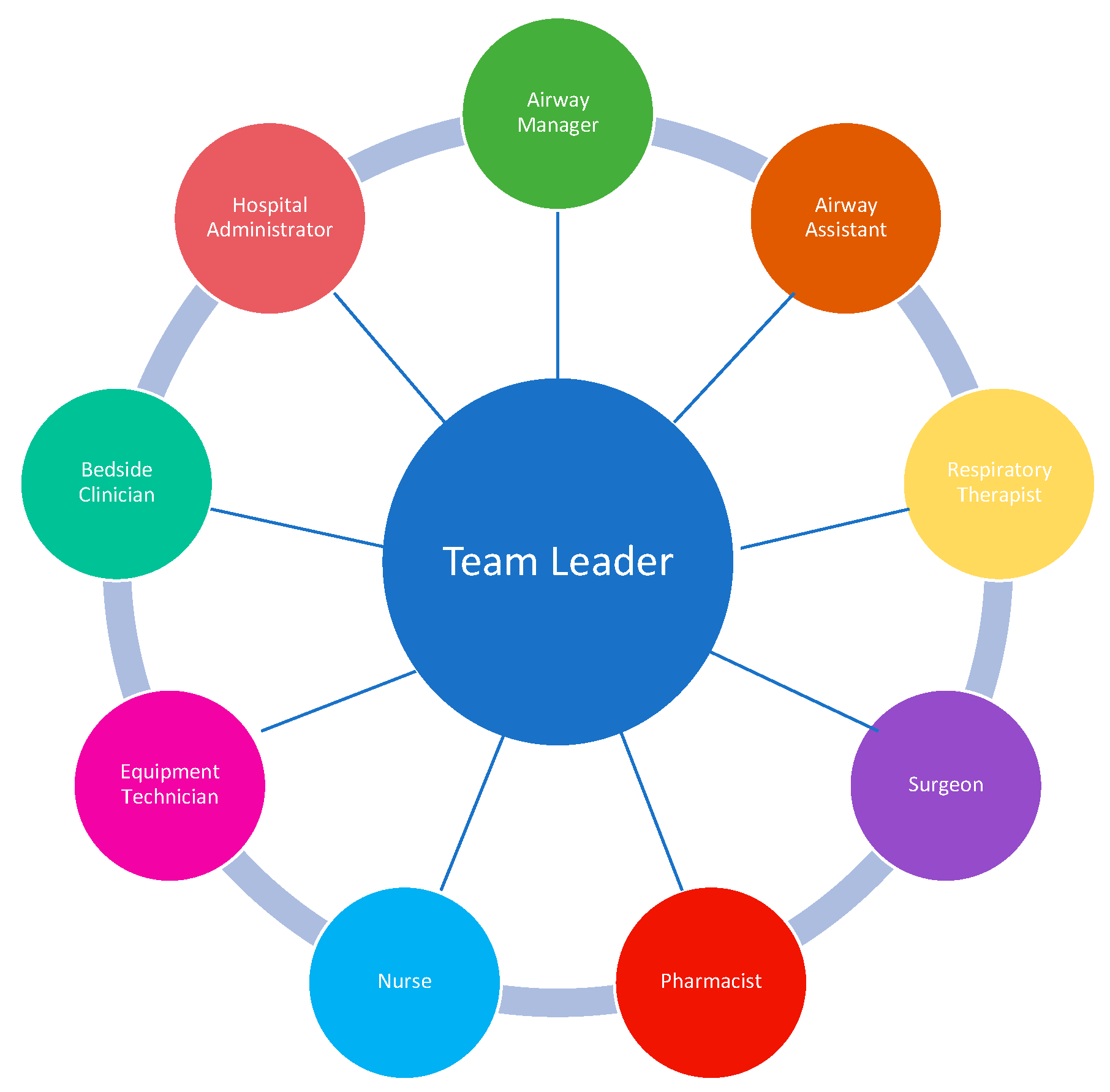
Figure 2. ART Team Members. Data from Long L, Vanderhoff B, Smyke N et al. [23] and Damrose JF, Eropkin W, Ng S et al. [24].
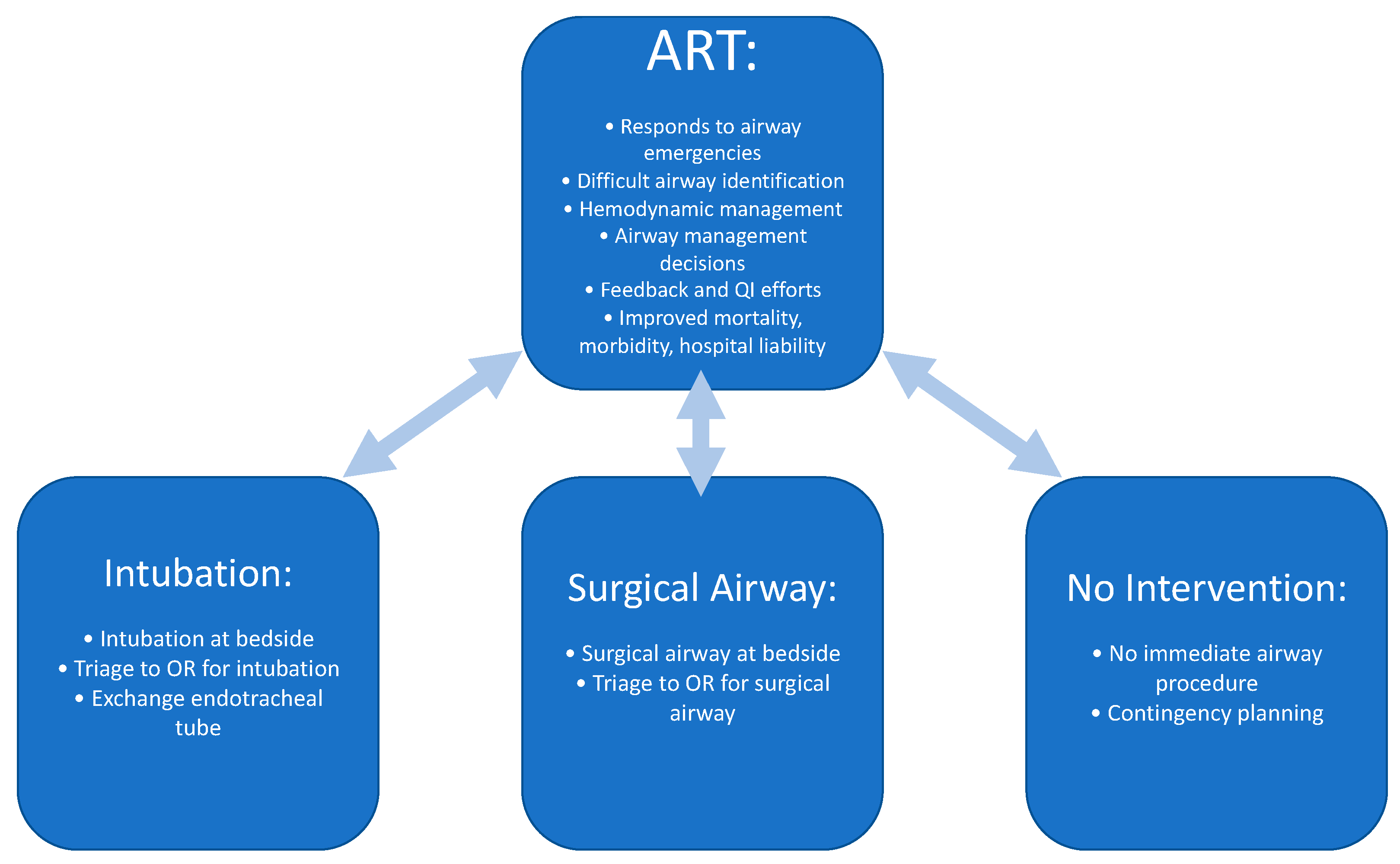
6. Activation
The ART is valuable not only for proceeding with emergent airway interventions but also for assessment, triaging, and planning of patients with airway issues [28]. While an ART often provides immediate airway intervention either by intubation or surgical airway, other valuable roles of the ART include triaging a patient to the OR for airway management, assessment and determination that no immediate action is necessary, formulating a plan should an airway management be required in the future, or assessing a patient with a history of difficult intubation for readiness prior to extubation (Figure 3).
Timely and appropriate activation of the ART are essential to ensure the best patient outcomes. Providing clinicians with clear criteria for ART activation and a consistent way to notify the team is key to success. Strategies to educate hospital staff on how and when to activate the ART include in training sessions, information sheets posted in key locations throughout email notifications, and required web-based training. Implementing an ART will require educating care teams as well as the ART responders. Staff should be educated on what information to provide to the ART at the time of activation (Figure 4). A system should be developed to monitor the timeliness and appropriateness of ART notifications and feedback should be provided to bedside providers and team members to improve performance.
References
- Russotto, V.; Myatra, S.N.; Laffey, J.G.; Tassistro, E.; Antolini, L.; Bauer, P.; Lascarrou, J.B.; Szułdrzyński, K.; Camporota, L.; Pelosi, P.; et al. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA 2021, 325, 1164–1172.
- Cook, T.M.; Woodall, N.; Harper, J.; Benger, J. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. Br. J. Anaesth. 2011, 106, 632–642.
- Mark, L.; Lester, L.; Cover, R.; Herzer, K. A decade of difficult airway response team: Lessons learned from a hospital-wide difficult airway response team program. Crit. Care Clin. 2018, 34, 239–251.
- Henderson, S.O.; McClung, C.D.; Sintuu, C.; Swadron, S.P. The Presence of an Emergency Airway Response Team and Its Effects on In-Hospital Code Blue. J. Emerg. Med. 2009, 36, 116–120.
- Berkow, L.C.; Greenberg, R.S.; Kan, K.H.; Colantuoni, E.; Mark, L.J.; Flint, P.W.; Corridore, M.; Bhatti, N.; Heitmiller, E.S. Need for Emergency Surgical Airway Reduced by a Comprehensive Difficult Airway Program. Anesth. Analg. 2009, 109, 1860–1869.
- Walsh, E.C.; Kwo, J.; Chang, M.G.; Pino, R.M.; Bittner, E.A. Rapid Expansion of the Airway Response Team to Meet the Needs of the COVID-19 Pandemic. J. Healthc. Qual. 2021, 43, 275–283.
- Higgs, A.; Cook, T.M.; McGrath, B.A. Airway management in the critically ill: The same, but different. Br. J. Anaesth. 2016, 117, i5–i9.
- Jabaley, C.; Bittner, E.A. Myths and misconceptions regarding emergency airway management 2016. In Current Concepts in Adult Critical Care; Society of Critical Care Medicine: Chicago, IL, USA, 2016.
- Cook, T.M.; MacDougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109, i68–i85.
- Hagberg, C.; Georgi, R.; Krier, C. Complications of managing the airway. Best Pract. Res. Clin. Anaesthesiol. 2005, 19, 641–659.
- Heffner, A.C.; Swords, D.; Kline, J.A.; Jones, A.E. The frequency and significance of postintubation hypotension during emergency airway management. J. Crit. Care 2012, 27, 417.e9–417.e13.
- Spaite, D.W.; Hu, C.; Bobrow, B.J.; Chikani, V.; Barnhart, B.; Gaither, J.B.; Denninghoff, K.R.; Adelson, P.D.; Keim, S.M.; Viscusi, C.; et al. The Effect of Combined Out-of-Hospital Hypotension and Hypoxia on Mortality in Major Traumatic Brain Injury. Ann. Emerg. Med. 2017, 69, 62–72.
- Cook, T.M.; Woodall, N.; Frerk, C. A national survey of the impact of NAP4 on airway management practice in United Kingdom hospitals: Closing the safety gap in anaesthesia, intensive care and the emergency department. Br. J. Anaesth. 2016, 117, 182–190.
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2020, 131, 818–829.
- Asai, T.; Hillman, D. Current difficult airway management—Not good enough! Anesthesiology 2019, 131, 774–776.
- Rassekh, C.H.; Zhao, J.; Martin, N.D.; Chalian, A.A.; Atkins, J.H. Tracheostomy complications as a trigger for an airway rapid response: Analysis and quality improvement considerations. Otolaryngol.-Head Neck Surg. 2015, 153, 921–926.
- Thomas, A.N.; McGrath, B. Patient safety incidents associated with airway devices in critical care: A review of reports to the UK National Patient Safety Agency. Anaesthesia 2009, 64, 358–365.
- Adams, M.C.; Schmidt, U.; Hess, D.R.; Stelfox, H.T.; Bittner, E.A. Examination of Patterns in Intubation by an Emergency Airway Team at a Large Academic Center: Higher Frequency During Daytime Hours. Respir. Care 2014, 59, 743–748.
- Bittner, E.A.; Schmidt, U. Examining the Learning Practice of Emergency Airway Management Within an Academic Medical Center: Implications for Training and Improving Outcomes. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520965257.
- Andrews, J.D.; Nocon, C.C.; Small, S.M.; Pinto, J.M.; Blair, E.A. Emergency airway management: Training and experience of chief residents in otolaryngology and anesthesiology. Head Neck 2012, 34, 1720–1726.
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357.
- Rochlen, L.R.; Housey, M.; Gannon, I.; Mitchell, S.; Rooney, D.M.; Tait, A.R.; Engoren, M. Assessing anesthesiology residents’ out-of-the-operating-room (OOOR) emergent airway management. BMC Anesthesiol. 2017, 17, 96.
- Long, L.; Vanderhoff, B.; Smyke, N.; Shaffer, L.E.T.; Solomon, J.; Steuer, J.D. Management of difficult airways using a hospital-wide “alpha team” approach. Am. J. Med. Qual. 2010, 25, 297–304.
- Damrose, J.F.; Eropkin, W.; Ng, S.; Cale, S.; Banerjee, S. The Critical Response Team in Airway Emergencies. Perm. J. 2019, 23, 18–219.
- Atkins, J.H.; Rassekh, C.H.; Chalian, A.A.; Zhao, J. An Airway Rapid Response System: Implementation and Utilization in a Large Academic Trauma Center. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 653–660.
- Sterrett, E.C.; Myer IV, C.M.; Oehler, J.; Das, B.; Kerrey, B.T. Critical airway team: A retrospective study of an airway response system in a pediatric hospital. Otolaryngol.-Head Neck Surg. 2017, 157, 1060–1067.
- Atkins, J.H.; Rassekh, C.H. Multidisciplinary airway response teams: Concept, structure, & implementation. Oper. Tech. Otolaryngol. Neck Surg. 2020, 31, 105–110.
- Bittner, E.A.; Sharifpour, M. The Team Approach to Emergency Airway Management: Rationale, Structure, & Implementation. In Airway and Mechanical Ventilation Management; Bittner, E.A., Wilcox, S., Gallagher, J., Eds.; Society of Critical Care Medicine: Chicago, IL, USA, 2021.
- Aho, J.M.; Thiels, C.A.; AlJamal, Y.N.; Ruparel, R.K.; Rowse, P.G.; Heller, S.F.; Farley, D.R. Every Surgical Resident Should Know How to Perform a Cricothyrotomy: An Inexpensive Cricothyrotomy Task Trainer for Teaching and Assessing Surgical Trainees. J. Surg. Educ. 2015, 72, 658–661.
- Higgs, A.; McGrath, B.A.; Goddard, C.; Rangasami, J.; Suntharalingam, G.; Gale, R.; Cook, T.M.; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; et al. Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 2018, 120, 323–352.
- Dalesio, N.M.; Lester, L.C.; Barone, B.; Deanehan, J.K.; Fackler, J.C. Real-time emergency airway consultation via telemedicine: Instituting the pediatric airway response team board! Anesth. Analg. 2020, 130, 1097–1102.
- Levin, B.S.; Chang, M.G.; Bittner, E.A. Teleguidance Technology for Endotracheal Intubation: A Scoping Review. Crit. Care Explor. 2021, 3, e0582.
- Feinleib, J.; Foley, L.; Mark, L. What we all should know about our patient’s airway: Difficult airway communications, database registries, and reporting systems registries. Anesthesiol. Clin. 2015, 33, 397–413.
More
Information
Subjects:
Critical Care Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
3 times
(View History)
Update Date:
10 Nov 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No